Fluid Cartilage as New Autologous Biomaterial in the Treatment of Minor Nose Defects: Clinical and Microscopic Difference Amongst Diced, Crushed, and Fluid Cartilage
Abstract
:1. Introduction
2. Materials and Methods
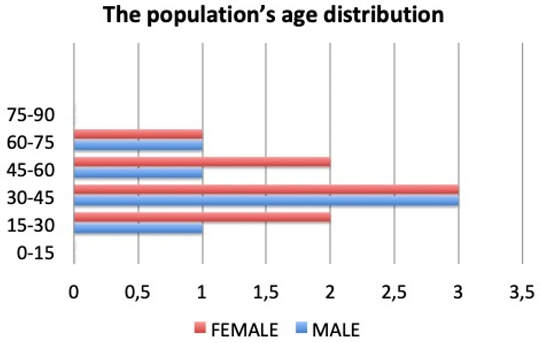
2.1. Patient Population
- Detailed therapeutic history (the outcomes of rhinoplasty or outcomes of trauma);
- Clinical examination (alar nose defects, dorsum, radix, and supra tip with minor contour deformity, nasal valve collapse);
- Blood test and urinalysis;
- CT scans
2.2. Fluid Cartilage Procedure
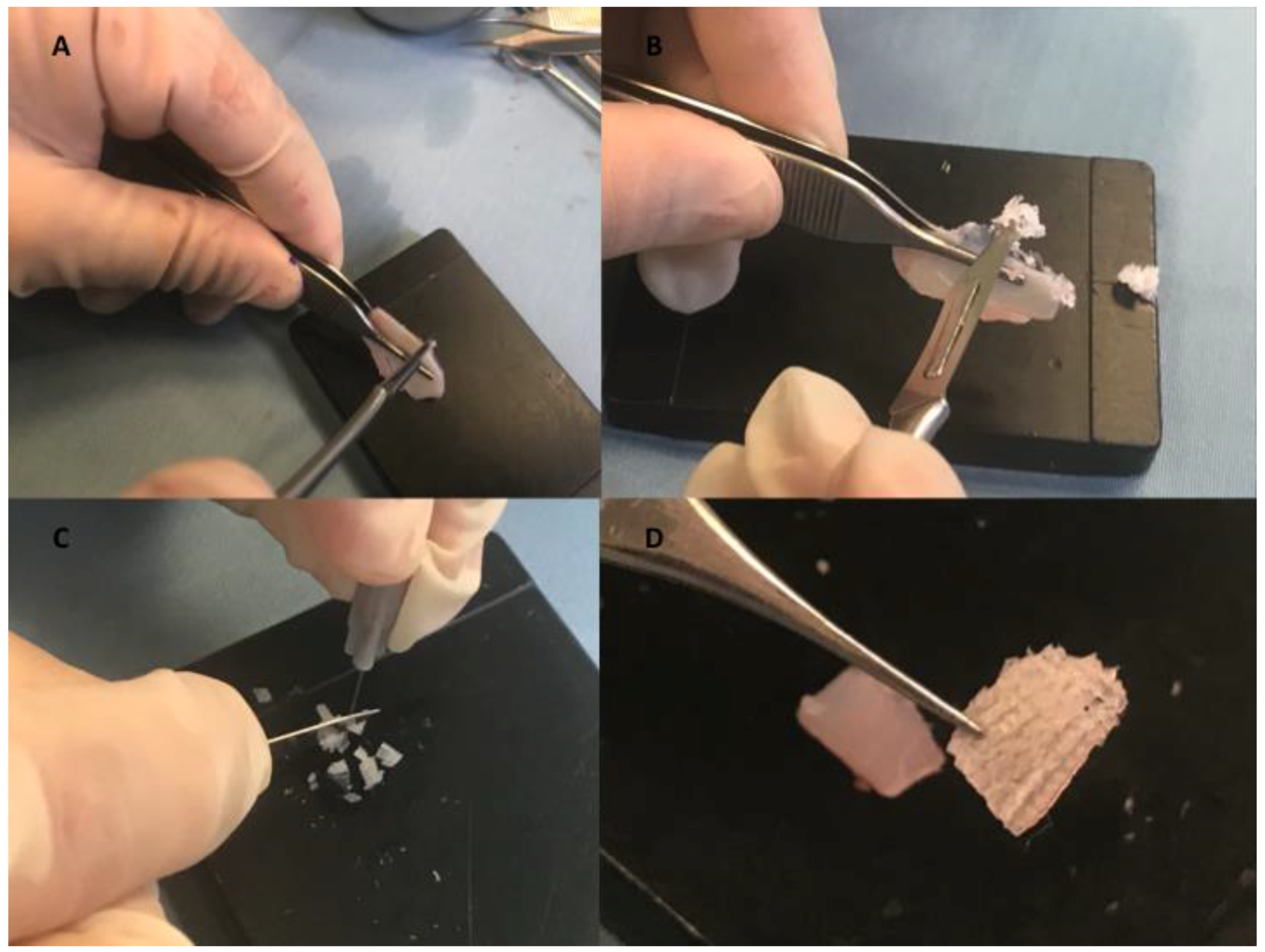
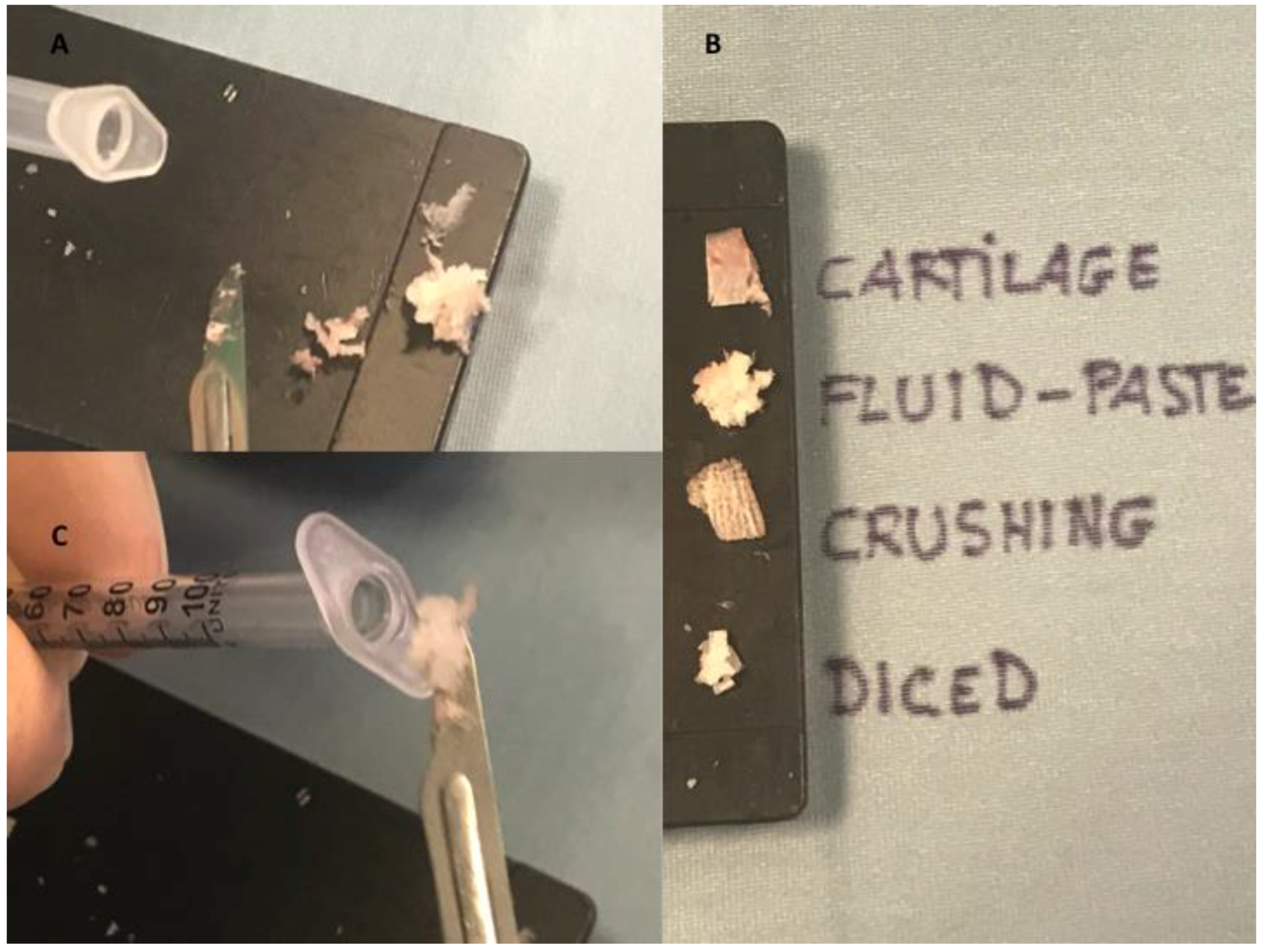
2.2.1. Fluid Cartilage Preparation
2.2.2. Indications and Injection of Fluid Cartilage as Filler
2.2.3. Clinical Observation
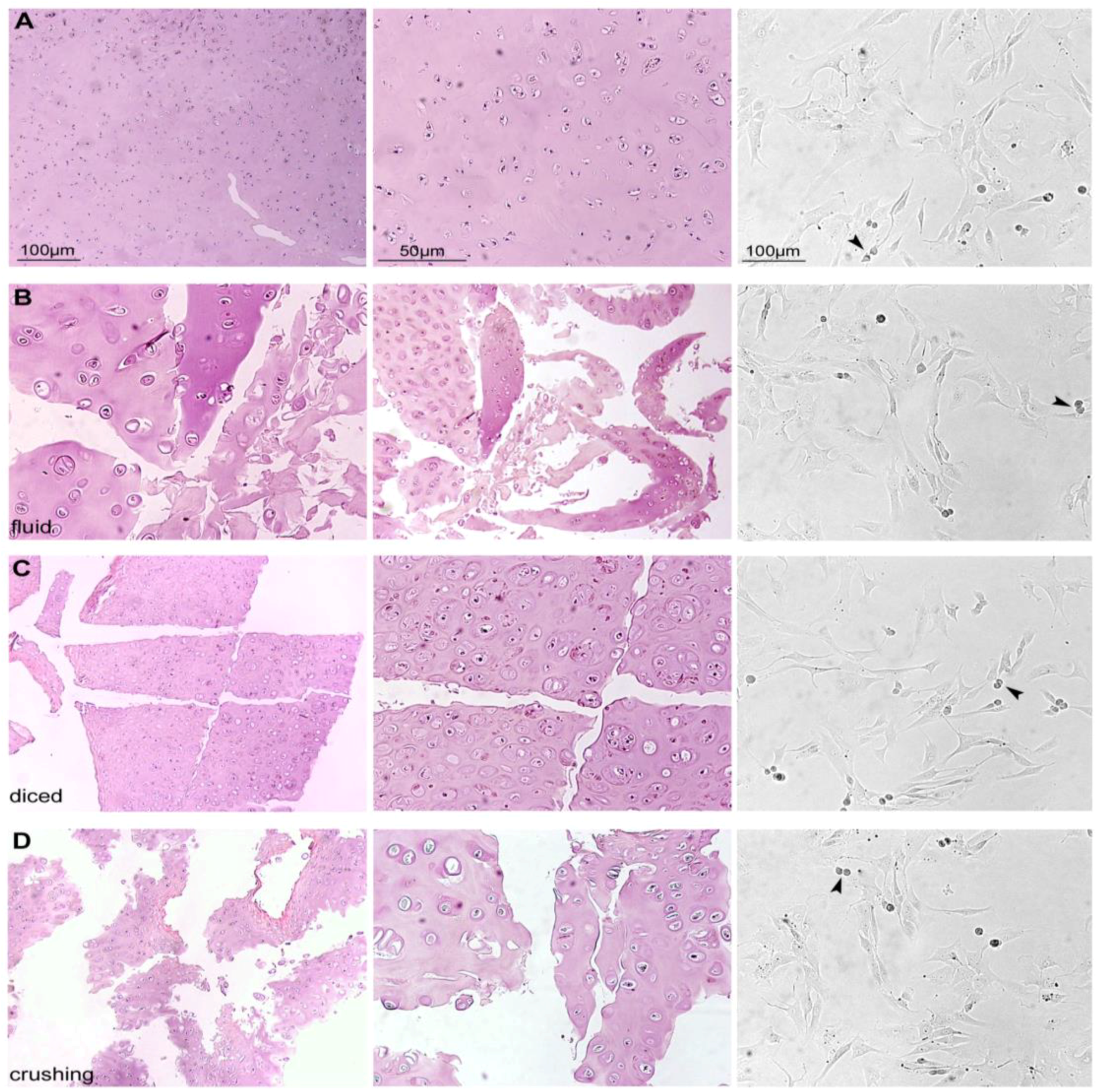
2.2.4. Histological Evaluation
2.2.5. Chondrocyte Isolation and Culture
2.2.6. Cytospin and Alcian–PAS Staining
2.2.7. RT-PCR Analysis
2.2.8. Statistical Analysis
3. Results
3.1. Histological, Morphological, and Phenotypic Analysis
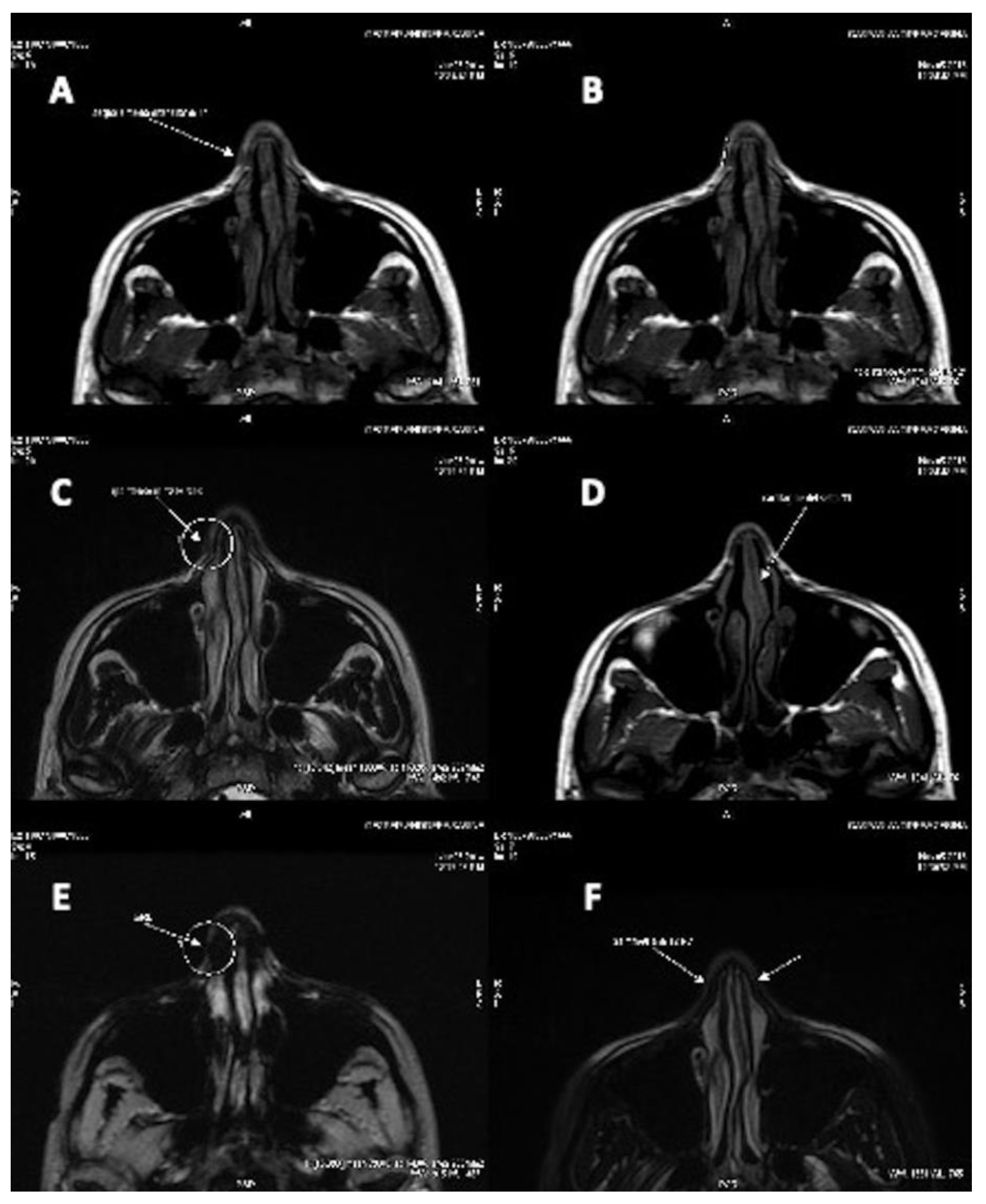
3.2. Clinical Long-Term Results and Instrumental Observation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics Approval and Consent to Participate
Abbreviations
| PRP | Platelet-Rich-Plasma |
| EC | European Parliament |
| CAT | Committe for Advanced treatments |
| GMP | Good Manufacturing Practices |
| GCP | Good Clinical Practices |
| SPSS | Statistical Package for the Social Sciences |
| CD | Cluster of differentiation |
| NaCl | Saline solution |
| MW | Molecular weight |
| PCR- | Negative control |
| HCs | Human Condrocytes |
| SD | Standard Deviation |
References
- Daniel, R.K.; Calvert, J.W. Diced cartilage grafts in rhinoplasty surgery. Plast. Reconstr. Surg. 2004, 113, 2156–2171. [Google Scholar] [CrossRef] [PubMed]
- Kreutzer, C.; Hoehne, J.; Gubisch, W.; Rezaeian, F.; Haack, S. Free diced cartilage: A new application of diced cartilage grafts in primary and secondary rhinoplasty. Plast. Reconstr. Surg. 2017, 140, 461–470. [Google Scholar] [CrossRef]
- Manafi, A.; Hamedi, Z.S.; Rajabiani, A.; Rajaee, A.; Manafi, F. Injectable cartilage shaving: An autologous and long lasting filler material for correction of minor contour deformities in rhinoplasty. World J. Plast. Surg. 2015, 4, 93–100. [Google Scholar]
- Sinanan, A.C.; Hunt, N.P.; Lewis, M.P. Human adult craniofacial muscle-derived cells: Neural-cell adhesion-molecule (NCAM; CD56)-expressing cells appear to contain multipotential stem cells. Biotechnol. Appl. Biochem. 2004, 40, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Papaccio, G.; Graziano, A.; d’Aquino, R.; Graziano, M.F.; Pirozzi, G.; Menditti, D.; De Rosa, A.; Carinci, F.; Laino, G. Long-term cryopreservation of dental pulp stem cells (SBP-DPSCs) and their differentiated osteoblasts: A cell source for tissue repair. J. Cell Physiol. 2006, 208, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Bianco, P.; Robey, P.G. Stem cells in tissue engineering. Nature 2001, 414, 118–121. [Google Scholar] [CrossRef]
- Calvi, L.M.; Adams, G.B.; Weibrecht, K.W.; Weber, J.M.; Olson, D.P.; Knight, M.C.; Martin, R.P.; Schipani, E.; Divieti, P.; Bringhurst, F.R.; et al. Osteoblastic cells regulate the haematopoietic stem cell niche. Nature 2003, 425, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Niu, C.; Ye, L.; Huang, H.; He, X.; Tong, W.G.; Ross, J.; Haug, J.; Johnson, T.; Feng, J.Q.; et al. Identification of the haematopoietic stem cell niche and control of the niche size. Nature 2003, 425, 836–841. [Google Scholar] [CrossRef] [PubMed]
- Ba, R.; Wei, J.; Li, M.; Cheng, X.; Zhao, Y.; Wu, W. Cell-bricks based injectable niche guided persistent ectopic chondrogenesis of bone marrow-derived mesenchymal stem cells and enabled nasal augmentation. Stem Cell Res. Ther. 2015, 6, 16. [Google Scholar] [CrossRef]
- Zhu, J.; Cai, B.; Ma, Q.; Chen, F.; Wu, W. Cell bricks-enriched platelet-rich plasma gel for injectable cartilage engineering—An in vivo experiment in nude mice. J. Tissue Eng. Regen. Med. 2013, 7, 819–830. [Google Scholar] [CrossRef]
- Noordzij, J.P.; Cates, J.M.; Cohen, S.M.; Bennett, M.L.; Ries, W.M.; Russell, P.T.; Haynes, D.; Garrett, C.G.; Ossoff, R.H. Preparation techniques for the injection of human autologous cartilage: An ex vivo feasibility study. Laryngoscope 2008, 118, 185–188. [Google Scholar] [CrossRef]
- Gentile, P.; Scioli, M.G.; Bielli, A.; Orlandi, A.; Cervelli, V. Reconstruction of alar nasal cartilage defects using a tissue engineering technique based on a combined use of autologous chondrocyte micrografts and platelet-rich plasma: Preliminary clinical and instrumental evaluation. Plast. Reconstr. Surg. Glob. Open 2016, 4, e1027. [Google Scholar] [CrossRef] [PubMed]
- Schuklenk, U.; Ashcroft, R. International research ethics. Bioethics 2000, 14, 158–172. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gtzsche, P.C.; Van-denbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Scioli, M.G.; Artuso, S.; D’Angelo, C.; Porru, M.; D’Amico, F.; Bielli, A.; Gentile, P.; Cervelli, V.; Leonetti, C.; Orlandi, A. Adipose-derived stem cell-mediated paclitaxel delivery inhibits breast cancer growth. PLoS ONE 2018, 13, e0203426. [Google Scholar] [CrossRef] [PubMed]
- Tarquini, C.; Mattera, R.; Mastrangeli, F.; Agostinelli, S.; Ferlosio, A.; Bei, R.; Orlandi, A.; Tarantino, U. Comparison of tissue transglutaminase 2 and bone biological markers osteocalcin, osteopontin and sclerostin expression in human osteoporosis and osteoarthritis. Amino Acids 2017, 49, 683–693. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.G.; Witsell, D.L.; Smith, T.L.; Weaver, E.M.; Yueh, B.; Hannley, M.T. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol. Head Neck Surg. 2004, 130, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Bottini, D.J.; Gentile, P.; Arpino, A.; Dasero, G.; Cervelli, V. Reconstruction of the nasal valve. J. Craniofac. Surg. 2007, 18, 516–519. [Google Scholar] [CrossRef]
- Hausamen, J.E. The scientific development of maxillofacial surgery in the 20th century and an outlook into the future. J. Craniomaxillofac. Surg. 2001, 29, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Kinnaird, T.; Stabile, E.; Burnett, M.S.; Lee, C.W.; Barr, S.; Fuchs, S.; Epstein, S.E. Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circ. Res. 2004, 94, 678–685. [Google Scholar] [CrossRef]
- Sun, X.; Altalhi, W.; Nunes, S.S. Vascularization strategies of engineered tissues and their application in cardiac regeneration. Adv. Drug Deliv. Rev. 2016, 96, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.N.; Byun, D.S.; Park, J.H.; Han, S.W.; Baik, J.S.; Kim, J.Y. Panophthalmoplegia and vision loss after cosmetic nasal dorsum injection. J. Clin. Neurosci. 2014, 21, 678–680. [Google Scholar] [CrossRef] [PubMed]
- Tammi, M.I.; Day, A.J.; Turley, E.A. Hyaluronan and homeostasis: A balancing act. J. Biol. Chem. 2002, 277, 4581–4584. [Google Scholar] [CrossRef] [PubMed]
- Duranti, F.; Salti, G.; Bovani, B.; Calandra, M.; Rosati, M.L. Injectable hyaluronic acid gel for soft tissue augmentation. A clinical and histological study. Dermatol. Surg. 1998, 24, 1317–1325. [Google Scholar] [CrossRef]
- De Boulle, K. Management of complications after implantation of fillers. J. Cosmet. Dermatol. 2004, 3, 2–15. [Google Scholar] [CrossRef]
- Cakmak, O.; Altintas, H. A classification for degree of crushed cartilage. Arch. Facial Plast. Surg. 2010, 12, 435–436. [Google Scholar] [CrossRef]
- Cakmak, O.; Bircan, S.; Buyuklu, F.; Tuncer, I.; Dal, T.; Ozluoglu, L.N. Viability of crushed and diced cartilage grafts: A study in rabbits. Arch. Facial Plast. Surg. 2005, 7, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Peer, L.A. Extended use of diced cartilage grafts. Plast. Reconstr. Surg. 1954, 14, 178–185. [Google Scholar] [CrossRef]
- Singh, S.K.; Sood, T.; Sabarigirish, K.; Ramakrishnan, N.; Rajguru, R.; Manoj Kumar, K. A New Era of diced cartilage rhinoplasty: Our experience. Indian J. Otolaryngol. Head Neck Surg. 2015, 67, 338–340. [Google Scholar] [CrossRef]
- Erol, O.O. The Turkish delight: A pliable graft for rhinoplasty. Plast. Reconstr. Surg. 2000, 105, 2229–2241, discussion 2242–2243. [Google Scholar] [CrossRef]
- Calvert, J.W.; Brenner, K.; DaCosta-Iyer, M.; Evans, G.R.; Daniel, R.K. Histological analysis of human diced cartilage grafts. Plast. Reconstr. Surg. 2006, 118, 230–236. [Google Scholar] [CrossRef]
- Lin, S.I.; Hsiao, Y.C.; Chang, C.S.; Chen, P.K.; Chen, J.P.; Ueng, S.H. Histology and long-term stability of diced cartilage graft for revision rhinoplasty in a cleft patient. Plast. Reconstr. Surg. Glob. Open 2016, 4, e763. [Google Scholar] [CrossRef] [PubMed]
- Kayabasoglu, G.; Ozbek, E.; Yanar, S.; Sahin, F.; Keles, O.N.; Yilmaz, M.S.; Guven, M. The comparison of the viability of crushed, morselized and diced cartilage grafts: A confocal microscopic study. Eur. Arch. Otorhinolaryngol. 2015, 272, 1135–1142. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, S.; Erçöçen, A.R.; Can, Z.; Yenidünya, S.; Edali, N.; Yormuk, E. Viability of diced, crushed cartilage grafts and the effects of Surgicel (oxidized regenerated cellulose) on cartilage grafts. Plast. Reconstr. Surg. 2001, 108, 1054–1060, discussion 1061–1062. [Google Scholar] [CrossRef]
- Daniel, R.K. The role of diced cartilage grafts in rhinoplasty. Aesthet. Surg. J. 2006, 26, 209–213. [Google Scholar] [CrossRef]
- Trivisonno, A.; Di Rocco, G.; Cannistra, C.; Finocchi, V.; Farr, S.; Monti, M.; Toietta, G. Harvest of superficial layers of fat with a microcannula and isolation of adipose tissue-derived stromal and vascular cells. Aesthet. Surg. J. 2014, 34, 601–613. [Google Scholar] [CrossRef] [PubMed]



© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trivisonno, A.; Cohen, S.R.; Magalon, G.; Magalon, J.; Sterodimas, A.; Pascali, M.; Cervelli, V.; Toietta, G.; Colaprietra, A.; Calcagni, F.; et al. Fluid Cartilage as New Autologous Biomaterial in the Treatment of Minor Nose Defects: Clinical and Microscopic Difference Amongst Diced, Crushed, and Fluid Cartilage. Materials 2019, 12, 1062. https://doi.org/10.3390/ma12071062
Trivisonno A, Cohen SR, Magalon G, Magalon J, Sterodimas A, Pascali M, Cervelli V, Toietta G, Colaprietra A, Calcagni F, et al. Fluid Cartilage as New Autologous Biomaterial in the Treatment of Minor Nose Defects: Clinical and Microscopic Difference Amongst Diced, Crushed, and Fluid Cartilage. Materials. 2019; 12(7):1062. https://doi.org/10.3390/ma12071062
Chicago/Turabian StyleTrivisonno, Angelo, Steven R. Cohen, Guy Magalon, Jèrèmy Magalon, Aris Sterodimas, Michele Pascali, Valerio Cervelli, Gabriele Toietta, Alfredo Colaprietra, Filippo Calcagni, and et al. 2019. "Fluid Cartilage as New Autologous Biomaterial in the Treatment of Minor Nose Defects: Clinical and Microscopic Difference Amongst Diced, Crushed, and Fluid Cartilage" Materials 12, no. 7: 1062. https://doi.org/10.3390/ma12071062
APA StyleTrivisonno, A., Cohen, S. R., Magalon, G., Magalon, J., Sterodimas, A., Pascali, M., Cervelli, V., Toietta, G., Colaprietra, A., Calcagni, F., Orlandi, A., Scioli, M. G., & Gentile, P. (2019). Fluid Cartilage as New Autologous Biomaterial in the Treatment of Minor Nose Defects: Clinical and Microscopic Difference Amongst Diced, Crushed, and Fluid Cartilage. Materials, 12(7), 1062. https://doi.org/10.3390/ma12071062






