Large full-thickness segmental defects of the maxilla, with oronasal and/or orosinus communications, represent one of the most challenging problems in reconstructive surgery of the face. Characterized by complex tissue loss, missing bone, mucosa, and teeth, surgery imposes both functional and aesthetical reconstructive objectives, particularly when the anterior arch is involved. The ideal treatment should provide adequate closure of the oronasal and/or orosinus communication while avoiding feeding and speech problems and creating stable bone and compatible dental arches for adequate mastication. The treatment should also provide good quality lining of attached mucosa allowing for dental rehabilitation with orthodontics and eventually dental implants and fixed prosthesis. Prosthetic rehabilitation could not be considered as structural reconstruction, presenting possible functional problems resulting from inadequate seal and/or instability during mastication and speech, and should be considered as an optional feature for those patients who are not candidates for surgery [
1,
2]. These kind of defects, due to their dimensions and missing compound tissues, are not eligible for traditional bone graft and the option of microvascular free flap presents problems for proper contouring and volumetric adaptation to the defect, bulkiness of soft-tissue coverage, which is incompatible with good aesthetical dental rehabilitation [
1,
3].
Distraction osteogenesis could be considered for bone defect reconstruction, as bifocal or trifocal bone transport systems. Present advantages such as the good quality of bone and lining mucosa similar to those that are missing, while obviating donor zones, with minimally invasive, shorter, less technically demanding, and consequently less risky operations, when compared with free flaps [
4]. Distraction osteogenesis is a true bioengineering method for bone and surrounding soft-tissue synthesis resulting from the gradual separation of bone segments by continuous traction forces generated by distraction devices [
5,
6]. The positive clinical results achieved using this method for treatment of several craniofacial congenital deformities allow for consolidation of its clinical indications in the past two decades. It is particularly useful for mandible elongations, which are being applied nowadays with younger patients, and even to neonates for treating micrognathia with airway obstruction because it is apparently very safe [
7,
8]. It is also a very important reconstructive tool exhibiting good and stable results for treating maxillary hypoplasia in patients with cleft lip and palate [
2,
9].
One disadvantage usually highlighted is the need for two operating procedures, as devices should be removed at the end of the treatment. In the case of bone transport, a third surgical procedure is needed to develop a compress focus when the transport disc meets the contralateral side of the defect or when both transport discs meet together on the middle of the defect, with debridement of interposed soft tissues and bone graft, sometimes called “docking site surgery” [
10,
11].
If the process of reconstruction could be done or at least started at the same surgical time of tumor excision, without compromising the full oncological treatment, this would be one obvious advantage. If the defect created by tumor excision could be left open without soft-tissue coverage, the first operative time could be shortened and the intermediate surgical docking site procedure for debridement of interposed soft tissues and bone grafting would not be required.
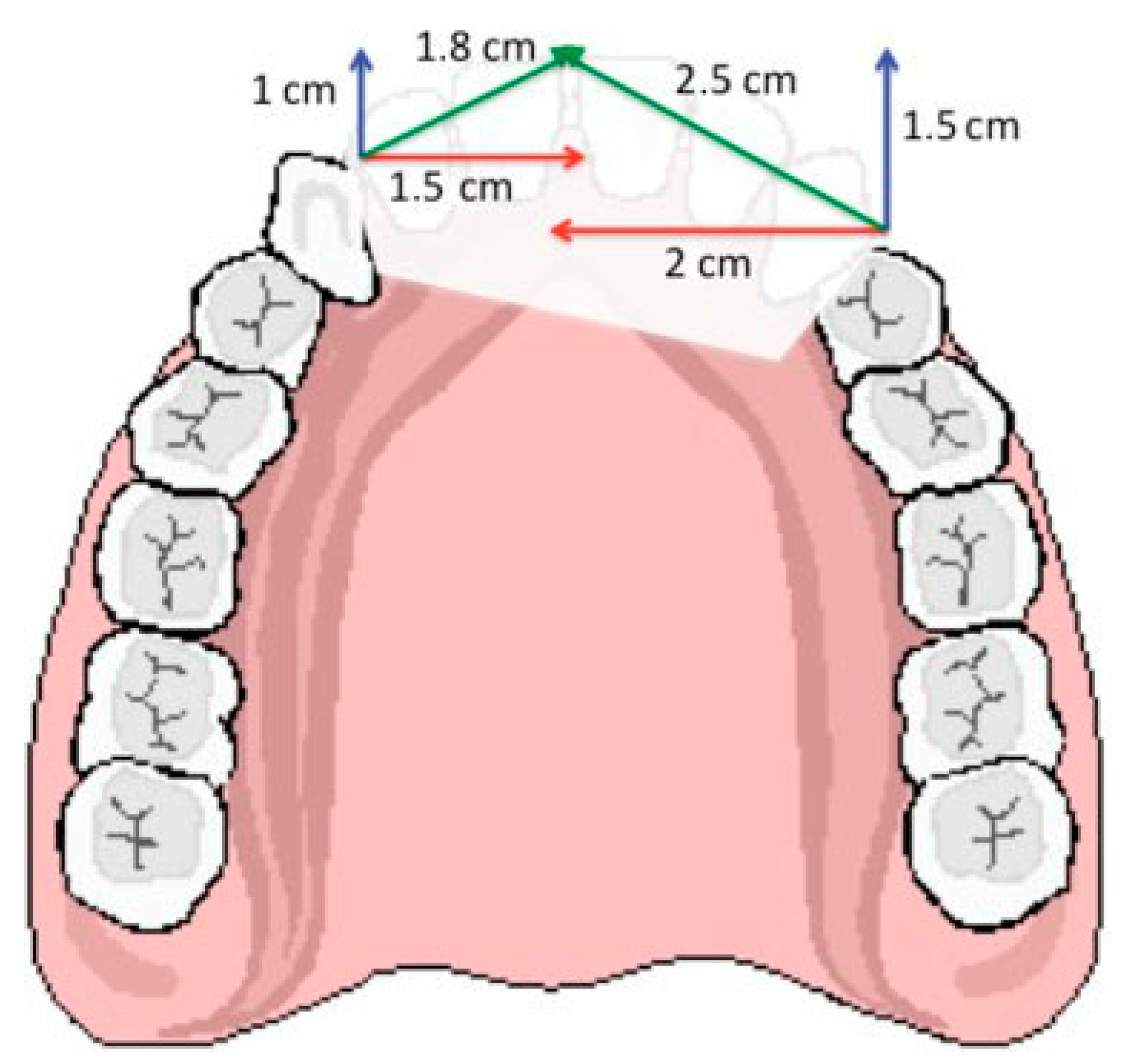
As with other indications for distraction osteogenesis, vector control is important, not only to achieve the closure of the defect but also to obtain the proper anterior projection of the reconstructed maxilla and consequently the dental arch compatibility [
12,
13]. The final vector or vectors of distraction have three components: the lateromedial, responsible for defect closure; the posteroanterior, responsible for projection of the maxilla; and the vertical component, responsible for dental arch compatibility. For a given defect, if a trifocal distraction is planned with two transport discs and two distractors, the width of the defect measured on the computed tomography (CT) scan, or on the defect itself, should be divided into two and the sum of both lateromedial component vectors would represent the width measure of the defect. Posteroanterior deficiency for each side could be measured on the lateral radiogram or on the defect itself and determines the posteroanterior component vector dimension. The final vector to which the body of the distractor device should be placed parallel is the result of graphic triangulation of these two (
Figure 1). The vertical component does not need to be calculated, as the final vector should be parallel to the occlusal plane. The final resultant vector calculated as described should have the direction and length to determine, respectively, the position of the distraction device body and the predicted length and consequently duration of distraction.
This planned distraction procedure should end with transported segments in the proper final position, but since a curvilinear reconstruction is intended, the preoperative plan should include the orthodontic manipulation of the consolidating callus. The second operative time for device removal should be done before complete consolidation, thus allowing for rotation of the segments, completion of the compress focus, and compatibility of dental arches. Eventual deviations of transported segments regarding the planned vectors could be corrected during this phase of callus remolding.
The aim of this work is to demonstrate a method for three-dimensional reconstruction of wide full-thickness anterior segmental maxillary defect by trifocal distraction osteogenesis that starts at the same surgical time of tumor excision without the need for intermediate surgical docking site procedure for creation of compress focus and bone grafting, thus requiring only one additional surgical procedure.
Materials and Methods
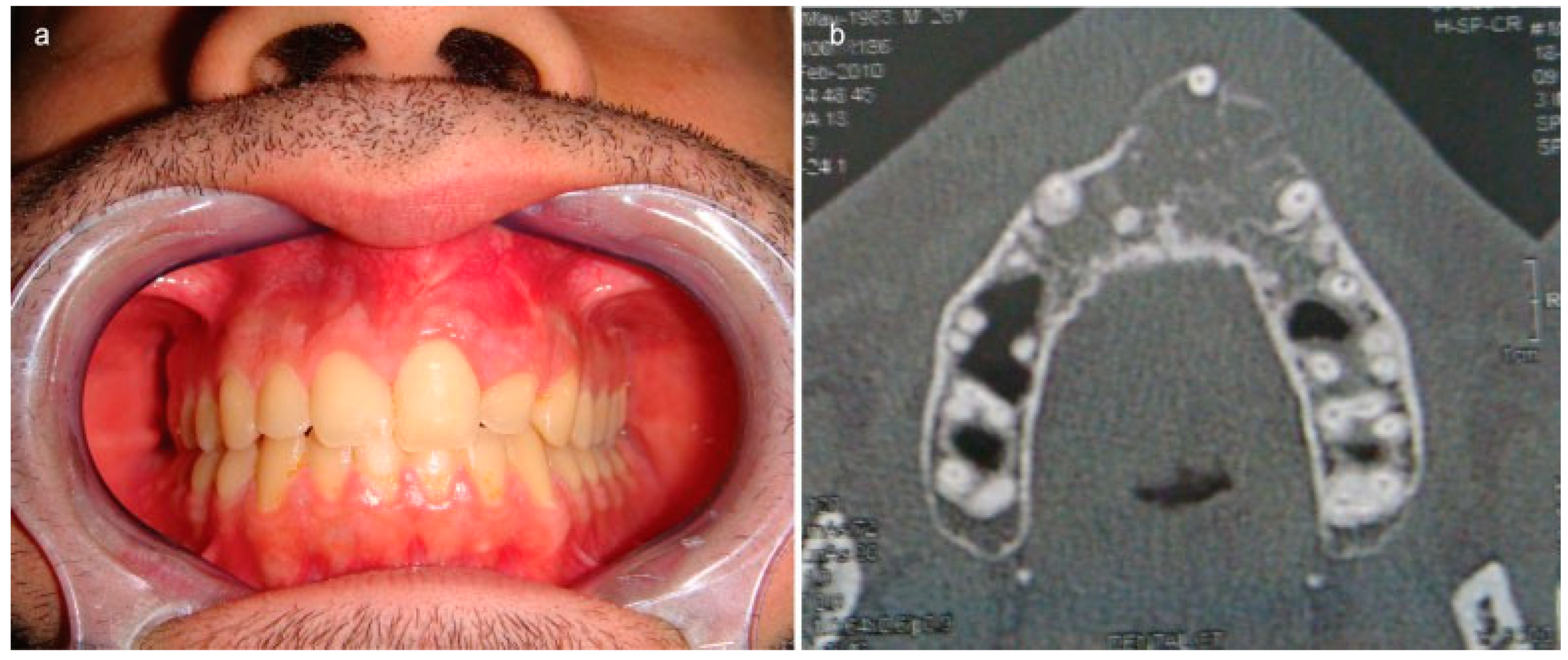
A 26-year-old male patient with a large bone tumor of the anterior maxilla extending between the right canine and left first premolar was treated (
Figure 2a).
Clinical presentation was a painless swelling visible and palpable on the anterolateral upper sulcus detected during a routine consultation. CT scan (
Figure 2b) revealed the bone expansive lesion with 2.7 cm diameter without involving soft tissues and the biopsy confirmed the diagnosis of odontogenic myxoma. Clinical and routine preoperative evaluations did not reveal any other pathology.
A multidisciplinary team approach was outlined, including the Otorhinolaryngologist, plastic surgeon, and orthodontist. It was agreed that reconstruction with bone transport would start on the tumor excision surgical time and the excisional defect left open.
Prior to treatment, the planning of the reconstruction procedure included prediction of the resultant defect dimensions after excision, vector distraction calculation, distractor device selection, surgical approach, and osteotomy lines for transport disc creation. Since the provisional defect was approximately 3.5 cm wide with 1 cm posteroanterior deficiency on the right and 1.5 cm posteroanterior deficiency on the left, a trifocal distraction was planned—placing two unidirectional distractors, one on each side. This allowed the reduction of the distraction phase by half of the time and creation of two segments of reconstructed bone for better molding using orthodontic appliances into the definitive curvilinear dental arch.
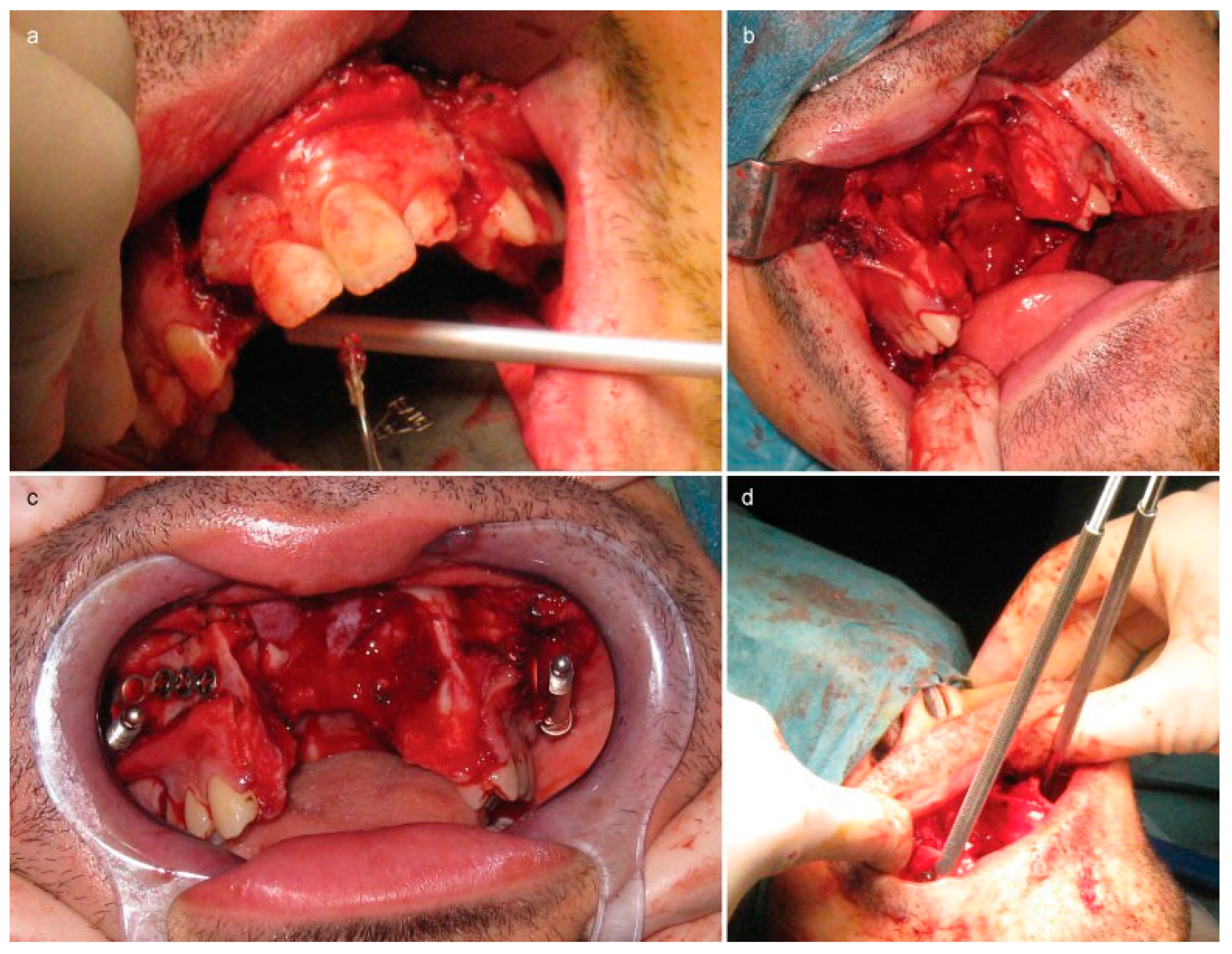
Under general anesthesia, a total upper buccal incision was performed exposing the piriform aperture and anterior walls of both maxillary sinuses.
Dental 1.2 and 2.3 extractions allowed for vertical osteotomies extending to the right nasal floor on the right, and maxillary sinus on the left (
Figure 3a). The left nasal lateral wall and septum, as well as the palate, were osteotomized, encompassing the bone tumor as planned according to the CT scan, thus completing the excision and leaving a full-thickness segmental defect with wide oral–nasal–sinus communication (
Figure 3b).
Two internal maxillary distractor devices (Synthes, Solothurn, Switzerland) with 2.5 cm body length on the left and 2.0 cm on the right were assembled and molded according to the anatomy of the patient and the planned asymmetrical vectors as described earlier. Temporary fixation was accomplished with 2.0-mm screws of the T footplate over the malar prominence and of the transport plate over the desired transport alveolar disc. Osteotomy lines were marked, devices removed, and inverted L osteotomies were performed, preserving the mucoperiosteal over-lining on both palatal and vestibular surfaces. Both distractors were fixed with an adequate number of 2.0-mm screws in the same position (
Figure 3c). Vectors and activation of both devices were verified (
Figure 3d).
Vestibular incisions were sutured over the devices. All other incisions and surgical wounds were left open. Paraffin gauze was sutured against the oral–nasal defect and nasogastric tube was left in place for 2 days.
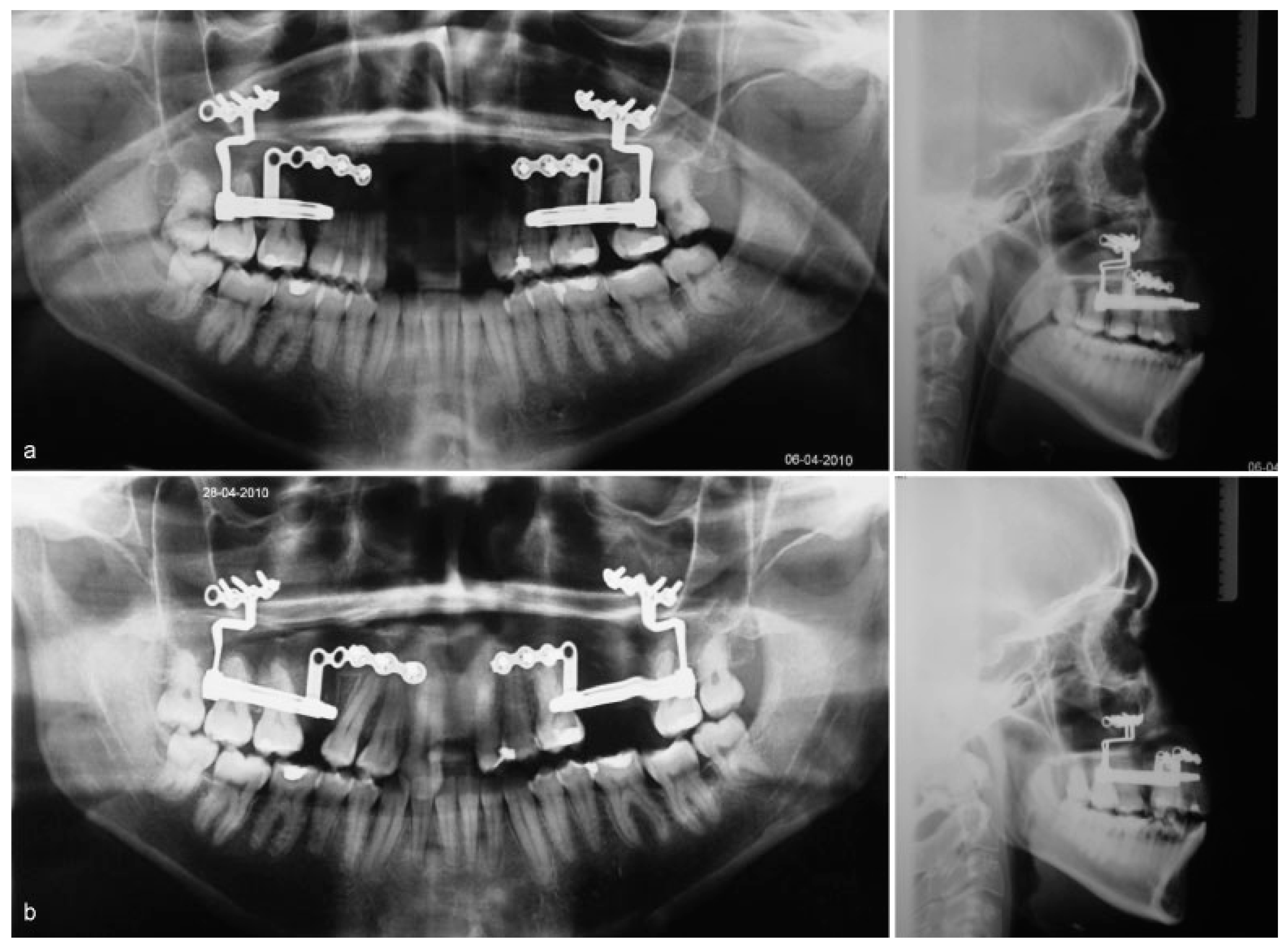
After 5 days’ latency period, activation of the devices started at a daily rate of 1 mm. Both devices achieved full activation, 25 mm on the left and 20 mm on the right, with good stability and maintenance of the planned vectors as shown by the perfect superimposing of devices on the profile radiograms (
Figure 4a,b).
Three weeks later, after both transport discs met each other in the middle (
Figure 5a), under general anesthesia, the devices were removed and left transport disc was manipulated and fixed in ideal place with one miniplate and 1.5-mm screws. A fully open 15-mm Rotterdam midline distractor device (KLS Martin, Tuttlingen, Germany) was fixed over the mucosa with 2.0-mm screws to both transport discs, intended to act as a “compression” device (
Figure 5b).
Compression started immediately postoperatively by reversely activating the distractor 1 mm daily over 10 days to achieve the adequate adaptation between both transport discs (
Figure 6).
The central “compression” distractor device was removed in the consultation room 4 weeks later after the end of the compression phase. Orthodontics started immediately with traction elastics keeping compression between transport discs while progressive teeth movements helped contour the dental arch.
Dental cusps of canine and premolars were carved to resemble incisors cusps.
Results
Tumor-free margins were confirmed by histopathologic exam of the surgical excision specimen. In total, 4.5-cm distraction osteogenesis was accomplished, 2.5 cm on the left and 2.0 cm on the right side. Good bone and teeth contact was obtained on the central compression focus, without the need of intermediate operative procedure for debridement of soft tissues or bone graft. Adequate and stable consolidation was achieved, allowing for dental orthodontic movements and permitting recreation of a nicely curved dental arch. Functional occlusion, mastication and dental aesthetics were reestablished.
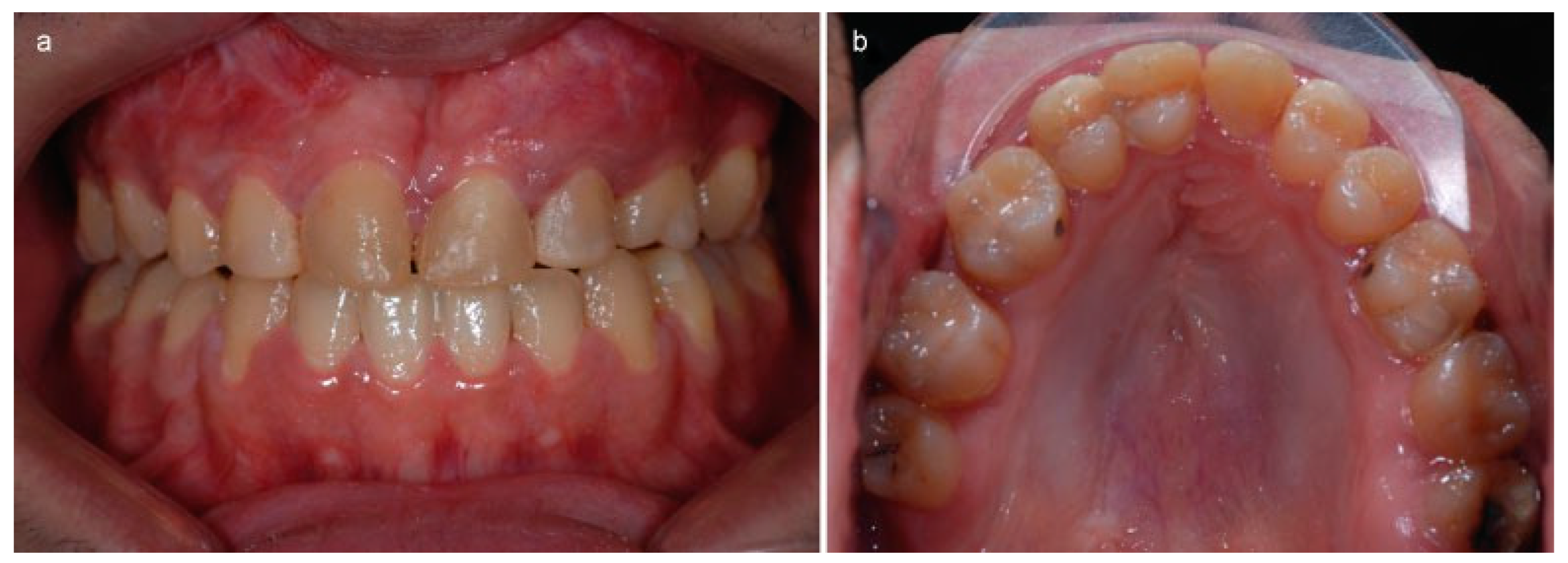
High-quality attached mucosa covered the entire dental arch contributing to the final aesthetical result (
Figure 7a).
The large oral–nasal–sinus communication was successfully closed, with newly formed bone completely bridging the palate and alveolar crest defect, allowing reestablishment of feeding and speech functions (
Figure 7b).
Anterior projection of the reconstructed maxilla supports the upper lip and nasal tip, allowing restoration of the preoperative facial appearance (
Figure 8a,b).
The 5-year follow-up confirms that this is a very stable reconstruction. Radiologic evidence excludes tumor recurrence.
Discussion
Traditional reconstructive methods have demonstrated good success rates resulting in closure of fistulae or segmental defects of the palate and alveolar crest. Once the adequate mucosal lining of both the oral and nasal–sinusal is guaranteed, bone grafting permits to reestablish bone continuity, closure of the defect, and provide a stable foundation for implant placement and orthodontic dental displacement, thereby allowing good dental rehabilitation [
14].
Frequent graft failure occurs when there is an inappropriate vascularized recipient bed, insufficient graft stabilization, inadequate covering with mucoperiosteal flaps, or when the initial defect is critically wide.
In such cases, free microvascular flaps are an option, permitting efficient closure of the defects and reestablishing bone continuity, but present several problems for dental rehabilitation, mainly related to difficult molding and adaptation to the defect and particularly to the bulkiness of softtissue covering. Additionally, they require experienced teams trained in microsurgical techniques and lengthy surgical times not affordable by patients with increased surgical anesthetic risks [
13].
Distraction osteogenesis represents an attractive option, particularly if bone donor zones can be avoided.
Experimental animal studies have shown that alveolar and palatal full-thickness defects could be successfully closed with bone transport distraction [
15,
16]. Several authors achieved the same objectives while treating patients with alveolar and palatal cleft, obtaining good functional results, and also showed that superior aesthetical dental rehabilitation is possible with implants and orthodontic treatment [
10,
11,
17,
18,
19]. Immediate application of distractors at the same surgical time of bone tumors excision was previously described as a successfully reconstructive option in the mandible, both in experimental works and also in clinical cases [
20,
21].
In the maxilla, the three-dimensional complexity of bone framework separating the oral cavity from nasal and sinus cavities, specialization of the attached mucosa, and aesthetical importance of the anterior dental arch present several particularities when considering this reconstructive option.
This article uniquely describes how distraction bone transport could also be applied in the maxilla immediately after tumor excision for reconstruction of a segmental full-thickness defect with wide oral–nasal–sinusal communication.
Other important differences between this article and those from other authors are that the compression focus development does not require further surgical time and a bone graft was not needed to achieve stable bone and mucosa continuity.
The bone stumps on the defect were left open and no attempt was made to close the surgical wounds due to the tumor excision, thus no soft tissues were interposed between transport discs and no debridement was needed.
Furthermore, the removal of the distractor devices before the complete consolidation of the regenerate, open callus manipulation and fixation of one of the two transport discs to the maxilla, and utilization of compression forces generated by another device distractor fixing both transport discs created a new dynamic system that simultaneously increases contact at the compression focus while the regenerated bone on the other side is molded to final position.
As this central distractor device is directly fixed over the mucosa, no additional surgical procedure was needed for its removal once complete consolidation was achieved.
The transport of two large discs, each one containing three teeth, allows for orthodontic repositioning and redistribution of dental pieces posteriorly. Meanwhile, anteriorly perfect adaptation of both segments avoids additional docking site surgery for alveolar reconstruction with bone grafting or alveolar distraction as described by other authors [
4,
17].
Several studies, both experimental [
22] and clinical [
23], have shown important advantages of callus manipulation and molding of regenerate of the new reconstructed bone, facilitating the better positioning of segments and avoiding problematic malocclusions at the end of the treatment process.
The described dynamic system for bone transport takes advantage of the possibility of regenerate molding prior to consolidation, using one side for stabilization with plate and screws, while the other side stays free for central displacement and anterior rotation promoted by the central device being applied at the same time. Posterior new bone regenerated by distraction allows easier dental orthodontic movements including those of molar teeth, which helps the reestablishment of smooth curvilinear dental arch. A good and stable dental arch could be restored and a compatible and functional dental occlusion could be returned to the patient. This study shows that this kind of defect could be successfully treated with bone transport, starting at the same surgical time of tumor excision with only one additional procedure, avoiding docking site bone grafting and taking advantage of open callus manipulation for application of a compression dynamic system.
Conclusion
Based on our experience and on the several reports in the literature, we consider that a detailed planning and extensive workup performed by an experienced multidisciplinary team is essential in the treatment of complex wide-segmental defects of the anterior maxilla. Bone transport with bilateral discs and two distractor devices, as trifocal distraction osteogenesis, is recommended for ideal functional and aesthetical results in the reconstruction of large segmental defects of the maxilla with oral–nasal–sinusal communication. Reconstruction could be immediately initiated at the same surgical time of tumor excision, without any attempt of bone coverage, thus avoiding two surgical procedures of the three usually needed in cases of secondary bone transport reconstruction.
The dynamic system described allows for simultaneous modeling of the regenerate and perfect adaptation at the docking site, thus avoiding additional surgical procedures, such as bone grafting, alveolar distraction, and dental implants, and contributing to nice reestablishment of a curvilinear dental arch. Reduction in total time of treatment, avoidance of other surgical proceedings, and use of additional devices could also represent important advantages regarding patient compliance to treatment and reduction in total treatment costs. Further clinical experience would be needed in treating other patients with this reconstructive approach to collect more evidence of its applicability and consistency of results.