Morphological Evaluation of Bone by CT to Determine Primary Stability—Clinical Study
Abstract
1. Introduction
2. Subjects and Methods
2.1. CT
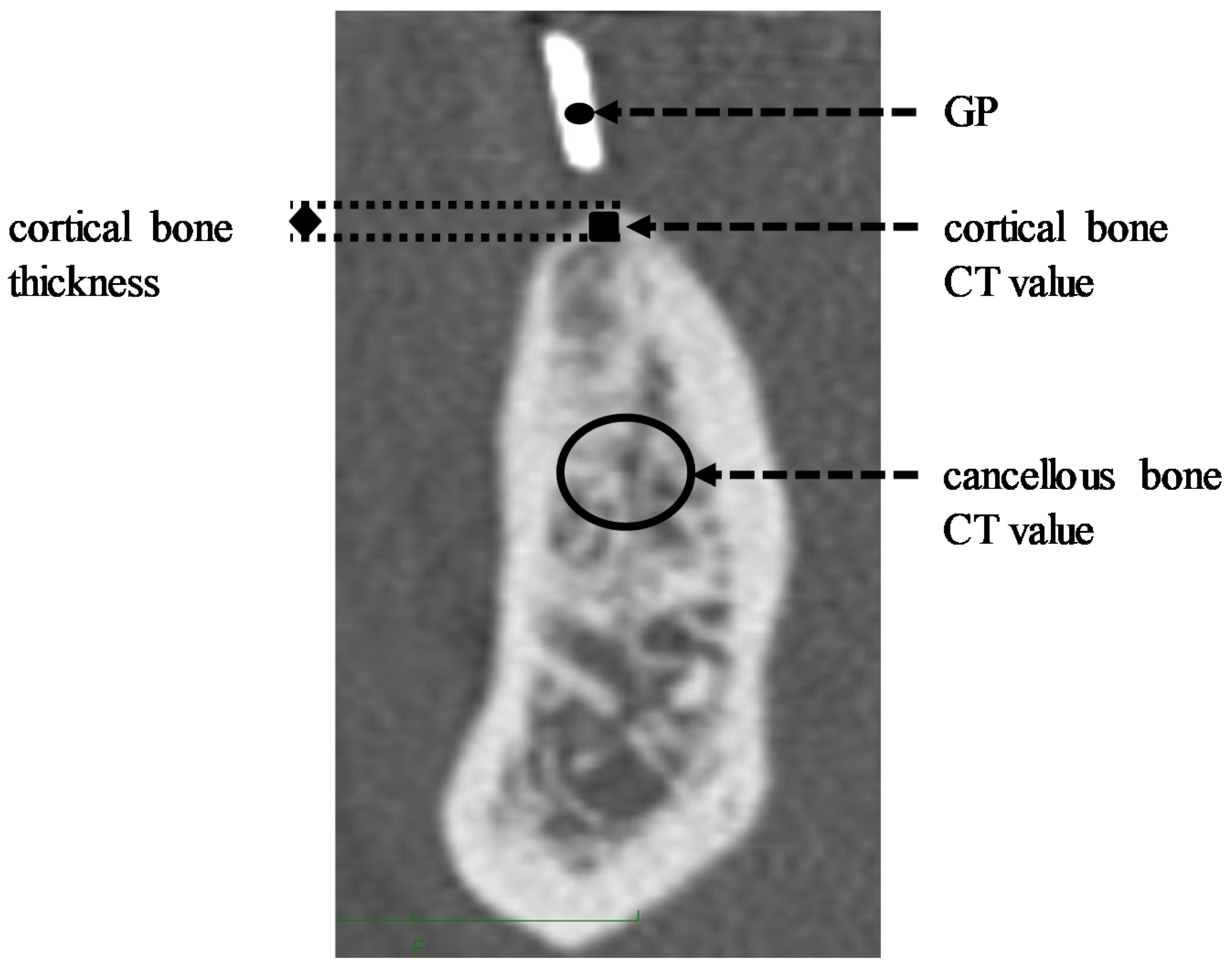
2.2. CT Measuring Method
2.3. CT Value Correction
2.4. ISQ
2.5. Analysis
3. Results
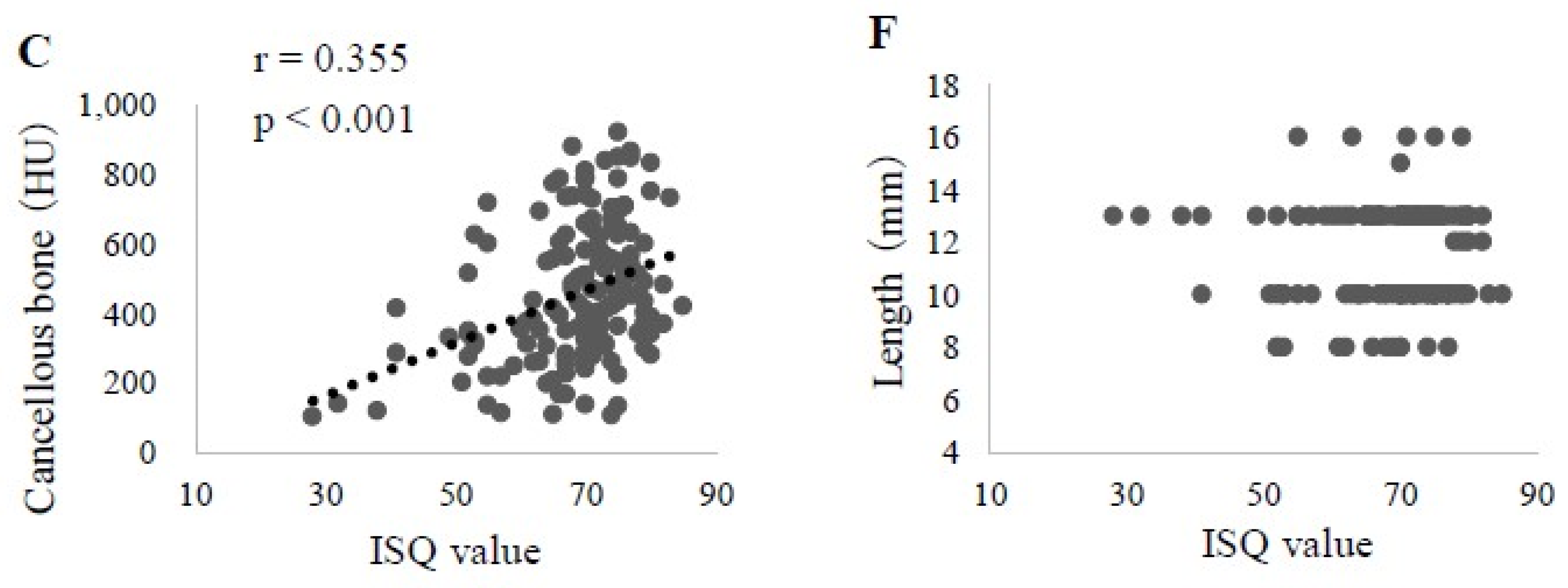
3.1. Factors Affecting ISQ Values in All Cases
3.2. Factors Affecting ISQ Values in Upper Jaw
3.3. Factors Affecting ISQ Values in Lower Jaw
4. Discussion
4.1. Subjects
4.2. CT Value Correction
4.3. Factors Affecting ISQ in Upper Jaw
4.4. Factors Affecting ISQ Value in Lower Jaw
5. Conclusions
- (1)
- Factors that showed a significant correlation with the ISQ value in all subjects were cortical bone thickness, cortical bone CT value, cancellous bone CT value, ITV, and implant diameter and length. Multiple regression analysis, using the ISQ value as the objective variable, revealed that cortical bone thickness and cancellous bone CT value had a significant association with ISQ. These results indicated that cortical bone thickness has a great effect on predicting the ISQ value.
- (2)
- In the upper jaw, cortical bone thickness, cortical bone CT value, cancellous bone CT value, ITV, and implant diameter showed a significant correlation with ISQ. Multiple regression analysis, using the ISQ value as the objective variable, revealed a significant association of cortical bone thickness and cancellous bone CT value with ISQ. These results also indicated a significant effect of cortical bone thickness for predicting the ISQ value.
- (3)
- In the lower jaw, cortical bone thickness and implant diameter were confirmed to be significantly correlated with ISQ. Multiple regression analysis, using the ISQ value as the objective variable, also showed that both had a significant association with ISQ. Again, the cortical bone thickness was indicated to have a significant effect as a factor for predicting the ISQ value.
Author Contributions
Funding
Conflicts of Interest
References
- Iplikcioglu, H.; Akca, K.; Cehreli, M.C. The use of computerized tomography for diagnosis and treatment planning in implant dentistry. J. Oral Implantol. 2002, 28, 29–36. [Google Scholar] [CrossRef]
- Japanese Society for Oral and Maxillofacial Radiology. Guidelines for the Diagnostic Imaging in Dental Implant Treatment, 2nd ed.; Niigata University Graduate School of Medical and Dental Studies: Niigata City, Japan, 2008; Volume 2, pp. 1–30. [Google Scholar]
- Abrahams, J.J. Anatomy of the jaw revisited with a dental CT software program. Am. J. Neuroradiol. 1993, 14, 979–990. [Google Scholar] [PubMed]
- Fagelman, D.; Huang, A.B. Prospective evaluation of lesions of the mandible and maxilla: Indings on multiplanar and three-dimensional CT. Am. J. Roentgenol. 1994, 163, 693–698. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Widmann, G.; Bale, R.J. Accuracy in computer-aided implant surgery: A review. Int. J. Oral Maxillofac. Implants 2006, 21, 305–313. [Google Scholar] [PubMed]
- Yosue, T.; Takamori, H.; Nomura, A.; Watanabe, Y.; Kamezawa, H.; Otani, K.; Hiraga, Y.; Nakaya, H. Utility of CT in Brånemark implant treatment. Odontology 1992, 80, 915–922. [Google Scholar]
- Iwata, H.; Yosue, T. The correlation between the CT value and the bone quality in the jaw bone of implant patients. Odontol. Spring Spec. Issue 2007, 94, 138–143. [Google Scholar]
- Rasmusson, L.; Meredith, N.; Kahnberg, K.E.; Sennerby, L. Stability assessments and histology of titanium implants placed simultaneously with autogenous onlay bone in the rabbit tibia. Int. J. Oral Maxillofac. Surg. 1998, 27, 229–235. [Google Scholar] [CrossRef]
- Olive, L.; Aparocio, C. The Periotest method as a measure of osseointegrated oral implant stability. J. Oral Maxillofac. Implants 1990, 5, 390–400. [Google Scholar]
- Scarano, A.; Carinci, F.; Quaranta, A.; Iezzi, G.; Piattelli, M.; Piattelli, A. Correlation Between Implant Stability Quotient (ISQ) With Clinical and Histological Aspects of Dental Implants Removed for Mobility. Int. J. Immunopathol. Pharmacol. 2007, 20, 33–36. [Google Scholar] [CrossRef]
- Scarano, A. Traditional Postextractive Implant Site Preparation Compared With Pre-extractive Interradicular Implant Bed Preparation in the Mandibular Molar Region, Using an Ultrasonic Device: A Randomized Pilot Study. Int. J. Oral Maxillofac. Implants 2017, 32, 655–660. [Google Scholar] [CrossRef]
- Rektosson, T.; Zarb, G.A.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants. Int. J. Oral Maxillofac. Implants 1986, 1, 11–25. [Google Scholar]
- Zarb, G.A.; Albrektsson, T. Symposium: Towards Optimized Treatment Outcomes for Dental Implants. Toronto, Ontario, April 24-25, 1998. Proceedings. Int. J. Prosthodont. 1998, 11, 385–521. [Google Scholar]
- Arakawa, H. Clinical epidemiology associated with dental implant survival in Japanese: Identification of risk factors for loss of retention and failure of acquiring Osseointegration. J. Okayama Dent. Soc. 2004, 23, 29–45. [Google Scholar]
- Bischof, M.; Nedir, R.; Szmukler-Moncler, S.; Bernard, J.P.; Samson, J. Implant stability measurement of delayed and immediately loaded implants during healing. Clin. Oral Implants Res. 2004, 15, 529–539. [Google Scholar] [CrossRef]
- Nedir, R.; Bischof, M.; Szmukler-Moncler, S.; Bernard, J.P.; Samson, J. Predicting osseointegration by means of implant primary stability. Clin. Oral Implants Res. 2004, 15, 520–528. [Google Scholar] [CrossRef]
- Winter, W.; Möhrle, S.; Holst, S.; Karl, M. Parameters of implant stability measurements based on resonance frequency and damping capacity: A comparative finite element analysis. Int. J. Oral Maxillofac. Implants 2010, 25, 532–539. [Google Scholar]
- Friberg, B.; Sennerby, L.; Linden, B.; Gröndahl, K.; Lekholm, U. Stability measurements of one-stage Brånemark implants during healing in mandibles. A clinical resonance frequency analysis study. Int. J. Oral Maxillofac. Surg. 1999, 28, 266–272. [Google Scholar] [CrossRef]
- Miyamoto, I.; Tsuboi, Y.; Wada, E.; Suwa, H.; Iizuka, T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery clinical, prospective, biomechanical, and imaging study. Bone 2005, 37, 776–780. [Google Scholar] [CrossRef]
- Kumasaka, A.; Okamoto, T.; Kataoka, T.; Kaibuchi, N.; Fujii, T. Relationship between assessment of bone with computed tomography and movement evaluation. J. Jpn. Soc. Oral Implant 2012, 25, 708–716. [Google Scholar]
- Fukutome, J.; Iwata, H.; Takamori, H.; Tosue, T. The correlation between the bone mineral density of cancellous bone and the bone quality in the jaw bone of implant patients. J. Jpn. Soc. Oral Implant 2008, 21, 13–20. [Google Scholar]
- Coppieters, M.; Stappaerts, K.; Janssens, K.; Jull, G. Reliability of detecting ‘onset of pain’ and ‘submaximal pain’ during neural provocation testing of the upper quadrant. Physiother. Res. Int. 2002, 7, 146–156. [Google Scholar] [CrossRef] [PubMed]
- Takechi, M.; Ohta, K.; Minami, M.; Shigeishi, H.; Kamata, N. Effect of cortical bone on dental implant stability quotient values. J. Jpn. Soc. Oral Implant 2008, 21, 319–326. [Google Scholar]
- Naitoh, M. Diagnostic imaging for dental implant treatment. Jpn. J. Oral Maxillofac. Surg. 2009, 55, 2–7. [Google Scholar] [CrossRef][Green Version]
- Stoppie, N.; Pattijin, V.; Cleynenbreugel, T.V.; Wevers, M.; Sloten, J.V.; Ignace, N. Structual and radiological parameters for the characterization of jawbone. Clin. Oral Implants Res. 2006, 17, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Shapurian, T.; Damoulis, P.D.; Reiser, G.M.; Griffin, T.J.; Rand, W.M. Quantitative evaluation of bone density using the Hounsfield index. Int. J. Oral Maxillofac. Implants 2006, 21, 290–297. [Google Scholar] [PubMed]
- Morita, Y.; Kanda, S. Understanding the properties of the jaw bone through computed tomography value. Quintessence 2010, 29, 168–174. [Google Scholar]
- Hoshino, M.; Kuroda, T.; Takamori, H.; Youe, T. The correlation of bone density between whole body and jaw in impant patients. J. Jpn. Soc. Oral Implant 2005, 18, 273–279. [Google Scholar]
- Turkyilmaz, I.; Tozum, T.F.; Tumer, C.; Ozbek, E.N. Assessment of correlation between computerized tomography values of the bone, and maximum torque and resonance frequency values at dental implant placement. J. Oral Rehabil. 2006, 33, 881–888. [Google Scholar] [CrossRef]
- Arai, K.; Iwata, M.; Saratani, K.; Tanaka, M.; Kawazoe, T. Influence of stiffness of the circumference of implant on the result of a wireless resonance frequency analyzer. J. Jpn. Soc. Oral Implant 2007, 20, 433–438. [Google Scholar]
- Arai, K.; Terauchi, R.; Umezaki, Y.; Kaida, K.; Kashiwagi, T.; Kashiwagi, K.; Baba, S.; Tanaka, M.; Kawazoe, T. Effect of dental implant size on intraosseous stability. J. Osaka Dent. Univ. 2014, 48, 79–85. [Google Scholar]
- Shiigai, T. Bone conditions and early, immediate loading implants. Pract. Prosthodont. 2005, 38, 146–157. [Google Scholar]
- Sennerby, L.; Meredith, N. Implant stability measurements using resonance frequency analysis: Biological and biomechanical aspects and clinical implications. Periodontology 2000 2008, 47, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Hong-Gi, Y.; Seong-Joo, H.; Jai-Young, K.; Seong-Kyun, K.; Su-Young, L. Effect of bone quality and implant surgical technique on implant stability quotient (ISQ) value. J. Adv. Prosthodont. 2011, 3, 10–15. [Google Scholar]
- Javed, F.; Almas, K.; Crespi, R.; Romanos, G.E. Implant surface morphology and primary stability: Is there a connection? Implant Dent. 2011, 20, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Elias, C.N.; Rocha, F.A.; Nascimento, A.L.; Coelho, P.G. Influence of implant shape, surface morphology, surgical technique and bone quality on the primary stability of dental implants. J. Mech. Behav. Biomed. Mater. 2012, 16, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Oue, H.; Doi, K.; Oki, Y.; Makihara, Y.; Kubo, T.; Perrotti, V.; Piattelli, A.; Akagawa, Y.; Tsuga, K. Influence of implant surface topography on primary stability in a standardized osteoporosis rabbit model study. J. Funct. Biomater. 2015, 6, 143–152. [Google Scholar] [CrossRef] [PubMed]




| Male | Female | Total | ||
| Cases of Implant Treatment | 36 | 62 | 98 | |
| Number of Implants | 92 | 155 | 247 | |
| Maxilla | Mandible | Total | ||
| Number of Implants | 154 | 93 | 247 | |
| Implant Length | Implant Diameter | Total | ||
| Narrow (3.5 mm) | Regular (4.3 mm) | Wide (5.0 mm) | ||
| 8 mm | 5 | 17 | 4 | 26 |
| 10 mm | 22 | 48 | 28 | 98 |
| 13 mm | 32 | 65 | 15 | 112 |
| 16 mm | 7 | 4 | 0 | 11 |
| Total | 66 | 134 | 47 | 247 |
| Explanatory Variable | Unstandardized Coefficient | Standardization | p Value | 95% Cofidence Interval | |
|---|---|---|---|---|---|
| B | Standard Error | β | |||
| Constant | 35.748 | 2.544 | |||
| Cortical bone thickness (mm) | 32.892 | 2.404 | 0.695 | 0.000 | 28.151–37.634 |
| Cancellous bone CT value (HU) | 0.005 | 0.002 | 0.132 | 0.010 | 0.001–0.009 |
| Explanatory Variable | Unstandardized Coefficient | Standardization | p Value | 95% Cofidence Interval | |
|---|---|---|---|---|---|
| B | Standard Error | β | |||
| Constant | 30.851 | 3.694 | |||
| Cortical bone thickness (mm) | 36.736 | 3.848 | 0.650 | <0.001 | 29.114–44.358 |
| Cancellous bone CT value (HU) | 0.007 | 0.003 | 0.159 | 0.021 | 0.001–0.013 |
| Explanatory Variable | Unstandardized Coefficient | Standardization | p Value | 95% Cofidence Interval | |
|---|---|---|---|---|---|
| B | Standard Error | β | |||
| Constant | 39.808 | 4.928 | |||
| Cortical bone thickness (mm) | 19.868 | 3.300 | 0.555 | <0.001 | 13.293–26.442 |
| Cancellous bone CT value (HU) | 3.138 | 1.157 | 0.250 | 0.008 | 0.834–5.442 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takechi, M.; Ishioka, Y.; Ninomiya, Y.; Ono, S.; Tada, M.; Nakagawa, T.; Sasaki, K.; Murodumi, H.; Shigeishi, H.; Ohta, K. Morphological Evaluation of Bone by CT to Determine Primary Stability—Clinical Study. Materials 2020, 13, 2605. https://doi.org/10.3390/ma13112605
Takechi M, Ishioka Y, Ninomiya Y, Ono S, Tada M, Nakagawa T, Sasaki K, Murodumi H, Shigeishi H, Ohta K. Morphological Evaluation of Bone by CT to Determine Primary Stability—Clinical Study. Materials. 2020; 13(11):2605. https://doi.org/10.3390/ma13112605
Chicago/Turabian StyleTakechi, Masaaki, Yasuki Ishioka, Yoshiaki Ninomiya, Shigehiro Ono, Misato Tada, Takayuki Nakagawa, Kazuki Sasaki, Hiroshi Murodumi, Hideo Shigeishi, and Kouji Ohta. 2020. "Morphological Evaluation of Bone by CT to Determine Primary Stability—Clinical Study" Materials 13, no. 11: 2605. https://doi.org/10.3390/ma13112605
APA StyleTakechi, M., Ishioka, Y., Ninomiya, Y., Ono, S., Tada, M., Nakagawa, T., Sasaki, K., Murodumi, H., Shigeishi, H., & Ohta, K. (2020). Morphological Evaluation of Bone by CT to Determine Primary Stability—Clinical Study. Materials, 13(11), 2605. https://doi.org/10.3390/ma13112605





