Activation of Alkaline Irrigation Fluids in Endodontics
Abstract
:1. Introduction
2. Current Irrigation Protocols
3. Limitations of Conventional Treatments
4. Improvements to Irrigation Protocols
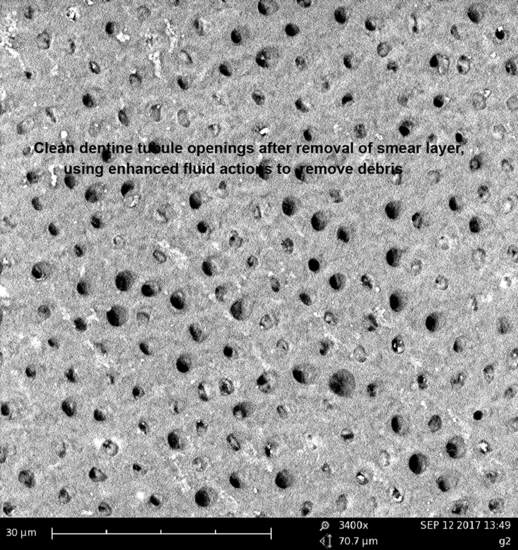
4.1. Improving Irrigant Flow in Root Canals Using Ultrasonic Agitation
4.2. Improving Irrigant Flow in Root Canals Using Middle Infrared Laser Activation
4.3. Improving Irrigant Flow in Root Canals Using Near Infrared Laser Activation
4.4. Optical Tip Designs for Improved Laser Agitation of Irrigants
5. Procedural Problems
5.1. Irrigant Fluid Extrusion
5.2. Endpoints for Laser Fluid Agitation
6. Methods for Assessing Effectiveness of Irrigation
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Narayan, G.S.; Venkatesan, S.M.; Karumaran, C.S.; Indira, R.; Ramachandran, S.; Srinivasan, M.R. A Comparative Evaluation on the Cleaning and Shaping Ability of Three Nickel Titanium Rotary Instruments using computerized tomography—An ex vivo study. Contemp. Clin. Dent. 2012, 3 (Suppl. 2), S151–S155. [Google Scholar] [CrossRef] [PubMed]
- Sen, B.H.; Wesselink, P.R.; Türkün, M. The Smear Layer: A Phenomenon in Root Canal Therapy. Int. Endod. J. 1995, 28, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Violich, D.R.; Chandler, N.P. The Smear Layer in Endodontics—A Review. Int. Endod. J. 2010, 43, 2–15. [Google Scholar] [CrossRef] [PubMed]
- Cobankara, F.K.; Ozkan, H.B.; Terlemez, A. Comparison of Organic Tissue Dissolution Capacities of Sodium Hypochlorite and Chlorine Dioxide. J. Endod. 2010, 36, 272–274. [Google Scholar] [CrossRef] [PubMed]
- Taneja, S.; Mishra, N.; Malik, S. Comparative Evaluation of Human Pulp Tissue Dissolution by Different Concentrations of Chlorine Dioxide, Calcium Hypochlorite and Sodium Hypochlorite: An in vitro Study. J. Conserv. Dent. 2014, 17, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Born, T.; Kontoghiorghe, C.N.; Spyrou, A.; Kolnagou, A.; Kontoghiorghes, G.J. EDTA Chelation Reappraisal Following New Clinical Trials and Regular use in Millions of Patients: Review of Preliminary Findings and Risk/Benefit Assessment. Toxicol. Mech. Methods 2013, 23, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Walker, A. A Definite and Dependable Therapy for Pulpless Teeth. J. Am. Dent. Assoc. 1936, 23, 1418–1425. [Google Scholar]
- Grossman, L.I.; Meiman, B.W. Solution of Pulp Tissue by Chemical Agents. J. Am. Dent. Assoc. 1941, 28, 223–225. [Google Scholar] [CrossRef]
- Berutti, E.; Marini, R. A Scanning Electron Microscopic Evaluation of the Debridement Capability of Sodium Hypochlorite at Different Temperatures. J. Endod. 1996, 22, 467–470. [Google Scholar] [CrossRef]
- Solovyeva, A.M.; Dummer, P.M. Cleaning Effectiveness of Root Canal Irrigation with Electrochemically Activated Anolyte and Catholyte Solutions: A Pilot Study. Int. Endod. J. 2000, 33, 494–504. [Google Scholar] [CrossRef] [PubMed]
- Fukuzaki, S. Mechanisms of Actions of Sodium Hypochlorite in Cleaning and Disinfection Processes. Biocontrol Sci. 2006, 11, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Rossi-Fedele, G.; Guastalli, A.R.; Doğramacı, E.J.; Steier, L.; De Figueiredo, J.A. Influence of pH Changes on Chlorine-containing Endodontic Irrigating Solutions. Int. Endod. J. 2011, 44, 792–799. [Google Scholar] [CrossRef] [PubMed]
- Kiran, S.; Prakash, S.; Siddharth, P.R.; Saha, S.; Geojan, N.E.; Ramachandran, M. Comparative Evaluation of Smear Layer and Debris on the Canal Walls prepared with a Combination of Hand and Rotary ProTaper Technique using Scanning Electron Microscope. J. Contemp. Dent. Pract. 2016, 17, 574–581. [Google Scholar] [PubMed]
- Ram, Z. Effectiveness of Root Canal Irrigation. Oral Surg. Oral Med. Oral Pathol. 1977, 44, 306–312. [Google Scholar] [CrossRef]
- Raisingani, D.; Meshram, G.K. Cleanliness in the Root Canal System: An Scanning Electron Microscopic Evaluation of Manual and Automated Instrumentation using 4% Sodium Hypochlorite and EDTA (Glyde File Prep)—An in vitro Study. Int. J. Clin. Pediatr. Dent. 2010, 3, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, J.F., Jr.; Rôças, I.N. Optimising Single-visit Disinfection with Supplementary Approaches: A Quest for Predictability. Aust. Endod. J. 2011, 37, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Gutarts, R.; Nusstein, J.; Reader, A.; Beck, M. In vivo Debridement Efficacy of Ultrasonic Irrigation following Hand-rotary Instrumentation in Human Mandibular Molars. J. Endod. 2005, 31, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Fedorowicz, Z.; Nasser, M.; Sequeira-Byron, P.; de Souza, R.F.; Carter, B.; Heft, M. Irrigants for Non-surgical Root Canal Treatment in Mature Permanent Teeth. Cochrane Database Syst. Rev. 2012, 9, CD008948. [Google Scholar]
- Da Mota, A.C.; Gonçalves, M.L.; Bortoletto, C.; Olivan, S.R.; Salgueiro, M.; Godoy, C.; Altavista, O.M.; Pinto, M.M.; Horliana, A.C.; Motta, L.J.; et al. Evaluation of the Effectiveness of Photodynamic Therapy for the Endodontic Treatment of Primary Teeth: Study Protocol for a Randomized Controlled Clinical Trial. Trials 2015, 16, 551. [Google Scholar] [CrossRef] [PubMed]
- Ng, R.; Singh, F.; Papamanou, D.A.; Song, X.; Patel, C.; Holewa, C.; Patel, N.; Klepac-Ceraj, V.; Fontana, C.R.; Kent, R.; et al. Endodontic Photodynamic Therapy ex vivo. J. Endod. 2011, 37, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Abou-Rass, M.; Piccinino, M.V. The Effectiveness of Four Clinical Irrigation Methods on the Removal of Root Canal Debris. Oral Surg. Oral Med. Oral Pathol. 1982, 54, 323–328. [Google Scholar] [CrossRef]
- Plotino, G.; Pameijer, C.H.; Grande, N.M.; Somma, F. Ultrasonics in Endodontics: A Review of the Literature. J. Endod. 2007, 33, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.; Pitt Ford, T.R.; Crum, L.A. Ultrasonic Debridement of Root Canals: Acoustic Streaming and its Possible Role. J. Endod. 1987, 13, 490–499. [Google Scholar] [CrossRef]
- Cameron, J.A. The Synergistic Relationship between Ultrasound and Sodium Hypochlorite: A Scanning Electron Microscope Evaluation. J. Endod. 1987, 13, 541–545. [Google Scholar] [CrossRef]
- Cameron, J.A. The Use of Ultrasound for the Removal of the Smear Layer. The Effect of Sodium Hypochlorite Concentration; SEM study. Aust. Dent. J. 1988, 33, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Haapasalo, M.; Shen, Y.; Qian, W.; Gao, Y. Irrigation in Endodontics. Dent. Clin. N. Am. 2010, 54, 291–312. [Google Scholar] [CrossRef] [PubMed]
- Walmsley, A.D. Ultrasound and Root Canal Treatment: The Need for Scientific Evaluation. Int. Endod. J. 1987, 20, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Kuah, H.G.; Lui, J.N.; Tseng, P.S.; Chen, N.N. The Effect of EDTA with and Without Ultrasonics on Removal of the Smear Layer. J. Endod. 2009, 35, 393–396. [Google Scholar] [CrossRef] [PubMed]
- Takeda, F.H.; Harashima, T.; Kimura, Y.; Matsumoto, K. Comparative Study about the Removal of Smear Layer by Three Types of Laser Devices. J. Clin. Laser Med. Surg. 1998, 16, 117–122. [Google Scholar] [PubMed]
- Takeda, F.H.; Harashima, T.; Kimura, Y.; Matsumoto, K. Efficacy of Er:YAG Laser Irradiation in Removing Debris and Smear Layer on Root Canal Walls. J. Endod. 1998, 24, 548–551. [Google Scholar] [CrossRef]
- Takeda, F.H.; Harashima, T.; Kimura, Y.; Matsumoto, K. A Comparative Study of the Removal of Smear Layer by Three Endodontic Irrigants and Two Types of Laser. Int. Endod. J. 1999, 32, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Jurič, I.B.; Anić, I. The Use of Lasers in Disinfection and Cleanliness of Root Canals: A Review. Acta Stomatol. Croat. 2014, 48, 6–15. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Meyers, I.A.; Walsh, L.J. Laser Activation of Endodontic Irrigants with Improved Conical Laser Fiber Tips for Removing Smear Layer in the Apical Third of the Root Canal. J. Endod. 2008, 34, 1524–1527. [Google Scholar] [CrossRef] [PubMed]
- De Groot, S.D.; Verhaagen, B.; Versluis, M.; Wu, M.K.; Wesselink, P.R.; van der Sluis, L.W. Laser-Activated Irrigation within Root Canals: Cleaning Efficacy and Flow Visualization. Int. Endod. J. 2009, 42, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Meire, M.A.; Havelaerts, S.; De Moor, R.J. Influence of Lasing Parameters on the Cleaning Efficacy of Laser-activated Irrigation with Pulsed Erbium Lasers. Lasers Med. Sci. 2016, 31, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Balić, M.; Lucić, R.; Mehadžić, K.; Bago, I.; Anić, I.; Jakovljević, S.; Plečko, V. The Efficacy of Photon-initiated Photoacoustic Streaming and Sonic-activated Irrigation combined with QMiX solution or Sodium Hypochlorite against intracanal E. faecalis Biofilm. Lasers Med. Sci. 2016, 31, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Arslan, D.; Guneser, M.B.; Dincer, A.N.; Kustarci, A.; Er, K.; Siso, S.H. Comparison of Smear Layer Removal Ability of QMix with Different Activation Techniques. J. Endod. 2016, 42, 1279–1285. [Google Scholar] [CrossRef] [PubMed]
- Blanken, J.; De Moor, R.J.; Meire, M.; Verdaasdonk, R. Laser Induced Explosive Vapor and Cavitation Resulting in Effective Irrigation of the Root Canal. Part 1: A Visualization Study. Lasers Surg. Med. 2009, 41, 514–519. [Google Scholar] [CrossRef] [PubMed]
- De Moor, R.J.; Blanken, J.; Meire, M.; Verdaasdonk, R. Laser Induced Explosive Vapor and Cavitation Resulting in Effective Irrigation of the Root Canal. Part 2: Evaluation of the Efficacy. Lasers Surg. Med. 2009, 41, 520–523. [Google Scholar] [CrossRef] [PubMed]
- Bago Jurič, I.; Plečko, V.; Anić, I. Antimicrobial Efficacy of Er,Cr:YSGG Laser-activated Irrigation compared with Passive Ultrasonic Irrigation and RinsEndo(®) against intracanal Enterococcus faecalis. Photomed. Laser Surg. 2014, 32, 600–605. [Google Scholar] [CrossRef] [PubMed]
- DiVito, E.E.; Colonna, M.P.; Olivi, G. The Photoacoustic Efficacy of an Er:YAG Laser with Radial and Stripped Tips on Root Canal Dentin Walls: An SEM Evaluation. J. Lasers Dent. 2011, 19, 156–161. [Google Scholar]
- Koch, J.D.; Jaramillo, D.E.; DiVito, E.; Peters, O.A. Irrigant Flow during Photon-induced Photoacoustic Streaming (PIPS) using Particle Image Velocimetry (PIV). Clin. Oral Investig. 2016, 20, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, A.; Uhles, J.P.; Clement, D.J.; Garcia-Godoy, F. Elimination of Intracanal Tissue and Debris through a Novel Laser-activated System Assessed using High-resolution Micro-computed Tomography: A Pilot Study. J. Endod. 2014, 40, 584–587. [Google Scholar] [CrossRef] [PubMed]
- Arslan, H.; Capar, I.D.; Saygili, G.; Gok, T.; Akcay, M. Effect of Photon-initiated Photoacoustic Streaming on Removal of Apically Placed Dentinal Debris. Int. Endod. J. 2014, 47, 1072–1077. [Google Scholar] [CrossRef] [PubMed]
- Akcay, M.; Arslan, H.; Mese, M.; Durmus, N.; Capar, I.D. Effect of Photon-initiated Photoacoustic Streaming, Passive Ultrasonic and Sonic Irrigation Techniques on Dentinal Tubule Penetration of Irrigation Solution: A Confocal Microscopic Study. Clin. Oral Investig. 2016. [Google Scholar] [CrossRef] [PubMed]
- Al Shahrani, M.; DiVito, E.; Hughes, C.V.; Nathanson, D.; Huang, G.T. Enhanced Removal of Enterococcus faecalis Biofilms in the Root Canal using Sodium Hypochlorite Plus Photon-induced Photoacoustic Streaming: An in vitro Study. Photomed. Laser Surg. 2004, 32, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Peters, O.A.; Bardsley, S.; Fong, J.; Pandher, G.; DiVito, E. Disinfection of Root Canals with Photon-initiated Photoacoustic Streaming. J. Endod. 2011, 37, 1008–1012. [Google Scholar] [CrossRef] [PubMed]
- Pedulla, E.; Genovese, C.; Campagna, E.; Tempera, R.E. Decontamination Efficacy of Photon-initiated Photoacoustic Streaming (PIPS) of Irrigants using Low-energy Laser Settings: An ex vivo Study. Int. Endod. J. 2012, 45, 865–870. [Google Scholar] [CrossRef] [PubMed]
- Sahar-Helfit, S.; Stabholz, A.; Moshonov, J.; Gutkin, V.; Redenski, I.; Steinberg, D. Effect of Er:YAG Laser Activated Irrigation Solution on Enterococcus faecalis Biofilm in an ex-vivo Root Canal Model. Photomed. Laser Surg. 2013, 31, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Yin, X.; Chang, J.W.; Wang, Y.; Cheung, G.S.; Zhang, C. Comparison of the Antibacterial Effect and Smear Layer Removal using Photon-initiated Photoacoustic Streaming Aided Irrigation versus a Conventional Irrigation in Single-rooted Canals: An in vitro Study. Photomed. Laser Surg. 2013, 31, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Olivi, G.; DiVito, E.; Peters, O.; Kaitsas, V.; Angiero, F.; Signore, A.; Benedicenti, S. Disinfection Efficacy of Photon-induced Photoacoustic Streaming on Root Canals infected with Enterococcus faecalis: An ex vivo Study. J. Am. Dent. Assoc. 2014, 145, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Guneser, M.B.; Arslan, D.; Usumez, A. Tissue Dissolution Ability of Sodium Hypochlorite Activated by Photon-initiated Photoacoustic Streaming Technique. J. Endod. 2015, 41, 729–732. [Google Scholar] [CrossRef] [PubMed]
- Akyuz Ekim, S.N.; Erdemir, A. Comparison of Different Irrigation Activation Techniques on Smear Layer Removal: An in vitro Study. Microsc. Res. Tech. 2015, 78, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Keles, A.; Kamalak, A.; Keskin, C.; Akçay, M.; Uzun, İ. The Efficacy of Laser, Ultrasound and Self-adjustable File in Removing Smear Layer Debris from Oval Root Canals following Retreatment: A Scanning Electron Microscopy Study. Aust. Endod. J. 2016, 42, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Deleu, E.; Meire, M.A.; De Moor, R.J. Efficacy of Laser-based Irrigant Activation Methods in Removing Debris from Simulated Root Canal Irregularities. Lasers Med. Sci. 2015, 30, 831–835. [Google Scholar] [CrossRef] [PubMed]
- Nasher, R.; Franzen, R.; Gutknecht, N. The Effectiveness of the Erbium:Yttrium Aluminum Garnet PIPS Technique in Comparison to Different Chemical Solutions in Removing the Endodontic Smear Layer—An in vitro Profilometric Study. Lasers Med. Sci. 2016, 31, 1871–1882. [Google Scholar] [CrossRef] [PubMed]
- Yost, R.A.; Bergeron, B.E.; Kirkpatrick, T.C.; Roberts, M.D.; Roberts, H.W.; Himel, V.T.; Sabey, K.A. Evaluation of 4 Different Irrigating Systems for Apical Extrusion of Sodium Hypochlorite. J. Endod. 2015, 41, 1530–1534. [Google Scholar] [CrossRef] [PubMed]
- Arslan, H.; Akcay, M.; Ertas, H.; Capar, I.D.; Saygili, G.; Meşe, M. Effect of PIPS Technique at Different Power settings on Irrigating Solution Extrusion. Lasers Med. Sci. 2015, 30, 1641–1645. [Google Scholar] [CrossRef] [PubMed]
- Azim, A.A.; Aksel, H.; Margaret Jefferson, M.; Huang, G.T. Comparison of Sodium Hypochlorite Extrusion by Five Irrigation Systems using an Artificial Root Socket Model and a Quantitative Chemical Method. Clin. Oral Investig. 2017. [Google Scholar] [CrossRef] [PubMed]
- Arslan, D.; Kustarci, A. Efficacy of Photon-initiated Photoacoustic Streaming on Apically Extruded Debris with Different Preparation Systems in Curved Canals. Int. Endod. J. 2017. [Google Scholar] [CrossRef] [PubMed]
- Hmud, R.; Kahler, W.A.; George, R.; Walsh, L.J. Cavitational Effects in Aqueous Endodontic Irrigants Generated by Near-infrared Lasers. J. Endod. 2010, 36, 275–278. [Google Scholar] [CrossRef] [PubMed]
- Hmud, R.; Kahler, W.A.; Walsh, L.J. Temperature Changes accompanying Near Infrared Diode Laser Endodontic Treatment of Wet Canals. J. Endod. 2010, 36, 908–911. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Rutley, E.B.; Walsh, L.J. Evaluation of Smear Layer: A Comparison of Automated Image Analysis versus Expert Observers. J. Endod. 2008, 34, 999–1002. [Google Scholar] [CrossRef] [PubMed]
- Lagemann, M.; George, R.; Chai, L.; Walsh, L.J. Activation of Ethylenediaminetetraacetic Acid by a 940 nm Diode Laser for Enhanced Removal of Smear Layer. Aust. Endod. J. 2014, 40, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Meire, M.A.; Poelman, D.; De Moor, R.J. Optical Properties of Root Canal Irrigants in the 300–3000-nm Wavelength Region. Lasers Med. Sci. 2014, 29, 1557–1562. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Walsh, L.J. Performance Assessment of Novel Side Firing Flexible Optical Fibers for Dental Applications. Lasers Surg. Med. 2009, 41, 214–221. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Walsh, L.J. Performance Assessment of Novel Side Firing Safe Tips for Endodontic Applications. J. Biomed. Opt. 2011, 16, 048004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, R.; Walsh, L.J. Laser Fiber-optic Modifications and Their Role in Endodontics. J. Laser Dent. 2012, 20, 24–30. [Google Scholar]
- George, R.; Walsh, L.J. Thermal Effects from Modified Endodontic Laser Tips used in the Apical Third of Root Canals with Erbium-doped Yttrium Aluminium Garnet and Erbium, Chromium-doped Yttrium Scandium Gallium Garnet Lasers. Photomed. Laser Surg. 2010, 28, 161–165. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Walsh, L.J. Apical Extrusion of Root Canal Irrigants when using Er:YAG and Er,Cr:YSGG Lasers with Optical Fibers: An in vitro Dye Study. J. Endod. 2008, 34, 706–708. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Chan, K.; Walsh, L.J. Laser-induced Agitation and Cavitation from Proprietary Honeycomb Tips for Endodontic Applications. Lasers Med. Sci. 2015, 30, 1203–1208. [Google Scholar] [CrossRef] [PubMed]
- Sainsbury, A.L.; Bird, P.S.; Walsh, L.J. DIAGNOdent Laser Fluorescence Assessment of Endodontic Infection. J. Endod. 2009, 35, 1404–1407. [Google Scholar] [CrossRef] [PubMed]
- Shakibaie, F.; Walsh, L.J. Surface Area and Volume Determination of Subgingival Calculus using Laser Fluorescence. Lasers Med. Sci. 2014, 29, 519–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, Q.V.; George, R.; Sainsbury, A.L.; Kahler, W.A.; Walsh, L.J. Laser Fluorescence Assessment of the Root Canal using Plain and Conical Optical Fibers. J. Endod. 2010, 36, 119–122. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walsh, L.J.; George, R. Activation of Alkaline Irrigation Fluids in Endodontics. Materials 2017, 10, 1214. https://doi.org/10.3390/ma10101214
Walsh LJ, George R. Activation of Alkaline Irrigation Fluids in Endodontics. Materials. 2017; 10(10):1214. https://doi.org/10.3390/ma10101214
Chicago/Turabian StyleWalsh, Laurence J., and Roy George. 2017. "Activation of Alkaline Irrigation Fluids in Endodontics" Materials 10, no. 10: 1214. https://doi.org/10.3390/ma10101214
APA StyleWalsh, L. J., & George, R. (2017). Activation of Alkaline Irrigation Fluids in Endodontics. Materials, 10(10), 1214. https://doi.org/10.3390/ma10101214