The pathologic sequelae of events leading to TMJ ankylosis is an episode of trauma leading to hemarthrosis which if unattended at the time of episode of trauma subsequently gets organized into solid bone, especially in children. Fibroosseous restructuring of hemarthrosis contributes to the formation of the ankylotic mass. The ankylotic mass demonstrates an aggressive capacity for regrowth and inadequate resection of this mass may result in its reorganisation [
5,
6]. Gap arthroplasty in present-day practice is discouraged because it has the disadvantage of reankylosis, short ramus, failure to remove all the bony pathology, malocclusion, and limited range of motion postoperatively [
7]. Many patients undergoing gap arthroplasty were reporting with reankylosis and the two main reasons were noncompliance to physiotherapy and inadequate resection without any reconstruction of the joint. A gap of 1.5 to 2.5 cm is considered as adequate resection [
8]. After adequate resection of the ankylotic chunk, reconstruction of the joint using alloplastic/autogenous material with emphasis on postoperative physiotherapy facilitates stable functional and aesthetic outcomes. Reluctance and noncompliance to physiotherapy regimen may lead to reankylosis.
Reconstruction of the joint after gap arthroplasty is of paramount importance to maintain vertical ramal height which in some modalities such as costochondral grafting (CCG) and titanium reconstruction plate with condylar head help maintain form and function of the jaws, whereas relining the joint with modalities such as temporalis fascia, temporalis muscle, and articular disc repositioning act as barriers between the base of skull and the ramal unit of mandible obliterating the dead joint space to prevent reankylosis. This article outlines the authors’ 14 years of experience in the reconstruction of posttraumatic TMJ ankylosis using various alloplastic and autogenous materials.
Results
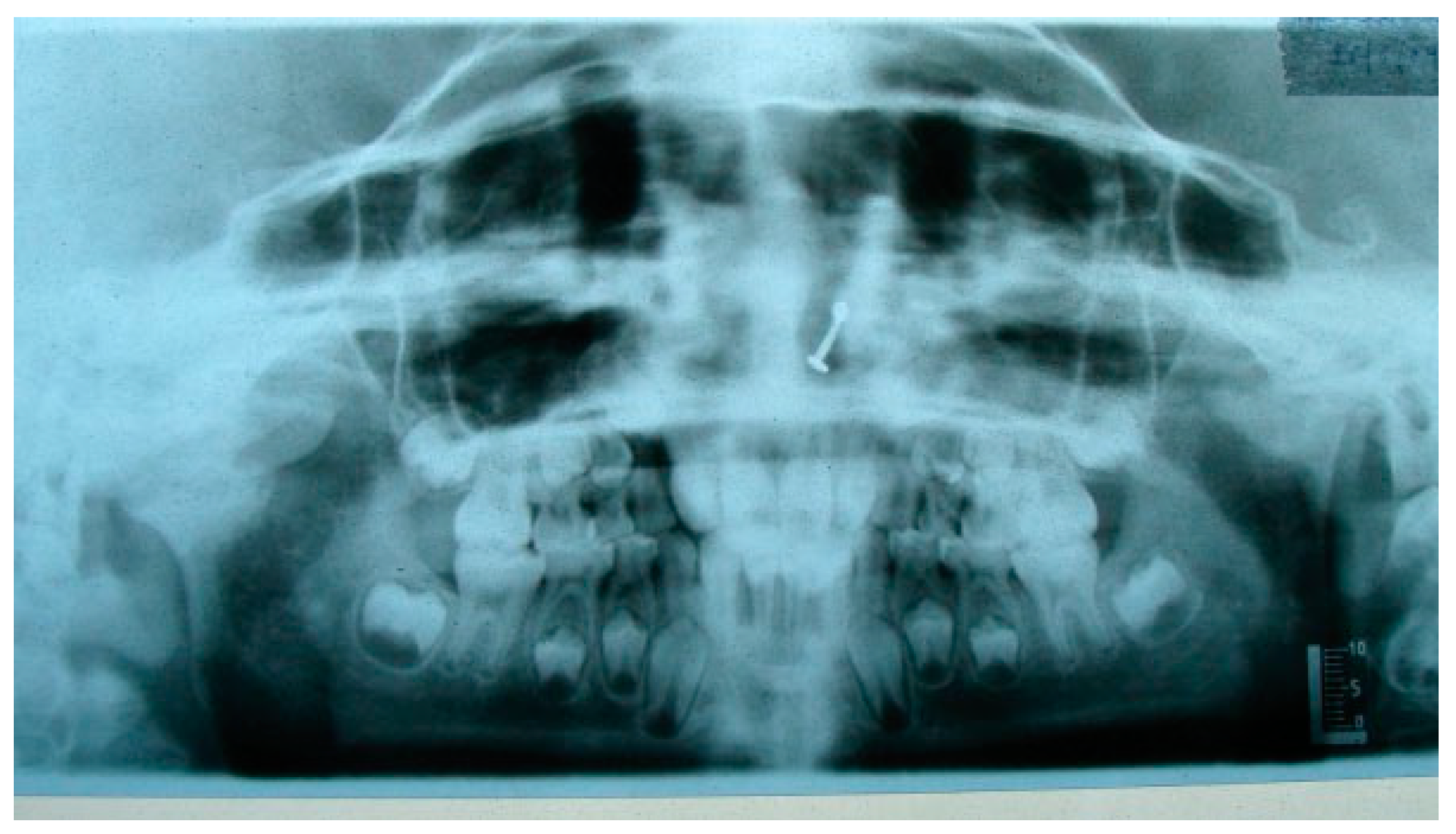
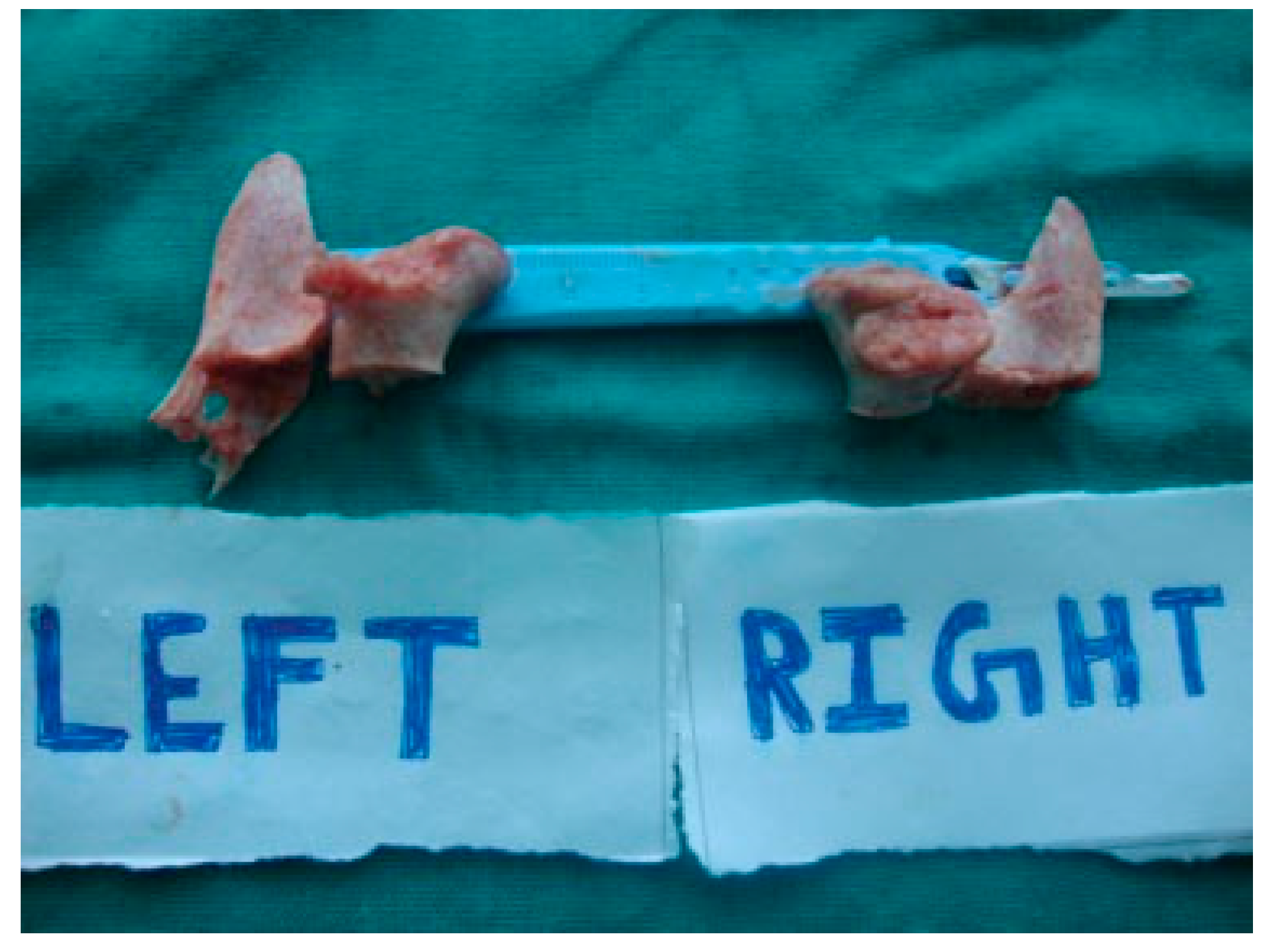
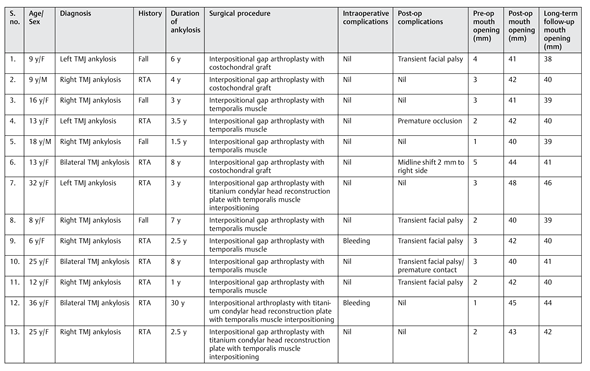
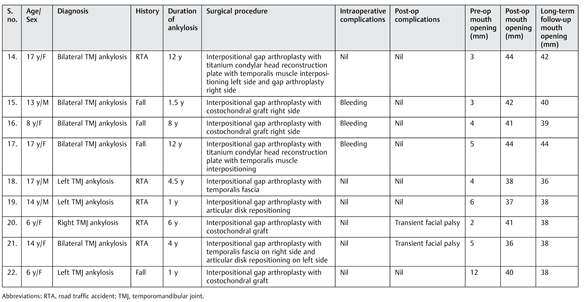
A total of 24 patients underwent surgery for TMJ ankylosis from 2002 to 2013, out of which 2 were excluded as they underwent simple gap arthroplasty. Eight out of the 22 patients had history of fall and the rest 14 had history of road traffic accidents. Twenty-two patients in this study included 5 males and 17 females. There were eight cases of bilateral TMJ ankylosis and 14 cases of unilateral TMJ ankylosis. Right sided ankylosed joints were 8, left sided were 6, and bilaterally ankylosed joints were 8 in number (
Table 1). Hence, 22 patients underwent the release of 30 ankylotic joints. Out of the 30 ankylotic joints, 28 had Sawhney’s Type IV ankylosis and 2 had Sawhney’s Type III ankylosis. Age groups ranged from 6 to 36 years with a mean age of 15.61 years. Average duration of ankylosis was 5.90 years.
Interpositional arthroplasty was done using temporalis fascia in two patients, temporalis muscle in seven patients, and articular disc repositioning in two patients, whereas joint reconstruction was done using CCG in seven patients and titanium reconstruction plate with condylar head in five patients.
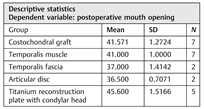
The various treatment modalities used in our series of 22 patients yielded satisfactory and comparable maximum inter-incisal mouth opening (MIMO) (
Table 2 and
Table 3) Transient facial palsy was present in 7 out of the 22 patients operated, which resolved in 3 to 6 weeks (
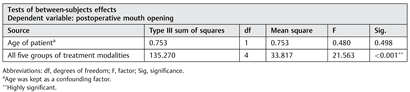
Table 1). Pain was present in patients postoperatively but absent 3 months postoperatively even during function. Protrusive and lateral movements significantly improved at 6-month follow-up. None of our patients reported with a reankylosis during the follow-up period. We compared the various treatment modalities using analysis of covariance after considering age as a confounding factor. Using ANCOVA,
p-value was found to be less than 0.001 which is highly significant, suggesting that all these treatment modalities give clinically acceptable yet different results in terms of postoperative MIMO. Further applying the post hoc multiple comparison test shows that titanium reconstruction plate with condylar head gives the best results in terms of MIMO postoperatively as compared with any other treatment modality of our group. Conceptually, this is essentially due to adult patients with a larger size stomatognathic apparatus compared with children. CCG and temporalis muscle give clinically similar results followed by temporalis fascia and articular disc in terms of MIMO postoperatively (
Table 2 and
Table 3). Functionally stable occlusion was achieved in all cases.
Discussion
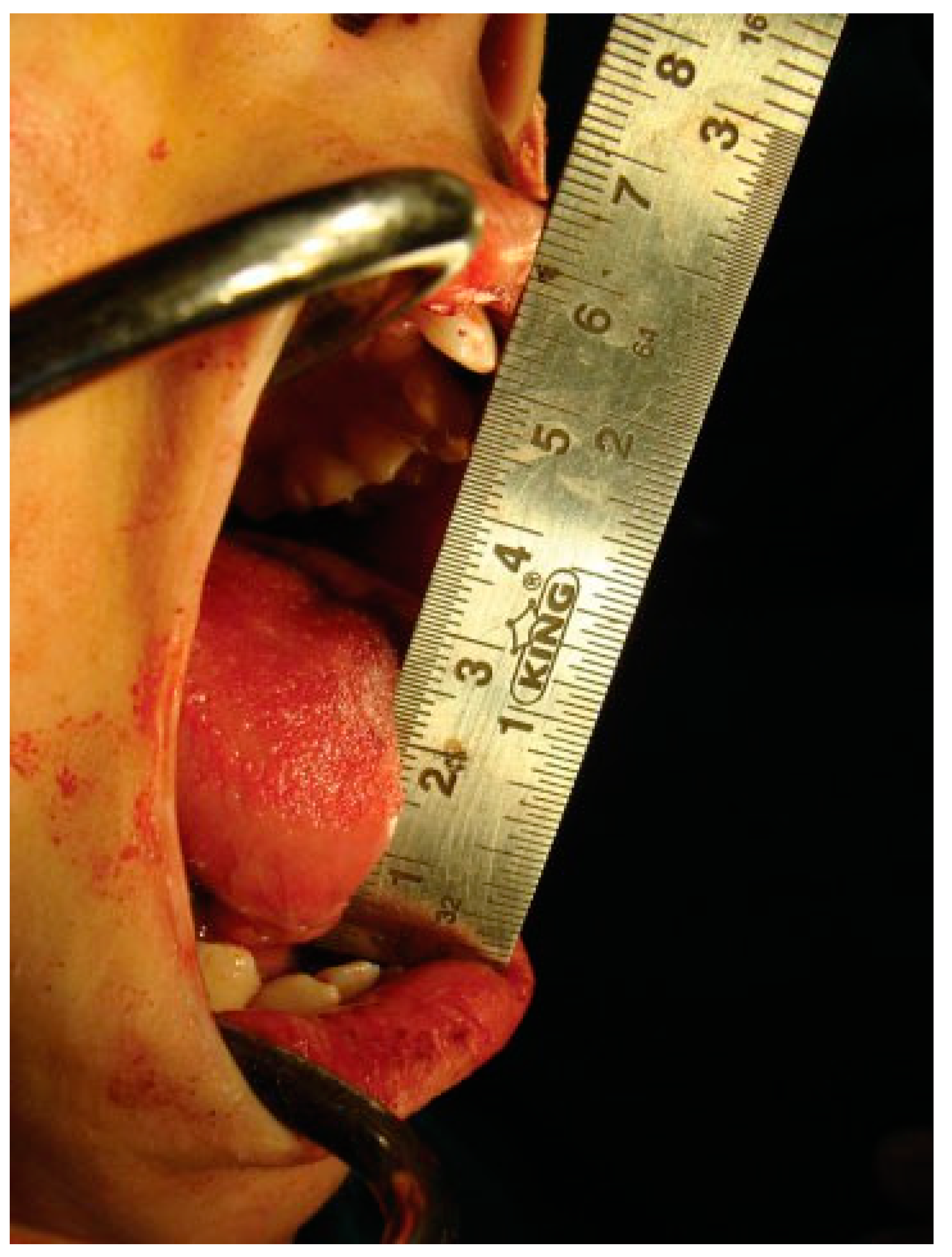
Reconstruction of the TMJ after release of ankylosis assumes paramount importance in terms of restoration of facial form and function. The goals of treatment in all the patients were the release of ankylotic mass, restoration of normal jaw form and function, symmetric growth of the mandible in children, and most importantly the prevention of reankylosis. All interpositional arthroplasties are to some extent the autogenous reconstruction of the morbid ankylotic TMJ after resection of the ankylotic mass. Merriam Webster Dictionary defines reconstruction as the act or process of building something that was damaged or destroyed again. Reconstructive surgery refers to a procedure whose goal is intended to restore form and function in structures deformed or damaged by disease, congenital anomaly, tumor, trauma, or infection (Farlex Partner Medical Dictionary Farlex 2012). The treatment of TMJ ankylosis is individualized based on the severity of ankylosis, age of the patient, and other patient factors. We have outlined our experience following Kaban’s protocol in the management of TMJ ankylosis. It is of paramount importance to obtain passive and maximal mouth opening using this protocol in terms of adequate resection and ipsilateral or contralateral coronoidectomy whenever required followed by aggressive physiotherapy (
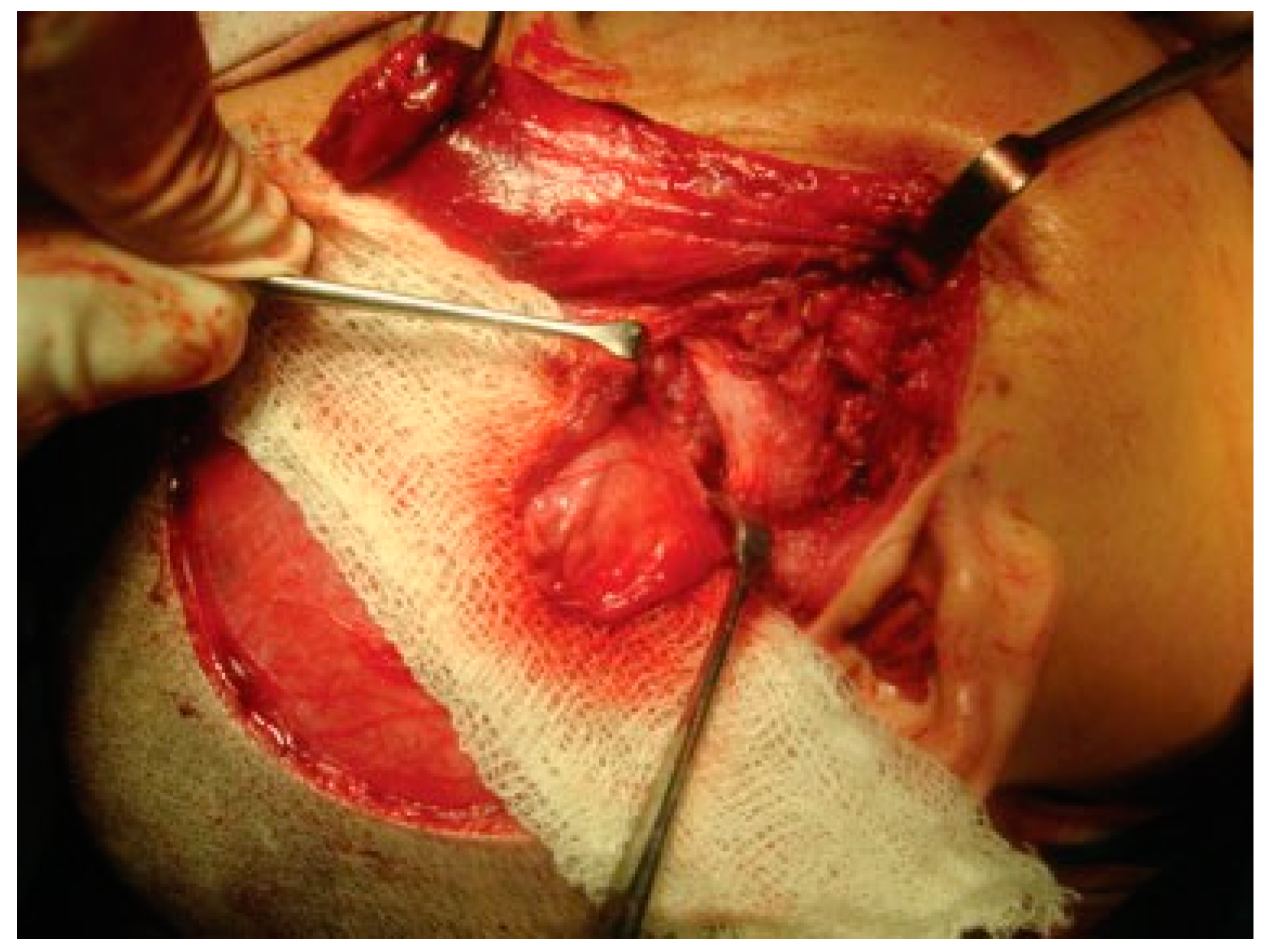
Figure 5 and
Figure 6). Physiotherapy was started on third day postoperatively using Heister mouth gag five times a day during the hospital stay of the patient. This device was purchased by the patient after discharge from the hospital for physiotherapy at home. The MIMO and excursive movements were recorded at various follow-ups for all the patients. No intermaxillary fixation/elastics were applied to any of the patients in the series.
We grouped all our patients based on Sawhney’s classification of TMJ ankylosis and all of them were Type III and Type IV TMJ ankylosis according to this classification, which are the progressively more severe types of TMJ ankylosis.
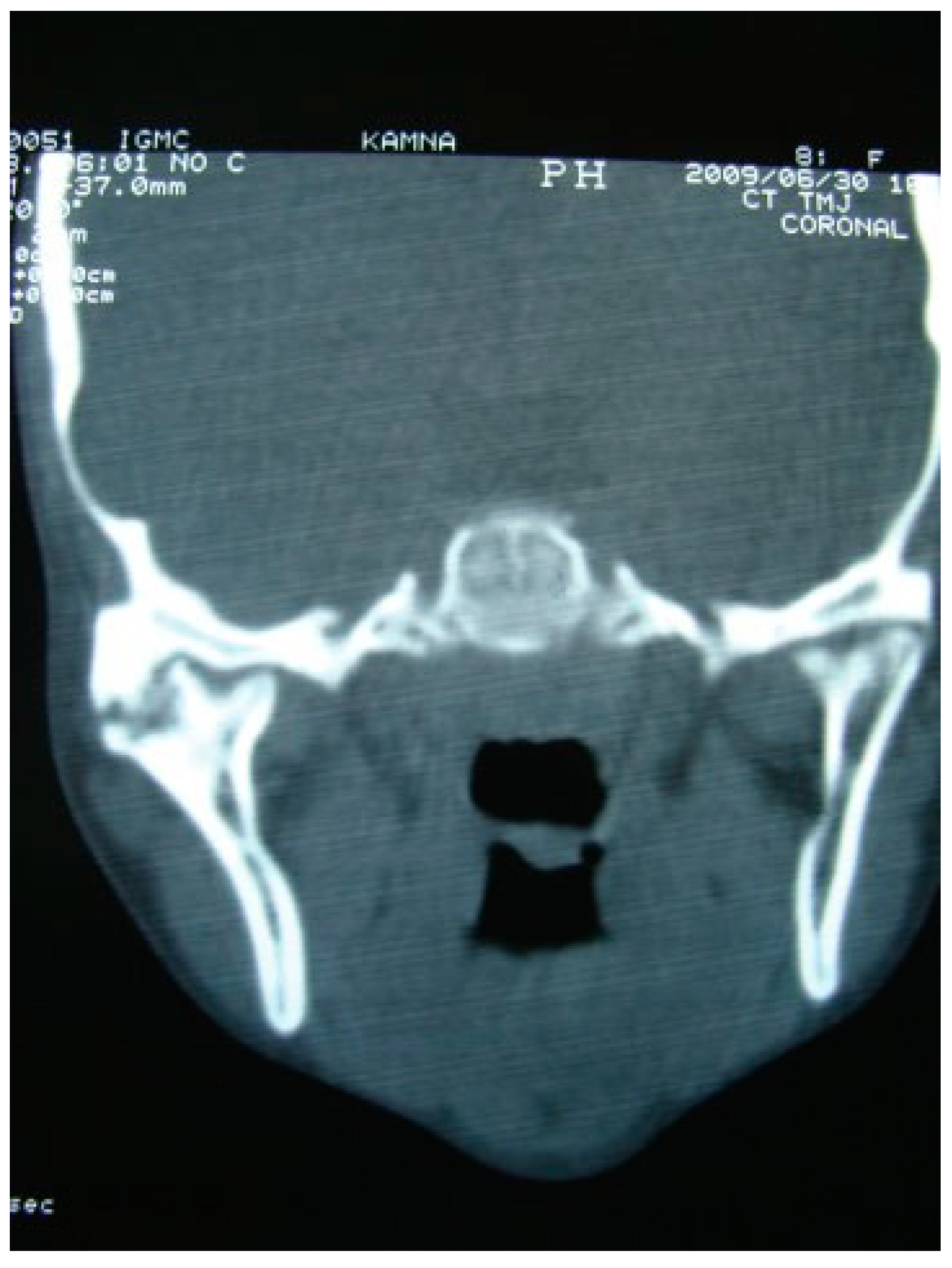
He et al devised a new classification of TMJ ankylosis which was a modification of Sawhney’s classification based on the coronal CT scan and based their treatment protocol accordingly. Type A1 is fibrous ankylosis, where post release of fibrous tissue, joint reconstruction was done using temporalis myofascial flap (TMF), masseter muscle flap (MMF), or CCG. Type A2 is ankylosis with bony fusion on the lateral side of the joint, while the residual condylar fragment is bigger than 0.5 of the condylar head in the medial side, and type A3 is similar to A2 but the residual condylar fragment is smaller than 0.5 of the condylar head. In both A2 and A3, lateral arthroplasty was done and reconstruction was done using CCG, TMF, or MMF. In type A4, there is complete bony fusion and reconstruction was done using CCG, TMF, or MMF [
9].
The key guidelines in the management of ankylosis followed by us were three-dimensional resection of the ankylotic mass measuring at least 2 to 2.5 cm to achieve passive mouth opening followed by interpositional arthroplasty using temporalis fascia, temporalis muscle, articular disc repositioning, reconstruction using CCG, and titanium condylar head reconstruction plate with temporalis muscle interpositioning. None of these patients had reankylosis on long-term follow-up ranging from 24 to 96 months.
Missed diagnosis or inadequate treatment after the initial episode of trauma with no subsequent follow-up of the patients was responsible for the development of TMJ ankylosis with patients often reporting months to years after the episode of trauma (one patient reported 30 years after the initial episode of trauma at the age of 36 years), when these patients had a debilitating restriction in mouth opening making their day-to- day chores impossible to carry out. The senior author (Y.B.) used various autogenous interpositional materials and alloplastic titanium reconstruction plate with condylar head, depending on the age and requirement of the patient.
Advantages of autogenous grafting include ease of adaptation to the host site and remodeling over time, low infection, and cost-effective technique. TMF has manifold advantages, such as its close proximity to the surgical site, adequate vascularity for maintaining viability, less chances of injury to the facial nerve since the plane of dissection is directly on the deep temporal fascia, and greater bulk to obliterate the joint space [
10]. Feinberg and Larsen described the use of a pedicled flap composed of temporalis muscle and pericranium as an interpositional material that simulates the disc functionally [
11]. Temporalis fascia lacks bulk, so the additional layers necessary to simulate the disc thickness may result in compromised vascularization and may jeopardize long-term viability [
12].
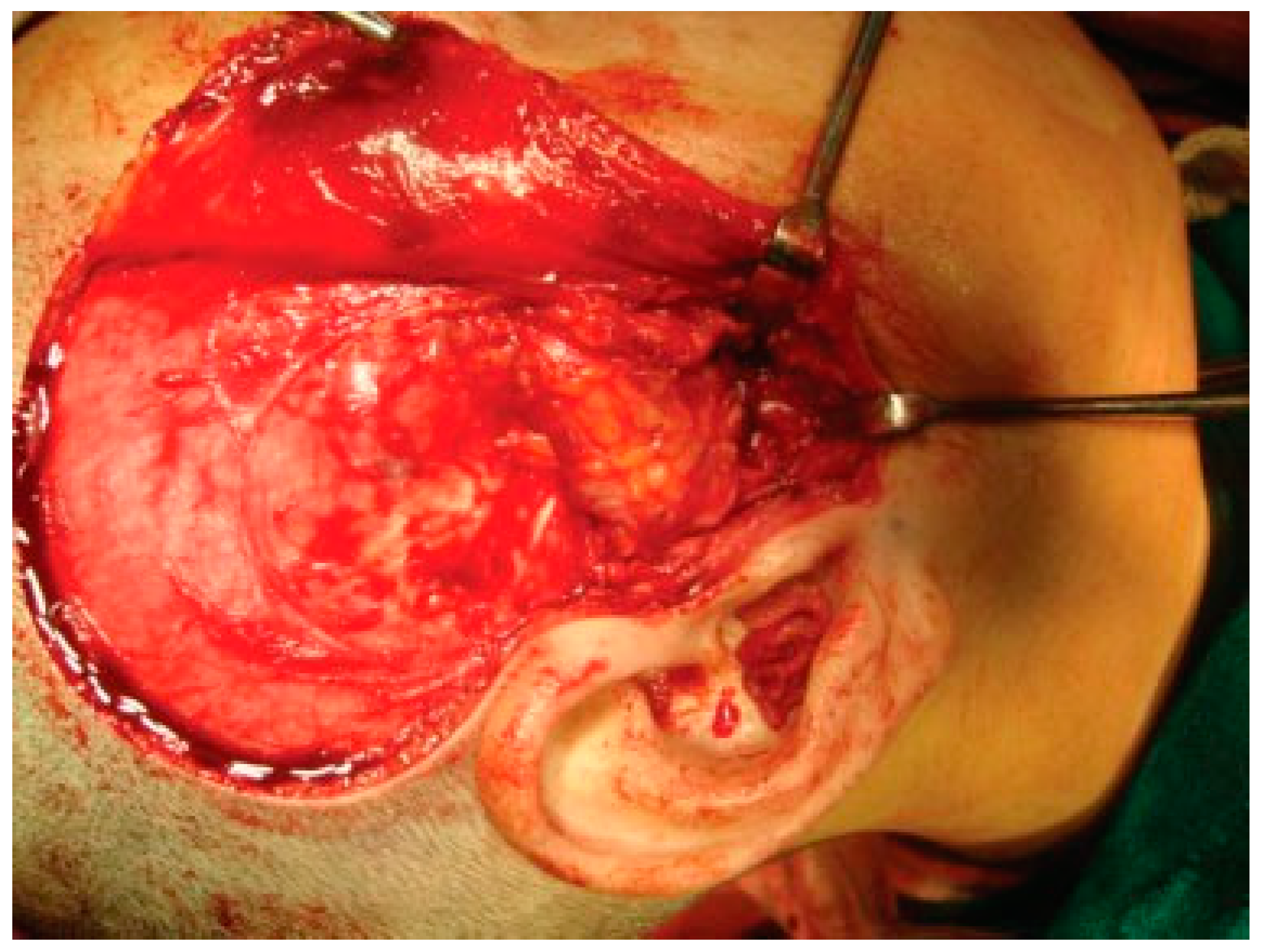
Temporalis muscle was used in seven patients and temporalis fascia was used in two patients. In our series, using temporalis fascia as an interpositional material in the postoperative MIMO was 37 mm. Temporalis fascia has the disadvantage of being thinner, taut, and nonelastic. Long-term follow-up showed premature contact of teeth on the operated side in both the patients and the ramal height was not maintained. When the temporalis muscle was used as interpositional material, we based our flap on one of the branches of deep temporal arteries to maintain its vascularity and the flap was turned over the zygomatic arch and placed into the glenoid fossa. Temporalis muscle provided us with more bulk to obliterate the joint space and was sandwiched between the chondral end of the CCG and temporal bone. After appropriate positioning has been established, the muscle is sutured in both the anterior and posterior directions. Moreover, there is no hematoma formation and hence had better long-term stability. In patients where temporalis muscle was used, the MIMO was 41 mm and ramal height was maintained in all the cases (
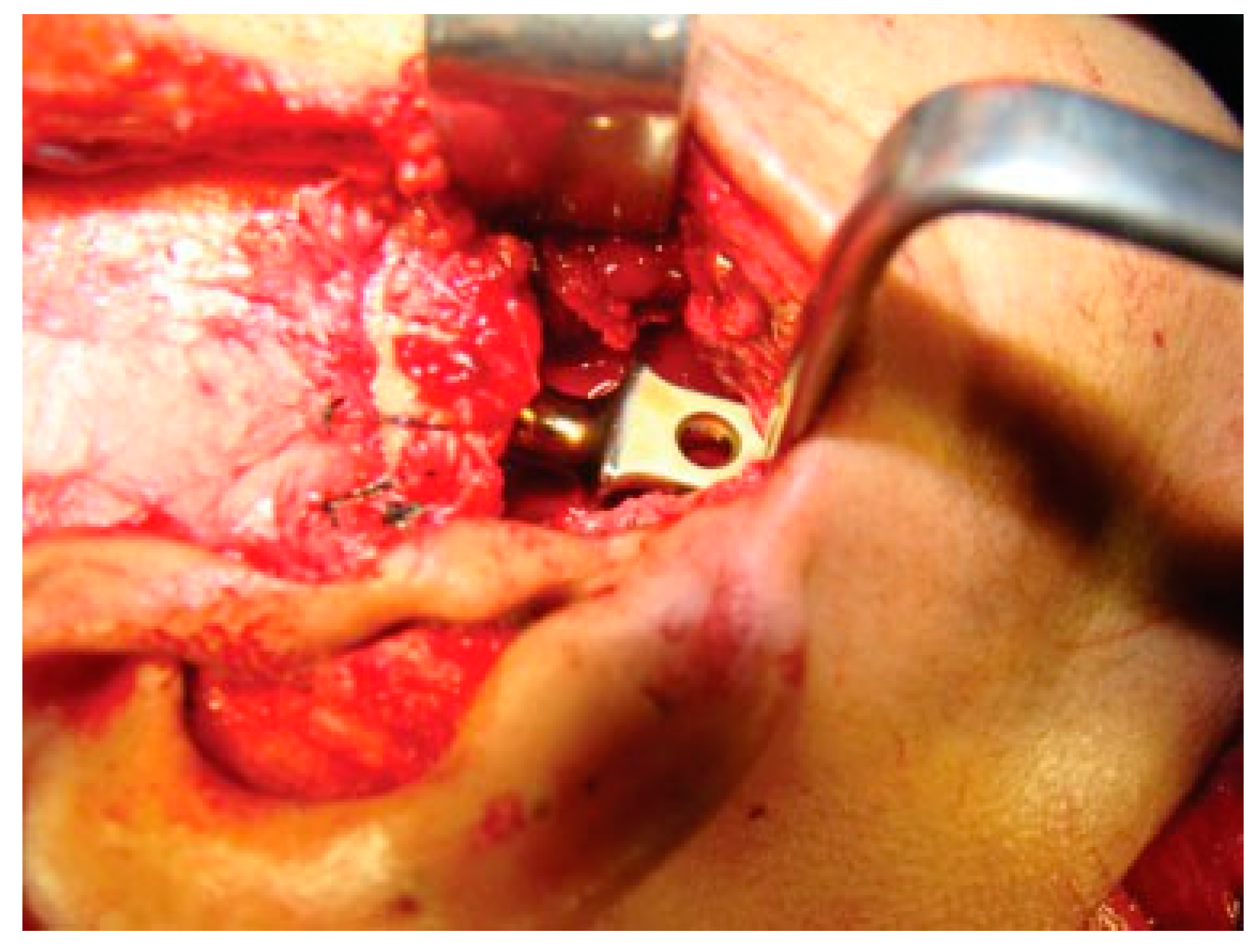
Figure 7 and
Figure 8). The ramal height was preserved in most of our cases possibly due to unilateral ankylosis with compensation by the contralateral mandibular unit. Management of ankylosis in children can be very challenging and our aim was to correct retrognathia in bilateral cases and reduce the possibility of further asymmetry in unilateral cases. Growth center transplantation using CCGs was done in seven growing children in the 6- to 13-year age group. The uses of this biologically compatible autograft in reconstruction are benefits of growth potential and ability to remodel into a neocondyle with time. Unpredictable growth pattern of the CCG, midline shift, and donor site morbidity are some of the disadvantages of this technique. Overgrowth of the graft has been attributed to the use of a large cartilaginous cap; hence, only 1 to 2 mm cartilaginous cap must be used to avoid such complications [
13,
14,
15]. We assessed the same using panoramic radiographs during follow-ups. The CCGs showed excellent mandibular growth along with complete integration of graft into the recipient site over the passage of time in all seven cases. The CCG was harvested from the sixth rib (contralateral side) using submammary incision and was secured using three 2-mm titanium screws at the recipient site. Due to the close proximity of the chondral cartilage to the base of skull, we routinely interposed temporalis muscle in these patients. The muscle pedicle acted as an artificial disc as well as a barrier between the base of skull and chondral cartilage (
Figure 9). Early and vigorous mobilization is important to prevent postoperative adhesions and reankylosis [
16]. The postoperative MIMO in seven patients was 41.5 mm. Asymmetry in the form of deviation of chin was found in one patient during long-term follow-up, where CCG overgrowth led to the deviation of the chin to the contralateral side.
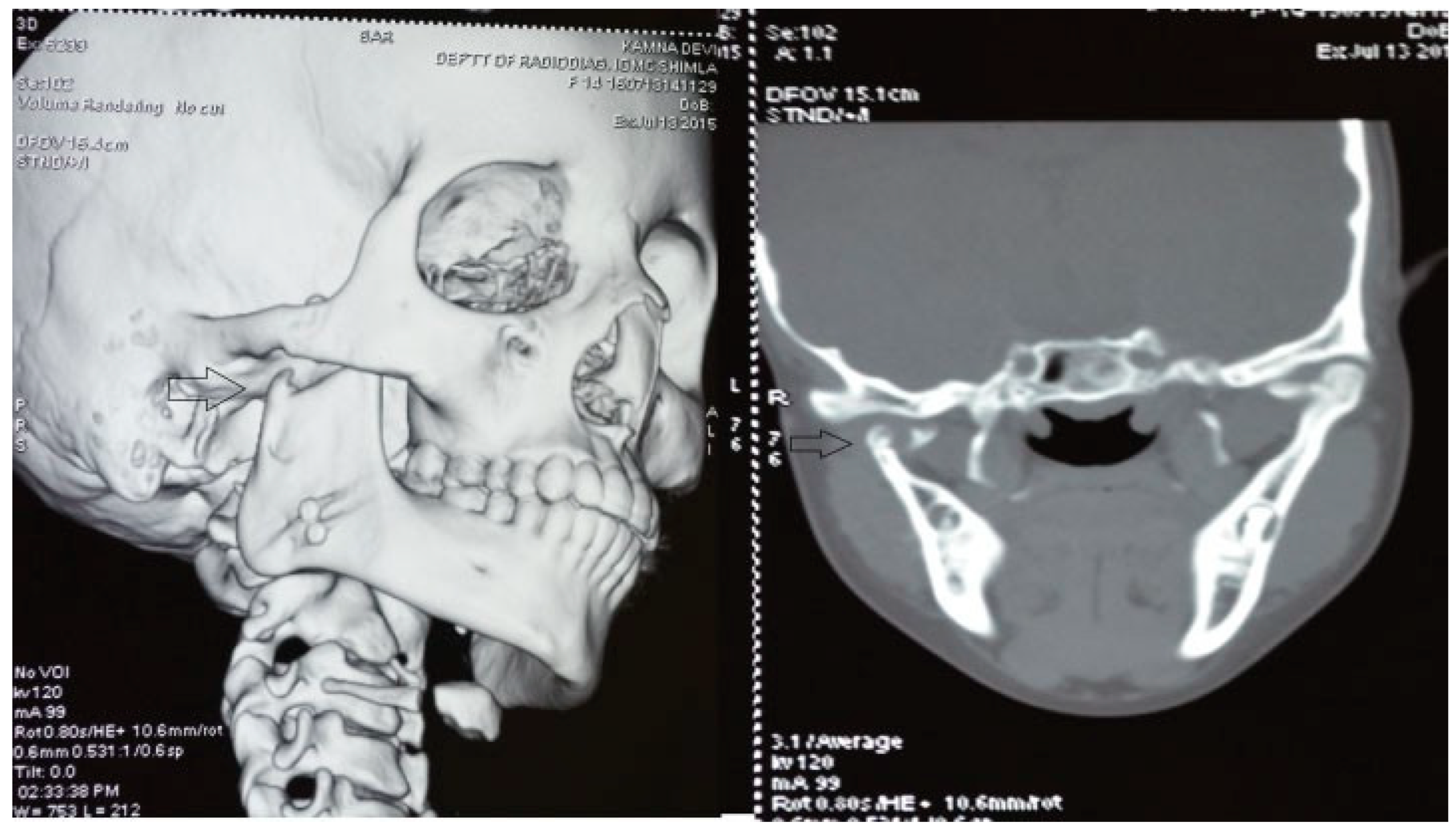
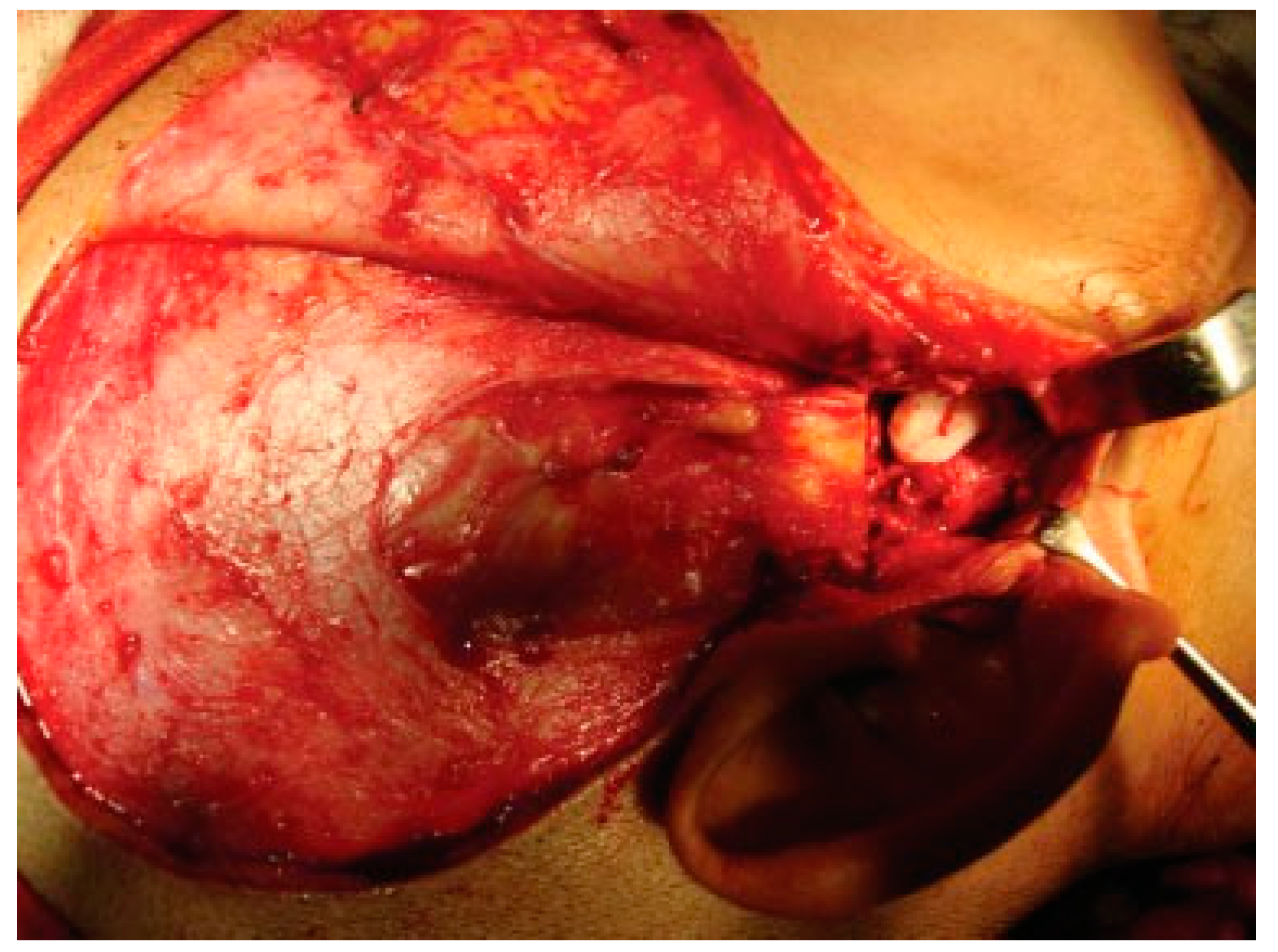
The unique ability of the CCG to remodel into neocondyle could be well appreciated on the digital OPG and CT scan of the patient. The length and width of the neocondyle was very much comparable to the length of the condyle on the unaffected side at 6 years follow-up. Thus, the neocondyle formed using the costochondral cartilage was identical to the unaffected mandibular condyle both structurally and functionally. Poor socioeconomic conditions and lack of awareness coupled with poor primary health care facilities lead many of these unfortunate patients to live with this debilitating condition well into adulthood. Five such adult patients with age ranging from 17 to 36 years reported to us for treatment of TMJ ankylosis. In all these patients, ankylotic bony mass extends beyond the boundaries of the joint capsule. Alloplastic reconstruction after the release of ankylosis was our method of treatment, although high cost of condylar prosthesis led us to use 2.4 mm condylar head reconstruction plate along with temporalis muscle interpositioning in these patients. Interpositional grafts may fail to restore the ramal height in bilaterally ankylosed adult patients, so alloplastic condylar reconstruction may become the preferred choice. Advantages of alloplastic TMJ reconstruction are that the physical therapy can begin immediately, there is no need for a secondary donor site, surgery time is decreased, and alloplasts can be constructed in such a way as to mimic the normal anatomic contours of the structures they are to replace [
17,
18]. Wolford and Karras have suggested autologous fat transplantation as a useful adjunct to prosthetic TMJ reconstruction, as it minimizes the occurrence of excessive joint fibrosis, heterotopic calcification, and improves the range of motion [
19]. However, they have categorically stated in their discussion that heterotopic bone formation is seen in multiple operated joints and joints with previously failed alloplastic implants. Another method to combat heterotopic bone formation is the use of 10 Gy of irradiation in five fractionated daily doses in the immediate postoperative period [
20]. In our series, none of the patients reported with heterotopic bone formation possibly because they had undergone a single surgical procedure for managing TMJ ankylosis. The risk of fossa perforation could have been taken care by interpositioning of temporalis muscle in all these patients.
The vertical ramal height was restored at least on one side using metallic condylar head in cases of bilateral TMJ ankylosis (
Figure 10). Postsurgery, the patients with alloplastic condylar head were more compliant to physiotherapy during the immediate postoperative period possibly due to restoration of anatomy. The range of mandibular movements was recovered earliest and best in cases where alloplastic condylar head was implanted. The postoperative mouth opening was 45.6 mmwhich is maximum in our entire series of 22 patients where increased mouth opening (
p < 0.001;
Table 2 and
Table 3) could be attributed to patients being adult with full development of stomatognathic apparatus as compared with younger patients. Long-term follow-up showed better adaptation because of its ability to conform to the associated bony contours as compared with any other autogenous material used in our series.
Nitzan et al suggested an alternative treatment for Sawhney’s Type III TMJ ankylosis. They suggested the preservation of the medially displaced condyle disc apparatus for an optimal outcome. The condyle disc apparatus maintains inherent joint function, conserves vertical ramus height, and protects the growth site in children [
21]. However, it may be of interest to observe that a medially dislocated condylar stump is not a viable solution biomechanically for functioning of TMJ. Long et al postulated that restoration of the normal structure of the TMJ and by preservation of disc, recurrence of traumatic TMJ ankylosis can be prevented [
22]. Disc repositioning prevents reankylosis and holding the disc in the appropriate position is critical for optimal outcomes in early posttraumatic TMJ ankylosis [
23]. Articular disc was used as an interpositional material in two patients, where CT scan evaluation showed that disc was intact over medially displaced condyle. In both these patients who had Sawhney’s Type III ankylosis, the articular disc was pulled and sutured to lateral aspect of condylar stump. None of these patients showed any evidence of reankylosis on follow-up. Both the patients had a postoperative mouth opening of 36.5 mm. There was no midline shift and the ramal height and occlusion were maintained. Repositioning the disc is successful in early trauma-induced TMJ ankylosis. The condyle disc apparatus maintains inherent joint function, conserves vertical ramus height, and protects the growth site in children [
21,
22,
23].