Rheological Characterization as an Alternative Method to Indentation for Determining the Setting Time of Restorative and Endodontic Cements
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Preparation
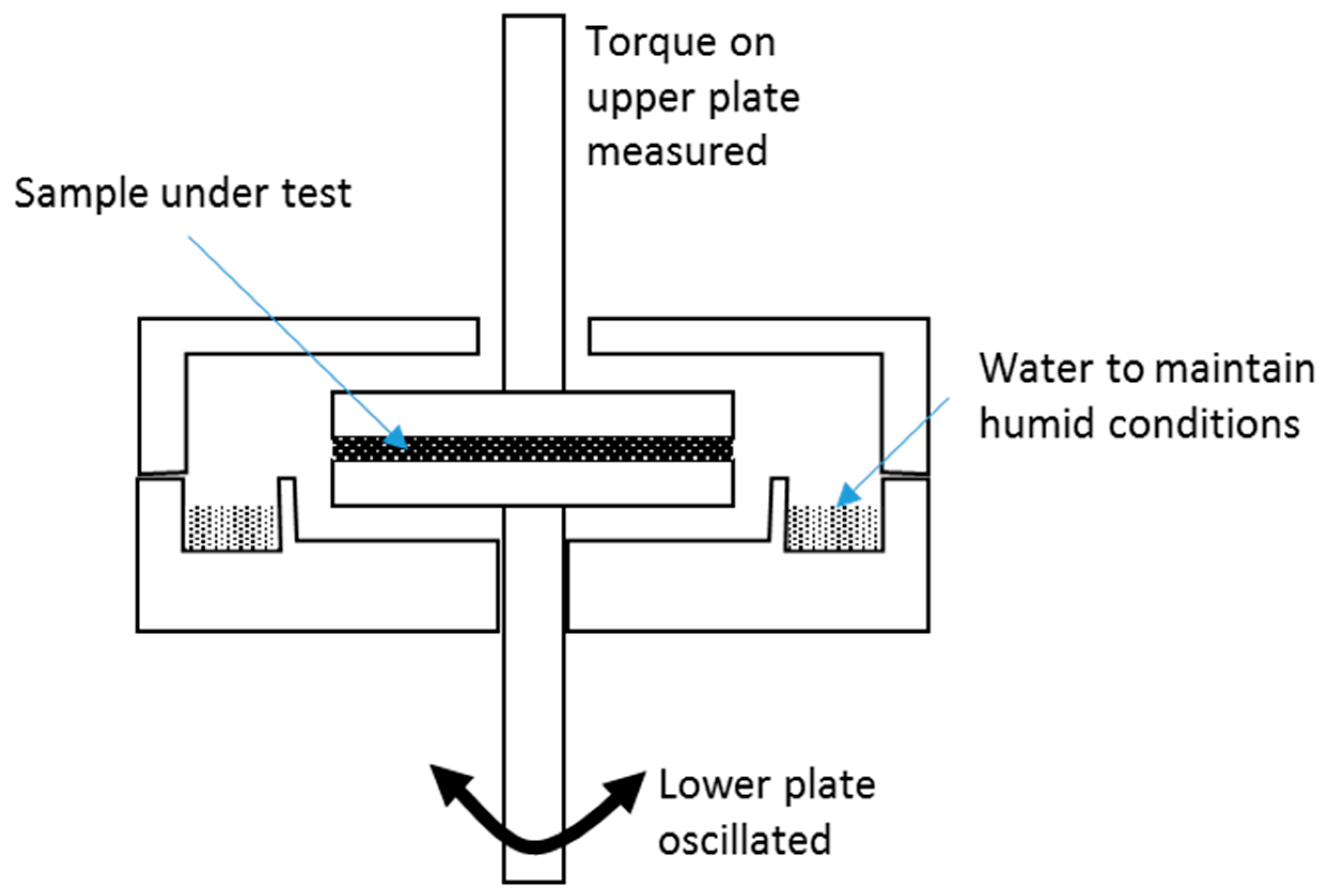
2.2. Rheological Testing
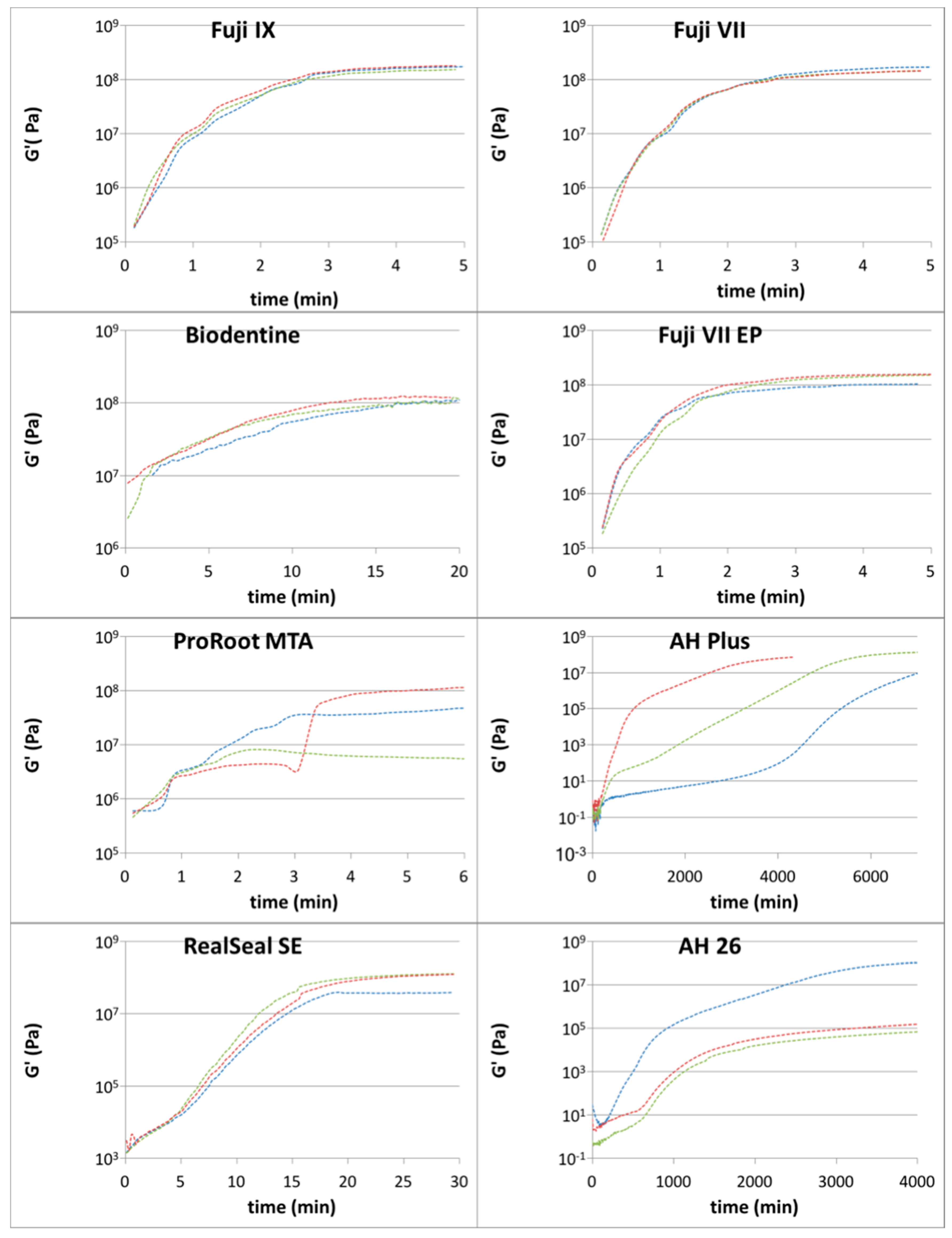
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ferro, K.J. The glossary of prosthodontic terms. J. Prosthet. Dent. 2005, 94, 10–92. [Google Scholar] [CrossRef]
- International Organization for Standardization. 1942:2009—Dentistry. Vocabulary, 2nd ed.; International Standard ISO 1942:2009; ISO: Geneva, Switzerland, 2009. [Google Scholar]
- American Association of Endodontists. Glossary of Endodontic Terms. Available online: http://www.nxtbook.com/nxtbooks/aae/endodonticglossary2016/-/0 (accessed on 17 August 2017).
- International Organization for Standardization. Dental Root Canal Sealing Materials, 3rd ed.; International Standard ISO 6876:2012; ISO: Geneva, Switzerland, 2012. [Google Scholar]
- International Organization for Standardization. Dentistry: Water-Based Cements. Part 1: Powder/Liquid Acid-Base Cements, 2nd ed.; International Standard ISO 9917-1:2007; ISO: Geneva, Switzerland, 2007. [Google Scholar]
- Ha, W.N.; Nicholson, T.; Kahler, B.; Walsh, L.J. Methodologies for measuring the setting times of mineral trioxide aggregate and Portland cement products used in dentistry. Acta Biomater. Odontol. Scand. 2016, 2, 25–30. [Google Scholar] [CrossRef] [PubMed]
- International Organization for Standardization. Dentistry—Polymer-Based Restorative Material, 4th ed.; International Standard ISO 4049:2009; ISO: Geneva, Switzerland, 2009. [Google Scholar]
- Macosko, C.W. Rheology: Principles, Measurements, and Applications; Wiley: Hoboken, NJ, USA, 1994; Available online: https://www.wiley.com/en-us/Rheology%3A+Principles%2C+Measurements%2C+and+Applications-p-9780471185758 (accessed on 20 December 2017).
- Lacey, S.; Pitt Ford, T.R.; Watson, T.F.; Sherriff, M. A study of the rheological properties of endodontic sealers. Int. Endod. J. 2005, 38, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.W.; Lee, Y.K.; Zhu, Q.; Shon, W.J.; Lee, W.C.; Kum, K.Y.; Baek, S.H.; Lee, I.B.; Lim, B.S.; Bae, K.S. Comparison of the rheological properties of four root canal sealers. Int. J. Oral Sci. 2015, 7, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Khedmat, S.; Momen-Heravi, F.; Pishvaei, M. Rheological properties of endodontic sealers: The effect of time, temperature, and composition. Iran. Polym. J. 2012, 21, 445–450. [Google Scholar] [CrossRef]
- Darvell, B.W. Materials Science for Dentistry, 9th ed.; Elsevier: Cambridge, UK, 2009; Available online: https://www.elsevier.com/books/materials-science-for-dentistry/darvell/978-1-84569-529-3 (accessed on 20 December 2017).
- Matsuya, S.; Maeda, T.; Ohta, M. IR and NMR analyses of hardening and maturation of glass-ionomer cement. J. Dent. Res. 1996, 75, 1920–1927. [Google Scholar] [CrossRef] [PubMed]
- Algera, T.J.; Kleverlaan, C.J.; Prahl-Andersen, B.; Feilzer, A.J. The influence of environmental conditions on the material properties of setting glass-ionomer cements. Dent. Mater. 2006, 22, 852–856. [Google Scholar] [CrossRef] [PubMed]
- Cook, W.D. Dental polyelectrolyte cements. III. Effect of additives on their rheology. Biomaterials 1983, 4, 85–88. [Google Scholar] [CrossRef]
- Cook, W.D. Dental polyelectrolyte cements: II: Effect of powder/liquid ratio on their rheology. Biomaterials 1983, 4, 21–24. [Google Scholar] [CrossRef]
- Torabinejad, J.; White, D.J. Tooth Filling Material and Method of Use. U.S. Patent 5,415,547, 16 May 1995. [Google Scholar]
- Tsujimoto, M.; Tsujimoto, Y.; Ookubo, A.; Shiraishi, T.; Watanabe, I.; Yamada, S.; Hayashi, Y. Timing for composite resin placement on mineral trioxide aggregate. J. Endod. 2013, 39, 1167–1170. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Park, S.J.; Lee, S.H.; Hwang, Y.C.; Yu, M.K.; Min, K.S. Biological effects and washout resistance of a newly developed fast-setting pozzolan cement. J. Endod. 2013, 39, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.B.; Park, S.J.; Kim, H.H.; Kwon, Y.S.; Lee, K.W.; Min, K.S. Physical properties and biological/odontogenic effects of an experimentally developed fast-setting alpha-tricalcium phosphate-based pulp capping material. BMC Oral Health 2014, 14, 87. [Google Scholar] [CrossRef] [PubMed]
- Ha, W.N.; Shakibaie, F.; Kahler, B.; Walsh, L.J. Deconvolution of the particle size distribution of ProRoot MTA and MTA Angelus. Acta Biomater. Odontol. Scand. 2016, 2, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Athanassiadis, B.; George, G.A.; Abbott, P.V.; Wash, L.J. A review of the effects of formaldehyde release from endodontic materials. Int. Endod. J. 2015, 48, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Dentsply DeTrey GmBH. AH Plus® Root Canal Sealer—Scientific Comendium. Available online: http://www.dentsply.ch/bausteine.net/f/7299/SCAHPlus050419rMV(Germanmarket).pdf?fd=2 (accessed on 19 December 2017).
- Kim, Y.K.; Grandini, S.; Ames, J.M.; Gu, L.S.; Kim, S.K.; Pashley, D.H.; Gutmann, J.L.; Tay, F.R. Critical review on methacrylate resin-based root canal sealers. J. Endod. 2010, 36, 383–399. [Google Scholar] [CrossRef] [PubMed]
- Meeks, K.W.; Carino, N.J. Curing of High-Performance Concrete: Report of the State-of-the-Art; NIST Internal Report 6295; NIST: Gaithersburg, MA, USA, 1999.
- Basturk, F.B.; Nekoofar, M.H.; Gunday, M.; Dummer, P.M. Effect of varying water-to-powder ratios and ultrasonic placement on the compressive strength of mineral trioxide aggregate. J. Endod. 2015, 41, 531–534. [Google Scholar] [CrossRef] [PubMed]
- Shahravan, A.; Jalali, S.P.; Torabi, M.; Haghdoost, A.A.; Gorjestani, H. A histological study of pulp reaction to various water/powder ratios of white mineral trioxide aggregate as pulp-capping material in human teeth: A double-blinded, randomized controlled trial. Int. Endod. J. 2011, 44, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- Ha, W.N.; Kahler, B.; Walsh, L.J. The influence of particle size and curing conditions on testing mineral trioxide aggregate cement. Acta Biomater. Odontol. Scand. 2016, 2, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.M.; Shen, Y.; Zheng, W.; Li, L.; Zheng, Y.F.; Haapasalo, M. Physical properties of 5 root canal sealers. J. Endod. 2013, 39, 1281–1286. [Google Scholar] [CrossRef] [PubMed]
- Kaup, M.; Schafer, E.; Dammaschke, T. An in vitro study of different material properties of Biodentine compared to Proroot MTA. Head Face Med. 2015, 11, 16. [Google Scholar] [CrossRef] [PubMed]
- Grech, L.; Mallia, B.; Camilleri, J. Investigation of the physical properties of tricalcium silicate cement-based root-end filling materials. Dent. Mater. 2013, 29, e20–e28. [Google Scholar] [CrossRef] [PubMed]
- Yesilyurt, C.; Yildirim, T.; Tasdemir, T.; Kusgoz, A. Shear bond strength of conventional glass ionomer cements bound to mineral trioxide aggregate. J. Endod. 2009, 35, 1381–1383. [Google Scholar] [CrossRef] [PubMed]
- Banfill, P. Rheology of fresh cement and concrete. Rheol. Rev. 2006, 2006, 61–130. [Google Scholar]
- Septodont. Biodentine™ Active Biosilicate Technology. 2010. Available online: http://www.plandent.no/images/Marketing/Infosenter/Biodentine%20Scientific%20File_web_dokumentasjon.pdf (accessed on 8 December 2017).
- Camilleri, J. Hydration mechanisms of mineral trioxide aggregate. Int. Endod. J. 2007, 40, 462–470. [Google Scholar] [CrossRef] [PubMed]
- Ha, W.N.; Bentz, D.P.; Kahler, B.; Walsh, L.J. D90: The strongest contributor to setting time in MTA and Portland cement. J. Endod. 2015, 41, 1146–1150. [Google Scholar] [CrossRef] [PubMed]
- Allan, N.A.; Walton, R.C.; Schaeffer, M.A. Setting times for endodontic sealers under clinical usage and in vitro conditions. J. Endod. 2001, 27, 421–423. [Google Scholar] [CrossRef] [PubMed]
| n | Mean (min) | SD (min) | SE | Margin of Error 1 (min) | Upper Bound (min) | Lower Bound (min) | Max (min) | Min (min) | Range (min) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Fuji IX GP Extra | 3 | 1.7 × 108 | 1.5 × 107 | 8.8 × 106 | 1.73 × 107 | 1.84 × 108 | 1.49 × 108 | 1.80 × 108 | 1.50 × 108 | 3.00 × 107 |
| Fuji VII | 3 | 1.5 × 108 | 1.7 × 107 | 1.0 × 107 | 1.96 × 107 | 1.70 × 108 | 1.30 × 108 | 1.70 × 108 | 1.40 × 108 | 3.00 × 107 |
| Fuji VII EP | 3 | 1.4 × 108 | 3.2 × 107 | 1.9 × 107 | 3.64 × 107 | 1.73 × 108 | 1.00 × 108 | 1.60 × 108 | 1.00 × 108 | 6.00 × 107 |
| Biodentine | 3 | 1.1 × 108 | 5.8 × 106 | 3.3 × 106 | 6.53 × 106 | 1.20 × 108 | 1.07 × 105 | 1.20 × 108 | 1.10 × 108 | 1.00 × 107 |
| ProRoot MTA | 3 | 6.4 × 107 | 5.6 × 107 | 3.2 × 107 | 6.33 × 107 | 1.27 × 108 | 7.20 × 108 | 1.20 × 108 | 8.10 × 108 | 1.12 × 108 |
| RealSeal SE | 3 | 9.6 × 107 | 5.0 × 107 | 2.9 × 107 | 5.65 × 107 | 1.53 × 108 | 3.99 × 107 | 1.30 × 108 | 3.90 × 107 | 9.10 × 107 |
| AH 26 | 3 | 4.3 × 107 | 7.5 × 107 | 4.3 × 107 | 8.48 × 107 | 1.28 × 108 | −4.13 × 107 | 1.30 × 108 | 1.80 × 105 | 1.30 × 108 |
| AH Plus | 3 | 7.5 × 107 | 6.4 × 107 | 3.7 × 107 | 7.19 × 107 | 1.47 × 108 | 2.72 × 106 | 1.40 × 108 | 1.30 × 107 | 1.27 × 108 |
| n | Mean (min) | SD (min) | SE | Margin of Error 1 (min) | Upper Bound (min) | Lower Bound (min) | Max (min) | Min (min) | Range (min) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Fuji IX GP Extra | 3 | 3.7 | 0.1 | 0.0 | 0.1 | 3.8 | 3.7 | 3.8 | 3.7 | 0.1 |
| Fuji VII | 3 | 3.6 | 0.2 | 0.1 | 0.2 | 3.8 | 3.4 | 3.8 | 3.5 | 0.3 |
| Fuji VII EP | 3 | 3.3 | 0.3 | 0.2 | 0.3 | 3.6 | 3.0 | 3.5 | 3.0 | 0.5 |
| Biodentine | 3 | 15.9 | 2.8 | 1.6 | 3.1 | 19.0 | 12.7 | 18.5 | 13.0 | 5.5 |
| ProRoot MTA | 3 | 5.1 | 2.8 | 1.6 | 3.2 | 8.3 | 1.9 | 7.6 | 2.0 | 5.6 |
| RealSeal SE | 3 | 22.2 | 3.6 | 2.1 | 4.1 | 26.3 | 18.2 | 24.4 | 18.1 | 6.3 |
| AH 26 | 3 | 5066.7 | 1674.3 | 966.7 | 1894.7 | 6961.3 | 3172.0 | 7000.0 | 4100.0 | 2900.0 |
| AH Plus | 3 | 5933.3 | 1686.2 | 973.5 | 1908.1 | 7841.5 | 4025.2 | 7100.0 | 4000.0 | 3100.0 |
| Dental Materials | Clinical Usage | Average Time to 90% Plateau G’ (min) | Marketed Setting Time 1 (min) | Testing Method of Setting Time 1 |
|---|---|---|---|---|
| Fuji IX GP Extra | General restorative | 3.7 | 2.0 | ISO 9917-1 |
| Fuji VII | General restorative | 3.6 | 2.5 | ISO 9917-1 |
| Fuji VII EP | General restorative | 3.3 | 2.5 | ISO 9917-1 |
| Biodentine | Root repair | 15.9 | 12.0 | Not stated |
| ProRoot MTA | Root repair | 5.1 | 240 | Not stated |
| RealSeal SE | Endodontic sealer | 22.2 | 45.0 | ISO 6876 |
| AH 26 | Endodontic sealer | 5933 | 540 to 900 | ISO 6876 |
| AH Plus | Endodontic sealer | 5066 | Minimum 480 | ISO 6876 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ha, W.N.; Nicholson, T.M.; Kahler, B.; Walsh, L.J. Rheological Characterization as an Alternative Method to Indentation for Determining the Setting Time of Restorative and Endodontic Cements. Materials 2017, 10, 1451. https://doi.org/10.3390/ma10121451
Ha WN, Nicholson TM, Kahler B, Walsh LJ. Rheological Characterization as an Alternative Method to Indentation for Determining the Setting Time of Restorative and Endodontic Cements. Materials. 2017; 10(12):1451. https://doi.org/10.3390/ma10121451
Chicago/Turabian StyleHa, William N., Timothy M. Nicholson, Bill Kahler, and Laurence J. Walsh. 2017. "Rheological Characterization as an Alternative Method to Indentation for Determining the Setting Time of Restorative and Endodontic Cements" Materials 10, no. 12: 1451. https://doi.org/10.3390/ma10121451
APA StyleHa, W. N., Nicholson, T. M., Kahler, B., & Walsh, L. J. (2017). Rheological Characterization as an Alternative Method to Indentation for Determining the Setting Time of Restorative and Endodontic Cements. Materials, 10(12), 1451. https://doi.org/10.3390/ma10121451







