The infraorbital nerve (ION) innervates the midface maxillary region [
1]. Most of the ION territory is supplied by the nasal and superior labial (SL) branches which divide within the infraorbital canal [
2]. The nasal nerves comprise the external nasal (EN) nerve which terminates in the ala of the nose and the internal nasal (IN) nerve which terminates in the nasal vestibule [
3]. The SL nerve gives a medial and a lateral sub-branch which terminates in the superior lip [
3]. A few reports exist that describe the variations of the nasal nerves, but there is paucity of data regarding the SL nerve.
Fusion of these branches has been reported previously. These mainly involve fusion of the EN and IN nerves but may also involve the sub-branches of the SL nerve [
4].
Unexpected variations reduce the chances of successful infraorbital nerve block (IONB) while increasing the possibility of iatrogenic injury [
5]. This study was premised on the expectation that a detailed investigation of the organization of the nerve may yet reveal new findings relevant for surgical procedures of the midface.
Materials and Methods
This study was performed on 84 IONs by dissecting the faces of 42 formalin-fixed cadavers from the Laboratory of Topographic Anatomy, Department of Human Anatomy, University of Nairobi. These included cadavers without facial malformations, injury, or evidence of surgical operation in the midface.
The point of emergence of the ION was determined by dissection and its branches were exposed. The course of the nasal and SL nerves was defined through meticulous dissection. The pattern of emergence was recorded as classical, fused, or from accessory foramen. Additional branches not in keeping with the normal pattern were noted. When the nerve emerged from an accessory foramen, the bone was drilled to confirm that it branched from the ION within the infraorbital canal. All instances of aberrant emergence were investigated further through wide dissection to confirm the branching point and exclude the possibility of the nerve being absent. The course of the nerves was followed to describe their distribution patterns. The terminal filaments of the facial nerve that join the sub-branches of the SL nerve to form the infraorbital plexus were nipped off to fully expose the SL branches and study their distribution.
Results
Each of the branches of the ION presented with a unique pattern of variations. These included absence, bifid, and variant sub-branches.
External Nasal Nerve
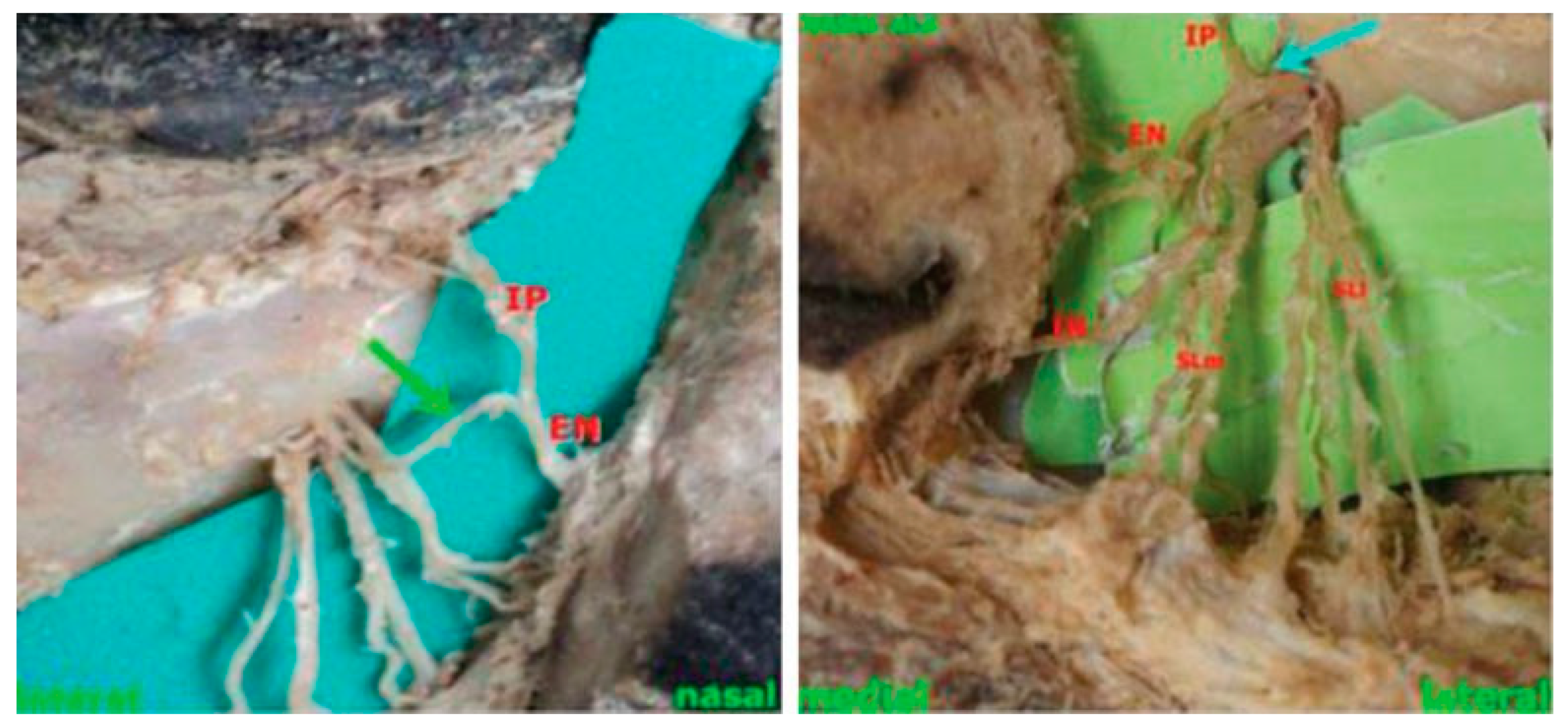
The EN nerve was identified in 55 cases (65.47%) and was absent in 29 (34.53%). Eight (9.5%) of the nerves were divided into three branches after emerging from the infraorbital foramen (IOF). Some of these branches also gave sub-branches which communicated with the IN nerve. The nerve was also found emerging as a common trunk with the inferior palpebral nerve (
Figure 1). This trunk ran medially for approximately 8 to 9 mm before bifurcating into the two nerves. The EN nerve had short oblique course before terminating into the ala of the nose.
Internal Nasal Nerve
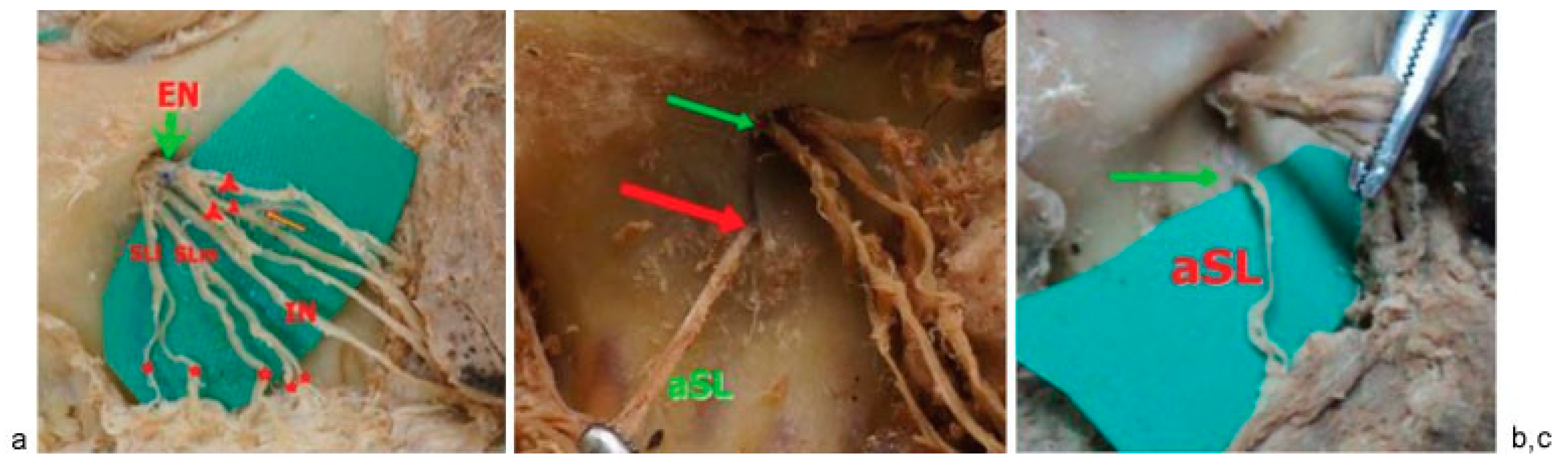
The IN nerve was present and emerged from the IOF in all cases studied. This nerve was bifid in 50 (59.5%) cases, while the other 34 nerves coursed as a single nerve. A further variation involved a communication with the EN nerve through an anastomosing branch. The nerve coursed obliquely across the cheek to terminate in the skin of the nasal vestibule (
Figure 2a).
Superior Labial Nerve
The SL nerve was unbranched at emergence in 50 (59.5%) cases. Of these nerves, 35 bifurcated after emergence and 15 trifurcated. The rest of the nerves (40.5%) had the classical two branches at emergence. The nerves branched further before terminating into the skin of the superior lip (
Figure 2a). Accessory SL nerves emerging from a separate foramen inferior to the IOF were identified in 9.52% of the hemifaces (
Figure 2b,c). These extra branches also terminated into the superior lip such as those emerging from the IOF.
Discussion
The EN branch was not identified in 34.53% of cases. The innervation of the skin over the lateral part of the nose is normally by the EN nerves from the ION and anterior ethmoidal nerve as well as the terminal twigs of the nasociliary nerve [
6]. These nerves run in close proximity and anastomose extensively [
7]. The EN branch of the ION normally joins the terminal twigs of the nasociliary nerve [
8] and in the absence of the EN branch of the ION, this area may be supplied by EN branch of the anterior ethmoidal nerve and the terminal twigs of the nasociliary and the infratrochlear nerves [
7]. Knowledge of this variation is important when considering the extent of anesthesia after extra-oral nerve block. IONB may be unsuccessful due to this variation in which case the other nerves may need to be blocked independently for rhinoplasty.
The EN nerve was also found to emerge as a common trunk with the inferior palpebral nerve. While this has not been reported earlier, it has been documented that the EN nerve compensates for the absence of the medial branch of the inferior palpebral nerve [
3], an indication that these nerves have close structural and functional relationship and the possibility of overlap in their distribution areas need to be taken into consideration. This is particularly so when loss of sensation in the medial part of the inferior eyelid is the early indication for damage to the EN nerve.
The IN nerve was identified in all cases in this study which was in keeping with a previous report [
3]. This nerve has received little attention both in text books [
3] and published studies. These findings provide evidence to the need for special care to this nerve during procedures such as rhinoplasty, as its injury may cause loss of sensation in its area of distribution. In tandem with previous reports, this nerve ran around the ala to innervate the nasal septum and the vestibule [
3], a pattern that recurred in all cases in this study. A previously reported variation in which the nerve supplies the philtrum [
3] was not observed in this study.
A further deviation from published reports was the finding of bifid IN nerves which occurred in majority of the cases studied. It may be necessary to perform live experiments to investigate whether the branches overlap in their distribution and may thus be considered for grafting.
Reports of SL nerve having a medial and lateral sub-branch have been documented [
3]. In this study, trifurcation of this nerve was also found but with a lower frequency than the bifid cases. A novel variation in the SL nerve was an accessory nerve emerging at a mean distance of 6 mm below the IOF. Details of such a variation were not found in the reviewed literature. Such a variation may lead to complications during maxillary reconstruction surgery, especially plate placement.
Conclusion
This detailed study reveals additional variations in the emergence and branching pattern of the ION. Caution is imperative during orbitozygomatic facial surgery to prevent injury to these branches. These variations also underlie the lack of response to surgical treatment for trigeminal neuralgia and also the need for a filtration to achieve full anesthesia after IONB. In addition, the extra branches identified raise the prospects of using these nerves for grafting purposes if their precise patterns are determined.