1. Introduction
Human gait is an essential means of locomotion for daily life and the most important function necessary for quality of life [
1]. Walking dysfunctions can lead to falling, fracture, progression of disease, decreased mobility, and depression; all limiting the performances in daily activities. Early diagnosis of gait-related impairments is important in preventing symptom aggravation and irreversible deformities. Reliable yet practical diagnostic medical devices with high resolution sensors need to be continuously advanced.
Substantial evidence on cognitive neuroscience and motor control suggests that gait parameters can reveal important factors that determine the overall health and well-being [
2,
3]. However, present gait analysis systems and the results reported are based on costly equipment, bulky and complicated set-up, require multiple types of sensors, and are limited to indoors [
4,
5,
6]. Therefore, development of high-performance, wearable smart analytic systems with affordable prices, is in demand for real-time daily activity monitoring and analysis. With practical methodologies, neurological, musculoskeletal, kinematic, and sports-related problems associated with gait and foot pathologies, can be more efficiently addressed.
Meaningful gait parameters include gait speed, step-count, stride-time, center of pressure (CoP), and phase coordination index (PCI) [
7,
8,
9,
10,
11,
12]. Walking speed is the product of step-length and step-frequency (step-count/time) and is considered the sixth vital sign, because it has been validated as a marker of frailty and mortality [
13,
14]. Wearable smart insole that can monitor the changes in walking speed, during various types of activities, is expected to enhance the quality of gait-related research and therapy.
For walking improvements in the elderly or rehabilitation patients, mobility skill practice is essential; use of a smart insole feedback system could accelerate the procedure. Step-count in a controlled environment is known to be a reliable and valid indicator in quantifying the temporal frequency of gait [
14]. It is used to evaluate current motor control functions and set future goals in rehabilitation therapy. Stride-time and stride-length present one’s gait cycle, and the coordination patterns of limb segments can be used to identify the joint mechanics [
15]. Understanding the coordination patterns, in movement analysis, can be used to diagnose and prognose neuro-cognitive functions. Plantar pressure analyses are considered meaningful in examining the biomechanical characteristics of the foot, because related sports injuries to functional deformities can be diagnosed [
16].
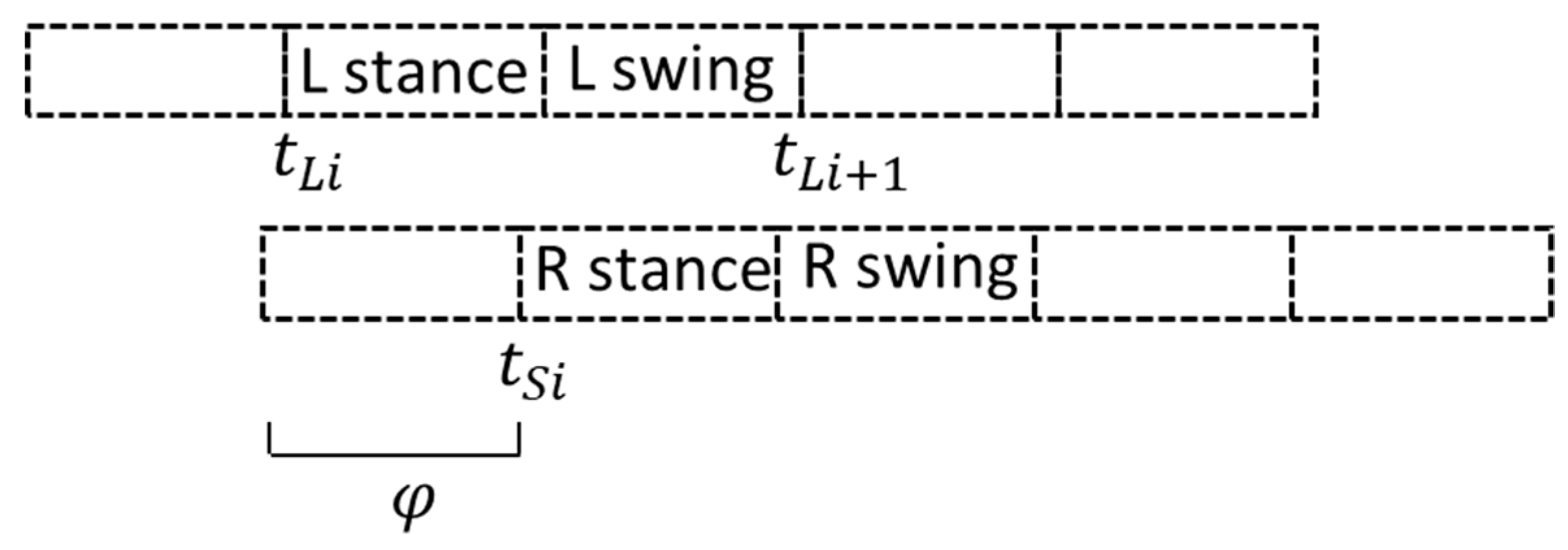
Among these parameters, PCI is reported to be a relatively more sensitive measure in analyzing the bilateral coordination or asymmetry of locomotion and balance, which are significant variables, especially in rehabilitative medicine [
17,
18,
19]. PCI is an indicator evaluating the coordination of left–right stepping phase, and the PCI value closer to 0% means that the two feet are moving in a higher coordination. Balance and coordination are fundamental motor control functions for normal gait. PCI analysis can also be extensively applied to diagnose the severity of scoliosis, hemiparesis, and aging. Despite the significance, most of the current insole sensors, used for gait analysis, are not designed to detect and analyze PCI. The need for development of a cost-effective wearable sensor that can measure PCI in real-life conditions, is prominent.
A number of scientists have developed wearable sensors for gait analysis, but most of them are equipped with multiple bulky measurement devices, including dual 3-axis accelerometer, gyroscope, torque, ground reaction force sensor, and pressure sensor, making the measuring procedure complicated and inconvenient [
20,
21,
22]. In recent studies by Wu et al. (2015) and Park et al. (2018), insole-type pressure sensor and a smart shoes system were developed for gait analysis and smart phone applications-enabled real-time monitoring of the activities have been carried out [
23,
24]. However, many of these research-based, newly developed wearable devices are rather expensive and the bio-signals collected and analyzed are not as accurate, compared to that of commercial sensors [
25].
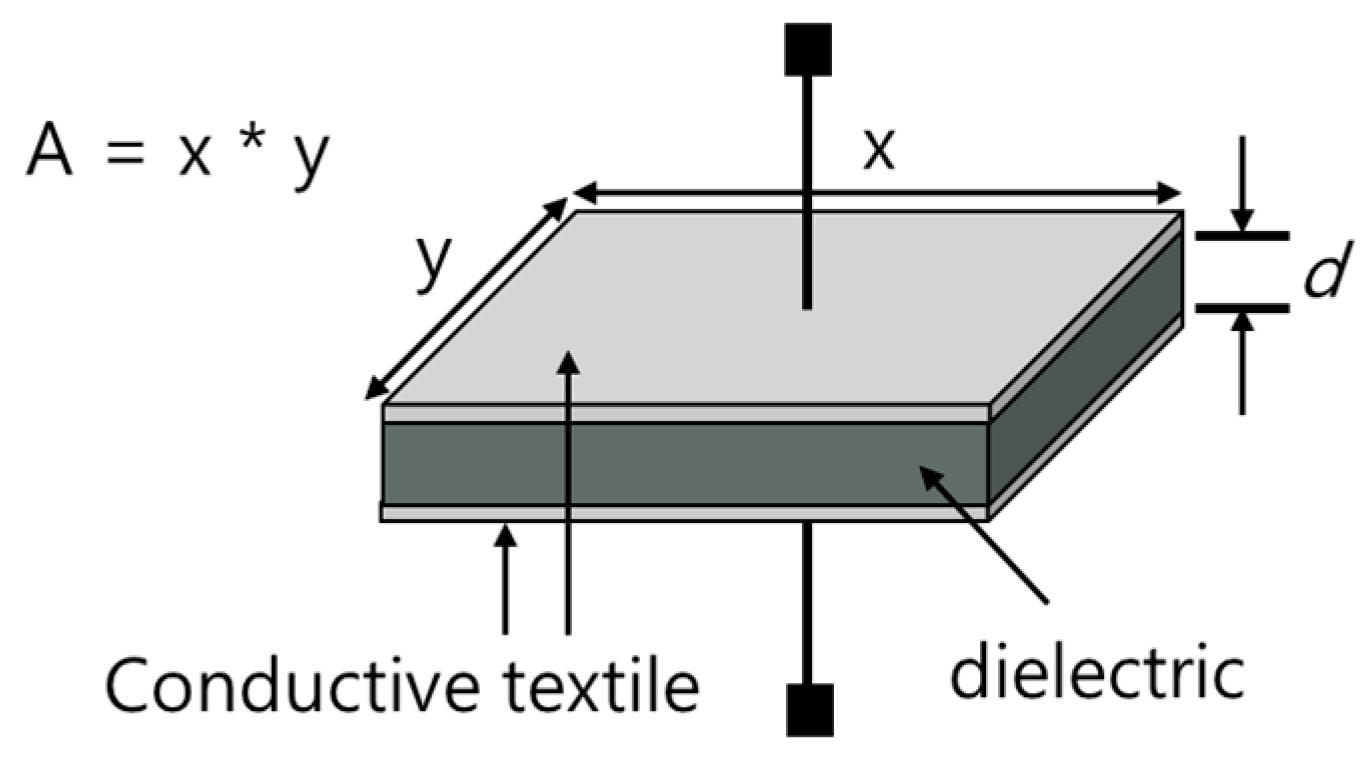
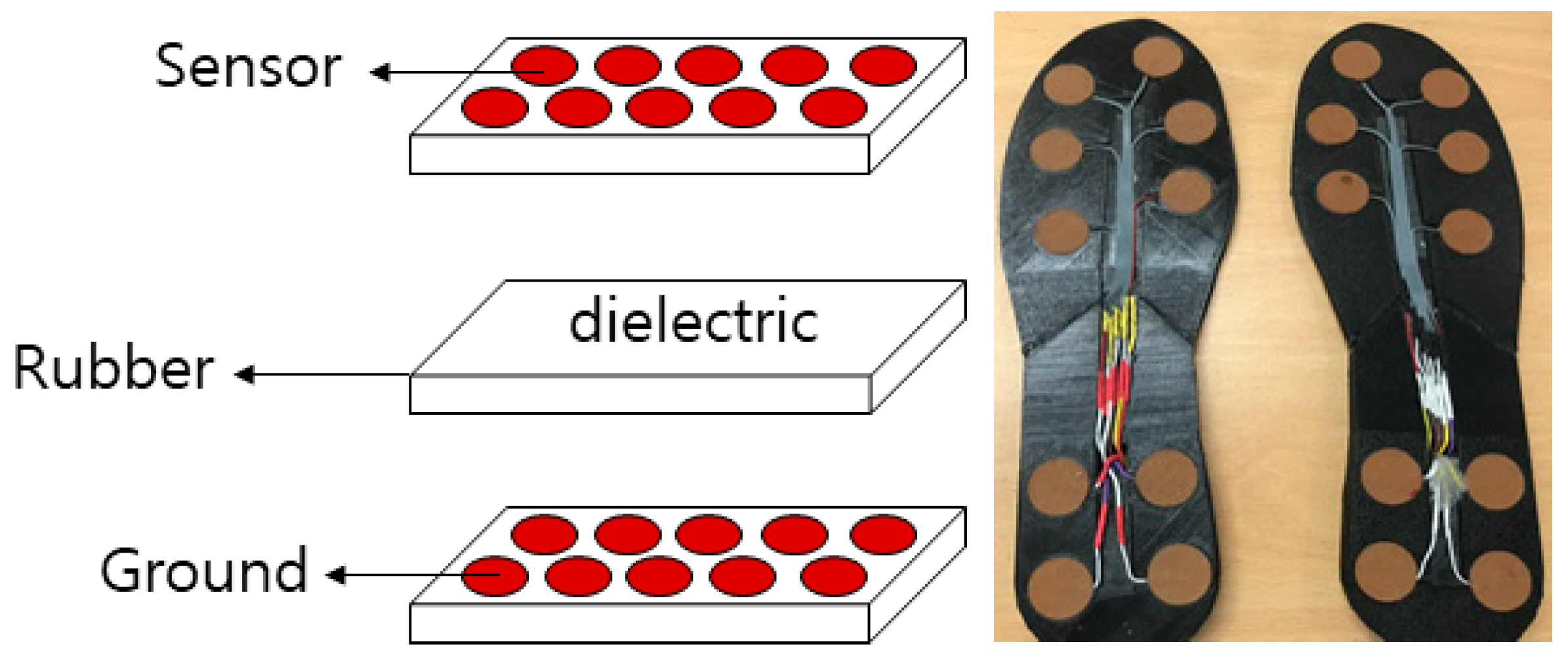
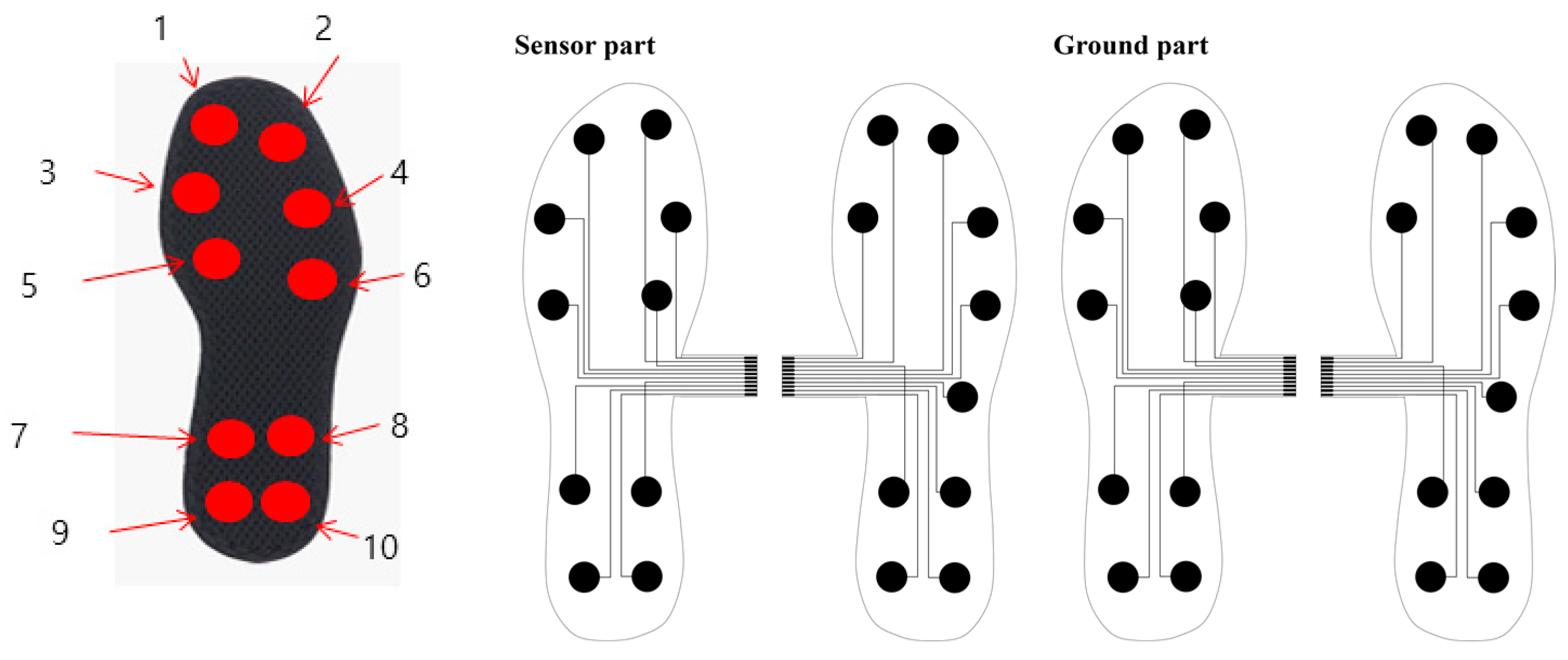
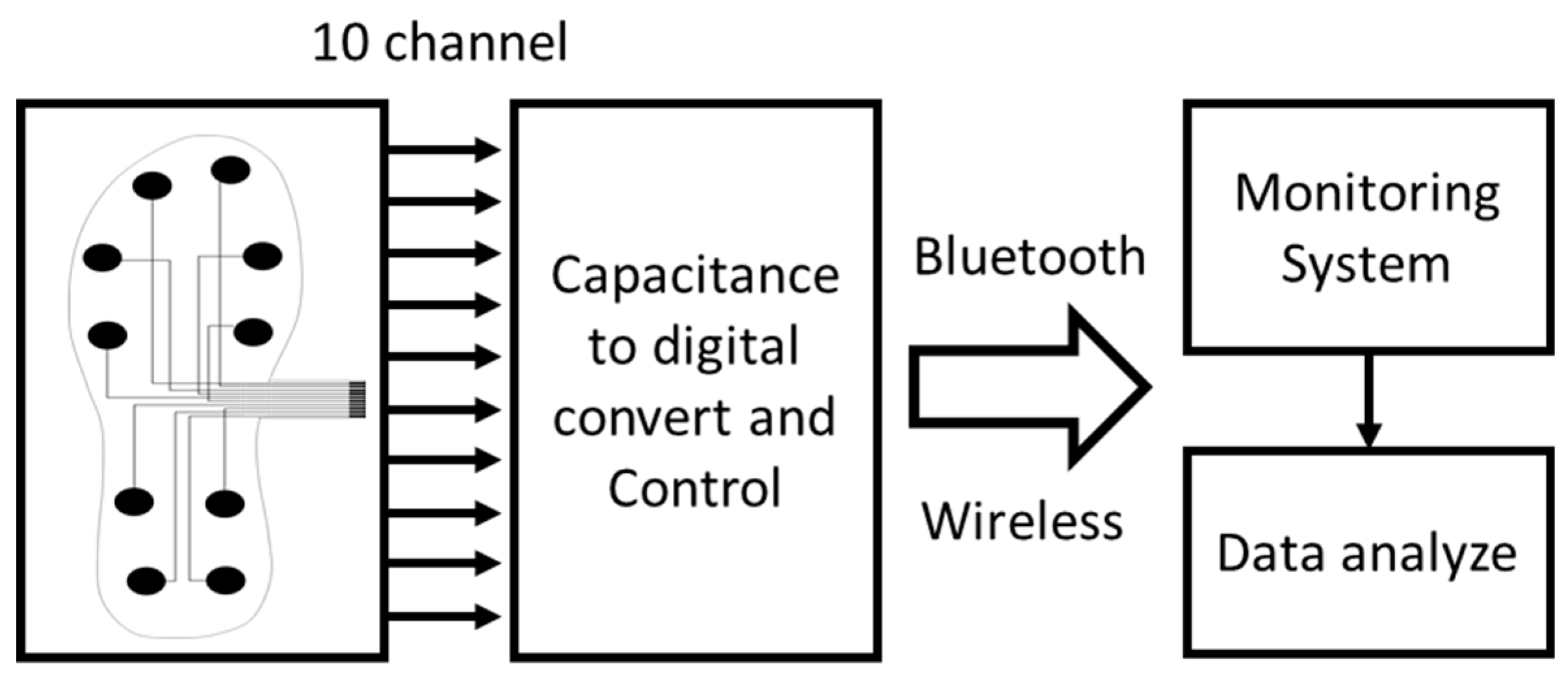
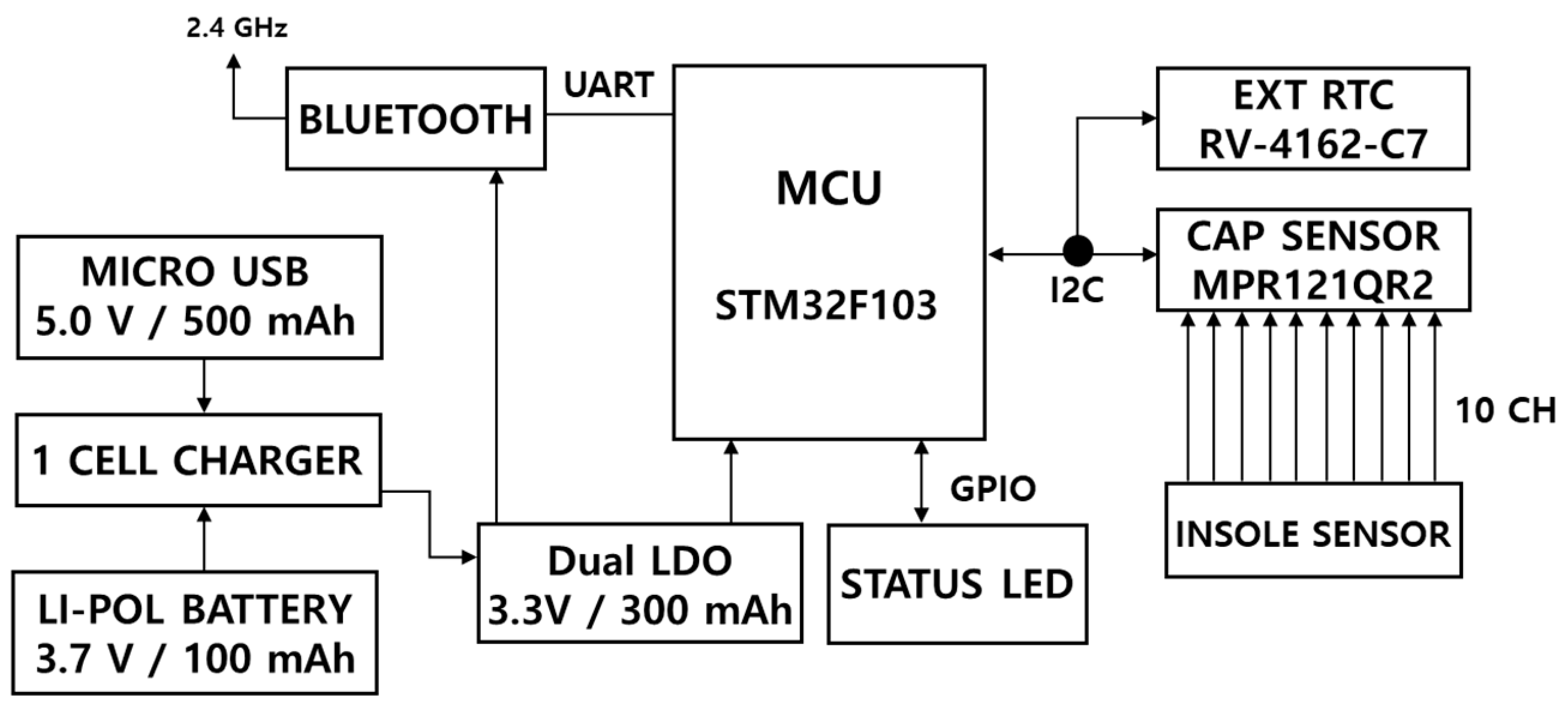
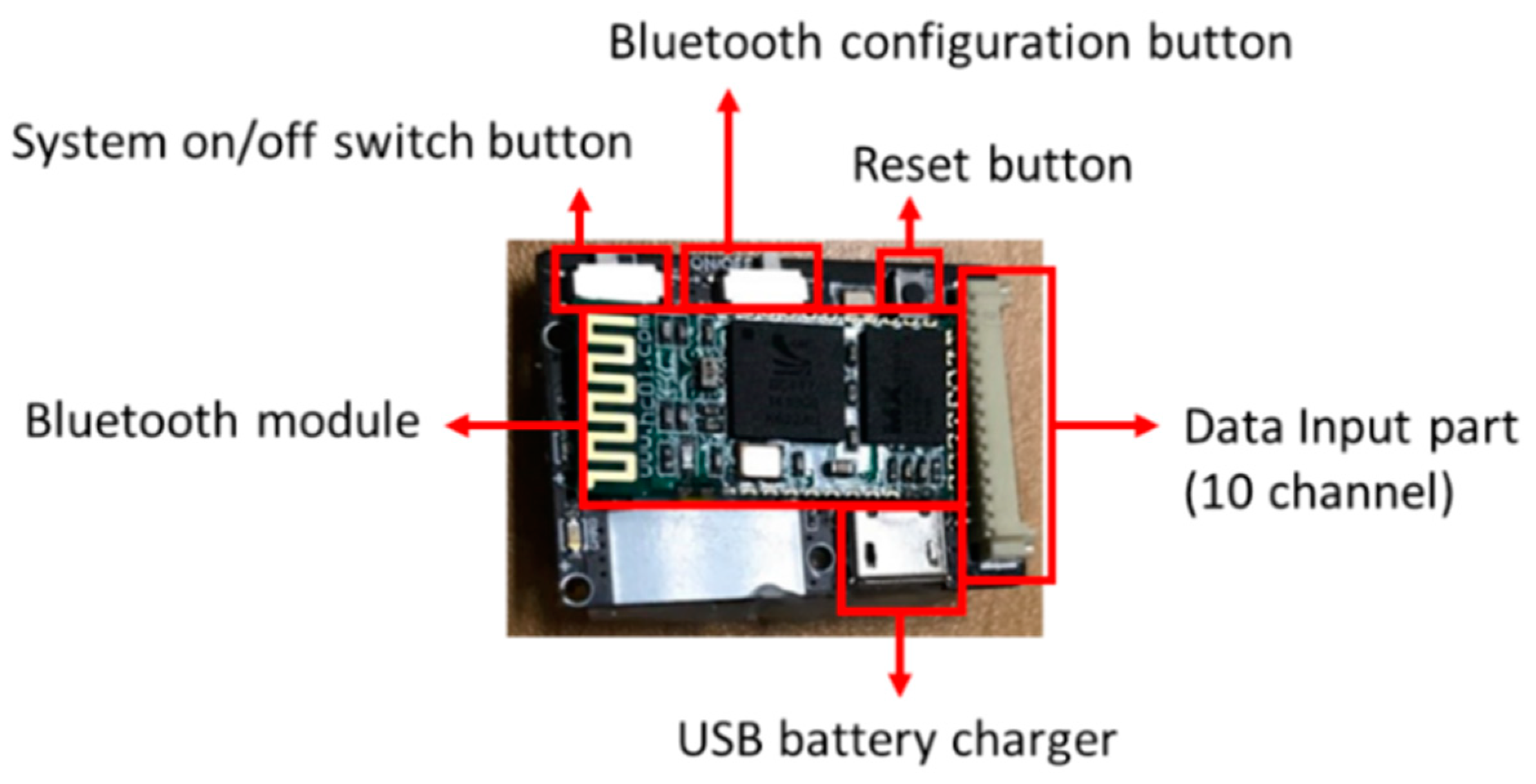
With the aim to overcome and complement the aforementioned limitations and fulfill the needs of a clinical field, this study used conductive textile, a type of soft material reported to be user-friendly, inexpensive, and easily transformable, to develop a practical sensor. A light-weight, durable, wireless, soft-material-based smart insole (SMSI) sensor was developed for accurate and affordable real-time gait analysis system and its range of feasibility was examined.
4. Discussion
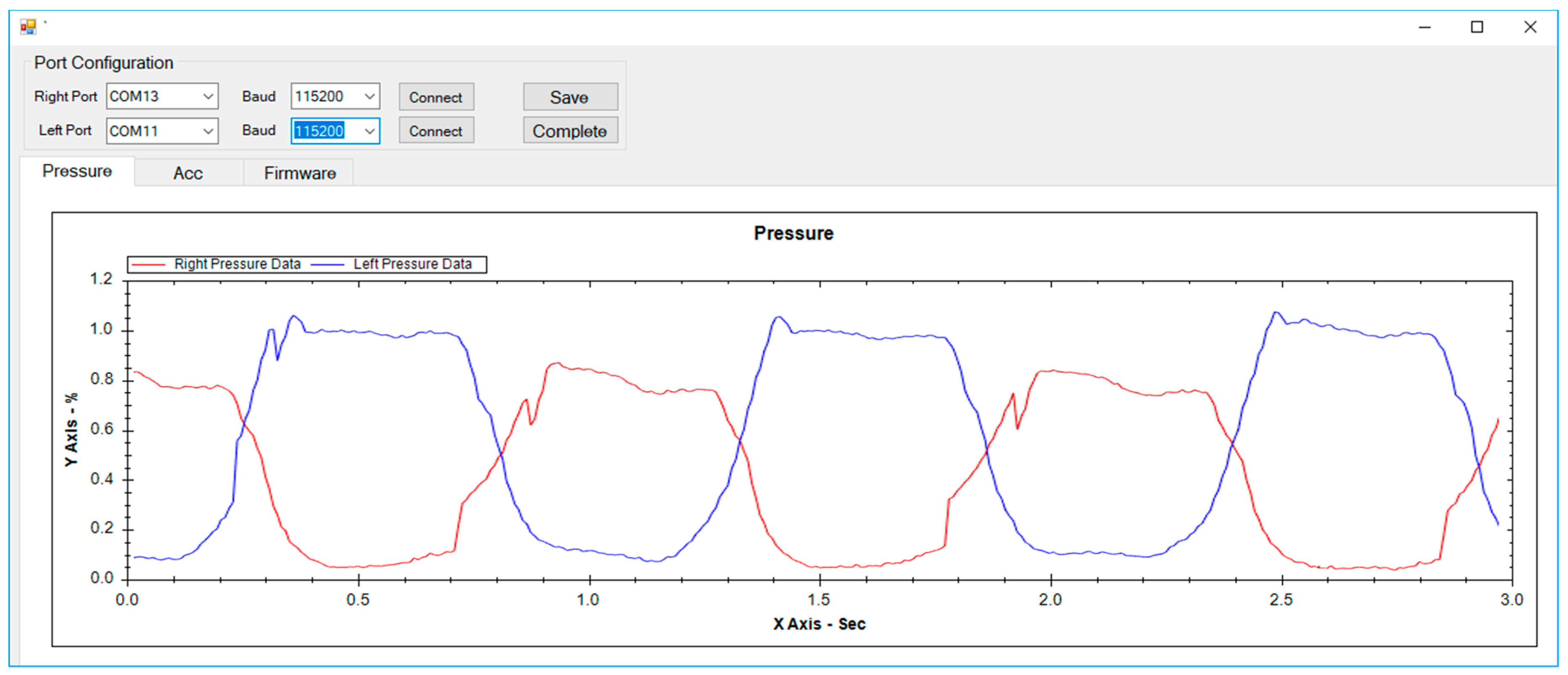
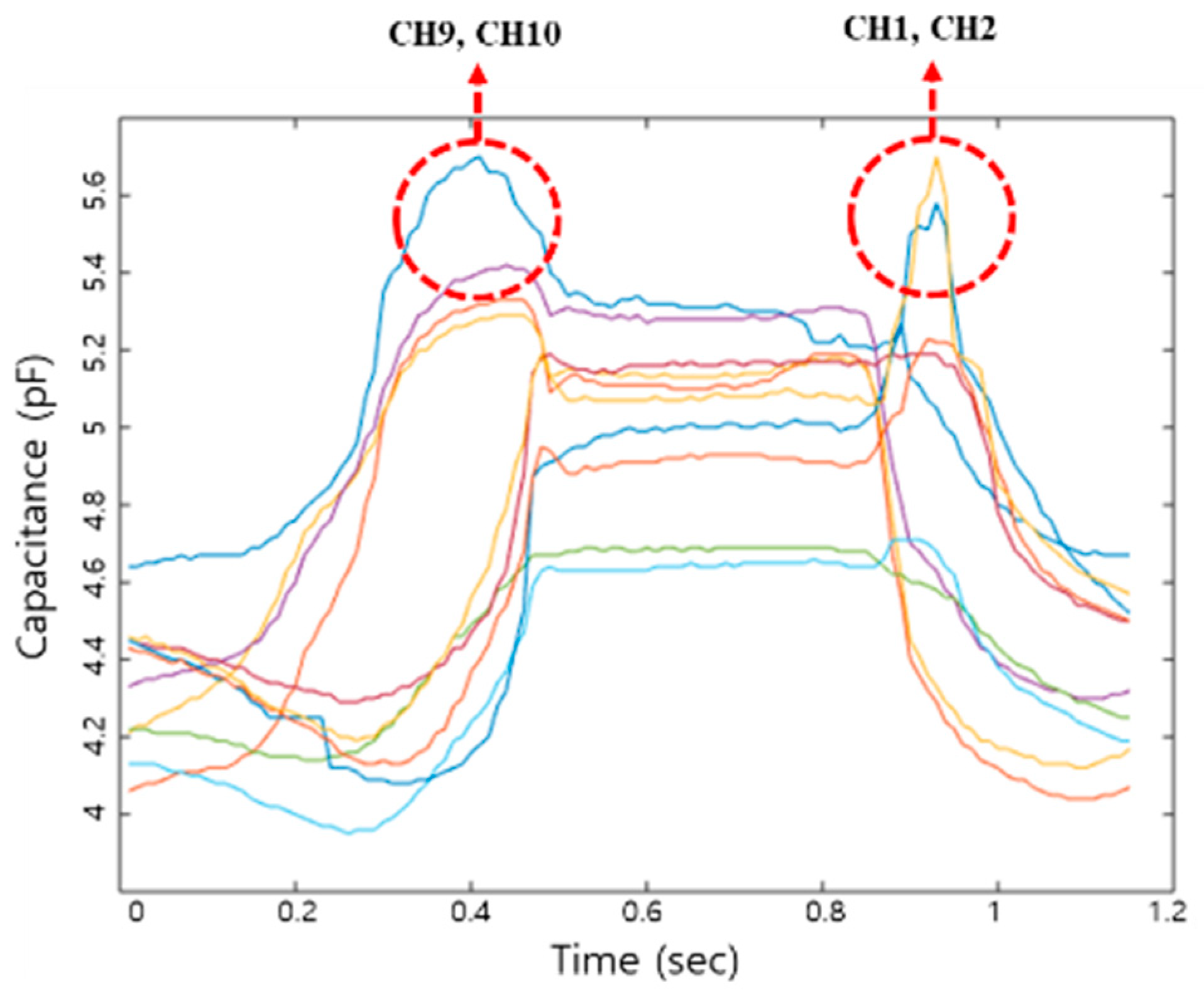
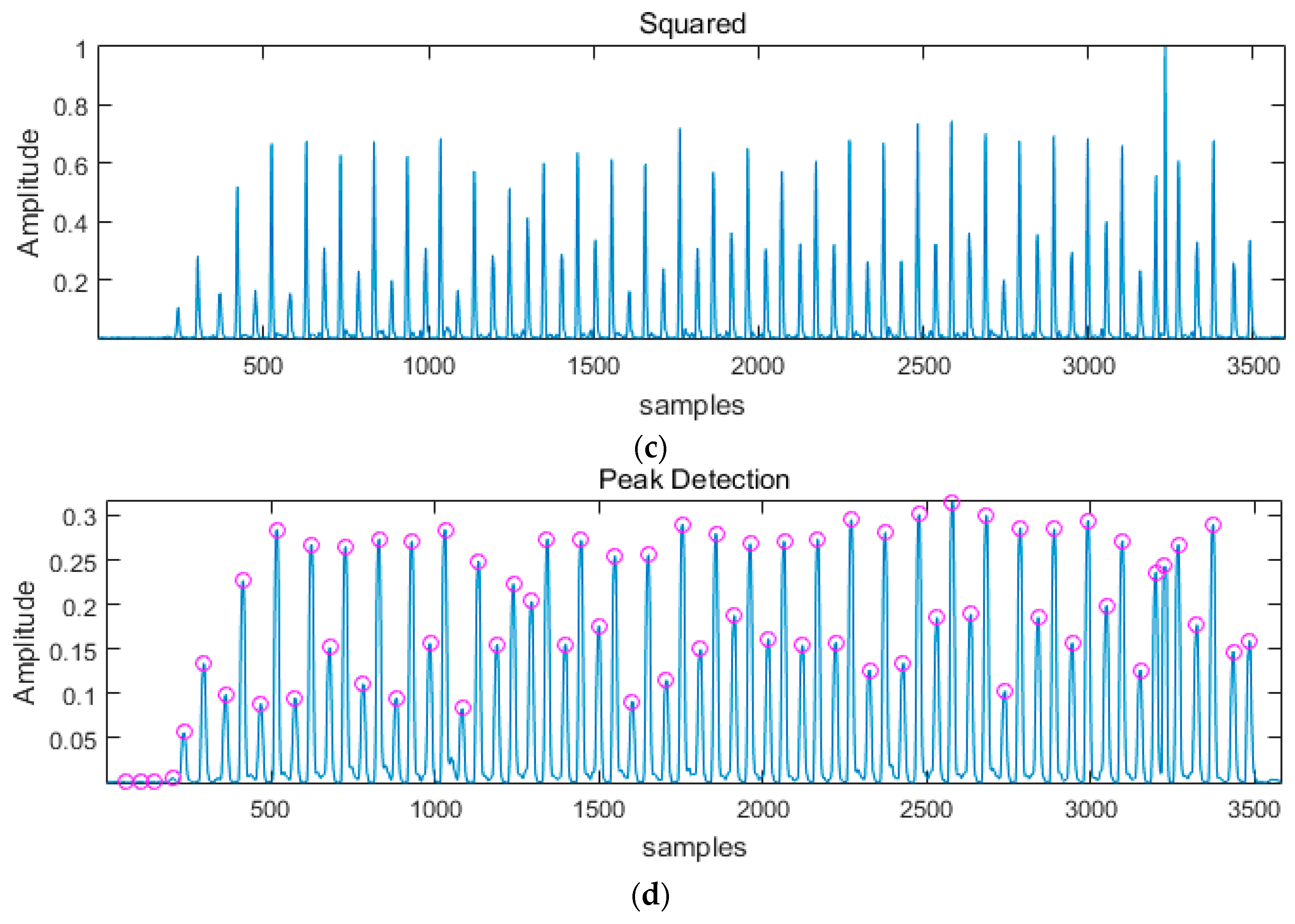
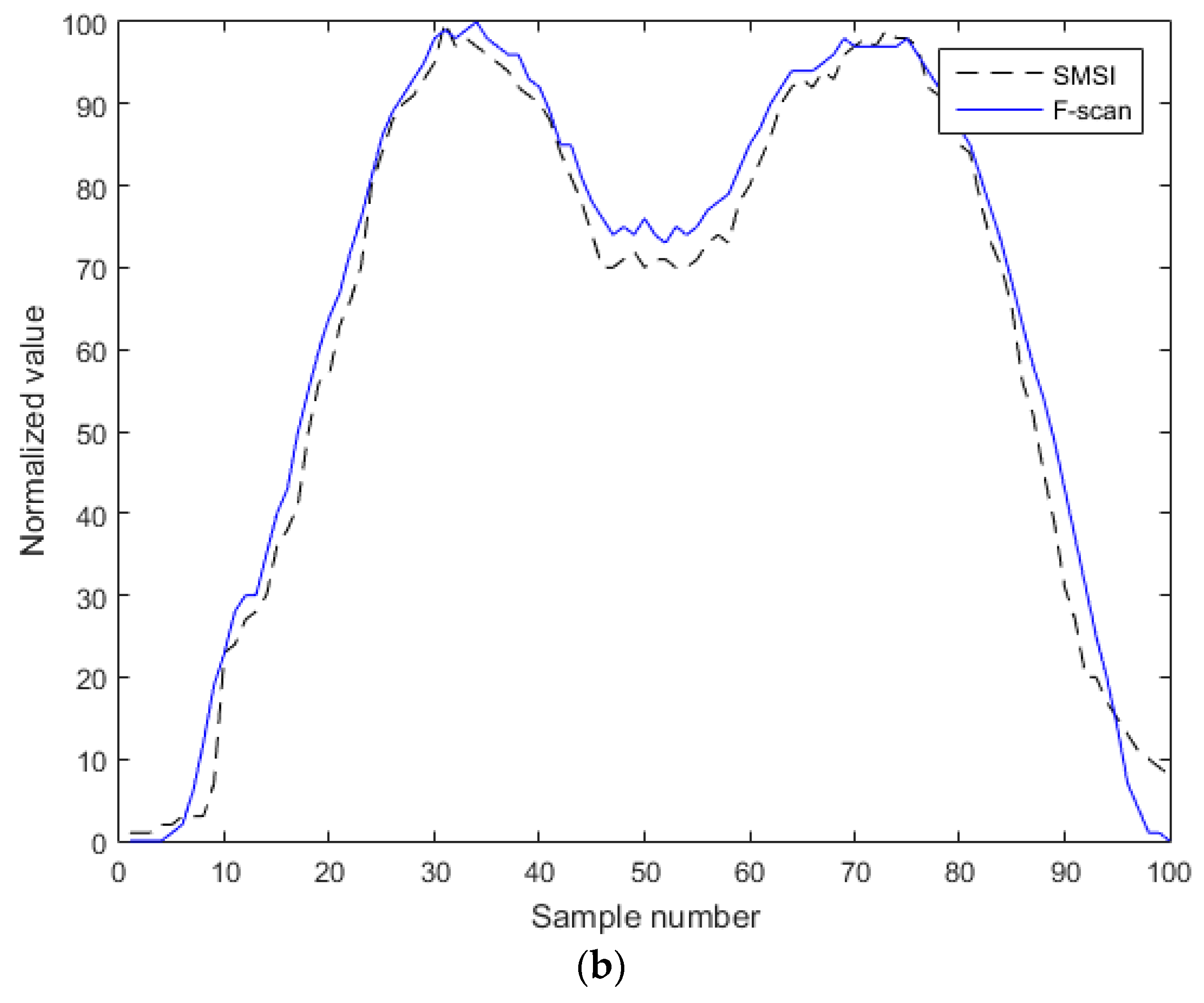
This study aimed to develop an SMSI and examine its feasibility for gait pattern analysis in healthy young adults. Gait data simultaneously collected by an SMSI and an F-scan, were compared in real-time, for analysis. Step-count was calculated by the peak detection method, and the results presented a 100% consistency in all four different gait speed conditions, showing that SMSI has an equivalent performance to the F-scan.
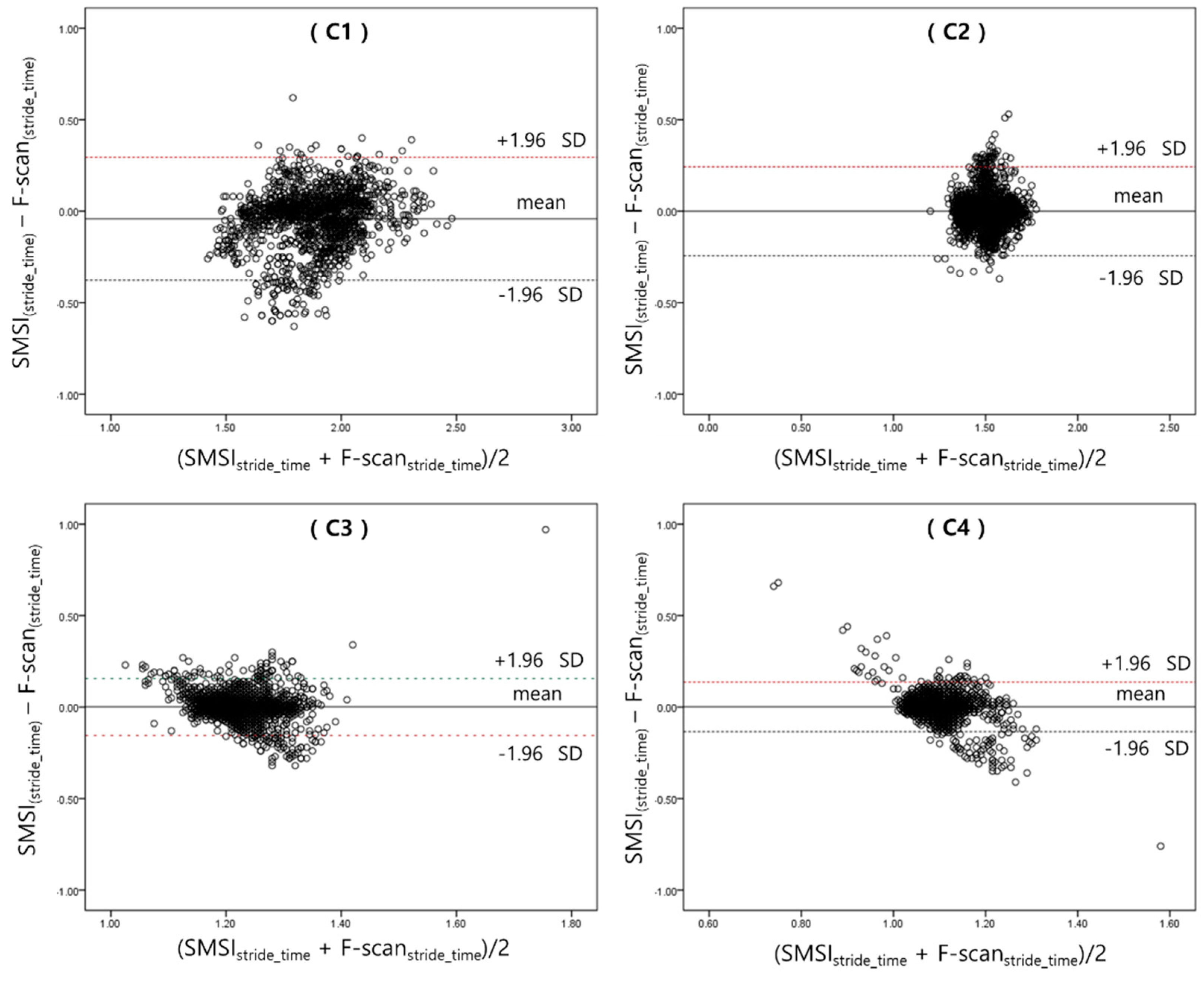
Considering the number of our subjects (n = 15), Spearman’s rho correlation analysis was performed to analyze the stride-time detected by the two sensors. R2 values for the left foot were higher or equal to 0.91 and those for the right foot were higher or equal to 0.90. The correlation coefficients showed to be statistically significant (p < 0.05), confirming the accuracy and feasibility of our sensor. However, the R2 values of C1, on both sides of the foot, were lower than those of the other speed conditions. This may have been caused by dislocation of the insole sensors, during gait; C1 being the slowest gait speed condition, the foot and the sensor may have got detached, from time-to-time.
We calculated the PCI value to test the clinical feasibility of the SMSI. The PCI is an indicator for evaluating balance function in the lower extremity and is presented in percentage. A value closer to 0% refers to higher balance between the two feet [
12,
17,
19,
28]. PCI was originally developed to evaluate the degree of asymmetry, during walking, and many studies evaluated the gait asymmetry of the patients with Parkinson’s disease and stroke [
17,
19,
28]. In the studies that evaluated gait asymmetry in healthy subjects, the PCI value was reported to be 2.52% and 2.47% [
17,
28].
In our study, the average PCI value of the SMSI was between 1.75 ± 0.80% (C1) and 1.72 ± 0.79% (C3), and that of the F-scan was between 1.66 ± 0.66% (C1) and 1.70 ± 0.62% (C4), which were similar to the findings from previous studies [
17,
28]. In addition, the R
2 values for the PCI showed a high correlation between the two sensors in both feet (R
2 ≥ 0.94,
p < 0.05). These values were also similar to the past findings, in other studies. Gait pattern is highly variable from person to person, especially when gender, age, body weight, cultural background, and medical history are taken into account. The reason behind the similarity in results may be due to the subject inclusion criteria. The average age of the healthy subjects in our study was 25.1 ± 2.64 and that of the other studies were 26.3 ± 0.5 and 26.3 ± 0.19, respectively.
Our study has a few limitations, even though our SMSI sensor was tested to have a high accuracy and performance capacity even with only ten channels embedded. Generalizing the results of this study may be difficult because the number of subjects was small. Future studies need to recruit a larger number of participants, as well as different age groups, for a more accurate and diverse data analysis. In this study, performance evaluation was conducted in a laboratory and did not consider temperature and humidity factors. As the results of this study showed clinical feasibility, further study in various environments (indoor and outdoor), considering changes in the temperature and humidity, could make use of the developed sensor and monitoring system, for both healthy and unhealthy individuals.
5. Conclusions
We developed a cost-effective, user-friendly, wearable soft-material-based smart insole sensor, with a real-time monitoring system and performed a feasibility test for the gait pattern analysis, in young healthy individuals, by compensating the limitations of the existing lab-based, expensive, analytic devices. Based on the results of this study, the utilization of our developed system is expected to expand to broader clinical, biomechanical, and quality of life-related studies.