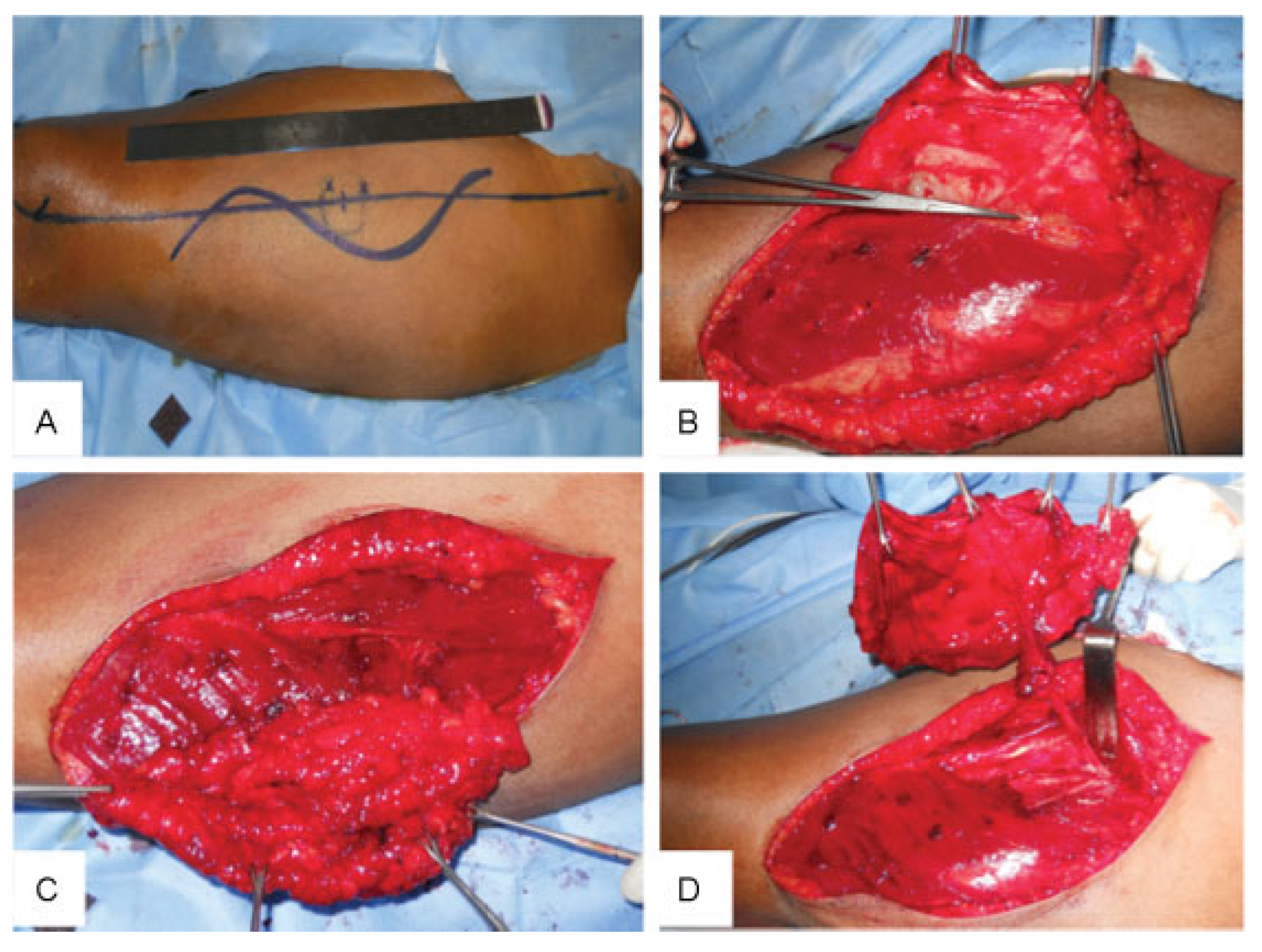
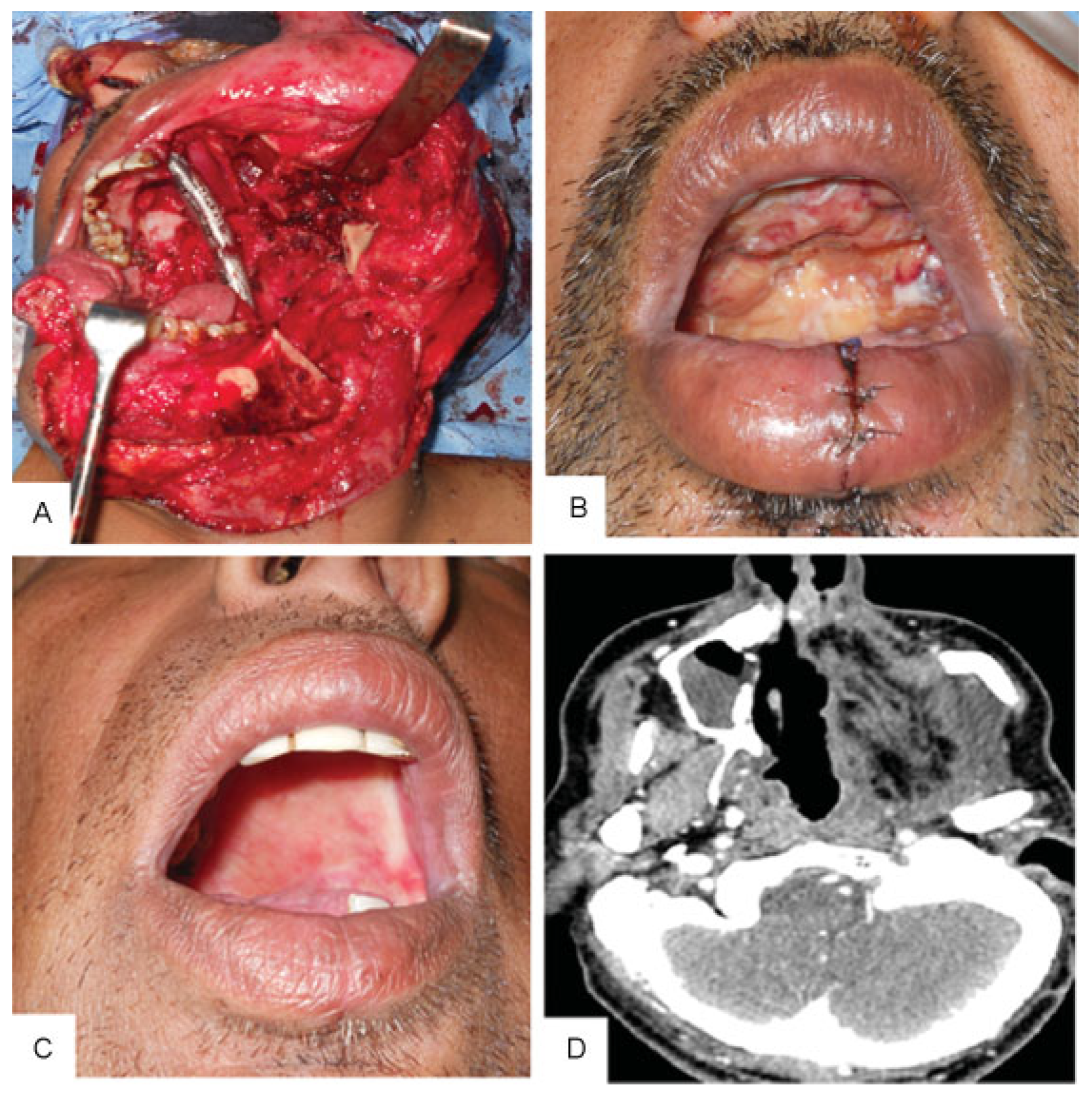
Versatility of Adipofascial Anterolateral Thigh Flap for Reconstruction of Maxillary Defects with Infratemporal Fossa Extension
Abstract
:Patients and Methods
Results
Discussion
Conflict of Interests
References
- Brown, J.S.; Shaw, R.J. Reconstruction of the maxilla and midface: introducing a new classification. Lancet Oncol 2010, 11, 1001–1008. [Google Scholar] [CrossRef]
- Cordeiro, P.G.; Santamaria, E. A classification system and algorithm for reconstruction of maxillectomy and midfacial defects. Plast Reconstr Surg 2000, 105, 2331–2346, discussion 2347–2348. [Google Scholar] [CrossRef]
- Okay, D.J.; Genden, E.; Buchbinder, D.; Urken, M. Prosthodontic guidelines for surgical reconstruction of the maxilla: a classification system of defects. J Prosthet Dent 2001, 86, 352–363. [Google Scholar] [CrossRef]
- Yamamoto, Y.; Kawashima, K.; Sugihara, T.; Nohira, K.; Furuta, Y.; Fukuda, S. Surgical management of maxillectomy defects based on the concept of buttress reconstruction. Head Neck 2004, 26, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Futran, N.D.; Mendez, E. Developments in reconstruction of midface and maxilla. Lancet Oncol 2006, 7, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Kekatpure, V.D.; Manjula, B.V.; Mathias, S.; Trivedi, N.P.; Selvam, S.; Kuriakose, M.A. Reconstruction of large composite buccal defects using single soft tissue flap—analysis of functional outcome. Microsurgery 2013, 33, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Agostini, V.; Dini, M.; Mori, A.; Franchi, A.; Agostini, T. Adipofascial anterolateral thigh free flap for tongue repair. Br J Plast Surg 2003, 56, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Agostini, T.; Agostini, V. Adipofascial versus fasciocutaneous anterolateral thigh flap in oral cavity reconstruction. Focus on the vascular supply. J Plast Reconstr Aesthet Surg 2009, 62, e633–e634. [Google Scholar] [CrossRef] [PubMed]
- Agostini, T.; Agostini, V. Further experience with adipofascial ALT flap for oral cavity reconstruction. J Plast Reconstr Aesthet Surg 2008, 61, 1164–1169. [Google Scholar] [CrossRef] [PubMed]
- Dalgorf, D.; Higgins, K. Reconstruction of the midface and maxilla. Curr Opin Otolaryngol Head Neck Surg 2008, 16, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Genden, E.M.; Wallace, D.I.; Okay, D.; Urken, M.L. Reconstruction of the hard palate using the radial forearm free flap: indications and outcomes. Head Neck 2004, 26, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, B.; Ferri, A.; Ferrari, S.; Copelli, C.; Sesenna, E. Maxillary reconstruction using anterolateral thigh flap and bone grafts. Microsurgery 2009, 29, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Kekatpure, V.D.; Trivedi, N.P.; Shetkar, G.; Manjula, B.V.; Mathan Mohan, A.; Kuriakose, M.A. Single perforator based anterolateral thigh flap for reconstruction of large composite defects of oral cavity. Oral Oncol 2011, 47, 517–521. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, B.; Bertolini, F.; Ferrari, S.; Sesenna, E. Maxillary reconstruction using rectus abdominis free flap and bone grafts. Br J Oral Maxillofac Surg 2006, 44, 526–530. [Google Scholar] [CrossRef] [PubMed]
- Hanasono, M.M.; Skoracki, R.J.; Silva, A.K.; Yu, P. Adipofascial perforator flaps for “aesthetic” head and neck reconstruction. Head Neck 2011, 33, 1513–1519. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Qiao, Q.; Liu, Z.; et al. Free anterolateral thigh adipofascial flap for hemifacial atrophy. Ann Plast Surg 2005, 55, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.H.; Yang, C.C.; Kuo, Y.R.; Tsai, H.H.; Jeng, S.F. Free anterolateral thigh adipofascial perforator flap. Plast Reconstr Surg 2003, 112, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Thankappan, K.; Trivedi, N.P.; Sharma, M.; Kuriakose, M.A.; Iyer, S. Free radial forearm adiposo-fascial flap for inferior maxillectomy defect reconstruction. Indian J Plast Surg 2009, 42, 100–103. [Google Scholar] [PubMed]
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age in y | 53 | 65 | 33 | 40 |
| Gender | M | F | M | M |
| Histology | ACC Palate | SCC palate | Ameloblastoma | ACC palate |
| ITF involvement | Yes | Yes | Yes | Yes |
| Mandibulotomy approach | Yes | No | Yes | Yes |
| Post-op RT | Yes | No | No | Yes |
| Local site complication | No | No | No | No |
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Size (cm2) | 180 | 150 | 150 | 120 |
| Number of perforators | 1 | 1 | 1 | 1 |
| Perforator type | Muscular | Septal | Muscular | Muscular |
| Pedicle | D | D | T | D |
| Donor-site morbidity | None | None | None | None |
| Mouth opening > 4 cm | Yes | Yes | Yes | Yes |
| Oroantral fistula | No | No | No | No |
| Oral diet | Yes | Yes | Yes | Yes |
© 2014 by the author. The Author(s) 2014.
Share and Cite
Kekatpure, V.D.; Hedne, N.; Chavre, S.; Pillai, V.; Trivedi, N.; Kuriakose, M.A. Versatility of Adipofascial Anterolateral Thigh Flap for Reconstruction of Maxillary Defects with Infratemporal Fossa Extension. Craniomaxillofac. Trauma Reconstr. 2014, 7, 213-217. https://doi.org/10.1055/s-0034-1371973
Kekatpure VD, Hedne N, Chavre S, Pillai V, Trivedi N, Kuriakose MA. Versatility of Adipofascial Anterolateral Thigh Flap for Reconstruction of Maxillary Defects with Infratemporal Fossa Extension. Craniomaxillofacial Trauma & Reconstruction. 2014; 7(3):213-217. https://doi.org/10.1055/s-0034-1371973
Chicago/Turabian StyleKekatpure, Vikram D., Naveen Hedne, Sachin Chavre, Vijay Pillai, Nirav Trivedi, and Moni Abraham Kuriakose. 2014. "Versatility of Adipofascial Anterolateral Thigh Flap for Reconstruction of Maxillary Defects with Infratemporal Fossa Extension" Craniomaxillofacial Trauma & Reconstruction 7, no. 3: 213-217. https://doi.org/10.1055/s-0034-1371973
APA StyleKekatpure, V. D., Hedne, N., Chavre, S., Pillai, V., Trivedi, N., & Kuriakose, M. A. (2014). Versatility of Adipofascial Anterolateral Thigh Flap for Reconstruction of Maxillary Defects with Infratemporal Fossa Extension. Craniomaxillofacial Trauma & Reconstruction, 7(3), 213-217. https://doi.org/10.1055/s-0034-1371973



