The orbital “blowout fracture” was initially defined by Smith and Regan [
1] in 1957 when cadaver studies showed that traumatic energy from orbital soft-tissue injuries produced predictable orbital floor fractures. These fractures correlated clinically with enophthalmos and restricted ocular motility. The current definition can include any internal orbital wall fracture, but primarily refers to the floor or medial wall. Acute signs and symptoms of orbital blowout fractures include orbital pain, enophthalmos, diplopia, and infraorbital nerve hypesthesia [
2]. Diplopia is the most common complication and often results from displacement of the fibrous septa that unite the inferior rectus sheath, the fibrofatty tissue, and the periosteum of the orbital floor [
3,
4]. Frank muscle entrapment presenting with limited upward gaze and vertical diplopia can also occur but probably does so with less frequency than previously thought [5.6]. Anatomic and volumetric changes of the bony orbit most significantly affect globe position and can lead to enophthalmos or hypoglobus [
6,
7]. The objective of fracture treatment is to reduce displaced soft tissues and restore the preinjury anatomic contour and volume of the bony orbit.
Surgery and observation are the main treatment options. Formerly, the indications and timing of surgery were controversial [
8,
9,
10]. Over the past few decades, however, orbital floor fracture management has changed significantly, culminating in an evidence-based protocol published by Burnstine [
2] that remains the preferred approach for many centers including ours (
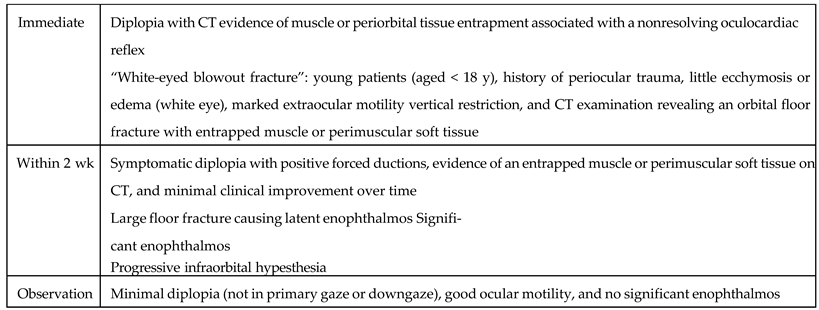
Table 1).
Clear indications for immediate surgery include entrapment and large fractures where latent enophthalmos is eminent. Conversely, observation is preferable for small fractures with minimal diplopia and intact extraocular movements. Subsequent surgical intervention is performed in those observational cases when diplopia persists or enophthalmos declares itself with resolving edema.
Complications from orbital surgery include infection of implanted material, implant migration, epiphora, worsening diplopia, lower-lid retraction, and blindness [
11,
12,
13,
14,
15,
16]. Visual loss is a rare but serious complication following repair of orbital fractures [
17,
18,
19]. The mechanism may be retrobulbar hemorrhage (RBH) or injury to the optic nerve from a displaced implant. The prognosis is good for visual recovery in RBH, given the potential reversibility with prompt treatment [
19,
20]. For this reason, some craniomaxillofacial (CMF) surgeons take the precaution of monitoring patients on an inpatient basis, while others send patients home the same day of surgery. The incidence of postoperative RBH has not been previously reported and existing data are limited to case reports.
In this retrospective cohort review, our goal is twofold: (1) to report our experience following operative repair of orbital floor fractures and (2) to determine trends in the postoperative management of orbital floor fractures by conducting a survey of North American CMF surgeons. We hypothesized that patients undergoing surgical repair for orbital floor fractures would have relatively low immediate postoperative complications at our institution. In addition, the practices of North American CMF surgeons would indicate that postoperative inpatient observation might not be routinely necessary.
Materials and Methods
A retrospective assessment was undertaken of patients undergoing surgical repair of the following types of orbital floor fractures: isolated orbital floor fracture, orbital floor fracture associated with a fracture of the medial orbital wall, or orbital floor fracture associated with a zygomaticomaxillary complex fracture. All patients were evaluated and treated by a faculty member at a tertiary care center from January 2001 through June 2010. Institutional review board approval was obtained prior to review of medical records. A total of 80 patients met inclusion criteria and had complete records for review. Mean age at surgery was 35 years (range: 13–87, standard deviation [SD] = 17). There were 55 males and 25 females.
To assess North American trends in orbital fracture management, we developed a 10-question survey that was sent to all 256 AO (Arbeitsgemeinschaft fur Osteosynthesefragen) CMF North American faculties. The questionnaire was sent as a hyperlink by electronic mail and surgeons were invited to complete the survey in an anonymous, encrypted, and confidential manner. During the 60-day period (August to September 2010), data were collected using an online survey tool (Surveymonkey.com; LLC, Palo Alto, CA). Summary reports prepared by the online service and responses to each question were analyzed.
Table 1.
Clinical recommendations for repair of isolated orbital floor fractures.
Table 1.
Clinical recommendations for repair of isolated orbital floor fractures.
We performed descriptive statistics for all survey questions. To identify patterns in orbital fracture care, we stratified some survey responses by respondent characteristics. We performed Chi-square tests to identify differences in postoperative management, as it correlates to a number of orbital repairs annually by AO faculty. Significance was established a priori at 0.05.
Results
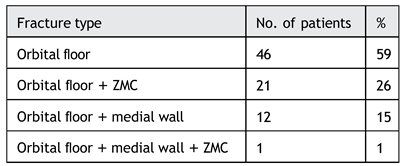
The distribution of patients by fractures type is represented in
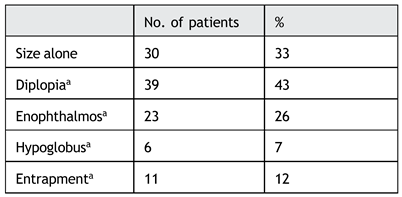
Table 2. The senior author (J.D.K) performed 70% of the repairs. Mean time to fracture repair was 9.6 days (SD = 16.4) when one outlier patient was excluded (time to repair = 1,825 days). For those with entrapment confirmed by ophthalmological consultation, mean time to repair was 1.7 days (SD = 1.9) with delay until 9 days in one case due to medical instability. Indications for repair are presented in
Table 3. In 33% of the cases, the decision was made to repair based on size alone and without other clinical findings (diplopia, extraocular limitation, etc.) with the expectation that enophthalmos would develop in the long term.
At our institution, the transconjunctival approach was used in 90% (
n = 72) of the cases. In 3% (
n = 2), an existing subciliary laceration was used, and for a period we experimented with the endoscopic approach (8%,
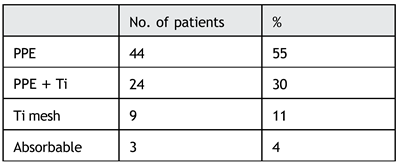
n = 6) but abandoned this due to increased anesthetic time without obvious clinical or cost–benefit. Implant type is represented in
Table 4. The majority of early repairs were performed with porous-polyethylene (PPE) or PPE with titanium (PPE + Ti). In recent years, we have increasingly used preformed titanium implants. Absorbable implants were used exclusively in the pediatric population.
Table 2.
Distribution by fracture type.
Table 2.
Distribution by fracture type.
Table 3.
Surgical indications.
Table 3.
Surgical indications.
Table 4.
Orbital implant type.
Table 4.
Orbital implant type.
Postoperative management consisted largely of overnight observation (<24 hours), occurring in 74% (n = 59) of patients with a mean length of stay of 17 hours (SD = 7.3) and range of 8.5 to 36.5 hours. One (1%) patient was sent home the same day of orbital surgery and recovered without complication. The remaining 25% (n = 20) remained in the trauma service of the hospital for other injuries.
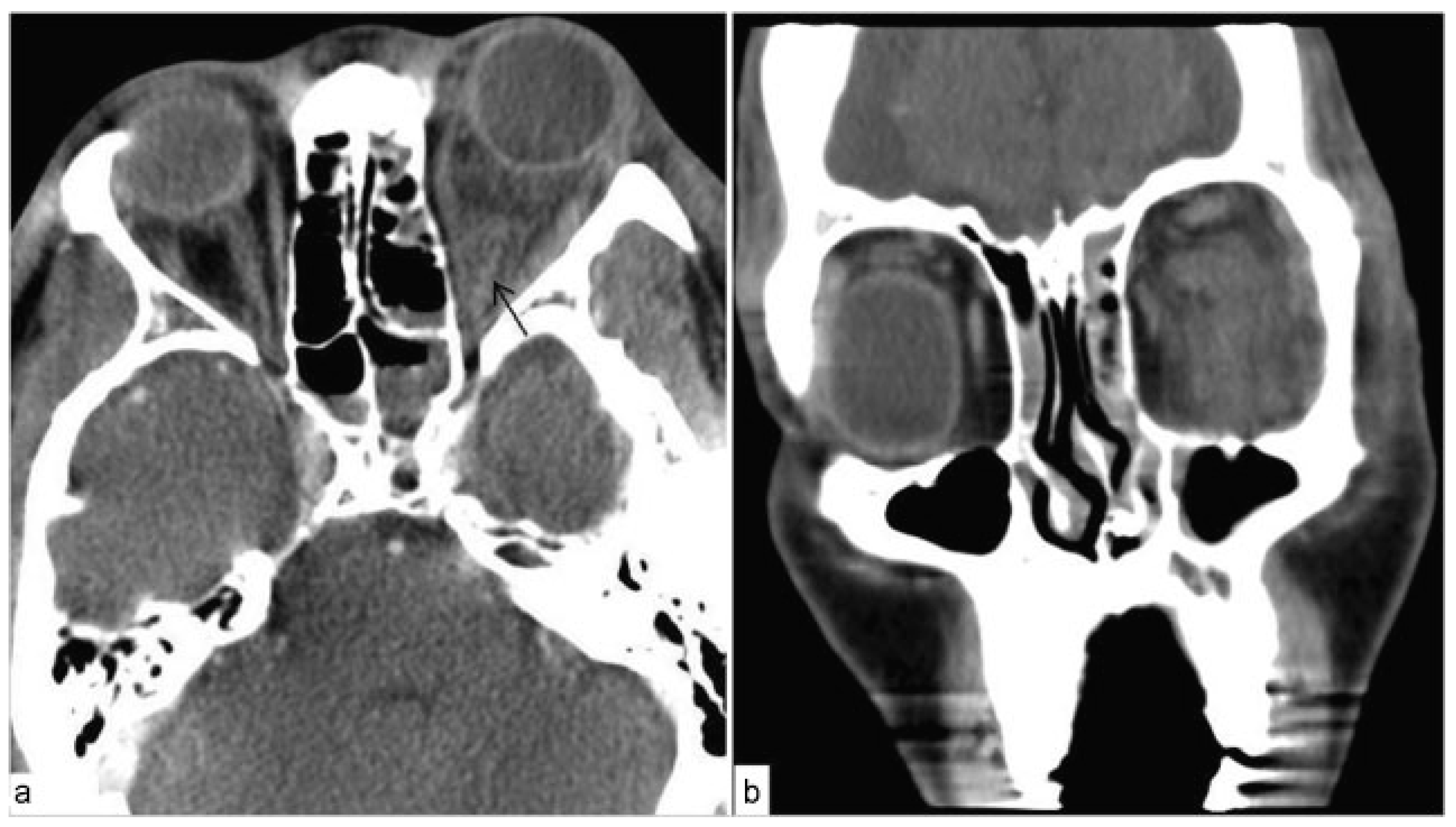
Out of 80 patients over the 9.5 year period, we had 1 (1.3%) immediate postoperative complication. Twenty hours postoperatively from an isolated orbital floor fracture, proptosis and firmness of the globe occurred in the operative eye. The patient was intubated and sedated on the ventilator due to other injuries. Intraocular pressure (IOP) of the affected eye was measured at 32 mm Hg. A lateral canthotomy and cantholysis were performed at the bedside; however, IOP continued to rise up to 52 mm Hg over the subsequent 2 hours. Computed tomography (CT) examination confirmed RBH (
Figure 1) and the patient was taken to the operating room for emergent orbital exploration. Inferior orbital bleeding was controlled with bipolar cautery, the implant was removed, and a maxillary antrostomy was performed to allow drainage. IOPs declined to 22 mm Hg 2 hours postoperatively and the patient eventually awoke and healed without sequelae.
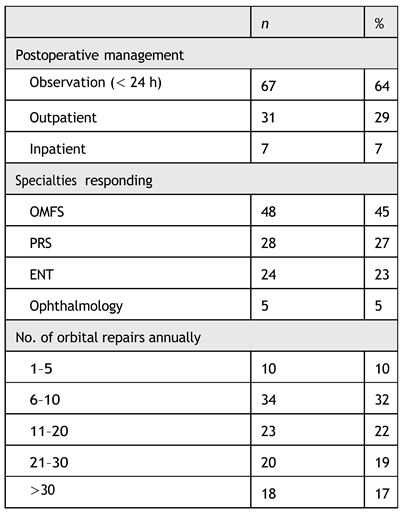
Out of 256 AO CMF faculties, 105 (41%) completed the survey.
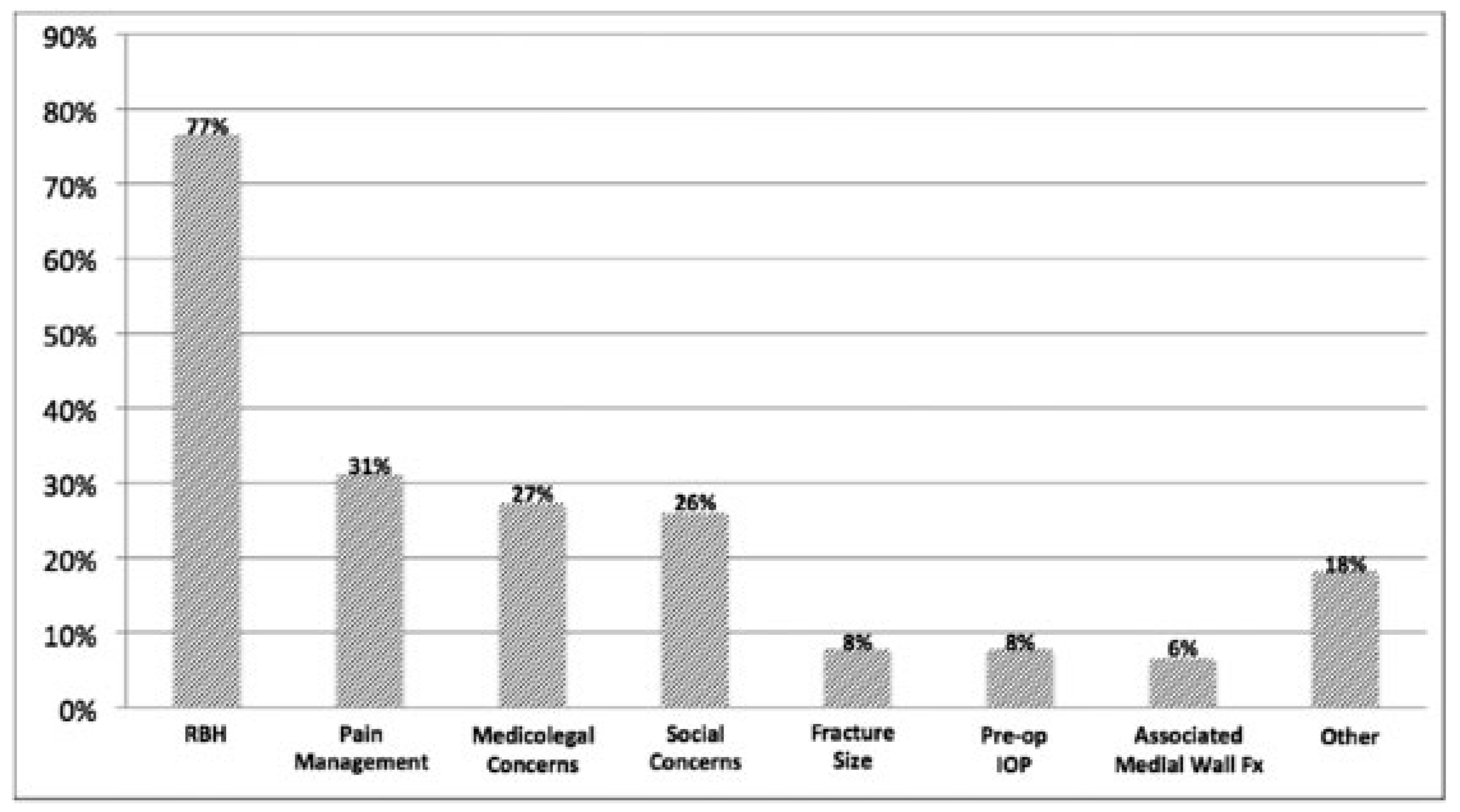
Table 5 outlines the key results of the survey. There were 77 (73%) faculties who responded to inquiry regarding their rationale for admission. Respondents were allowed to check multiple answers. The results are summarized in
Figure 2.
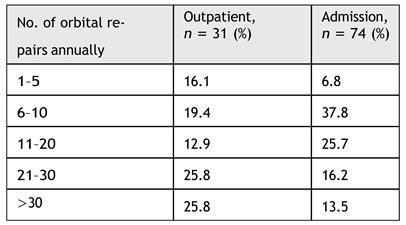
We analyzed the practice patterns of faculties who send their patients home the same day of surgery. There was no significant difference in postoperative management based on implant type or use of a drain in the orbit. According to the survey, performing more than 20 orbital repairs annually significantly increased the likelihood that faculty would manage patients on an outpatient basis postoperatively (
p = 0.03, χ
2). This trend is emphasized in
Table 6.
Discussion
In this report, we conducted a 9-year retrospective cohort study of 80 patients who underwent orbital blowout repair. The majority of the patients in our study underwent surgical repair for orbital floor fractures, where size and diplopia were the most common indications for surgery. In our retrospective study, we identified a low incidence of postoperative RBH that was limited to one patient (1.3%,
n = 1). The single RBH was recognized and treated promptly without sequelae. The low incidence of RBH at our institution is consistent with those reported in the literature. Postoperative RBH is infrequent enough, however, that a consensus on incidence has yet to be determined. Single-institution reviews have reported a prevalence ranging from 0.16% (2/1,180) to 0.39% (4/1,240) [
21]. Similar to other reports, our patient with RBH presented with symptoms of acute orbital pain, proptosis, and firmness on physical exam in the setting of increased IOPs and decreased visual acuity [
15,
21]. Upon review of similar cases of postoperative RBH, the only consistent symptom across all presentations was change in visual acuity, where proptosis, firmness, and pain varied.
Figure 1.
CT ~24 hours post-op from orbital floor repair confirming retrobulbar hematoma. (a) Axial image highlights proptosis with increase hyperdensity within the left posterior orbit (arrow). (b) Coronal images show increase hyperdensity within the left orbit with distortion of the softtissue planes.
Figure 1.
CT ~24 hours post-op from orbital floor repair confirming retrobulbar hematoma. (a) Axial image highlights proptosis with increase hyperdensity within the left posterior orbit (arrow). (b) Coronal images show increase hyperdensity within the left orbit with distortion of the softtissue planes.
Table 5.
Survey responses (n = 105).
Table 5.
Survey responses (n = 105).
Despite RBH being a known rarity, our survey among North American AO CMF surgeons indicates that RBH is overwhelmingly (77%) the primary factor behind admitting patients postoperatively. The majority of our patients (74%) were kept for less than 24-hour observation, with an average length of stay of 17 hours. Similarly, our survey indicated the majority of CMF surgeons (64%) kept patients for less than 24-hour observation, though an additional 7% kept patients as an inpatient for more than 24 hours. Interestingly, our case of RBH presented 20 hours postoperatively, which is well past our average length of stay of 17 hours. Nicholson and Guzak [
19] and Ord [
20] reported similar experiences where RBH did not present until up to 36 hours postoperatively. Cheon et al presented two cases where postoperative RBH occurred at 29 hours and 7 days postoperatively [
21]. Girotto et al presented three cases complicated by postoperative RBH: two of them occurred approximately 48 hours postoperatively and the third case was delayed until postoperative day 10 secondary to patient’s poor mental status and inability to communicate changes in visual acuity [
15]. These findings may raise questions regarding the benefits of inpatient 24-hour observation postoperatively.
The survey among North American CMF faculties does demonstrate a considerable proportion (29%) of surgeons who send patients home the same day of orbital fracture repair (
Table 5). Furthermore, the survey indicated that surgeons who performed more than 20 orbital fracture repairs annually were more likely to manage patients as an outpatient postoperatively (
Table 6). The variability in postoperative admission management was consistent across all the disciplines including oromaxillofacial surgery, plastic surgery, and otolaryngology (
Table 5). Additionally, our survey did not indicate that implant material influenced patient management patterns, though some studies have suggested a correlation between the use of polydioxanone sheets and increased incidence of postoperative RBH [
22,
23]. A porous polyethylene/titanium sheet was used in the repair of orbital floor fractures in our patient with RBH.
Figure 2.
Survey results from questionnaire for rational behind admission after orbital fracture repair. Retrobulbar hematoma was overwhelmingly the primary motivating factor for postoperative admission.
Figure 2.
Survey results from questionnaire for rational behind admission after orbital fracture repair. Retrobulbar hematoma was overwhelmingly the primary motivating factor for postoperative admission.
While it is difficult to make any definitive recommendations on inpatient versus outpatient management following orbital floor repair, our findings do suggest that there may be a role for outpatient management. Although the incidence of RBH is low, recognition of RBH and time until treatment as an inpatient versus outpatient does present a dilemma. Interestingly, our data and literature review do highlight that onset of RBH typically occurs outside the standard 24-hour observation. Our case of RBH had an onset of 20 hours postoperatively, while the mean length of time for admission was 17 hours, thus falling outside of average length of stay. Furthermore, other reported cases or RBH fall outside the first 24 hours postoperatively, ranging from 29 to 48 hours postoperatively [
15,
19,
21]. Ultimately, the value of overnight observation for RBH surveillance is unclear because the onset of RBH frequently fall outside the observation period.
The main limitation of these data includes a relatively small number of patients (n = 80) over the 9.5-year period. We included only patients treated by our department. A multicenter or prospective study would provide a more accurate incidence of postoperative RBH after orbital fracture repair. Furthermore, we did not address a relative assessment of RBH incidence, time of onset, and type of implant in this survey. Including this information in the future could provide not only a better estimate of the incidence of postoperative RBH but also further information to support inpatient versus outpatient postoperative management.
Conclusion
The combined results of our retrospective cohort study and the survey of North American AO CMF surgeons seem to indicate that postoperative inpatient observation may not be routinely necessary. In fact, survey results indicate a varied approach in postoperative management among surgeons across multiple specialties. As such, we believe patients who are reliable, educated about RBH symptoms, live nearby, and have an uncomplicated orbital repair are potential candidates for same-day discharge. This approach conserves diminishing healthcare resources.