Managing the Frontal Sinus in the Endoscopic Age: Has the Endoscope Changed the Algorithm?
Abstract
:Why Is Management of the Frontal Sinus so Challenging?
What Might the Endoscope Offer?
- Diagnosis
- Primary treatment
- Delayed intervention
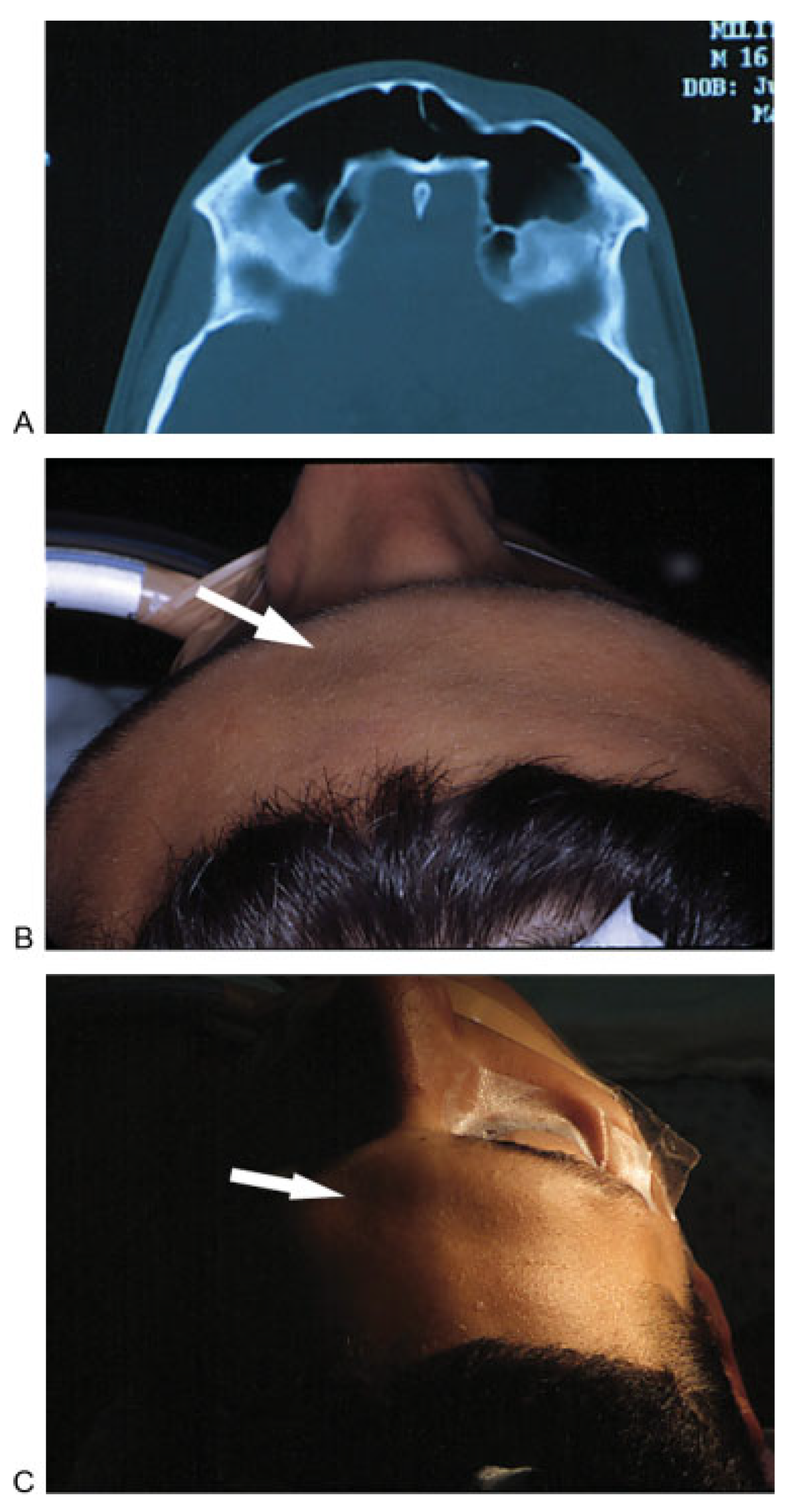
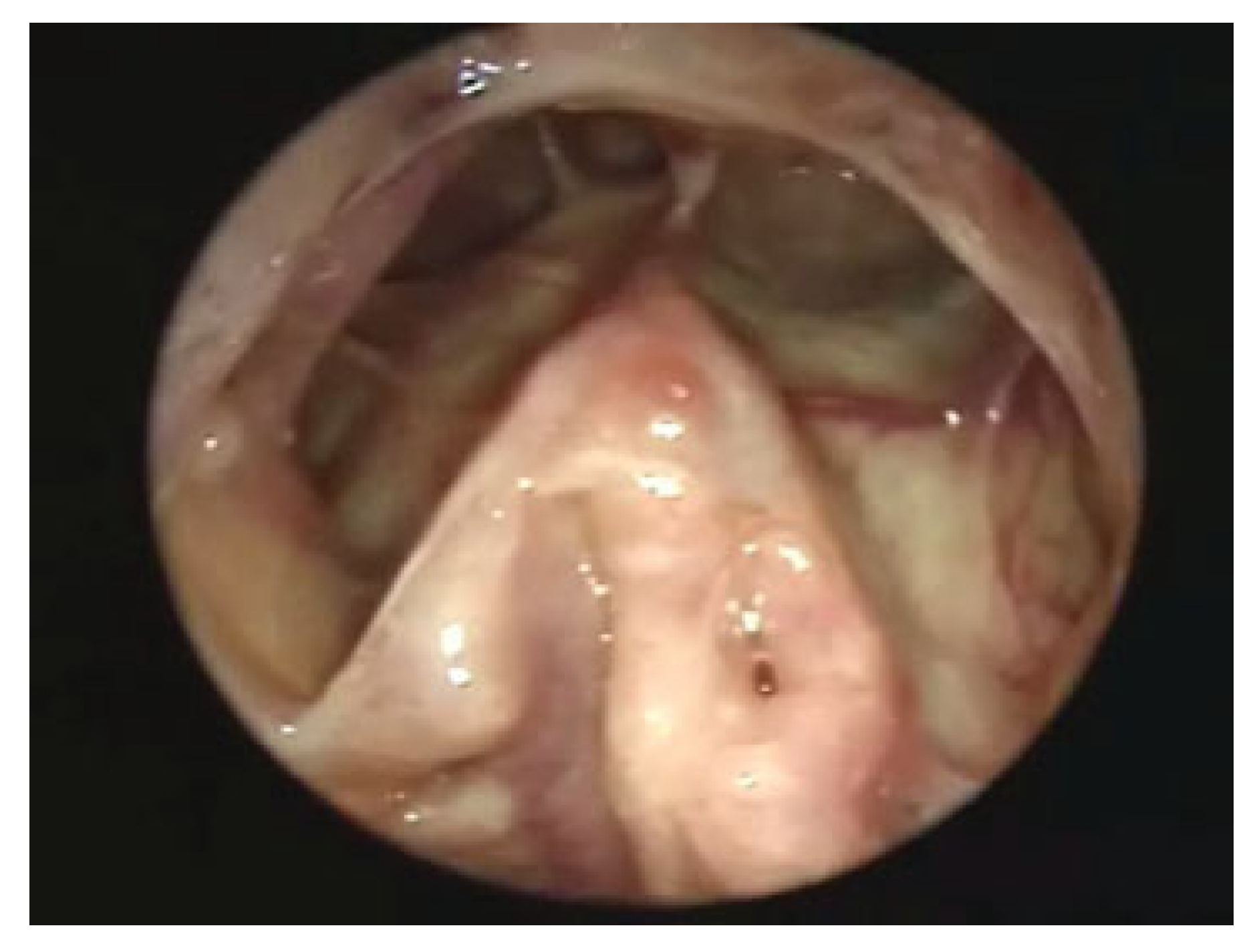
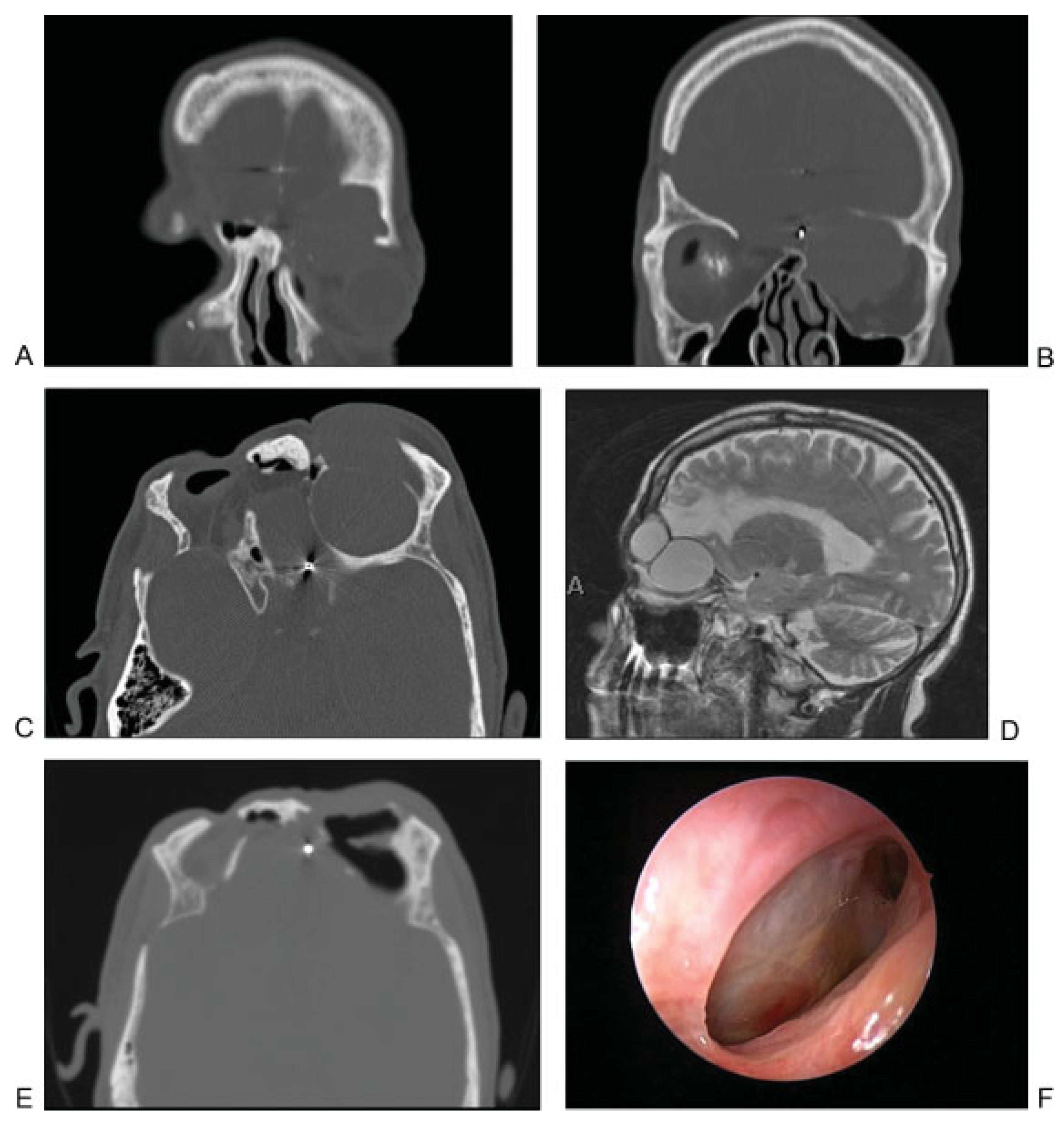
Use of the Endoscope in Diagnosis
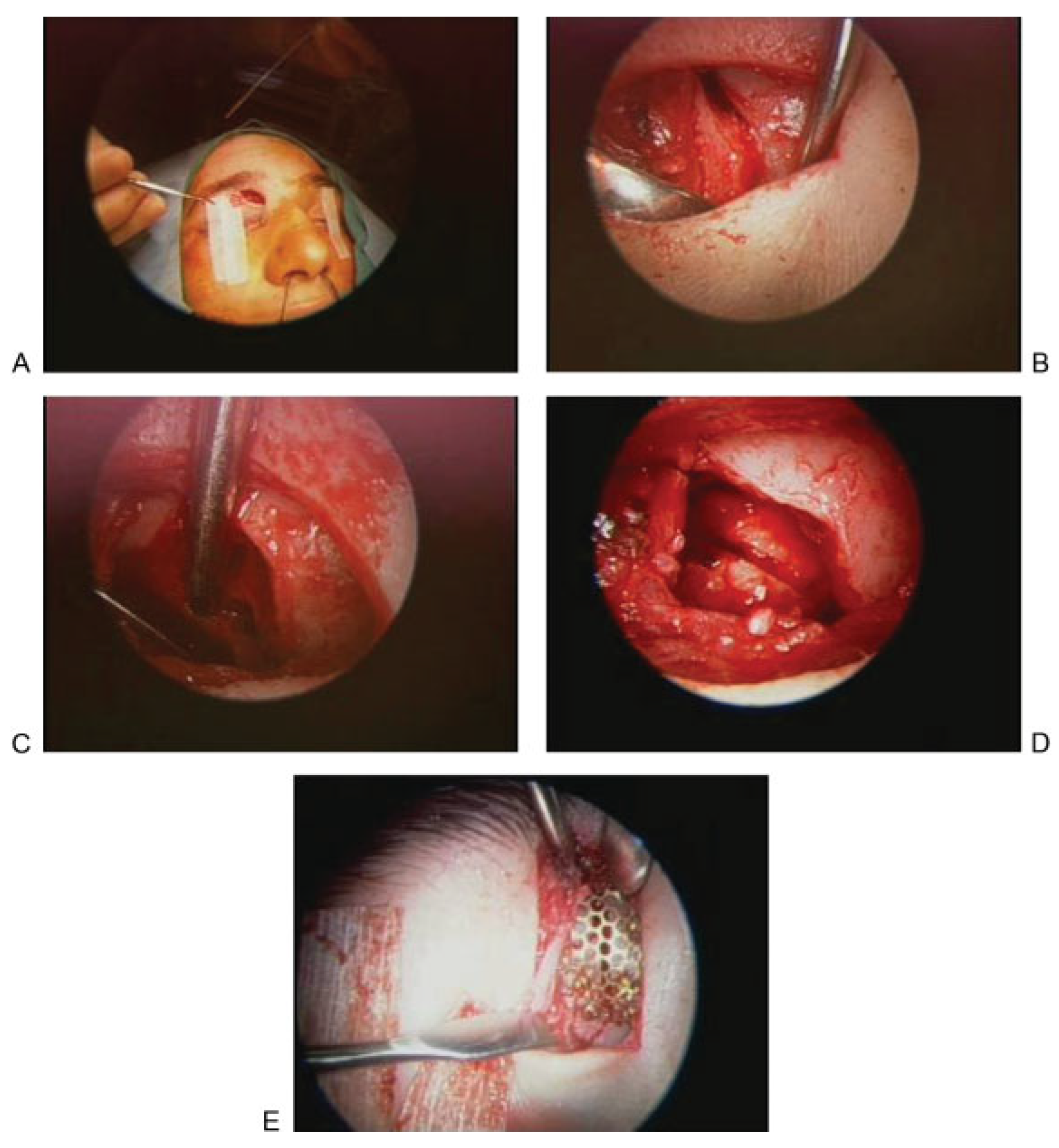
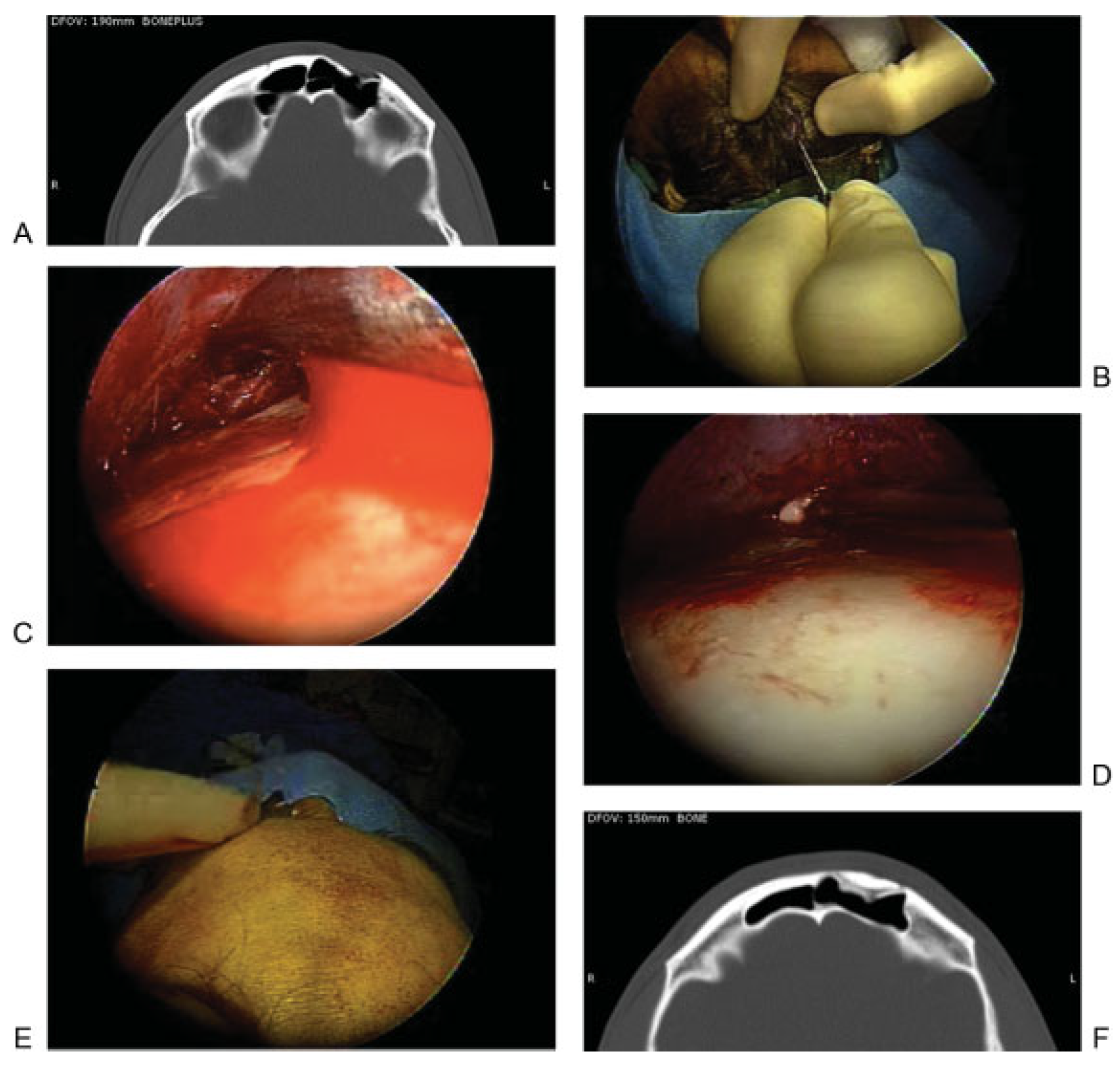
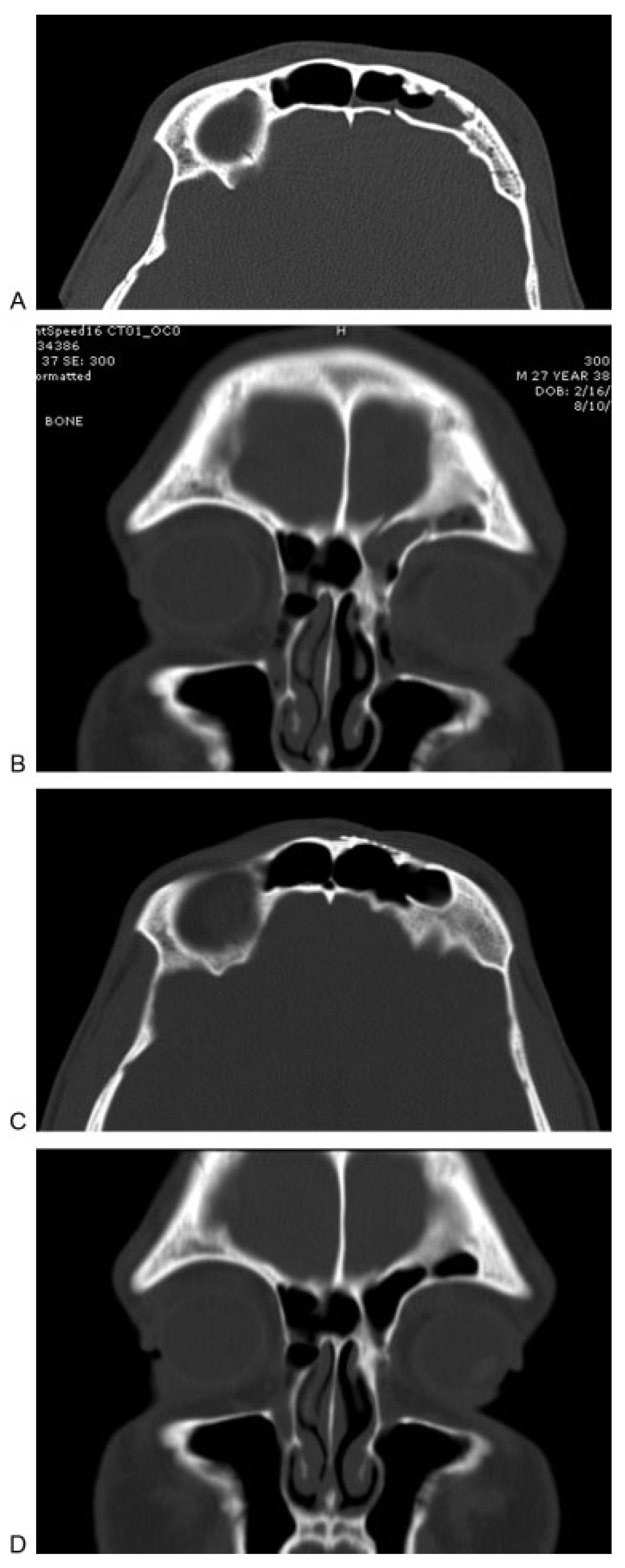
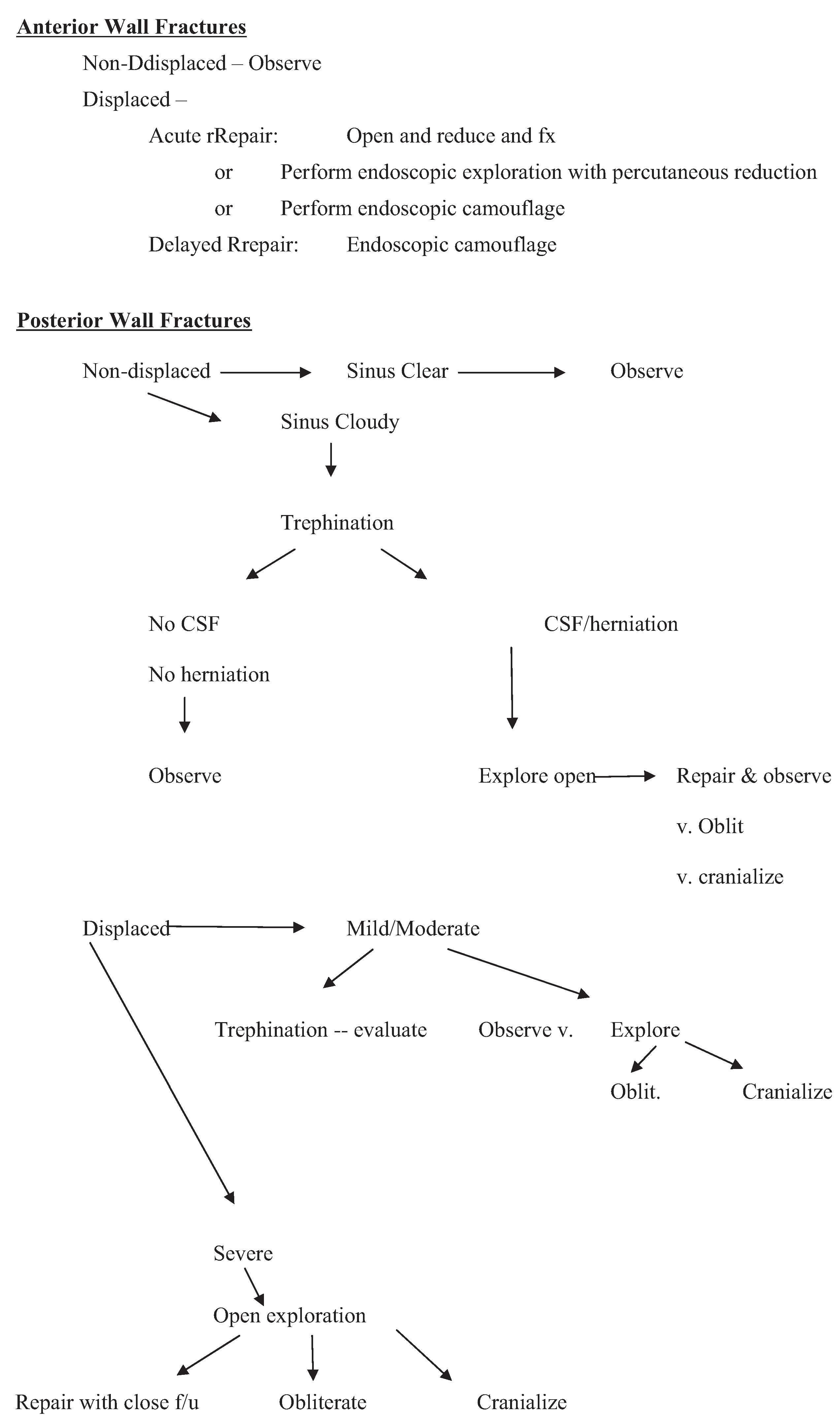
Endoscopic Management of Fractures
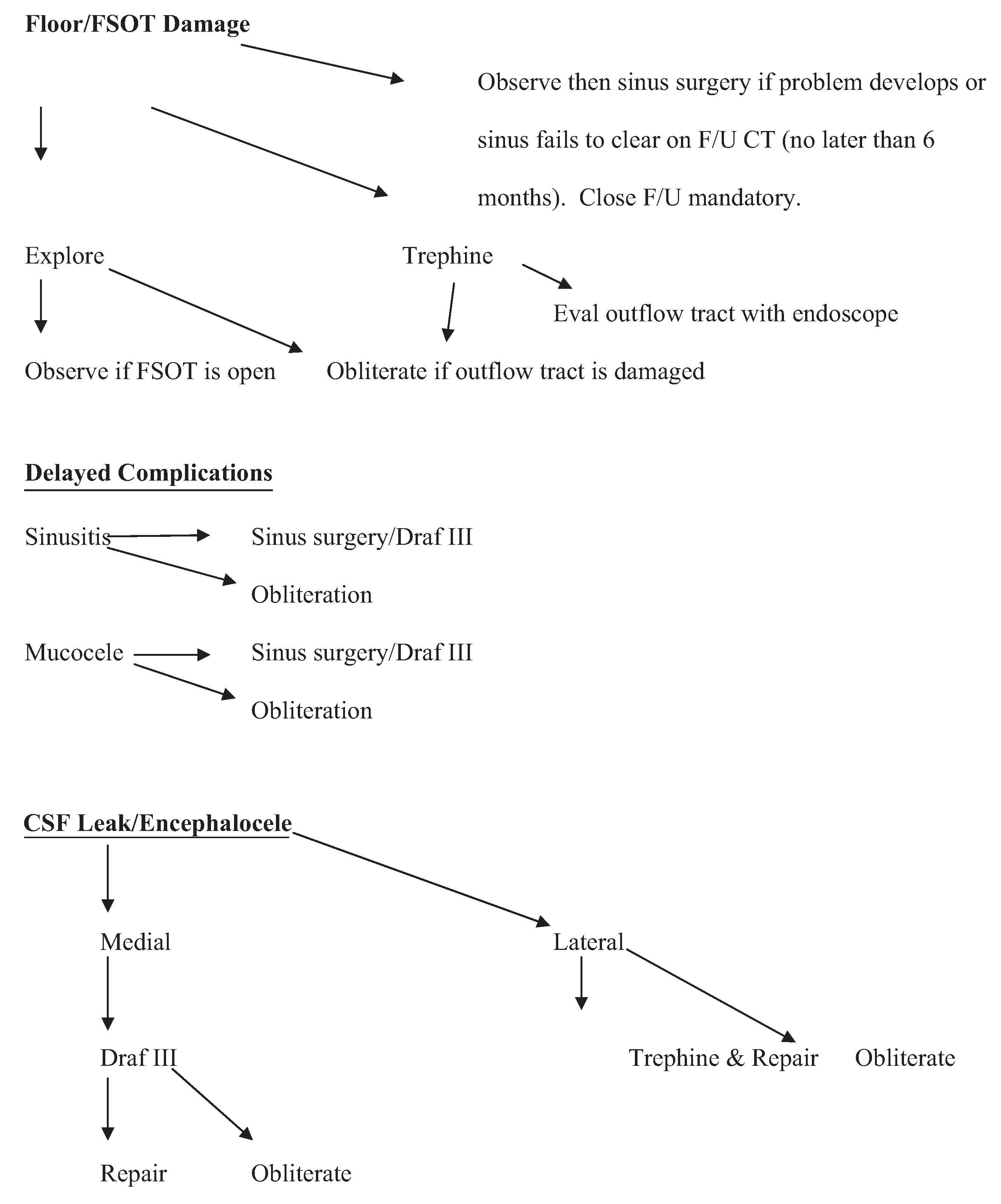
Outflow Tract/Frontal Sinus Outflow Tract Injury
Posterior Wall Defects
New Algorithm in the Endoscopic Age
Conclusion
Notes
References
- Bell, R.B.; Dierks, E.J.; Brar, P.; Potter, J.K.; Potter, B.E. A protocol for the management of frontal sinus fractures emphasizing sinus preservation. J Oral Maxillofac Surg 2007, 65, 825–839. [Google Scholar] [CrossRef]
- Stanley, R.B., Jr.; Becker, T.S. Injuries of the nasofrontal orifices in frontal sinus fractures. Laryngoscope 1987, 97, 728–731. [Google Scholar] [CrossRef] [PubMed]
- Gonty, A.A.; Marciani, R.D.; Adornato, D.C. Management of frontal sinus fractures: a review of 33 cases. J Oral Maxillofac Surg 1999, 57, 372–379, discussion 380–381. [Google Scholar] [CrossRef] [PubMed]
- Gonty, A.A.; Marciani, R.D.; Adornato, D.C. Management of frontal sinus fractures: a review of 33 cases. J Oral Maxillofac Surg 1999, 57, 372–379, discussion 380–381. [Google Scholar] [CrossRef]
- Raveh, J.; Vuillemin, T.; Sutter, F. Subcranial management of 395 combined frontobasal-midface fractures. Arch Otolaryngol Head Neck Surg 1988, 114, 1114–1122. [Google Scholar] [CrossRef]
- Schultz, R.C. Frontal sinus and supraorbital fractures from vehicle accidents. Clin Plast Surg 1975, 2, 93–106. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, E.D.; Stanwix, M.G.; Nam, A.J.; et al. Twenty-six-year experience treating frontal sinus fractures: a novel algorithm based on anatomical fracture pattern and failure of conventional techniques. Plast Reconstr Surg 2008, 122, 1850–1866. [Google Scholar] [CrossRef]
- Metzinger, S.E.; Metzinger, R.C. Complications of frontal sinus fractures. Craniomaxillofac Trauma Reconstr 2009, 2, 27–34. [Google Scholar] [CrossRef]
- Swinson, B.D.; Jerjes, W.; Thompson, G. Current practice in the management of frontal sinus fractures. J Laryngol Otol 2004, 118, 927–932. [Google Scholar] [CrossRef]
- Rohrich, R.J.; Hollier, L.H. Management of frontal sinus fractures. Changing concepts. Clin Plast Surg 1992, 19, 219–232. [Google Scholar] [CrossRef]
- Rohrich, R.J.; Hollier, L. The role of the nasofrontal duct in frontal sinus fracture management. J Craniomaxillofac Trauma 1996, 2, 31–40. [Google Scholar] [PubMed]
- Weber, R.; Draf, W.; Keerl, R.; et al. Osteoplastic frontal sinus surgery with fat obliteration: technique and long-term results using magnetic resonance imaging in 82 operations. Laryngoscope 2000, 110, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.T.; Chen, C.T.; Mardini, S.; Tsay, P.K.; Chen, Y.R. Frontal sinus fractures: a treatment algorithm and assessment of outcomes based on 78 clinical cases. Plast Reconstr Surg 2006, 118, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Crozier, D.L.; Hwang, P.H.; Goyal, P. The endoscopic-assisted trephination approach for repair of frontal sinus cerebrospinal fluid leaks. Laryngoscope 2013, 123, 321–325. [Google Scholar] [CrossRef]
- Strong, E.B. Endoscopic repair of anterior table frontal sinus fractures. Facial Plast Surg 2009, 25, 43–48. [Google Scholar] [CrossRef]
- Steiger, J.D.; Chiu, A.G.; Francis, D.O.; Palmer, J.N. Endoscopic-assisted reduction of anterior table frontal sinus fractures. Laryngoscope 2006, 116, 1978–1981. [Google Scholar] [CrossRef]
- Kellman, R.M. Endoscopy in craniomaxillofacial surgery. Facial Plast Surg 2009, 25, 1. [Google Scholar] [CrossRef]
- Hybels, R.L.; Newman, M.H. Posterior table fractures of the frontal sinus: I. An experimental study. Laryngoscope 1977, 87, 171–179. [Google Scholar] [CrossRef]
- Smith, T.L.; Han, J.K.; Loehrl, T.A.; Rhee, J.S. Endoscopic management of the frontal recess in frontal sinus fractures: a shift in the paradigm? Laryngoscope 2002, 112, 784–790. [Google Scholar] [CrossRef]
- Carter, K.B., Jr.; Poetker, D.M.; Rhee, J.S. Sinus preservation management for frontal sinus fractures in the endoscopic sinus surgery era: a systematic review. Craniomaxillofac Trauma Reconstr 2010, 3, 141–149. [Google Scholar] [CrossRef]
- Har-El, G. Endoscopic management of 108 sinus mucoceles. Laryngoscope 2001, 111, 2131–2134. [Google Scholar] [CrossRef] [PubMed]
- Sautter, N.B.; Citardi, M.J.; Perry, J.; Batra, P.S. Paranasal sinus mucoceles with skull-base and/or orbital erosion: is the endoscopic approach sufficient? Otolaryngol Head Neck Surg 2008, 139, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Woodworth, B.A.; Schlosser, R.J.; Palmer, J.N. Endoscopic repair of frontal sinus cerebrospinal fluid leaks. J Laryngol Otol 2005, 119, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Jones, V.; Virgin, F.; Riley, K.; Woodworth, B. Changing paradigms in frontal sinus cerebrospinal fluid leak repair. Int Forum Allergy Rhinol 2012, 2, 227–232. [Google Scholar] [CrossRef]
- Chen, D.J.; Chen, C.T.; Chen, Y.R.; Feng, G.M. Endoscopically assisted repair of frontal sinus fracture. J Trauma 2003, 55, 378–382. [Google Scholar] [CrossRef]
- Hueman, K.; Eller, R. Reduction of anterior frontal sinus fracture involving the frontal outflow tract using balloon sinuplasty. Otolaryngol Head Neck Surg 2008, 139, 170–171. [Google Scholar] [CrossRef]
- Chaaban, M.R.; Conger, B.; Riley, K.O.; Woodworth, B.A. Transnasal endoscopic repair of posterior table fractures. Otolaryngol Head Neck Surg 2012, 147, 1142–1147. [Google Scholar] [CrossRef]

| Author | Number of patients | Summary | Findings |
|---|---|---|---|
| Smith et al. [19] | 7 | Patients with frontal sinus fractures suspected of outflow tract injury were managed medically with antibiotics and follow-up imaging studies. | 5 of 7 patients had aerated frontal sinuses on follow-up. 2 patients with obstruction underwent endoscopic sinus surgery and had restoration of frontal sinus patency on follow-up. |
| Chen et al. [25] | 7 | Patients with depressed anterior table fractures were treated with endoscopic browlift approach and microplate fixation of the fractures. | All patients underwent successful reduction and fixation with microplates. |
| Steiger et al. [16] | 5 | Fractures with depression of anterior table were treated with reduction by way of frontal sinusotomy or frontal sinus trephination. | All had good cosmetic outcomes and all had patent and functional frontal sinuses based on CTs performed 2 months after surgery. |
| Hueman and Eller [26] | 1 | Endoscopic balloon sinuplasty was performed to reduce an anterior table fracture with involvement of the frontal outflow tract. | Successful reduction was performed. Follow-up imaging showed good reduction and aeration of the frontal sinus. |
| Chaaban et al. [27] | 13 | 12 patients with skull base defects from posterior table fractures were managed with Draf 2B (1 with concurrent trephination). One patient was managed with Draf 3. | All patients were repaired successfully with septal flap and/or free tissue grafts. One required revision frontal sinusotomy. |
| Crozier et al. [14] | 2 | 2 patients with skull base defects from posterior table fractures were managed using an endoscopic assisted trephination technique. | Both patients underwent successful repair using bone and/or mucosal grafts. |
© 2014 by the author. The Author(s) 2014.
Share and Cite
Kellman, R.; Goyal, P. Managing the Frontal Sinus in the Endoscopic Age: Has the Endoscope Changed the Algorithm? Craniomaxillofac. Trauma Reconstr. 2014, 7, 203-212. https://doi.org/10.1055/s-0034-1371773
Kellman R, Goyal P. Managing the Frontal Sinus in the Endoscopic Age: Has the Endoscope Changed the Algorithm? Craniomaxillofacial Trauma & Reconstruction. 2014; 7(3):203-212. https://doi.org/10.1055/s-0034-1371773
Chicago/Turabian StyleKellman, Robert, and Parul Goyal. 2014. "Managing the Frontal Sinus in the Endoscopic Age: Has the Endoscope Changed the Algorithm?" Craniomaxillofacial Trauma & Reconstruction 7, no. 3: 203-212. https://doi.org/10.1055/s-0034-1371773
APA StyleKellman, R., & Goyal, P. (2014). Managing the Frontal Sinus in the Endoscopic Age: Has the Endoscope Changed the Algorithm? Craniomaxillofacial Trauma & Reconstruction, 7(3), 203-212. https://doi.org/10.1055/s-0034-1371773



