Measurement of Fracture Strength of Zirconia Dental Implant Abutments with Internal and External Connections Using Acoustic Emission
Abstract
:1. Introduction
2. Materials and Methods
2.1. Material Preparation
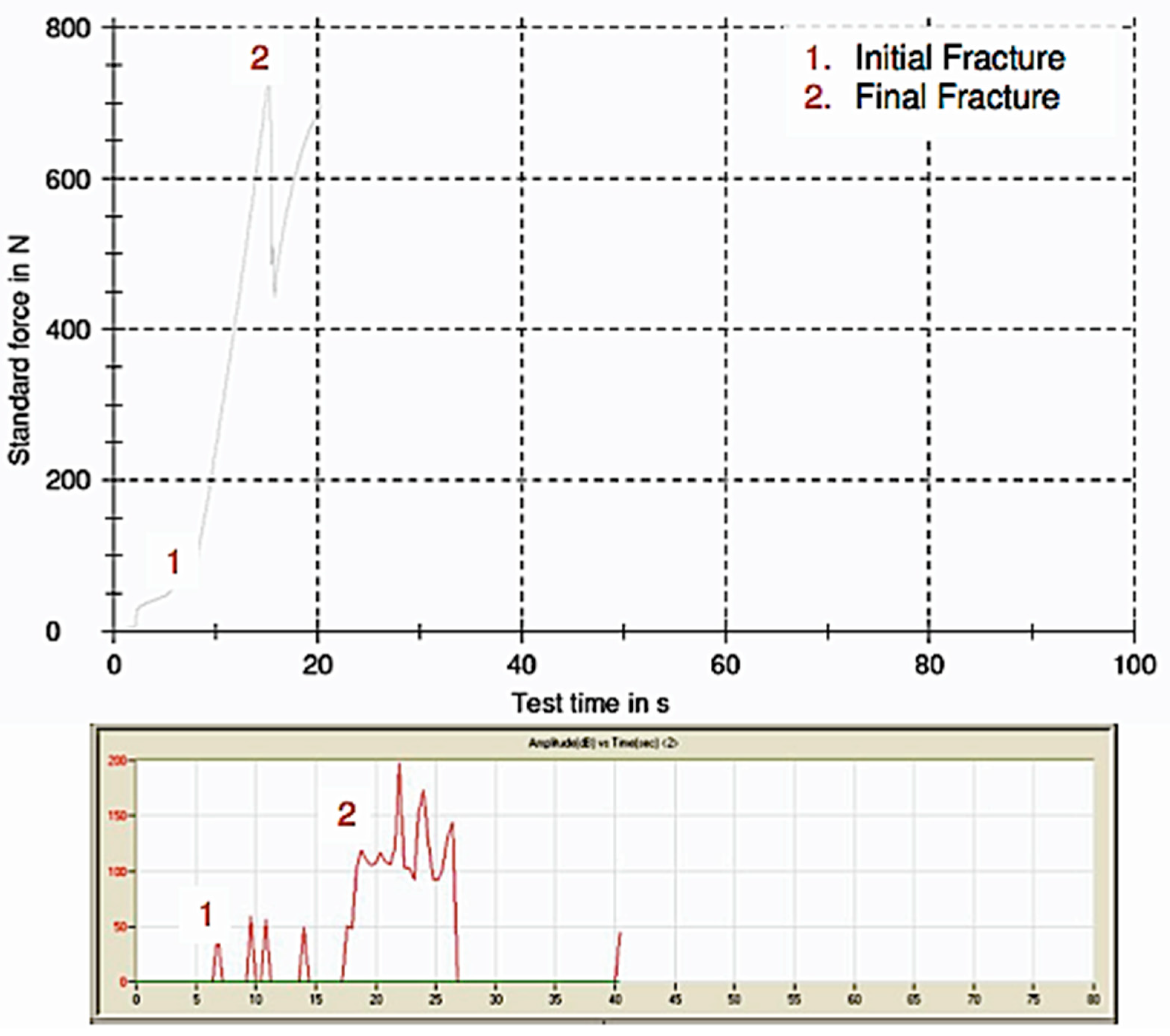
2.2. Universal Loading Machine
2.3. Acoustic Emission
2.4. Statistical Analysis
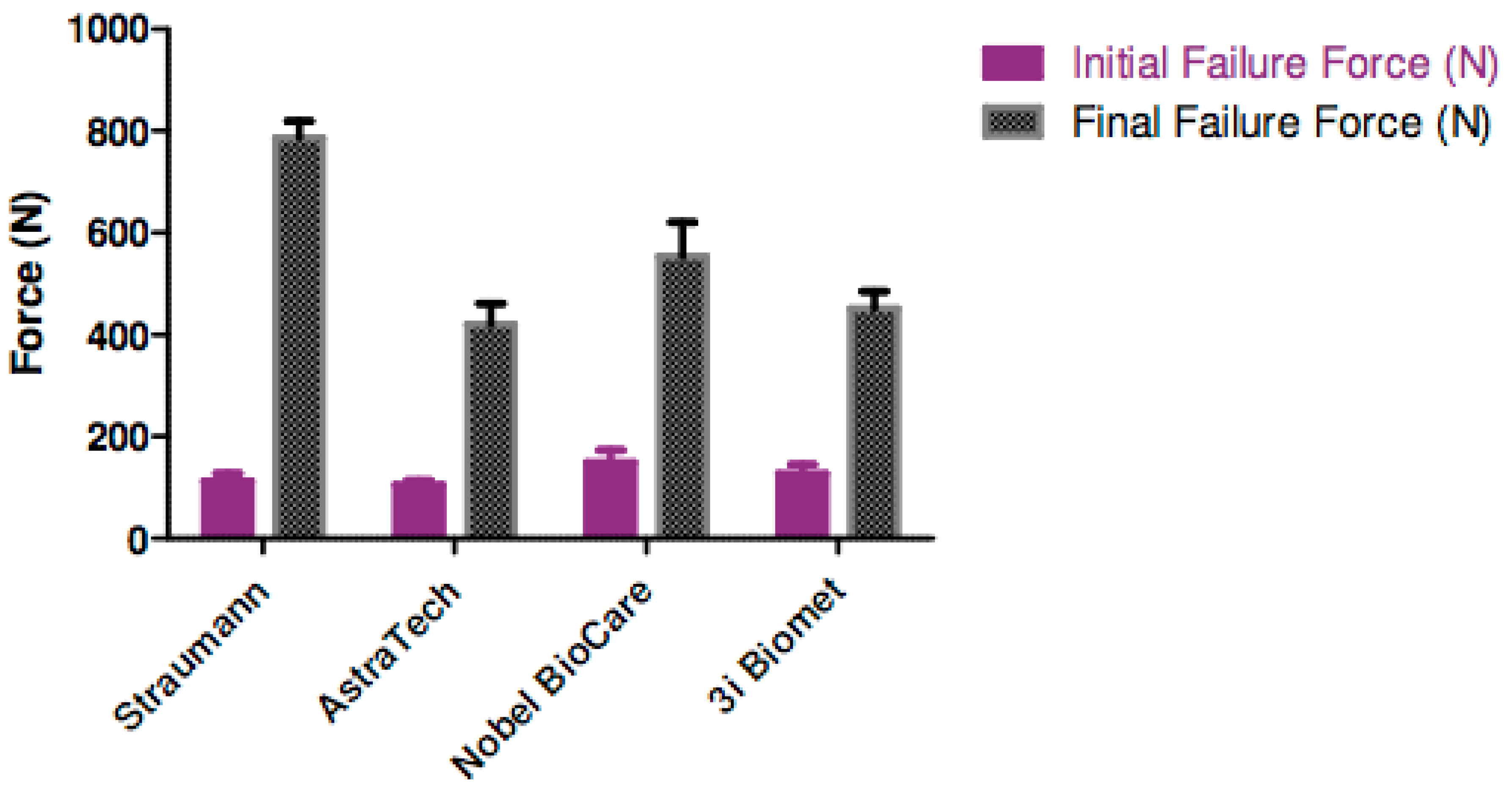
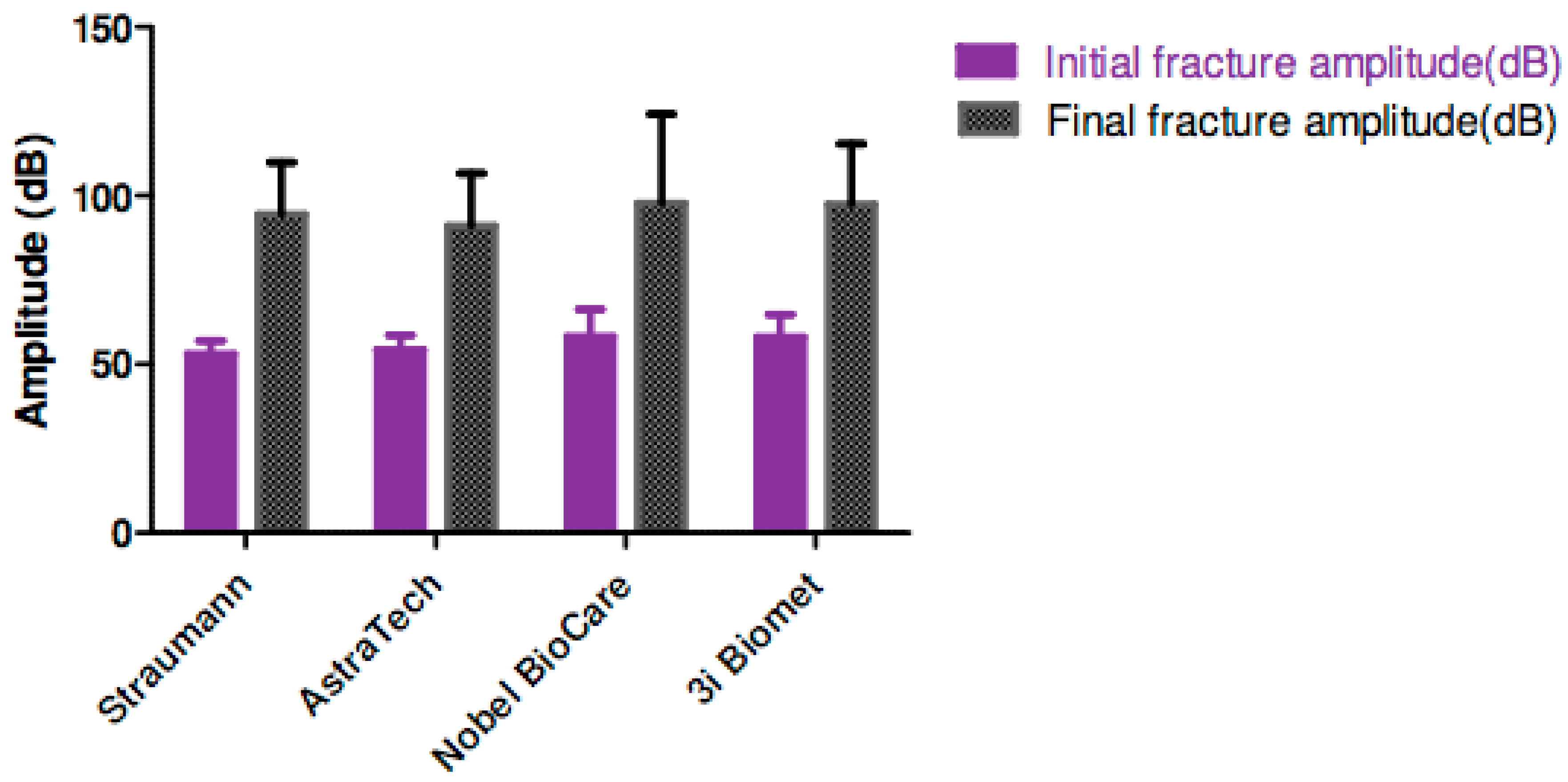
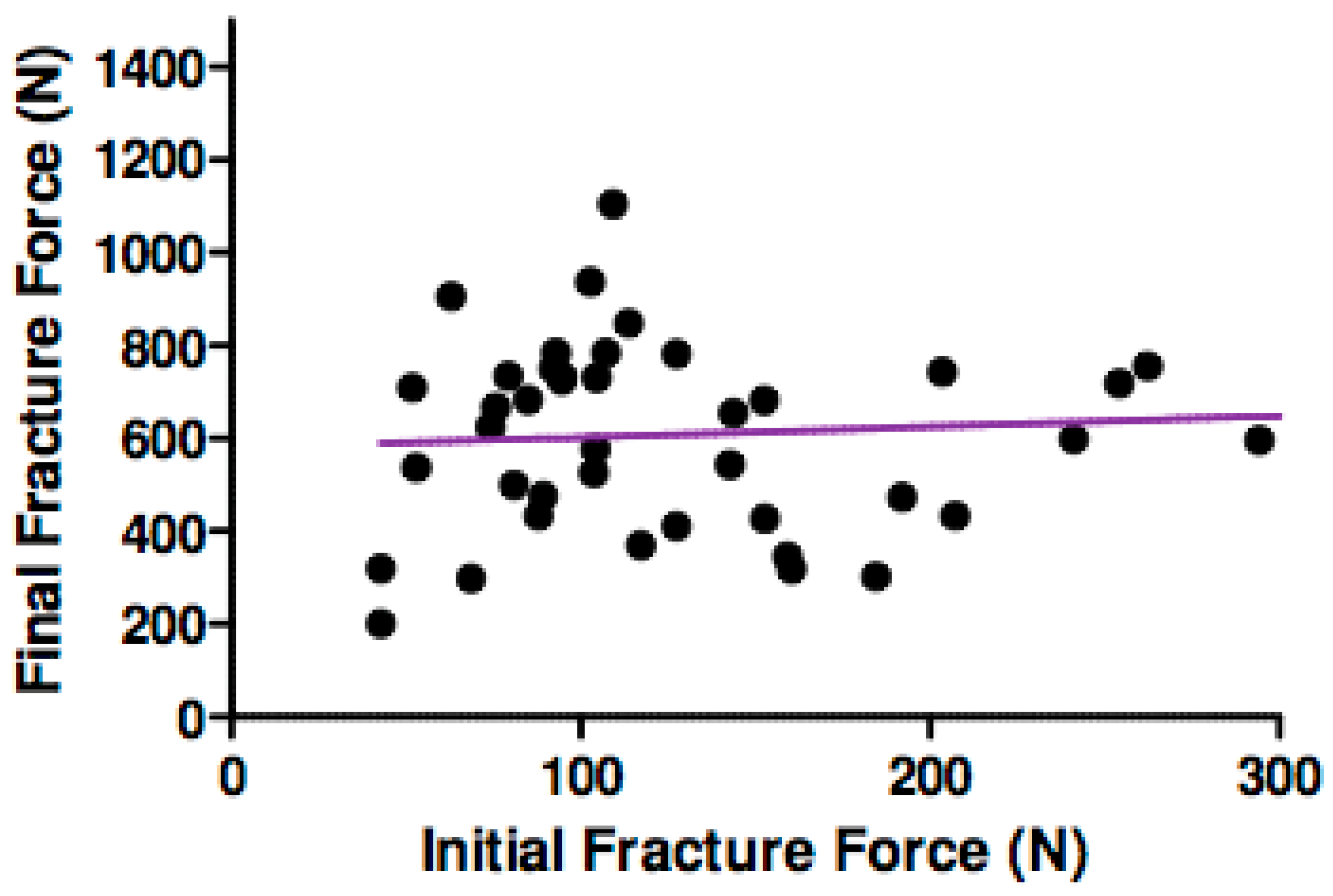
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef]
- Jivraj, S.; Chee, W. Rationale for dental implants. Br. Dent. J. 2006, 200, 661–665. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Holderegger, C.; Sailer, I.; Khraisat, A.; Suter, A.; Hämmerle, C.H.F. The effect of all-ceramic and porcelain-fused-to-metal restorations on marginal peri-implant soft tissue color: A randomized controlled clinical trial. Int. J. Periodontic. Restor. Dent. 2008, 28, 357–365. [Google Scholar]
- Sailer, I.; Zembic, A.; Jung, R.E.; Hämmerle, C.H.F.; Mattiola, A. Single-Tooth Implant Reconstructions: Esthetics Factors Influencing the Decision Between Titanium and Zirconia Abutments in Anterior Regions. Eur. J. Esthet. Dent. 2007, 2, 296–310. [Google Scholar] [PubMed]
- Truninger, T.C.; Stawarczyk, B.; Leutert, C.R.; Sailer, T.R.; Hämmerle, C.H.F.; Sailer, I. Bending moments of zirconia and titanium abutments with internal and external implant–abutment connections after aging and chewing simulation. Clin. Oral Implant. Res. 2012, 23, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Griggs, J.A. Dental implants. Dent. Clin. 2017, 61, 857–871. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, C.J.; Bernal, G.; Rungcharassaeng, K.; Kan, J.Y.K. Clinical complications with implants and implant prostheses. J. Prosthet. Dent. 2003, 90, 121–132. [Google Scholar] [CrossRef]
- Att, W.; Kurun, S.; Gerds, T.; Strub, J.R. Fracture resistance of single-tooth implant-supported all-ceramic restorations: An in vitro study. J. Prosthet. Dent. 2006, 95, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Sailer, T.; Stawarczyk, B.; Jung, R.E.; Hämmerle, C.H. In vitro study of the influence of the type of connection on the fracture load of zirconia abutments with internal and external implant-abutment connections. Int. J. Oral Maxillofac. Implant. 2009, 24, 850–858. [Google Scholar]
- Zarone, F.; Sorrentino, R.; Traini, T.; Caputi, S. Fracture resistance of implant-supported screw-versus cement-retained porcelain fused to metal single crowns: SEM fractographic analysis. Dent. Mater. 2007, 23, 296–301. [Google Scholar] [CrossRef]
- Merz, P.; Freisleben, B. Fitness landscape analysis and memetic algorithms for the quadratic assignment problem. IEEE Trans. Evolut. Comput. 2000, 4, 337–352. [Google Scholar]
- Li, T.; Hu, K.; Cheng, L.; Ding, Y.; Ding, Y.; Shao, J.; Kong, L. Optimum selection of the dental implant diameter and length in the posterior mandible with poor bone quality–A 3D finite element analysis. Appl. Math. Model. 2011, 35, 446–456. [Google Scholar] [CrossRef]
- Alander, P.; Lassila, L.V.J.; Tezvergil, A.; Vallittu, P.K. Acoustic emission analysis of fiber-reinforced composite in flexural testing. Dent. Mater. 2004, 20, 305–312. [Google Scholar] [CrossRef]
- Pollock, A.A. Acoustic emission inspection. Met. Handb. 1989, 17, 278–294. [Google Scholar]
- Hamstad, M.A. Testing fiber composites with acoustic emission monitoring. J. Acoust. Emiss. 1982, 1, 151–164. [Google Scholar]
- Piconi, C.; Maccauro, G. Zirconia as a ceramic biomaterial. Biomaterials 1999, 20, 1–25. [Google Scholar] [CrossRef]
- Andersson, B.; Ödman, P.; Boss, A.; Jörnéus, L. Mechanical Testing of Superstructures on the CeraOne Abutment in the Brånemark System. Int. J. Oral Maxillofac. Implant. 1994, 9, 665–672. [Google Scholar]
- Haraldson, T.; Carlsson, G.E. Bite force and oral function in patients with osseointegrated oral implants. Eur. J. Oral Sci. 1977, 85, 200–208. [Google Scholar] [CrossRef]
- Tripodakis, A.P.D.; Strub, J.R.; Kappert, H.F.; Witkowski, S. Strength and mode of failure of single implant all-ceramic abutment restorations under static load. Int. J. Prosthodont. 1995, 8, 265–272. [Google Scholar] [PubMed]
- Yildirim, M.; Fischer, H.; Marx, R.; Edelhoff, D. In vivo fracture resistance of implant-supported all-ceramic restorations. J. Prosthet. Dent. 2003, 90, 325–331. [Google Scholar] [CrossRef]
- Al Rafee, M.A.; Nagy, W.W.; Fournelle, R.A.; Dhuru, V.B.; Tzenakis, G.K.; Pechous, C.E. The effect of repeated torque on the ultimate tensile strength of slotted gold prosthetic screws. J. Prosthet. Dent. 2002, 88, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Satoh, T.; Sogo, M. In vitro differences of stress concentrations for internal and external hex implant–abutment connections: A short communication. J. Oral Rehabil. 2006, 33, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Merz, B.R.; Hunenbart, S.; Belser, U.C. Mechanics of the implant-abutment connection: An 8-degree taper compared to a butt joint connection. Int. J. Oral Maxillofac. Implant. 2000, 15. [Google Scholar]
- Mühlemann, S.; Truninger, T.C.; Stawarczyk, B.; Hämmerle, C.H.F.; Sailer, I. Bending moments of zirconia and titanium implant abutments supporting all-ceramic crowns after aging. Clin. Oral Implant. Res. 2014, 25, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Ereifej, N.; Silikas, N.; Watts, D.C. Initial versus final fracture of metal-free crowns, analyzed via acoustic emission. Dent. Mater. 2008, 24, 1289–1295. [Google Scholar] [CrossRef] [PubMed]

| Implant Manufacturer | Implant | Abutment | Connection Type |
|---|---|---|---|
| Astra Tech, Molndal, Sweden | 4.0 mm (D) × 11 mm (L) Osseospeed | ZirDesign™ Abutment 3.5/4.0 4.5, 3 mm | Internal |
| Straumann, Basel, Switzerland | 4.1 mm (D) RC × 10 mm (L) Bone Level SLA | Straumann RC Anatomical IPS e.max® Abutment Straight, GH 3.5 mm, MO 0 | Internal |
| Nobel Biocare, Goteberg, Sweden | 4.0 mm (D) × 10 mm (L) RP MK III Groovy Implant | Procera® Esthetic Abutment RP | External |
| Implant Innovations (Biomet 3i), Palm Beach, FL, USA | 4.0 mm (H) × 10 mm (L) Certain | ZiReal® Post 4.1 mm (D) × 4 mm (H) | External |
| Implant Assembly | Initial Fracture Force (N) | Final Fracture Force (N) | % of Initial to Final Force | Initial Fracture Amplitude (dB) | Final Fracture Amplitude (dB) |
|---|---|---|---|---|---|
| Astra Tech/ZirDesign™ Abutment (Internal connection) | 105.3 | 420.1 | 25.1 | 54.3 | 91.0 |
| Nobel Biocare/Procera® Esthetic (External connection) | 149.9 | 553.4 | 27.1 | 58.1 | 97.6 |
| Straumann/Straumann RC Anatomical IPS e.max® (Internal connection) | 113.0 | 785.9 | 14.4 | 53.0 | 94.4 |
| Implant Innovations (Biomet 3i)/ZiReal® Post (External connection) | 127.2 | 451.4 | 28.2 | 58.1 | 97.4 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soo, S.Y.; Silikas, N.; Satterthwaite, J. Measurement of Fracture Strength of Zirconia Dental Implant Abutments with Internal and External Connections Using Acoustic Emission. Materials 2019, 12, 2009. https://doi.org/10.3390/ma12122009
Soo SY, Silikas N, Satterthwaite J. Measurement of Fracture Strength of Zirconia Dental Implant Abutments with Internal and External Connections Using Acoustic Emission. Materials. 2019; 12(12):2009. https://doi.org/10.3390/ma12122009
Chicago/Turabian StyleSoo, Suet Yeo, Nikolaos Silikas, and Julian Satterthwaite. 2019. "Measurement of Fracture Strength of Zirconia Dental Implant Abutments with Internal and External Connections Using Acoustic Emission" Materials 12, no. 12: 2009. https://doi.org/10.3390/ma12122009





