Cervicomediastinal emphysema (CME) clinically manifests as palpable neck and chest subcutaneous crepitus, swelling and pain in the neck and chest, dyspnea, and a sore throat. Traumatic CME results from the entry and spread of air into the soft tissues of the neck and chest. These two anatomical areas communicate via fascial spaces. The fascial spaces are a conduit for the spread of pathology (e.g., infection, blood, and air) between the neck and chest [
1,
2].
There are several ways air can enter the soft tissues in this anatomical region in the trauma setting. Air may enter externally via penetrating injuries (e.g., missile-type injuries from gunshot wounds) or closed nonpenetrating external neck injuries (e.g., strangulation, blunt neck trauma). Air from the aerodigestive tract may leave and enter the neck or chest if there has been intraluminal violation (e.g., perforated viscus from traumatic endotracheal intubations, esophagoscopies, and ingestion of sharp foreign bodies). Air may be iatrogenically introduced into the tissues of the head and neck from the thorax (e.g., from excessive positive pressure ventilation and barotrauma) or peritoneum (e.g., from abdominal laparoscopic procedures that employ gas insufflation) [
1,
2,
3,
4].
Air descending into the neck and mediastinum originating from the orofacial region has been reported less frequently. CME as a result of dental procedures has been associated with powered handpieces, such as high-speed drills and air–water dental syringes [
3]. Air from the working end of the handpiece enters the oral tissues surrounding the dentition and spreads into the neck and chest. CME has been associated with traumatic facial fractures, such as maxillary, orbital wall, and mandible fractures [
4,
5]. The common setting by which these fractures create CME is a forceful blunt blow to the face with the bony defect communicating with one of the pneumatized paranasal sinuses. A proposed ball-valve effect at the fracture site by which air only exits unidirectionally into the soft tissues or subsequent Valsalva or nose blowing may be responsible mechanisms for CME [
4].
We report a case of a high-velocity impact injury to the mastoid bone from a batted baseball. The pneumatized spaces of the mastoid bone were disrupted with subsequent pneumodissection down both sides of the neck and mediastinum.
Case Report
An 18-year-old male was struck with a batted baseball to the right mastoid during a recreational baseball game. He presented to the emergency room immediately after the accident for further evaluation. By report, he did not have any bloody right otorrhea. He denied any hearing loss, dizziness, dysphagia, dyspnea, or chest pain. He denied any vigorous nose blowing. He did not lose consciousness; he only described himself as being in a “daze.”
Physical examination result was significant for palpable tenderness at the right mastoid tip, palpable crepitus overlying the right mastoid process and right lateral neck, and mild right external auditory canal erythema. Physical examination did not reveal any focal neurologic findings or deficits. Right facial nerve function was normal and symmetric (HouseBrackmann grade I). The right tympanic membrane was intact and no hemotympanum was visualized.
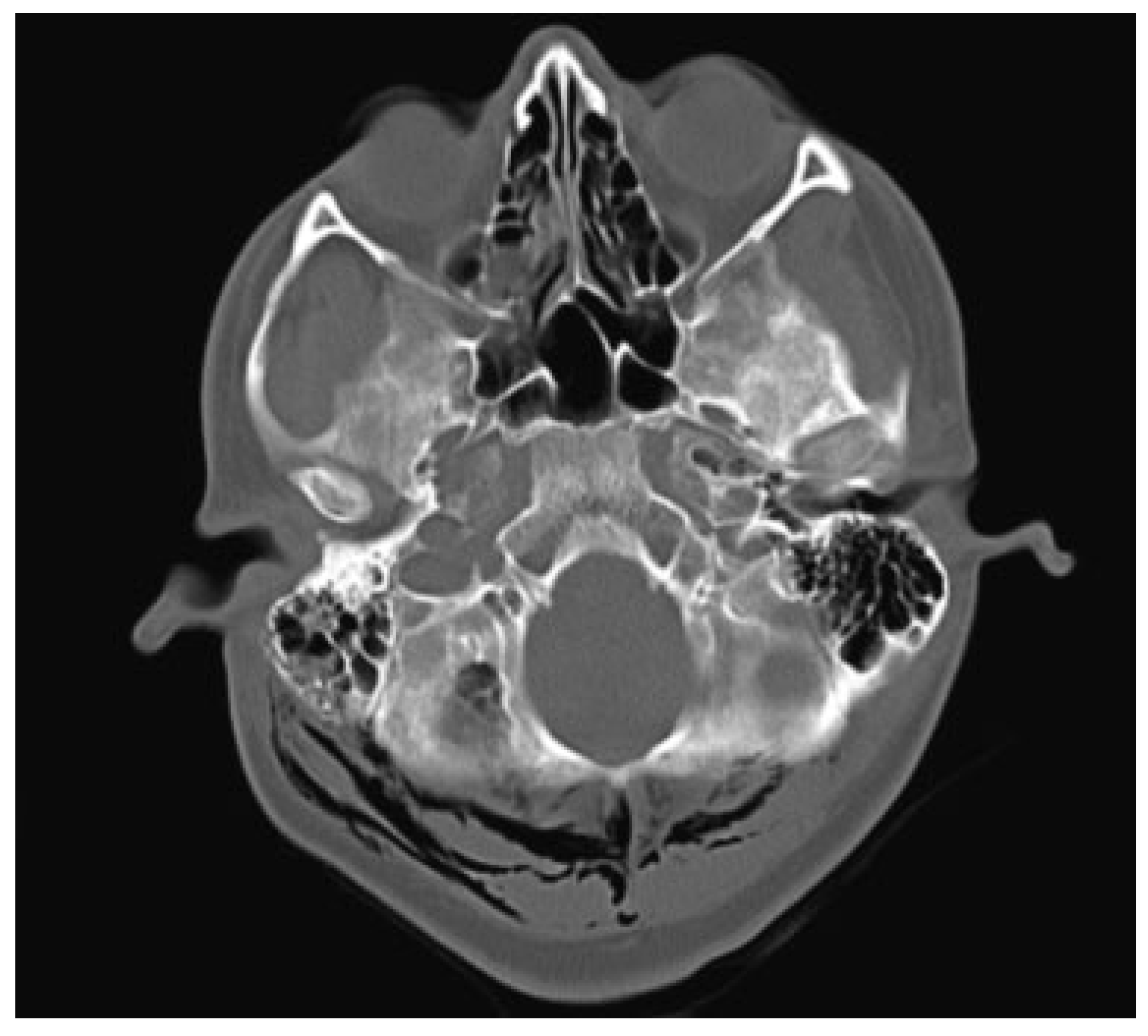
Head computed tomographic (CT) scan did not demonstrate intracranial injury. There was no midline shift or mass effect on the brain. It did demonstrate a right mastoid bone fracture with extensive soft-tissue gas along the skull base and surrounding cervical emphysema (
Figure 1).
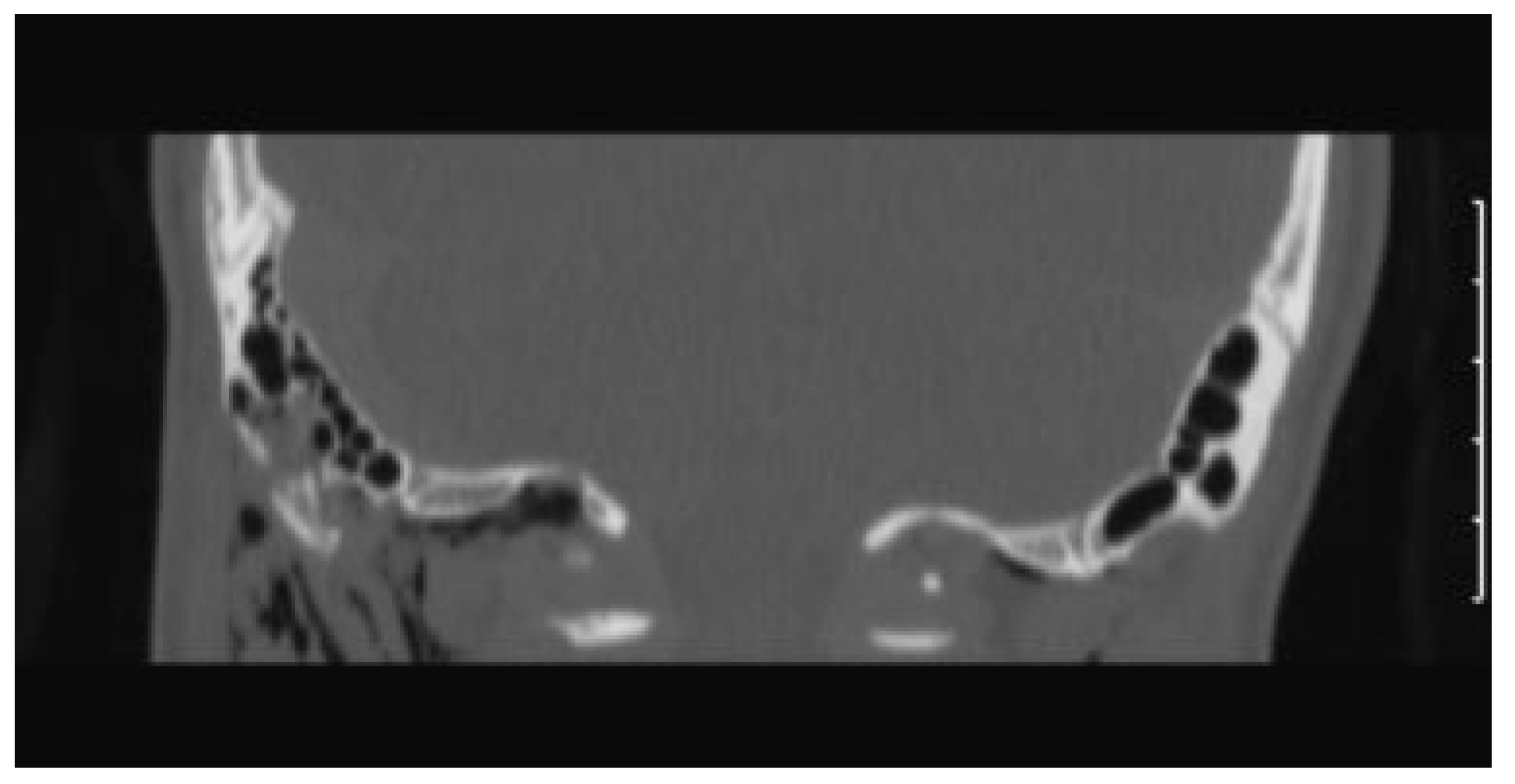
Temporal bone CT scan confirmed the presence of an isolated right comminuted mastoid process fracture with extensive right cervical emphysema extending from the fracture to involve the skull base, cervical soft tissues bilaterally, and adjacent musculature (
Figure 2). There was opacification of the mastoid air cells surrounding the fracture lines. There was no violation of the otic capsule and ossicular alignment was normal.
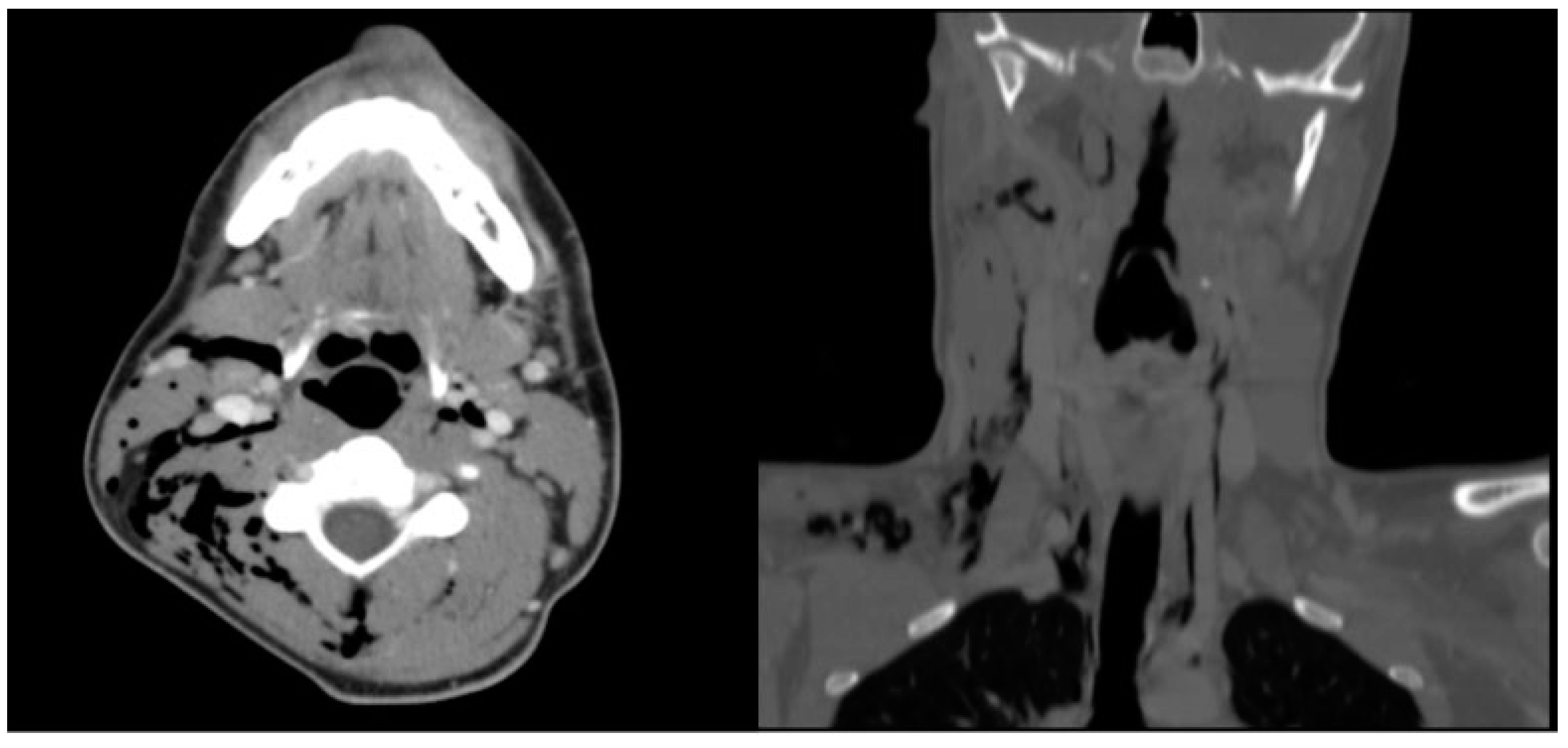
Neck CT scan revealed extensive subcutaneous and deep cervical emphysema extending from the posterior occiput caudally into the superior mediastinum. The air extended into the parapharyngeal spaces, bilateral carotid spaces, and intramuscularly into the right sternocleidomastoid muscle (
Figure 3).
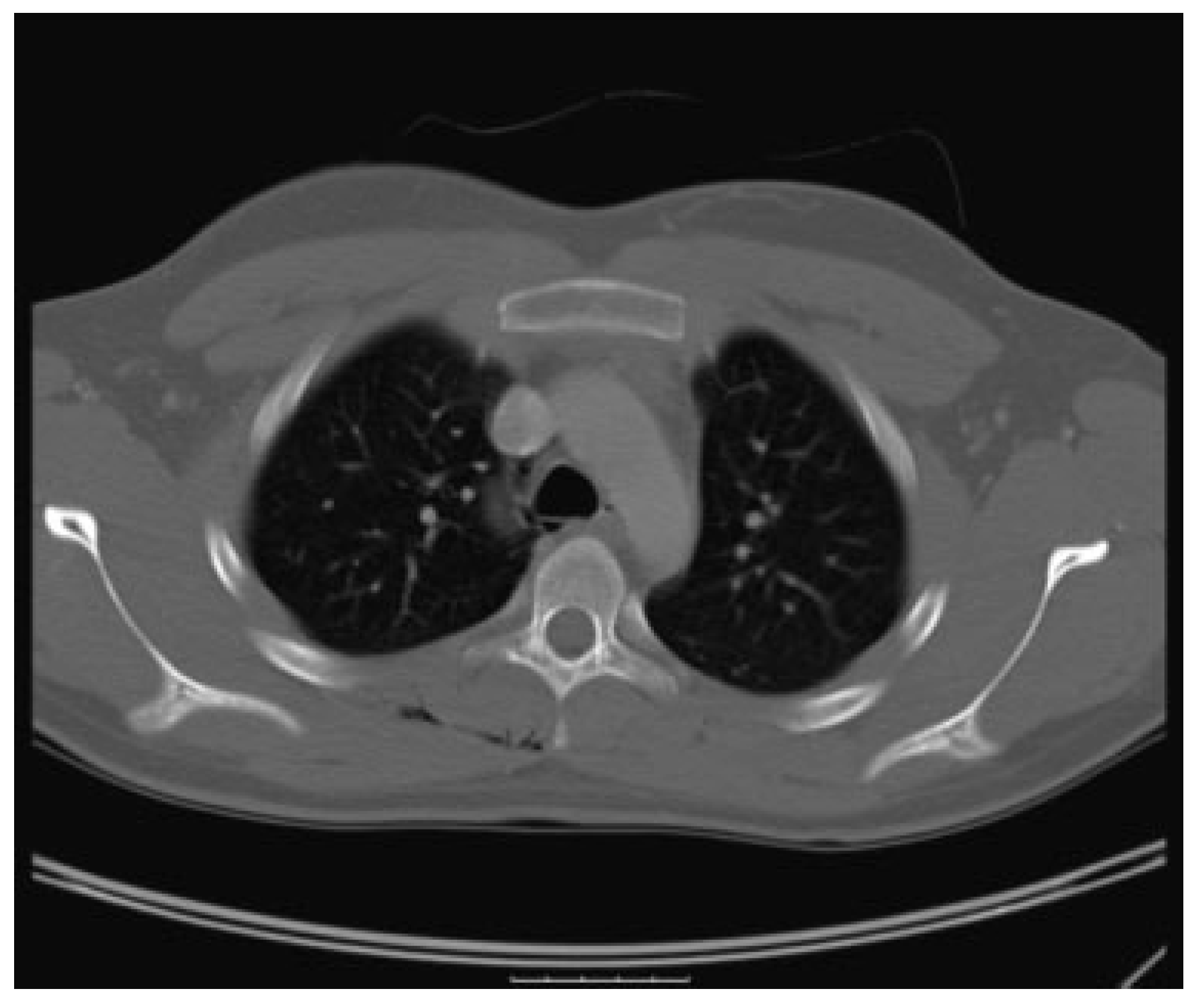
Chest CT scan demonstrated inferior extension of the softtissue air into the superior mediastinum and right posterior upper chest wall (
Figure 4).
The patient was observed in the emergency room for several hours without change in his overall condition. His vital signs remained normal and stable. At 1-week outpatient otolaryngologic follow-up, he was asymptomatic and demonstrated no sequelae from the injury.
Discussion
The focus of this report is the posttraumatic spread of subcutaneous air originating from the mastoid bone into the mediastinum. The clinical presentation of an isolated mastoid fracture leading to CME has only been reported once before this study [
6]. In that case, a patient was kicked in the mastoid several times and this resulted in a linear closed fracture of the mastoid. The authors attributed the source of the air from the patient’s self-induced Valsalva maneuvers that forced air out beyond the fracture.
This present case features a rare injury—a high velocity, focal impact to the mastoid bone that resulted in a comminuted fracture of the mastoid. The impact likely displaced the mastoid air into the soft tissues. The air exited with sufficient force to dissect through the fascial planes and even into the attached musculature. Entry of air from the mastoid to the mediastinum assumed a path along the surrounding myofascial planes. The soft-tissue neck CT scan demonstrates air dissecting from the mastoid across the posterior nuchal musculature to the prevertebral fascial space to the contralateral carotid sheath. When the air is followed inferiorly, it tracks into the right parapharyngeal space and bilateral carotid sheaths to enter the mediastinum.
The amount and extent of subcutaneous air was greater in this present case. Several factors may be responsible for this finding. It may be attributed to the severity of the injury. Injuries caused by batted baseballs can be catastrophic such as impact to the head, trachea and chest, the latter leading to death from blunt precordial trauma resulting in cardiac arrhythmia (commotio cordis) [
7]. Additionally, a larger amount of air may have exited the mastoid because of a larger bony defect. While the previously reported case described a linear fracture, the fracture in this present case was comminuted. Therefore, with a larger bony defect, there would be multiple areas of potential air egress.
It has been hypothesized that the mastoid air cells system (MACS), with its intricate honeycomb pattern of aerated spaces, may serve as protective cushioning to the otic capsule, facial nerve, and brain [
8]. The situation is similar to shock absorbing properties of the paranasal sinuses. In a study looking at the fracture characteristics in temporal bones subjected to lateral trauma from a 9-kg pendulum swinging at 3.35 m/second (7.5 mile/hour), there was more injury in the temporal bones which had the MACS exenterated and filled with a solid material when compared with well-pneumatized control temporal bones [
8]. Fractures of the facial canal, carotid canal, and jugular foramen were more frequent in the de-pneumatized and solid-filled temporal bones compared with the control group. Although direct comparison between this study and our case cannot be made, a baseball typically weighs 5.25 ounces (0.15 kg) and its batted speed can reach up to 100 mile/hour. The degree of mastoid pneumatization in our case was extensive, degree IV based on temporal pneumatization classification by Han et al. [
9]. Our patient did not have any injury to the facial canal or otic capsule nor did he clinically present with any facial weakness, hearing loss, or vertigo from the trauma. This demonstrates the protective effects of a well-aerated MACS.
In summary, this unusual case presents several clinical highlights. In the setting of traumatic CME, both ascending and descending sources of air entry into the neck and mediastinum must be considered. A fractured mastoid should be added to the list of descending sources of air into the mediastinum. In our case, the air originated from the pneumatized spaces of the mastoid that was forced out from the impact. Further contribution of the soft-tissue air could have putatively come from autoinflation through the Eustachian tube, but no such history was obtained. The air, once outside the mastoid, can permeate through myofascial planes to the parapharyngeal space and carotid sheaths where it will descend into the mediastinum. This case is an example of how effective a well-pneumatized mastoid can absorb such a forceful impact without a serious injury.