Sterol O-Acyltransferase Inhibition Ameliorates High-Fat Diet-Induced Renal Fibrosis and Tertiary Lymphoid Tissue Maturation after Ischemic Reperfusion Injury
Abstract
:1. Introduction
2. Results
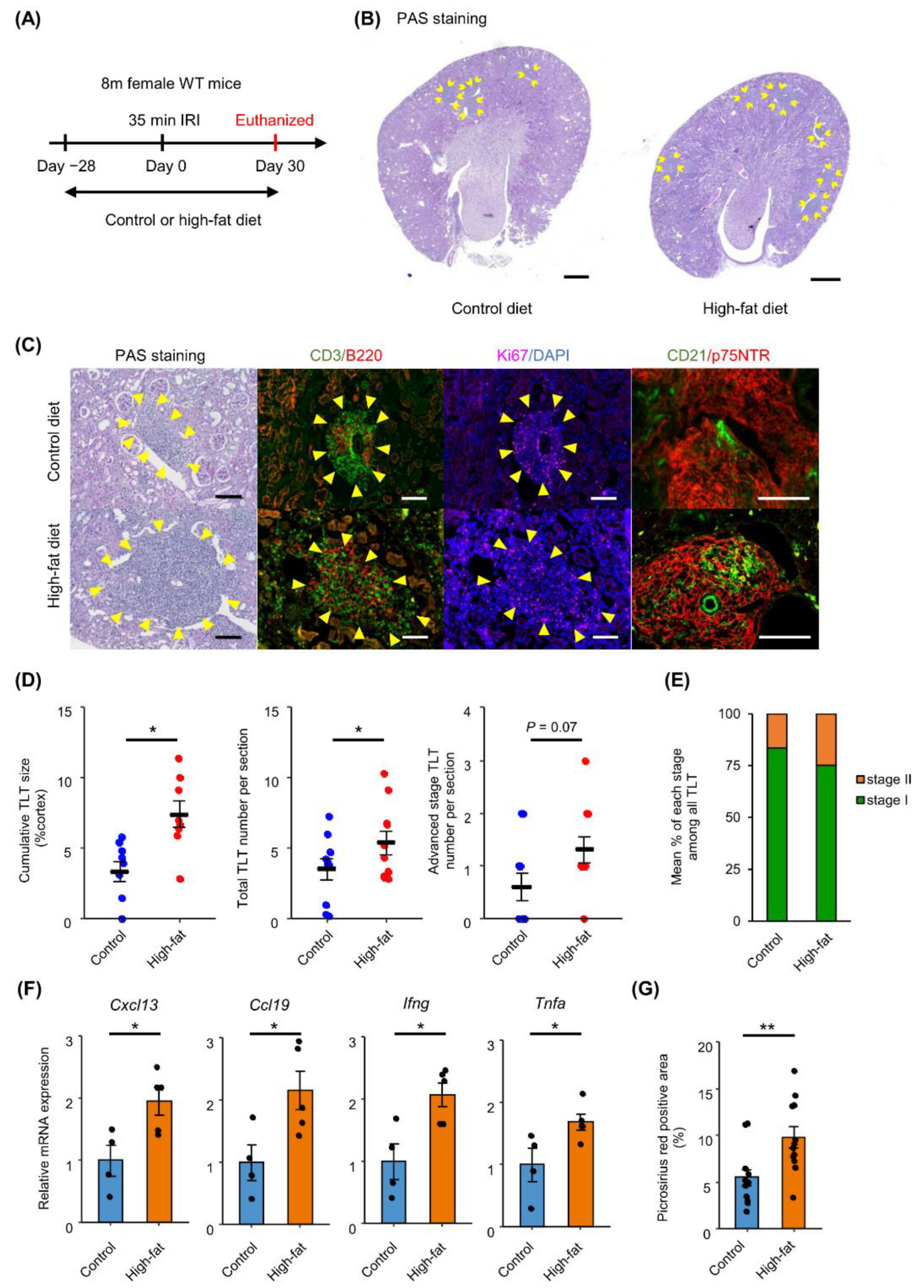
2.1. HFD Feeding Promotes TLT Formation in Aged Kidneys after Ischemic Reperfusion Injury (IRI)
2.2. Untargeted Lipidomics Reveals Prominent Increase of Cholesteryl Ester in Aged Injured Kidneys with TLTs
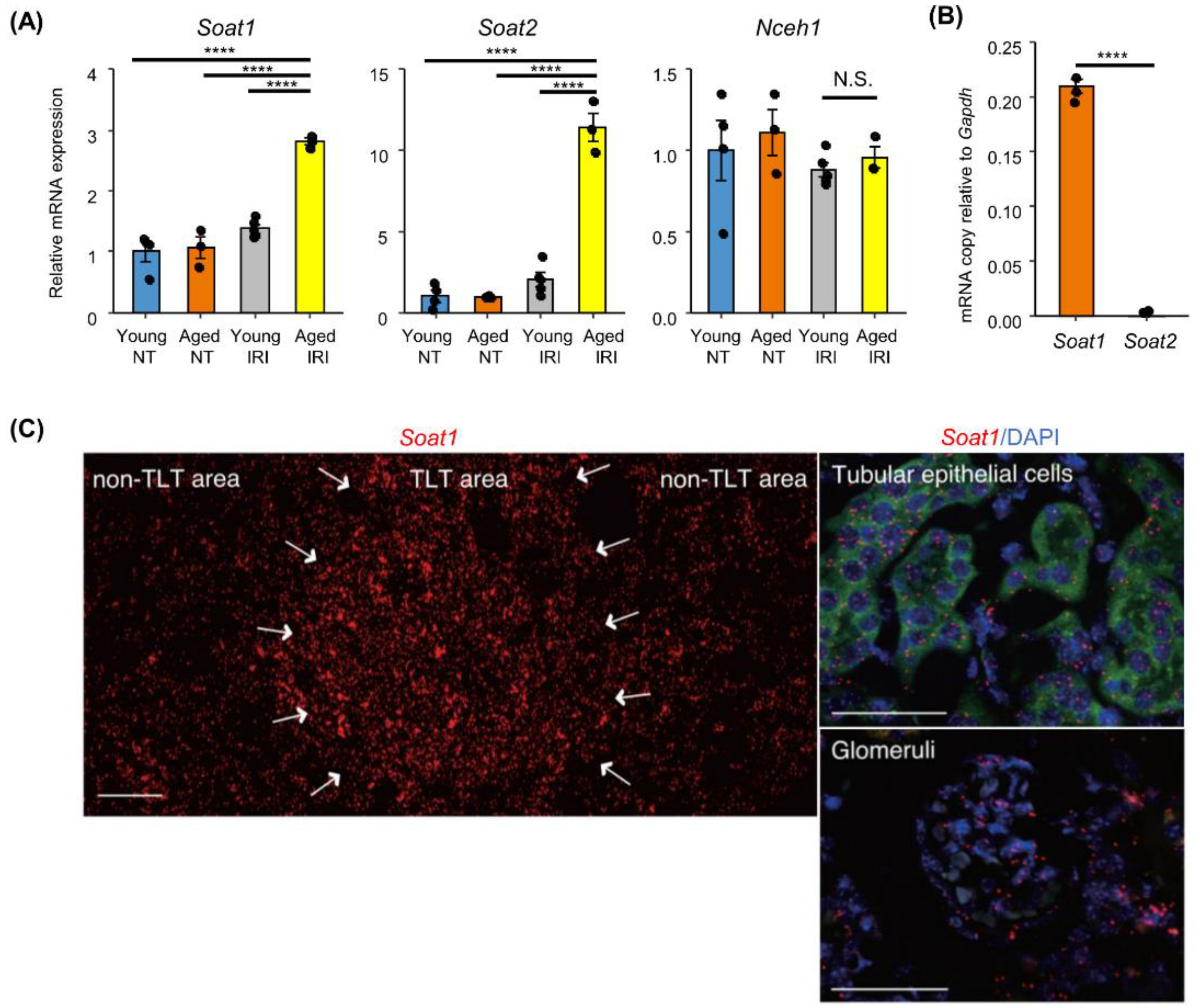
2.3. Increased Sterol O-Acyltransferase (SOAT) Expression in Aged Kidneys after IRI
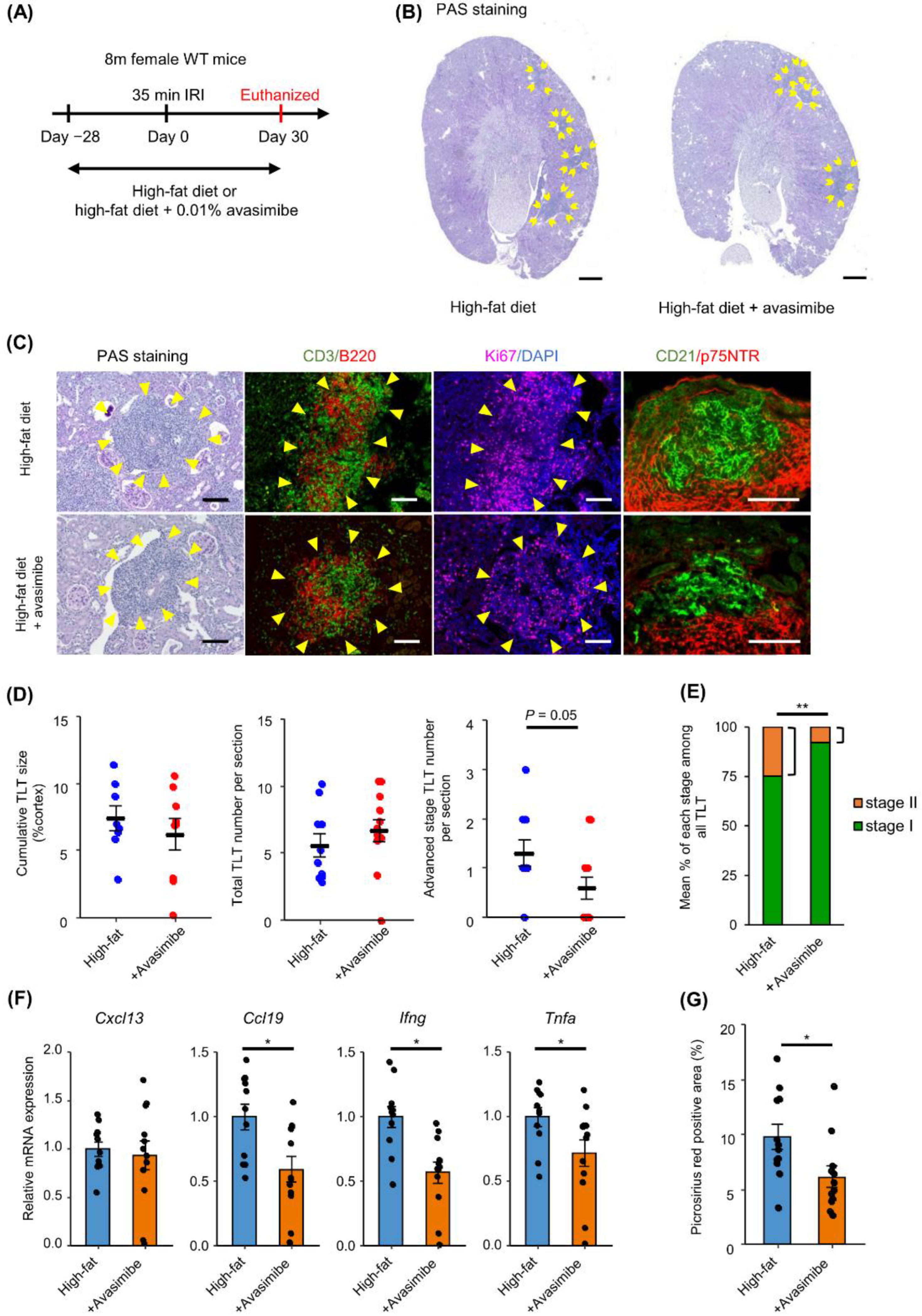
2.4. SOAT Inhibition Ameliorates TLT Maturation and Renal Fibrosis
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Kidney Ischemic Reperfusion Injury Model
4.3. Lipid Extraction
4.4. Liquid Chromatography-Mass Spectrometry-Based Untargeted Lipidomics
4.5. Annotation and Quantification of Lipids
4.6. Quantification of TLT Size
4.7. Evaluation of TLT Stage
4.8. Evaluation of Fibrotic Area
4.9. Immunofluorescence
4.10. Quantitative Reverse Transcription Polymerase Chain Reaction (RT-qPCR)
4.11. In Situ Hybridization
4.12. Statistics and Data Visualization
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, Y.; Chen, X.; Song, Y.; Caballero, B.; Cheskin, L.J. Association between Obesity and Kidney Disease: A Systematic Review and Meta-Analysis. Kidney Int. 2008, 73, 19–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, C.; McCulloch, C.E.; Iribarren, C.; Darbinian, J.; Go, A.S. Body Mass Index and Risk for End-Stage Renal Disease. Ann. Intern. Med. 2006, 144, 21–28. [Google Scholar] [CrossRef] [PubMed]
- D’Agati, V.D.; Chagnac, A.; de Vries, A.P.J.; Levi, M.; Porrini, E.; Herman-Edelstein, M.; Praga, M. Obesity-Related Glomerulopathy: Clinical and Pathologic Characteristics and Pathogenesis. Nat. Rev. Nephrol. 2016, 12, 453–471. [Google Scholar] [CrossRef] [PubMed]
- de Vries, A.P.J.; Ruggenenti, P.; Ruan, X.Z.; Praga, M.; Cruzado, J.M.; Bajema, I.M.; D’Agati, V.D.; Lamb, H.J.; Barlovic, D.P.; Hojs, R.; et al. Fatty Kidney: Emerging Role of Ectopic Lipid in Obesity-Related Renal Disease. Lancet Diabetes Endocrinol. 2014, 2, 417–426. [Google Scholar] [CrossRef]
- Sun, Y.; Ge, X.; Li, X.; He, J.; Wei, X.; Du, J.; Sun, J.; Li, X.; Xun, Z.; Liu, W.; et al. High-Fat Diet Promotes Renal Injury by Inducing Oxidative Stress and Mitochondrial Dysfunction. Cell Death Dis. 2020, 11, 914. [Google Scholar] [CrossRef]
- Sato, Y.; Takahashi, M.; Yanagita, M. Pathophysiology of AKI to CKD Progression. Semin. Nephrol. 2020, 40, 206–215. [Google Scholar] [CrossRef]
- Sato, Y.; Mii, A.; Hamazaki, Y.; Fujita, H.; Nakata, H.; Masuda, K.; Nishiyama, S.; Shibuya, S.; Haga, H.; Ogawa, O.; et al. Heterogeneous Fibroblasts Underlie Age-Dependent Tertiary Lymphoid Tissues in the Kidney. JCI Insight 2016, 1, e87680. [Google Scholar] [CrossRef] [Green Version]
- Sato, Y.; Oguchi, A.; Fukushima, Y.; Masuda, K.; Toriu, N.; Taniguchi, K.; Yoshikawa, T.; Cui, X.; Kondo, M.; Hosoi, T.; et al. CD153/CD30 Signaling Promotes Age-Dependent Tertiary Lymphoid Tissue Expansion and Kidney Injury. J. Clin. Investig. 2022, 132, e146071. [Google Scholar] [CrossRef]
- Gago da Graça, C.; van Baarsen, L.G.M.; Mebius, R.E. Tertiary Lymphoid Structures: Diversity in Their Development, Composition, and Role. J. Immunol. 2021, 206, 273–281. [Google Scholar] [CrossRef]
- Sato, Y.; Yanagita, M. Immunology of the Ageing Kidney. Nat. Rev. Nephrol. 2019, 15, 625–640. [Google Scholar] [CrossRef]
- Sato, Y.; Tamura, M.; Yanagita, M. Tertiary Lymphoid Tissues: A Regional Hub for Kidney Inflammation. Nephrol. Dial. Transplant. 2021, gfab212. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Boor, P.; Fukuma, S.; Klinkhammer, B.M.; Haga, H.; Ogawa, O.; Floege, J.; Yanagita, M. Developmental Stages of Tertiary Lymphoid Tissue Reflect Local Injury and Inflammation in Mouse and Human Kidneys. Kidney Int. 2020, 98, 448–463. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Sato, Y.; Saito, M.; Fukuma, S.; Saito, M.; Yamamoto, S.; Komatsuda, A.; Yamada, N.; Satoh, S.; Lee, S.-H.; et al. Advanced Tertiary Lymphoid Tissues in Protocol Biopsies Are Associated with Progressive Graft Dysfunction in Kidney Transplant Recipients. J. Am. Soc. Nephrol. 2022, 33, 186–200. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.L.; Cho, K.W.; Del Proposto, J.L.; Oatmen, K.E.; Geletka, L.M.; Martinez-Santibanez, G.; Singer, K.; Lumeng, C.N. Adipose Tissue Macrophages Function as Antigen-Presenting Cells and Regulate Adipose Tissue CD4+ T Cells in Mice. Diabetes 2013, 62, 2762–2772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishikawa, S.; Yasoshima, A.; Doi, K.; Nakayama, H.; Uetsuka, K. Involvement of Sex, Strain and Age Factors in High Fat Diet-Induced Obesity in C57BL/6J and BALB/cA Mice. Exp. Anim. 2007, 56, 263–272. [Google Scholar] [CrossRef] [Green Version]
- Sato, Y.; Yanagita, M. Functional Heterogeneity of Resident Fibroblasts in the Kidney. Proc. Jpn. Acad. Ser. B 2019, 95, 468–478. [Google Scholar] [CrossRef] [Green Version]
- Krautler, N.J.; Kana, V.; Kranich, J.; Tian, Y.; Perera, D.; Lemm, D.; Schwarz, P.; Armulik, A.; Browning, J.L.; Tallquist, M.; et al. Follicular Dendritic Cells Emerge from Ubiquitous Perivascular Precursors. Cell 2012, 150, 194–206. [Google Scholar] [CrossRef] [Green Version]
- Pasparakis, M.; Alexopoulou, L.; Episkopou, V.; Kollias, G. Immune and Inflammatory Responses in TNF Alpha-Deficient Mice: A Critical Requirement for TNF Alpha in the Formation of Primary B Cell Follicles, Follicular Dendritic Cell Networks and Germinal Centers, and in the Maturation of the Humoral Immune Response. J. Exp. Med. 1996, 184, 1397–1411. [Google Scholar] [CrossRef]
- Huang, L.-H.; Melton, E.M.; Li, H.; Sohn, P.; Jung, D.; Tsai, C.-Y.; Ma, T.; Sano, H.; Ha, H.; Friedline, R.H.; et al. Myeloid-Specific Acat1 Ablation Attenuates Inflammatory Responses in Macrophages, Improves Insulin Sensitivity, and Suppresses Diet-Induced Obesity. Am. J. Physiol.-Endocrinol. Metab. 2018, 315, E340–E356. [Google Scholar] [CrossRef] [Green Version]
- Melton, E.M.; Li, H.; Benson, J.; Sohn, P.; Huang, L.-H.; Song, B.-L.; Li, B.-L.; Chang, C.C.Y.; Chang, T.-Y. Myeloid Acat1/Soat1 KO Attenuates pro-Inflammatory Responses in Macrophages and Protects against Atherosclerosis in a Model of Advanced Lesions. J. Biol. Chem. 2019, 294, 15836–15849. [Google Scholar] [CrossRef]
- Wu, N.; Li, R.-Q.; Li, L. SOAT1 Deficiency Attenuates Atherosclerosis by Regulating Inflammation and Cholesterol Transportation via HO-1 Pathway. Biochem. Biophys. Res. Commun. 2018, 501, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Eum, J.Y.; Lee, J.C.; Yi, S.S.; Kim, I.Y.; Seong, J.K.; Moon, M.H. Aging-Related Lipidomic Changes in Mouse Serum, Kidney, and Heart by Nanoflow Ultrahigh-Performance Liquid Chromatography-Tandem Mass Spectrometry. J. Chromatogr. A 2020, 1618, 460849. [Google Scholar] [CrossRef]
- Rampanelli, E.; Ochodnicky, P.; Vissers, J.P.; Butter, L.M.; Claessen, N.; Calcagni, A.; Kors, L.; Gethings, L.A.; Bakker, S.J.; de Borst, M.H.; et al. Excessive Dietary Lipid Intake Provokes an Acquired Form of Lysosomal Lipid Storage Disease in the Kidney. J. Pathol. 2018, 246, 470–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, G.W.; Hill, D.G.; Jones, S.A. Understanding Immune Cells in Tertiary Lymphoid Organ Development: It Is All Starting to Come Together. Front. Immunol. 2016, 7, 401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lei, L.; Xiong, Y.; Chen, J.; Yang, J.-B.; Wang, Y.; Yang, X.-Y.; Chang, C.C.Y.; Song, B.-L.; Chang, T.-Y.; Li, B.-L. TNF-Alpha Stimulates the ACAT1 Expression in Differentiating Monocytes to Promote the CE-Laden Cell Formation. J. Lipid Res. 2009, 50, 1057–1067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, J.-B.; Duan, Z.-J.; Yao, W.; Lee, O.; Yang, L.; Yang, X.-Y.; Sun, X.; Chang, C.Y.; Chang, T.-Y.; Li, B.-L. Synergistic Transcriptional Activation of HumanAcyl-Coenzyme A: Cholesterol Acyltransterase-1 Gene by Interferon-γ and All-Trans-Retinoic Acid THP-1 Cells. J. Biol. Chem. 2001, 276, 20989–20998. [Google Scholar] [CrossRef] [Green Version]
- Hori, M.; Miyazaki, A.; Tamagawa, H.; Satoh, M.; Furukawa, K.; Hakamata, H.; Sasaki, Y.; Horiuchi, S. Up-Regulation of Acyl-Coenzyme A: Cholesterol Acyltransferase-1 by Transforming Growth Factor-Β1 during Differentiation of Human Monocytes into Macrophages. Biochem. Biophys. Res. Commun. 2004, 320, 501–505. [Google Scholar] [CrossRef]
- Lin, H.-J.; Lin, C.-W.; Mersmann, H.J.; Ding, S.-T. Sterol-O Acyltransferase 1 Is Inhibited by Gga-MiR-181a-5p and Gga-MiR-429-3p through the TGFβ Pathway in Endodermal Epithelial Cells of Japanese Quail. Comp. Biochem. Physiol. Part B Biochem. Mol. Biol. 2020, 240, 110376. [Google Scholar] [CrossRef]
- Lan, H.Y. Diverse Roles of TGF-β/Smads in Renal Fibrosis and Inflammation. Int. J. Biol. Sci. 2011, 7, 1056–1067. [Google Scholar] [CrossRef] [Green Version]
- Delsing, D.J.M.; Offerman, E.H.; van Duyvenvoorde, W.; van der Boom, H.; de Wit, E.C.M.; Gijbels, M.J.J.; van der Laarse, A.; Jukema, J.W.; Havekes, L.M.; Princen, H.M.G. Acyl-CoA: Cholesterol Acyltransferase Inhibitor Avasimibe Reduces Atherosclerosis in Addition to Its Cholesterol-Lowering Effect in ApoE*3-Leiden Mice. Circulation 2001, 103, 1778–1786. [Google Scholar] [CrossRef]
- Shibuya, Y.; Niu, Z.; Bryleva, E.Y.; Harris, B.T.; Murphy, S.R.; Kheirollah, A.; Bowen, Z.D.; Chang, C.C.Y.; Chang, T.-Y. Acyl-CoA: Cholesterol Acyltransferase 1 Blockage Enhances Autophagy in the Neurons of Triple Transgenic Alzheimer’s Disease Mouse and Reduces Human P301L-Tau Content at the Pre-Symptomatic Stage. Neurobiol. Aging 2015, 36, 2248–2259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casemayou, A.; Fournel, A.; Bagattin, A.; Schanstra, J.; Belliere, J.; Decramer, S.; Marsal, D.; Gillet, M.; Chassaing, N.; Huart, A.; et al. Hepatocyte Nuclear Factor-1 β Controls Mitochondrial Respiration in Renal Tubular Cells. JASN 2017, 28, 3205–3217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nevers, T.; Salvador, A.M.; Velazquez, F.; Ngwenyama, N.; Carrillo-Salinas, F.J.; Aronovitz, M.; Blanton, R.M.; Alcaide, P. Th1 Effector T Cells Selectively Orchestrate Cardiac Fibrosis in Nonischemic Heart Failure. J. Exp. Med. 2017, 214, 3311–3329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Ducasa, G.M.; Mallela, S.K.; Kim, J.-J.; Molina, J.; Mitrofanova, A.; Wilbon, S.S.; Ge, M.; Fontanella, A.; Pedigo, C.; et al. Sterol-O-Acyltransferase-1 Has a Role in Kidney Disease Associated with Diabetes and Alport Syndrome. Kidney Int. 2020, 98, 1275–1285. [Google Scholar] [CrossRef]
- Meuwese, M.C.; de Groot, E.; Duivenvoorden, R.; Trip, M.D.; Ose, L.; Maritz, F.J.; Basart, D.C.G.; Kastelein, J.J.P.; Habib, R.; Davidson, M.H.; et al. ACAT Inhibition and Progression of Carotid Atherosclerosis in Patients with Familial Hypercholesterolemia: The Captivate Randomized Trial. JAMA 2009, 301, 1131–1139. [Google Scholar] [CrossRef]
- Nissen, S.E.; Sipahi, I.; Schoenhagen, P.; Crowe, T.D.; Wisniewski, L.M.; Kassalow, L.M. Effect of ACAT Inhibition on the Progression of Coronary Atherosclerosis. N. Engl. J. Med. 2006, 354, 1253–1263. [Google Scholar] [CrossRef]
- Tardif, J.-C.; Grégoire, J.; L’Allier, P.L.; Anderson, T.J.; Bertrand, O.; Reeves, F.; Title, L.M.; Alfonso, F.; Schampaert, E.; Hassan, A.; et al. Effects of the Acyl Coenzyme A:Cholesterol Acyltransferase Inhibitor Avasimibe on Human Atherosclerotic Lesions. Circulation 2004, 110, 3372–3377. [Google Scholar] [CrossRef] [Green Version]
- Naoe, S.; Tsugawa, H.; Takahashi, M.; Ikeda, K.; Arita, M. Characterization of Lipid Profiles after Dietary Intake of Polyunsaturated Fatty Acids Using Integrated Untargeted and Targeted Lipidomics. Metabolites 2019, 9, 241. [Google Scholar] [CrossRef] [Green Version]
- Tsugawa, H.; Ikeda, K.; Takahashi, M.; Satoh, A.; Mori, Y.; Uchino, H.; Okahashi, N.; Yamada, Y.; Tada, I.; Bonini, P.; et al. A Lipidome Atlas in MS-DIAL 4. Nat. Biotechnol. 2020, 38, 1159–1163. [Google Scholar] [CrossRef]
- Saeed, A.I.; Sharov, V.; White, J.; Li, J.; Liang, W.; Bhagabati, N.; Braisted, J.; Klapa, M.; Currier, T.; Thiagarajan, M.; et al. TM4: A Free, Open-Source System for Microarray Data Management and Analysis. BioTechniques 2003, 34, 374–378. [Google Scholar] [CrossRef]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An Open-Source Platform for Biological-Image Analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ariyasu, Y.; Sato, Y.; Isobe, Y.; Taniguchi, K.; Yanagita, M.; Arita, M. Sterol O-Acyltransferase Inhibition Ameliorates High-Fat Diet-Induced Renal Fibrosis and Tertiary Lymphoid Tissue Maturation after Ischemic Reperfusion Injury. Int. J. Mol. Sci. 2022, 23, 15465. https://doi.org/10.3390/ijms232415465
Ariyasu Y, Sato Y, Isobe Y, Taniguchi K, Yanagita M, Arita M. Sterol O-Acyltransferase Inhibition Ameliorates High-Fat Diet-Induced Renal Fibrosis and Tertiary Lymphoid Tissue Maturation after Ischemic Reperfusion Injury. International Journal of Molecular Sciences. 2022; 23(24):15465. https://doi.org/10.3390/ijms232415465
Chicago/Turabian StyleAriyasu, Yuki, Yuki Sato, Yosuke Isobe, Keisuke Taniguchi, Motoko Yanagita, and Makoto Arita. 2022. "Sterol O-Acyltransferase Inhibition Ameliorates High-Fat Diet-Induced Renal Fibrosis and Tertiary Lymphoid Tissue Maturation after Ischemic Reperfusion Injury" International Journal of Molecular Sciences 23, no. 24: 15465. https://doi.org/10.3390/ijms232415465
APA StyleAriyasu, Y., Sato, Y., Isobe, Y., Taniguchi, K., Yanagita, M., & Arita, M. (2022). Sterol O-Acyltransferase Inhibition Ameliorates High-Fat Diet-Induced Renal Fibrosis and Tertiary Lymphoid Tissue Maturation after Ischemic Reperfusion Injury. International Journal of Molecular Sciences, 23(24), 15465. https://doi.org/10.3390/ijms232415465




