This article describes a case of successful TORD and simultaneous reconstruction using condylar reconstruction plate with iliac crest free bone graft.
Operative Procedure
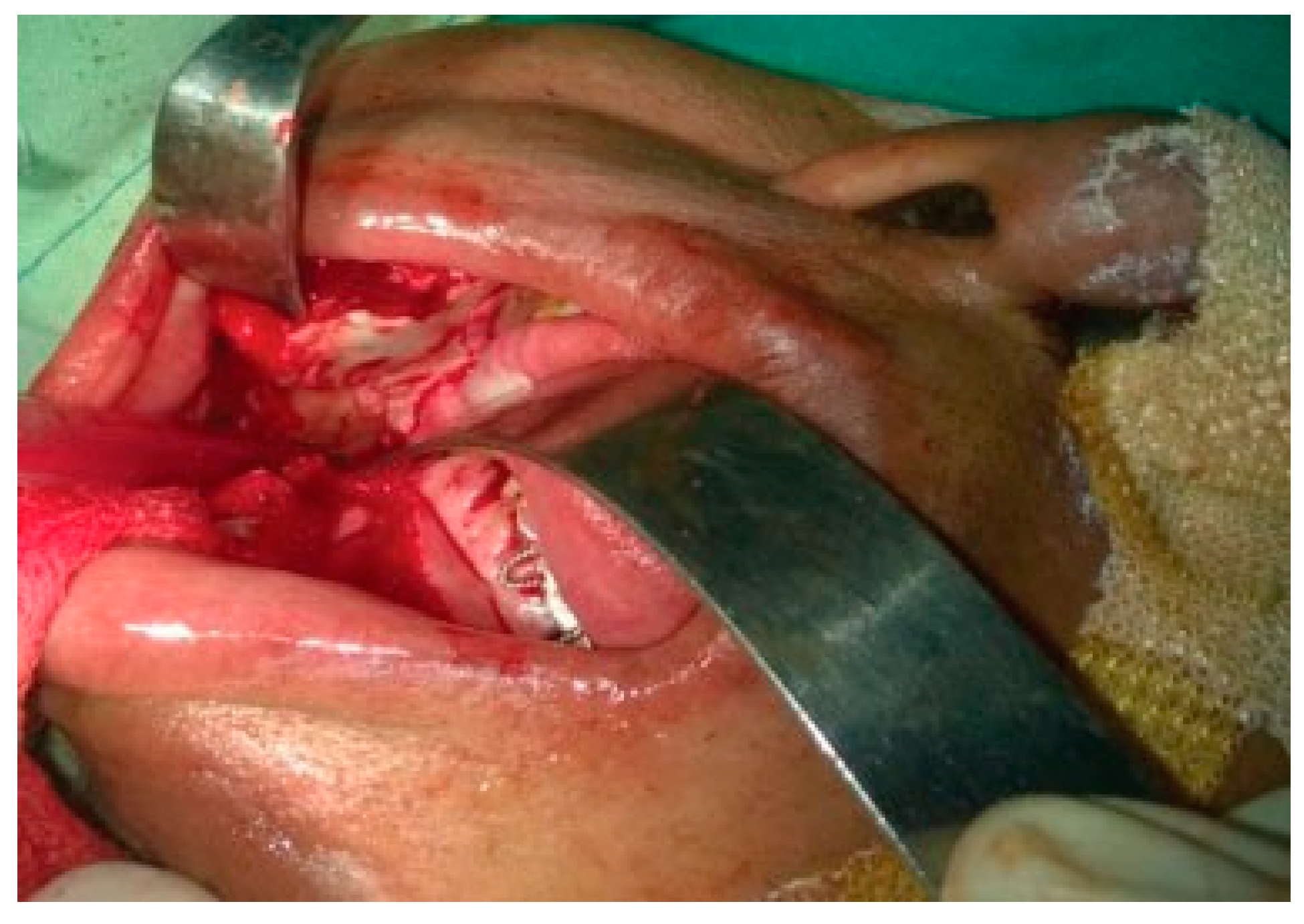
A transoral vestibular incision was given extending from left canine region to the entire right canine and body region of the mandible and extending upward along the anterior border of the ramus till the level of upper molars on the right side (
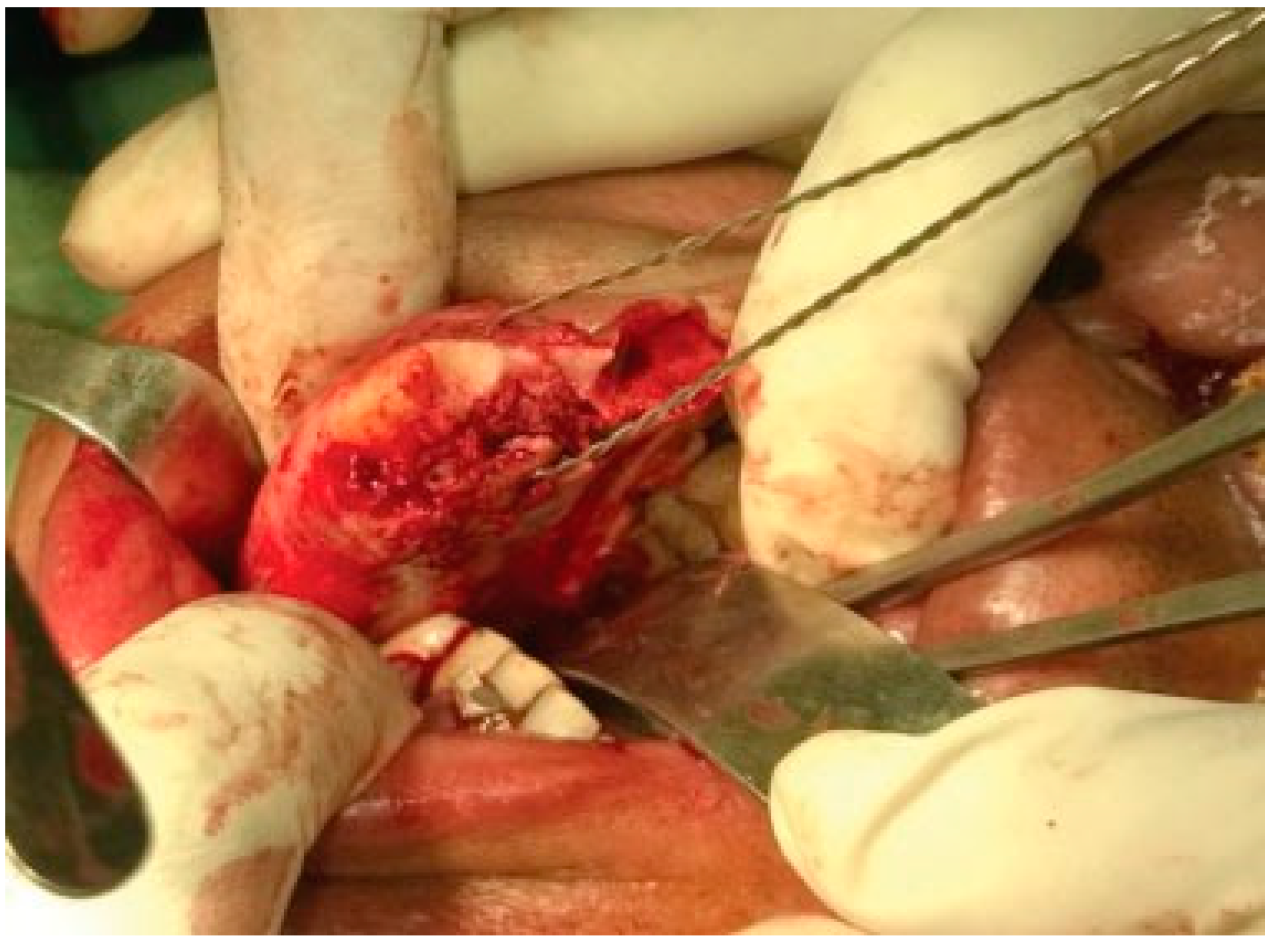
Figure 4). Lateral aspect of the entire mandible was exposed till the ramus. Osteotomy was performed between the right lateral incisor and canine to fracture the mandible. The fractured mandible was swung laterally to expose the lingual side to facilitate subperiosteal exposure of the medial side of the fractured mandible (
Figure 5). Posteriorly, the inferior alveolar neurovascular bundle was identified, clamped and ligated before severing it at its entry into the mandibular canal, progressing along the medial surface of ramus detaching the medial pterygoid muscle. A hole was then drilled onto the anterior aspect of fractured mandibular segment and a twisted wired was passed through to assist anterolateral traction for disarticulation (
Figure 6). Under traction, the temporalis fibers were detached from the coronoid process and similarly the condyle was freed from capsular attachment to facilitate its disarticulation. The segment of the mandible along with the condylar and coronoid process on the right side till the fractured area was successfully removed transorally (
Figure 7). The bleeders were identified and ligated and the wound was packed with wet gauge to arrest oozing of the blood from the adjacent soft tissues.
Figure 1.
Frontal view showing mild swelling in the right body region of the mandible.
Figure 1.
Frontal view showing mild swelling in the right body region of the mandible.
Figure 2.
Submandibular view showing mandibular swelling.
Figure 2.
Submandibular view showing mandibular swelling.
Figure 3.
Orthopantomogram showing a large multilocular radiolucent lesion with well-defined border and involving the entire right side of the body and ramus of the mandible.
Figure 3.
Orthopantomogram showing a large multilocular radiolucent lesion with well-defined border and involving the entire right side of the body and ramus of the mandible.
Figure 4.
Transoral vestibular incision.
Figure 4.
Transoral vestibular incision.
Figure 5.
Subperiosteal exposure of the medial side of the fractured mandible.
Figure 5.
Subperiosteal exposure of the medial side of the fractured mandible.
Figure 6.
Twisted wired passed through the fractured segment to assist anterolateral traction for disarticulation.
Figure 6.
Twisted wired passed through the fractured segment to assist anterolateral traction for disarticulation.
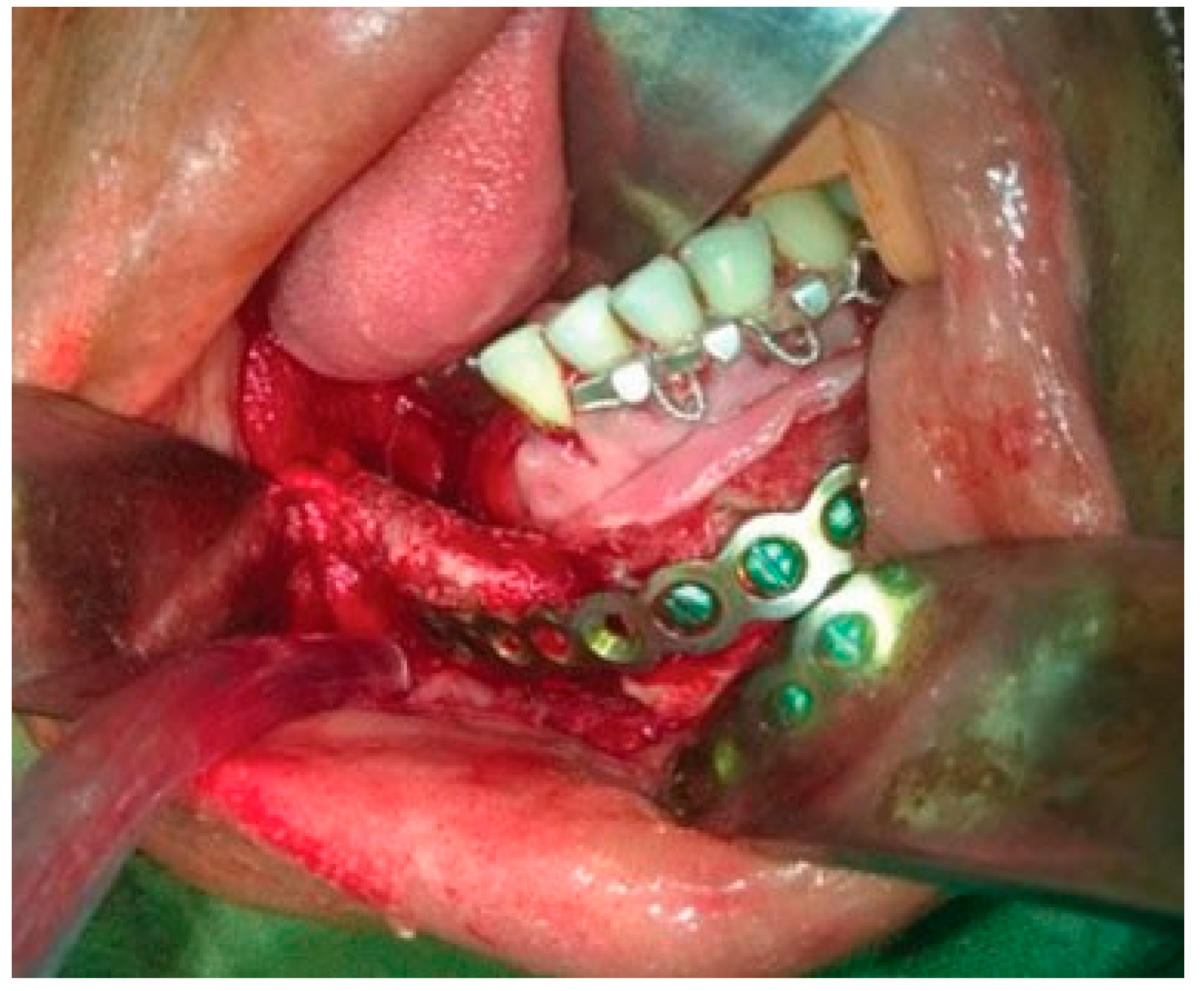
A reconstruction plate was then contoured along the resected mandible and fixed to the anterior region of the mandible with the help of five bicortical screws. A 5 cm × 2 cm cortico-cancellous bone graft was then harvested from the iliac crest to reconstruct the resected body of the mandible (
Figure 8). A double-layer closure of the wound was done to obtain watertight closure.
Postoperative recovery was fast and uneventful. As the swelling subsided gradually during the postoperative phase, excellent symmetry of the face was observed. Although the postoperative orthopantomogram (OPG) revealed that the condylar head of the plate was placed away from the glenoid fossa (
Figure 9), the occlusion was intact with minor deviation of the jaw toward the resected side during mouth opening at the 6-month follow-up (
Figure 10). Postoperative follow-up at 6 months shows appreciable facial harmony and maintenance of perioral musculature (
Figure 11).
Figure 7.
Resected specimen.
Figure 7.
Resected specimen.
Figure 8.
Reconstruction with condylar reconstruction plate and corticocancellous bone graft.
Figure 8.
Reconstruction with condylar reconstruction plate and corticocancellous bone graft.
Figure 9.
One-year postoperative orthopantomogram.
Figure 9.
One-year postoperative orthopantomogram.
Discussion
Maximum success in skeletal surgery depends on adequate access to and exposure of the skeleton. Skeletal surgery is simplified and expedited when the involved parts are sufficiently exposed. Incisions are usually placed very near to the area of interest, while major nerves and blood vessels are retracted [
3].
Figure 10.
Postoperative occlusion.
Figure 10.
Postoperative occlusion.
Figure 11.
Postoperative photograph showing appreciable facial harmony and maintenance of perioral musculature.
Figure 11.
Postoperative photograph showing appreciable facial harmony and maintenance of perioral musculature.
Many approaches to a given skeletal region are possible and the choice is usually based on surgeons’ training, experience, and bias [
3].
Ellis and Zide have highlighted three important differences in placing an incision on the facial region as compared with other parts of the body [
3]:
The primary factor in incision placement is not surgical convenience but facial esthetics.
Presence of the muscles and nerve (cranial nerve VII) of facial expression.
Presence of many important sensory nerves exiting the skull at multiple locations.
Consideration of these differences had led to innovation of various incisions to approach the mandible for surgical exploration.
Surgical exposure of the mandible can be done through extraoral or intraoral approach depending on the site and area of exposure required for the surgical procedure.
In intraoral approach, the greatest benefit to the patient is the hidden intraoral scar in contrast to extraoral approach. Although access is limited in some regions, such as the lower border of the mandible at the angle and parts of the ramus, the approach is also relatively rapid and simple. Complications are few but include mental nerve damage and lip malposition, both of which are minimized with proper technique.
In extraoral approach, the mandible can be exposed by surgical approaches using incisions placed on the skin of the face. The position of the incision and anatomy vary according to the region of the mandible approached.
Extraoral approaches to the mandibular condyle region can be divided into three major categories in terms of the height of the approach: high, middle, and low [
4].
High approach, involving the preauricular and perilobular approach, has been applied to the reduction of high condylar neck or condylar head fractures. Very good camouflaged scar and clearer direct exposure are the advantages of these approaches.
Disadvantages include mild neuropraxia up to 13 months and in case of transparotid approach, postoperative sialoceles and salivary fistulas can be a nuisance [
5].
Middle height approaches, retromandibular approach, allows identification of the buccal and marginal mandibular branches of the facial nerve and avoid possible facial nerve damage; however, retraction of the parotid gland may lead to facial nerve injury [
6].
Low height approach is also known as Risdon approach. In this approach, the marginal mandibular nerve is identified easily without much dissection, and if a flap is elevated, including the nerve, there is no risk of facial nerve damage [
7]. The extraoral approach has some advantages, specifically ease of reduction under good visibility. However, this method leaves a facial scar and has the potential to cause facial nerve damage [
8].
Transoral resection and reconstruction was first reported by Givol et al [
1]. following Myers’ principal: “secondary cosmetic deformities should be avoided unless no other alternative is satisfactory in the situation” [
9]. They have reported resection of anterior mandible and immediate microvascular reconstruction with fibular graft and have laid down criteria for patient selection that includes “resection should be limited to intermolar area.” In our case, however, anterior as well as the ramus of the mandible was involved in the pathology and therefore required resection of the part of parasymphyseal region along with entire body and ramus including the condylar and coronoid process.
Myers has extensively enumerated upon principles of reconstructive surgery, [
9]. wherein he has emphasized that approach used should not limit or interfere with the extirpative procedure. TORD can be successfully accomplished in any patient with benign pathological lesion of the mandible without cortical perforation, as after osteotomy the desired segment can be adequately mobilized to permit subperiosteal dissection of the entire lateral aspect of the mandible till the coronoid process and on the medial aspect also subperiosteal dissection till the inferior attachment of the capsular ligament of the condylar process can be effectively carried out. The inferior alveolar neurovascular bundle can also be effectively identified for ligation. Inferior traction of the osteotomized segment permits sharp incision on the inferior aspect of the capsular ligament for successful disarticulation.
Subperiosteal dissection provides a relative safety for the major vessels in the vicinity but still poses significant chances of injury to maxillary artery specially during sharp dissection of the temporomandibular joint (TMJ) capsule while disarticulating; hence, we recommend placement of condylar retractor on the medial aspect of the condyle while disarticulating. Bleeding from other potential sources such as pterygoid venous plexus, retro mandibular vein, and specially capillary bleed from vessels entering the bone from the periosteum can also add to surgical difficulty because of limited access and difficulty in ligation. Although most of the bleeding can effectively be controlled by hypotensive anesthesia and pressure packing, measures such as external carotid artery ligation may need to be considered in case of a dire need. Transoral approach, in our experience, does not restrict adequate dissection or resection and disarticulation.
Early restoration of form and function after ablative surgery is also possible via transoral approach, as it preserves the contour of the facial skin and function of the perioral musculature. The resected mandible can be used as a template (in the absence of stereolithographic model) for contouring of the reconstruction plate, which can be used for reconstruction with or without bone grafts; however, it has to be borne in mind that contouring of plate on the resected bony segment can often lead to suboptimal contouring leading to improper alignment with the remaining bone and could be attributed to the displaced condylar head of the reconstruction plate in our case. Even in absence of bone grafts, the reconstruction plate provides enough support to the overlying structures for maintenance of facial form and proportions. In our case, the reconstruction plate was augmented with nonvascularized autogenous iliac graft to maintain the facial form. One study claims that under ideal conditions, 100% of nonvascularized grafts will take, [
10]. while others indicate that nonvascularized grafting can provide a better bulk of bone for implant placement and the contour may be more satisfactory because there are few limits to the quantity of nonvascularized bone that can be inserted and the ability to shape it to the mandible. However, it undergoes considerable remodeling after placement, which means that implants can only be inserted with reliability once the remodeling has ceased. The failure rate for the nonvascularized graft increases for those longer than 6 cm, and the procedure should be done with extreme caution in defects exceeding 9 cm in length. Additionally, nonvascularized grafts offer considerable savings in terms of days in hospital and hours in the operating room and therefore has considerable financial advantage [
11,
12]. Vascularized grafts also requires an advanced operating facility and specialized skill, a combination which is difficult and expensive to find in developing nations with poor population. Hence, in spite of the fact that reconstruction done in this case cannot be labeled as optimal, nonvascularized iliac graft was the only choice we had for this patient. One-year follow-up of the patient shows excellent uptake of the graft, but functional rehabilitation with implant-supported prosthesis still remains questionable with conventional dental implants.
Akinmoladun et al, in an analysis of 20 cases of condylar disarticulation followed by reconstruction with autogenous nonvascularized iliac crest bone graft, have also mentioned that poor resource practice and cost continue to constitute barriers against optimum reconstruction of patients who undergo major ablative surgery involving the joint [
13].
Fixation of the reconstruction plate in the remaining anterior region of the mandible can also be accomplished effectively, transorally. Hence, quick and simple reconstruction is also achieved, fulfilling Myers’ criteria for ablative surgery.
The concern for surgical morbidity is also addressed, as most of the dissection is performed under safety of periosteal curtain, thereby eliminating or minimizing the chances of injury to adjacent vital structures.
Carlson [
14]. has highlighted three major postoperative complications occurring with reconstruction plate after disarticulation resection:
Facial nerve palsy resulting because of inferior and lateral dislocation of the plate, thereby resulting in compression of the main trunk of facial nerve
Displacement of condylar prosthesis into the middle cranial fossa
Cutaneous exposure of the reconstruction bone plate in a patient who received external beam radiation therapy after surgery
Liu et al did a retrospective analysis of 660 patients who received primary reconstruction of the mandible and reported the total complication rate as 14.7% (97/660), which included screw loosening 5.8% (38/660), plate fracture 3.3% (22/660), plate exposure 3.8% (25/660), infection 7.4% (49/660), and malunion or nonunion 2.9% (19/660). The mandibular defects reconstructed by reconstructive plates had a higher complication rate than that by bone grafts. The complications were associated with radiation therapy and diabetes. Radiation therapy had a significant effect on plate exposure [
15].
In more than a year of follow-up, our patient showed no signs of any adverse morbidity in addition to slight deviation of the jaw toward the operated side during mouth opening. Other possible complications such as screw loosening and plate fracture were also not observed in 1 year follow-up of the patient and could be attributed to the reason that the resected side was devoid of any functional loading and the plate was fixed with five bicortical screws to the healthy bone. The traditional approach for a mandibulectomy is associated with troublesome esthetic sequela including disfiguring scars, lip vermilion notching, and loss of chin pad contour [
16].
The advantages of TORD are as follows [
2]:
Possibility of removing and repositioning of the mandible intraorally
No facial scar
Both removal of lesion and reconstruction procedure simultaneously result in better healing
Make more ideal contour of face
No damage to facial vein and artery, and less bleeding and hematoma
No damage to marginal mandibular nerve that innervate lips
Adaptation of the plate provides a better condylar position
Transoral mandibular resection with disarticulation and immediate nonvascularized grafting may not seem to be an optimal procedure in terms of reconstruction, but appears to be a good alternative in limited resources as it bears a significant advantage of scarless surgery along with preservation of vital structure.
Encouraging results and convenience of the procedure prompted us to document this case so that more input from various surgeons can be gathered to conclusively establish the efficacy, limitations, and possible complications of TORD.