Discussion
Beyond dispute, fractures of the mandibular condyle are considered to be most frequent among the different fracture locations of the mandible, with incidences reported between 17.5 and 50%. [
1] In contrast to fractures of the cranial vault, skull base, and midfacial fractures, the management of fractures of the mandibular condylar process will usually be performed first of all by oral and maxillofacial surgeons, less frequently by plastic or otolaryngology-head and neck surgeons. Though one might expect these specialists with experience in the field of mandibular traumatology therefore to be fairly familiar with the special anatomical site of the condylar process, nevertheless competencies and specific anatomical knowledge of this surgically demanding area vary considerably both on a national and an international level. This may first of all be due to the varying educational systems, as the indication for closed or open treatment of condylar process fractures is a highly controversial subject and has not been currently agreed upon. Whereas the conservative (i.e., nonsurgical) treatment of condylar process fractures is based on a centuries-old tradition, the first experiences with open surgery made in the 1920s were associated with a high rate of severe complications, such as facial nerve palsies, pseudarthrosis, and ankylosis. [
8] These major drawbacks explain why nonsurgical treatment modalities remained the undisputed therapy of choice until late in the 1980s or even 1990s of the last century. This strictly conservative viz. nonsurgical approach to condylar process fractures still prevails in less specialized trauma centers as well as in many departments of oral and maxillofacial surgery even nowadays. On the other hand, those surgeons following a nonsurgical treatment regime were not able to get familiar with the specific anatomy and the surgical aspects associated with specific fracture patterns of the condylar process, especially in the condylar neck and head region. Until the 1950s, osteosynthesis techniques kept on being based on wire sutures, thus hampering the progress of open reduction until the introduction of functionally stable osteosynthesis proce-dures for the condylar process including the condylar neck region, such as by miniplates or lag screws, [
9,
10,
11] allowing for the first time an immediate mobilization of the temporoman-dibular joint. Over the last two decades there has been a continuous advancement of osteosynthesis techniques and materials, improving the functional outcome of open reduction and internal fixation. This also benefitted the refinement of surgical approaches to the fractures as well as the techniques for reposition and functionally stable osteosynthesis, thus largely improving the surgeons’ understanding of the anatomical injury patterns. In 2006 a first multicenter study was able to demonstrate that both objective functional results and patients’ comfort were significantly better following open reduction. [
4] Today, surgeons have a broad spectrum of safe surgical approaches at hand, such as the periangular, retromandibular, transparotideal, preauricular, and retroauricular as well as the transoral approach, [
12] allowing a sufficient localization and exposure of condylar base, neck, and head fractures, which is mandatory for correct anatomical reposition and the application of stable osteosynthesis methods. This grand advancement in condylar process traumatology, however, was also largely due to the advancements in X-ray imaging, with CT enhancement and immediate availability in the emergency rooms allowing a significantly better preoperative evaluation of the fracture lines and position of the fragments. Currently, an orthopantomogram in combination with a computerized tomogram (obligatory coronal and axial view, preferably supplemented by a sagittal view) are considered as “golden standard” in condylar process fracture diagnostics and allow more difficult diagnoses to be made, especially regarding condylar head fractures, the latter one’s going often undiagnosed in the pre-CT era. CT or recently also cone beam CT offer differentiated sectional images, allowing assessing fracture height and rather precise degree of angulation, displacement or dislocation. 3D reconstructions facilitate a proper classification, especially for the upper neck and head region.
Last but not the least, this improvement in preoperative X-ray imaging, in combination with corresponding anatomical knowledge gained by increasing indications for open surgery, also took great intuence upon the current classification of condylar process fractures, which in turn is a prerogative for an appropriate handling of the fractures of the mandibular condyle.
The wide range of classifications coexisting on an international level makes comparison between treatment outcomes profoundly challenging. [
3] Mc Lennan and Glas [
13] proposed aclassification differentiating between extra- and intra-articular fractures. The apprehension of the topography and morphology of condylar head fractures, however, has dramatically improved with the advent of CT-imaging techniques. In essence condylar head fractures turned out as shearing fractures with a typical sagittal course in a laterocranial to a mediocaudal direction. The traditional distinction between an intra-and extracapsular location to delineate a condylar head fracture therefore is no more valid, as fractures through the condylar head have been shown to encroach on extracapsular bony portions on the medial or dorsal aspect of the condylar neck. Based on surgical experiences, as already in the early 1990s, Rasse [
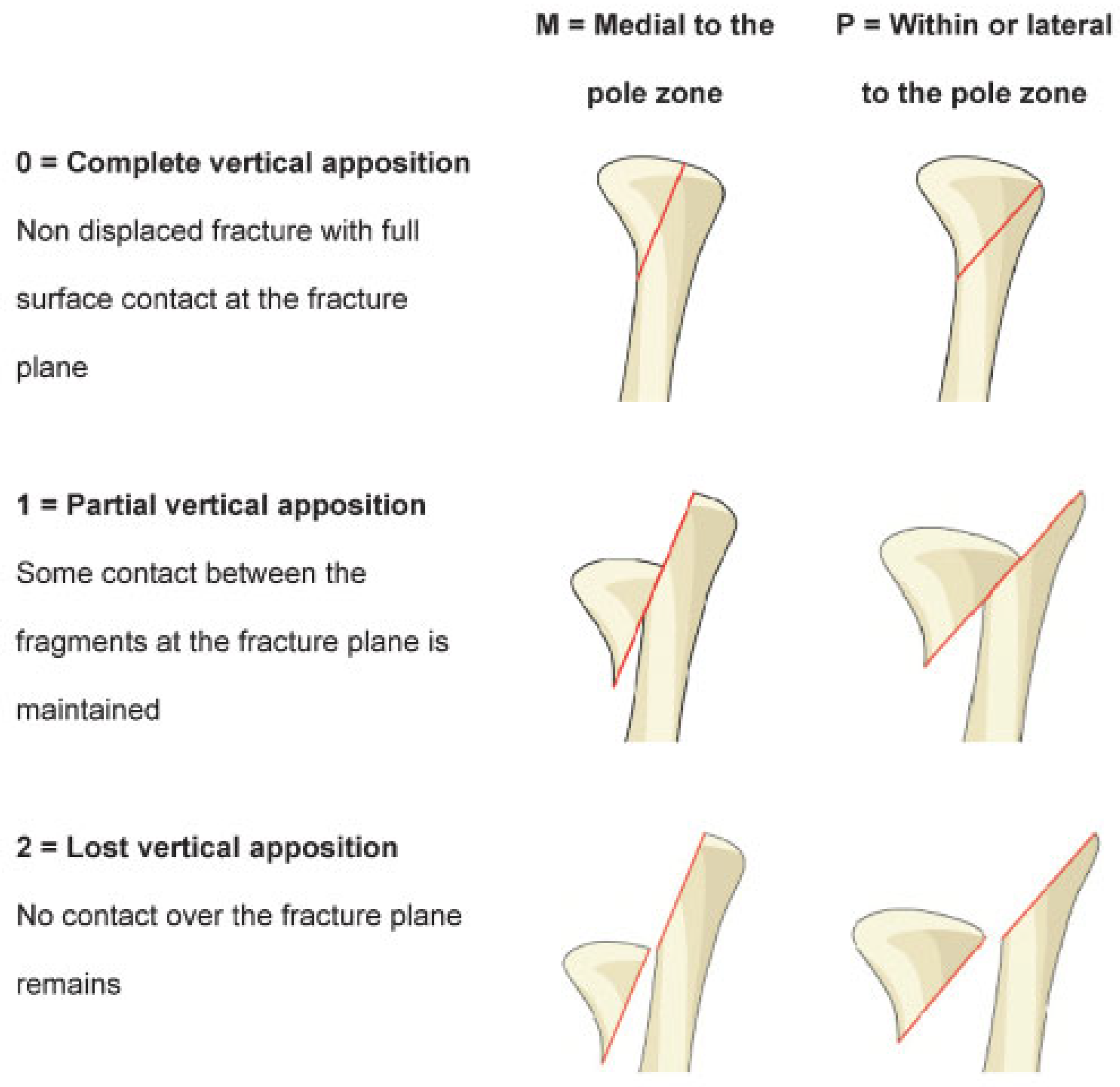
14] was able to show in a CT-based study, that fractures of the condylar head typically present both intra- and extra-articular fracture lines and therefore coined the term of diacapitular fracture. If the medial fragment in condylar head fractures undergoes a displacement it follows—almost without exception—a stereotypic pathway. According to its vector the lateral pterygoid muscle pulls it out of the glenoid fossa into an anteromedial position. Since the medial fragment leaves the glenoid fossa a displaced condylar head fracture represents a dislocation fracture. Equally, every displacement of the medial condylar head fragment is associated with a displacement out of the fossa. Nevertheless, condylar head fractures are still frequently referred to as intracapsular fractures, most probably due to a lack of knowledge of the corresponding anatomical site. In this context, a further point for repetitive confusion especially in the German speaking countries lies in the homonymic term “dislocation” and the German
Dislokation, which means “displacement.” Basically, the English classification terms regarding malposition of condylar process fractures are deviation, displacement, and dislocation, with displacement describing just a deviation of the proximal fragment, while the shifted fragments are still more or less in contact. Displacement (German term
Dislokation) means loss of contact of the fragments, with a condyle to fossa relation that remains basically intact, whereas dislocation describes the exarticulation of the condyle-bearing fragment out of the fossa (German term
Luxation). For the clinician, however, this classification regarding malposition is of utmost importance for the decision-making regarding nonsurgical versus surgical therapy of condylar process fractures.
In the past, there have already been multiple attempts to classify the fractures of the mandibular condylar process according to their anatomical position. Köhler distinguished fractures of the head, subcondylar fractures, as well as medium and deep condylar neck fractures at the level of the sigmoid notch. [
15] Reichenbach identified high and deep condylar neck fractures. [
16] Wassmund related fractures also to the cause of trauma with vertical collum fractures including fractures of the condylar head, transversal, and diagonal condylar neck fractures. [
17] It is noteworthy that these elder classifications were primarily based on conventional radiological X-rays [
18] and were not calibrated by surgical experiences, especially for the neck and head region. Nevertheless, a basic classification according to anatomical criteria has always been in general use among clinicians. In 1977 Lindahl and Hollender proposed a trendsetting classification, subdividing the condylar process according to the height of the fracture as fractures of the “condylar head,” the “condylar neck,” and the “subcondylar region.” [
18] This classification was standardized in 2005 by Loukota et al according to defined anatomical landmarks, subdividing the condylar process now more precisely into fractures of the condylar base, fractures of the condylar neck and diacapitular [
4] or fractures of the condylar head, respectively. [
19] Nevertheless, the degree of displacement or dislocation, which are decisive from a surgical point of view, are not represented in this widely accepted and reproducible classification. Whereas classifications with regard to the insertion of the lateral pterygoid muscle, [
20,
21] failed to establish themselves, the classification according to Spiessl and Schroll [
22] has made its way into clinical and scientific use, differentiating between low or high condylar fractures without displacement, with displacement or dislocation, respectively, and condylar head fractures. Though the Spiessl and Schroll classification is coming increasingly into use, for example, for comparative studies, [
5] it does not allow a precise assessment of the degrees of angulation, displacement or dislocation and fails to specify defining borderlines between low or high fractures. As precise definitions of high and deep fractures were missing, Loukota et al—with special regard to the Spiessl and Schroll basic discrimination of “low” versus “high” fractures—defined the sigmoid notch as the point of determination between the high (neck) and low (base) condylar process. [
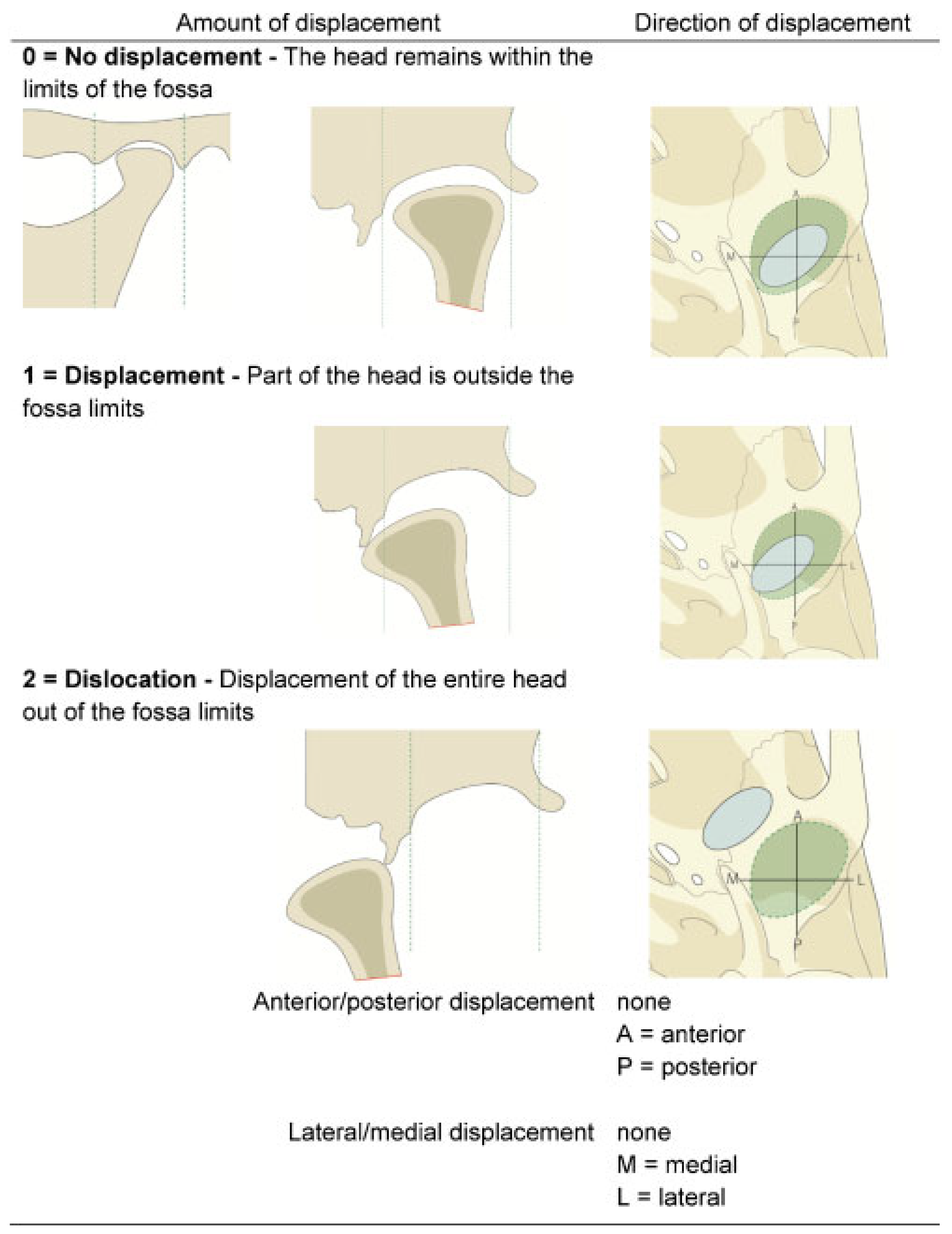
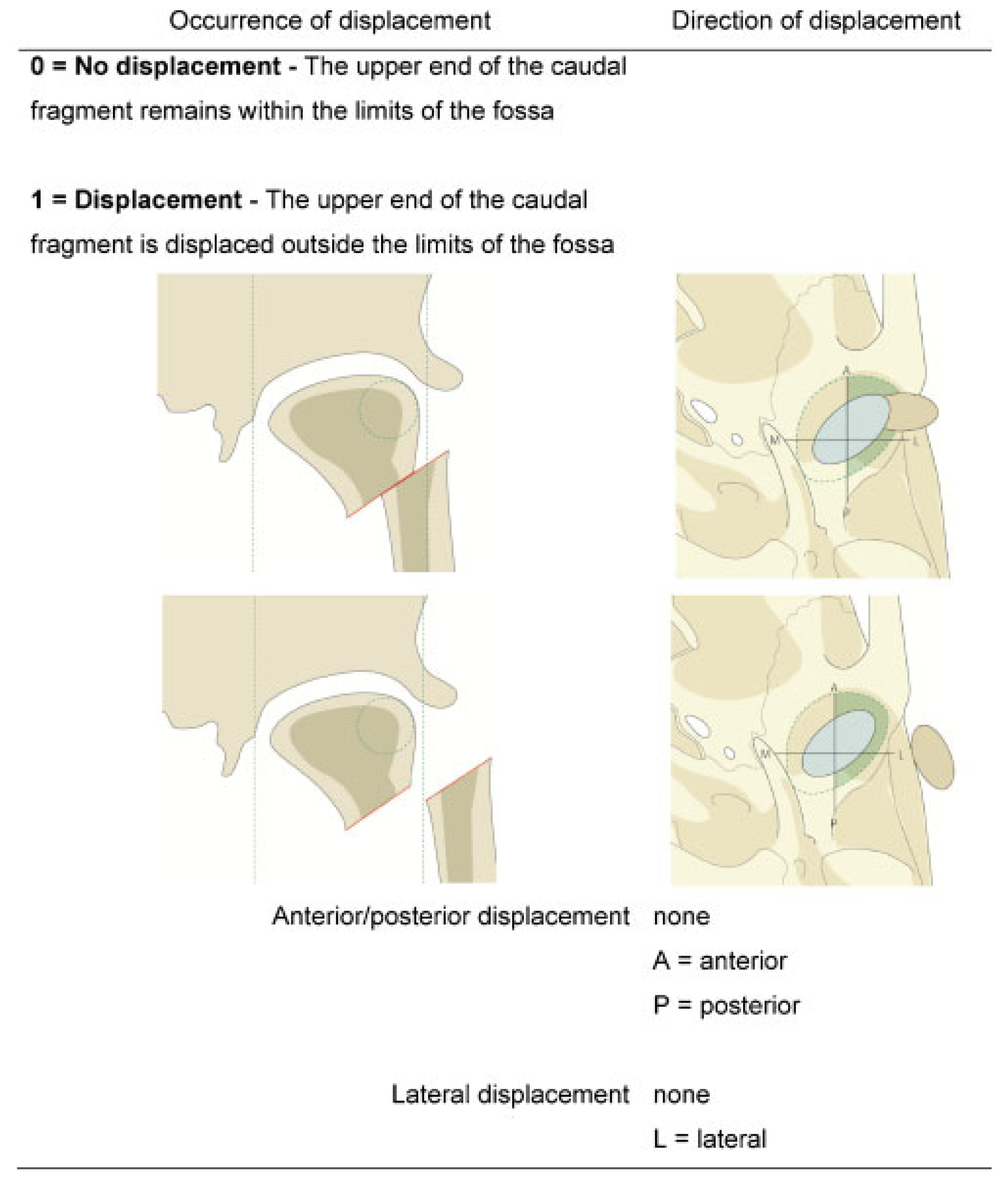
4] Furthermore, the above mentioned current classifications do not explicitly demarcate the direction of displacement or dislocation (medially, laterally, ventrally, and dorsally), with medial or lateral displacement of the small fragment being a major factor for the clinical decision-making, for example, regarding extraoral versus transoral approaches to the condylar base and lower neck.
As far as the condylar head region is concerned, Rasse’s diacapitular classification [
14] was widened out following augmenting surgical experience with fractures of the temporomandibular joint. Considering common surgical procedures and aspects of indication for diacapitular and fractures in proximity to the lateral ligament, Neff et al [
23] included the latter ones into the entity of head fractures. Under prognostic considerations head fractures were further basically subdi-vided into fractures with or without loss of vertical height. [
19,
23] Further subclassifications were introduced regarding anatomical fracture locations of the head [
23,
24] and comminution. [
25] Though the treatment of condylar process fractures, and even more so of the condylar head area is still a highly controversial topic, the enormous developments in this field over the last two decades has led to a shift of the focus of interest to the surgical approaches and the discussion of optimized osteosynthesis methods. As long as conservative (i.e., nonsurgical) or functional treatment was applied uniformly to all fractures of the condylar process or at last the whole of condylar neck and head fractures with displacement or dislocation, the specific fracture pattern remained more or less a matter of academic interest or the purpose of documentation. At present, with efficient and stable osteosyn-thesis methods and even new materials at hand, an up to date classification of the condylar process must meet the following demands, first of all from a clinical point of view, though should also remain based on essential biological characteristics, that is, fracture topography and morphology. [
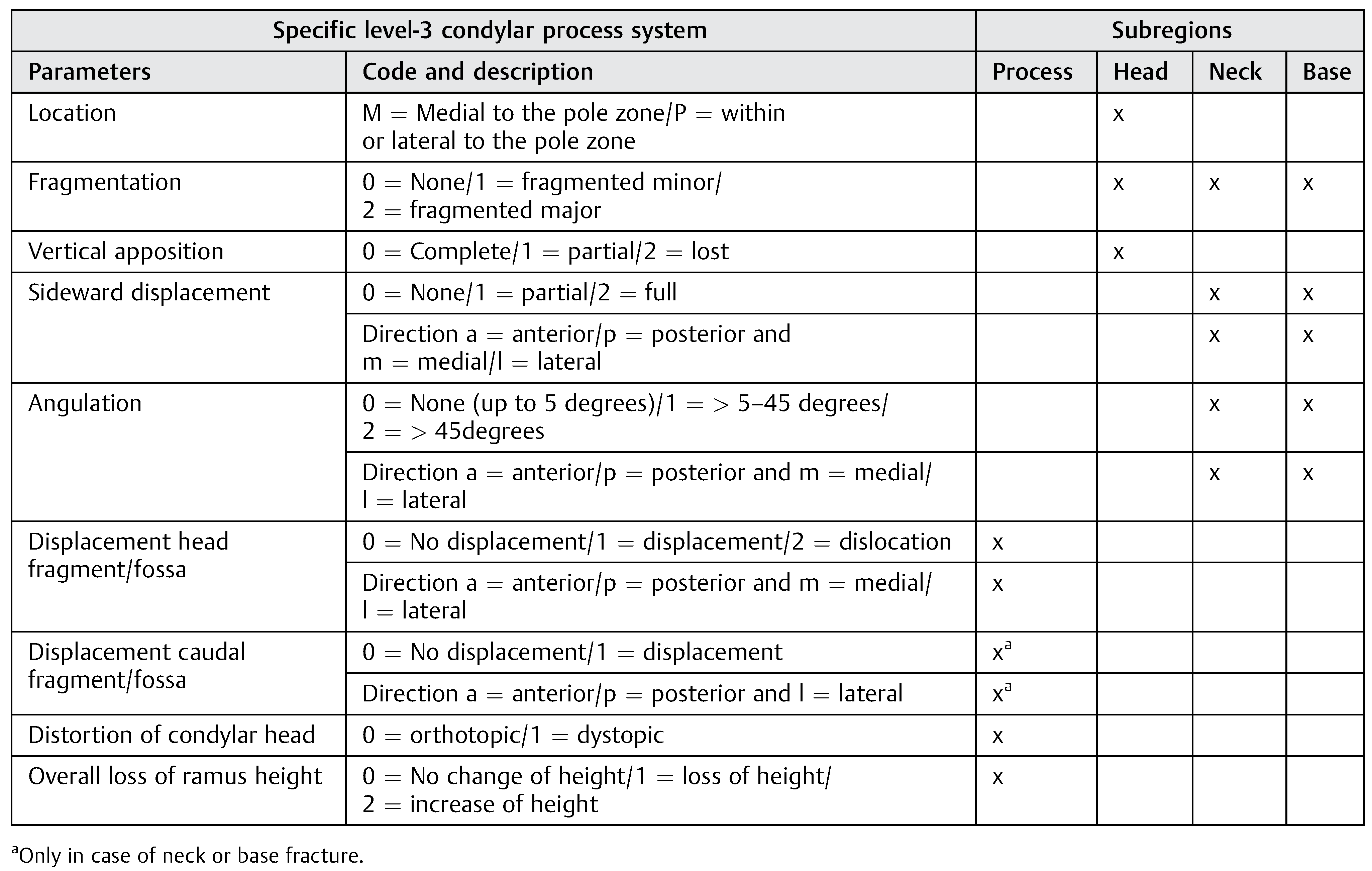
26]
Precise anatomical description of the fracture level location with regard to the selection of the best fitting approach and also osteosynthesis method, that is, which will allow best visualization and application of a stable osteosynthesis (e.g., the preauricular or retroauricular approach for high condylar neck and head fractures, the anteroparotideal/transparotideal or conditionally the retromandibular approach for lower neck fractures, the angular, retromandibular or the transoral approach where appropriate for base fractures) but also timing of nonsurgical or functional treatment regimes.
Assessment of the direction of displacement of the proximal fragment (first of all medially or laterally) in condylar base and neck fractures with regard to the selection of fractures amenable to osteosynthesis via transoral approaches.
Information about the amount of vertical height reduction, the degree of angulation (deviation) or dislocation under prognostic aspects and for the decision-making of closed or open treatment.
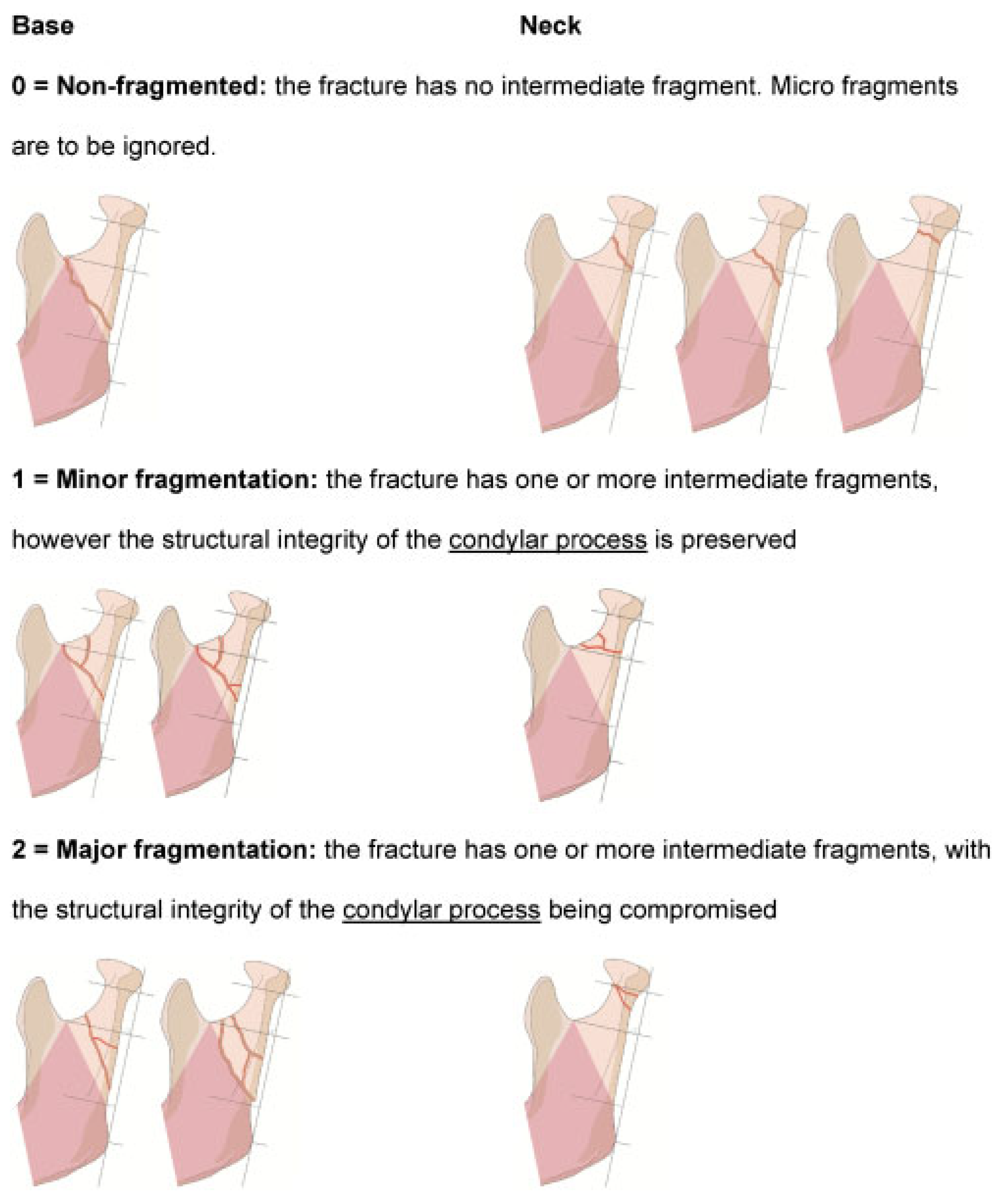
Provision of specifying information with regard to the selection of adequate nonsurgical or osteosynthesis procedures or the overall functional outcome after closed or open treatment, such as major or minor fragmentation or alterations of the condyle to fossa relation.
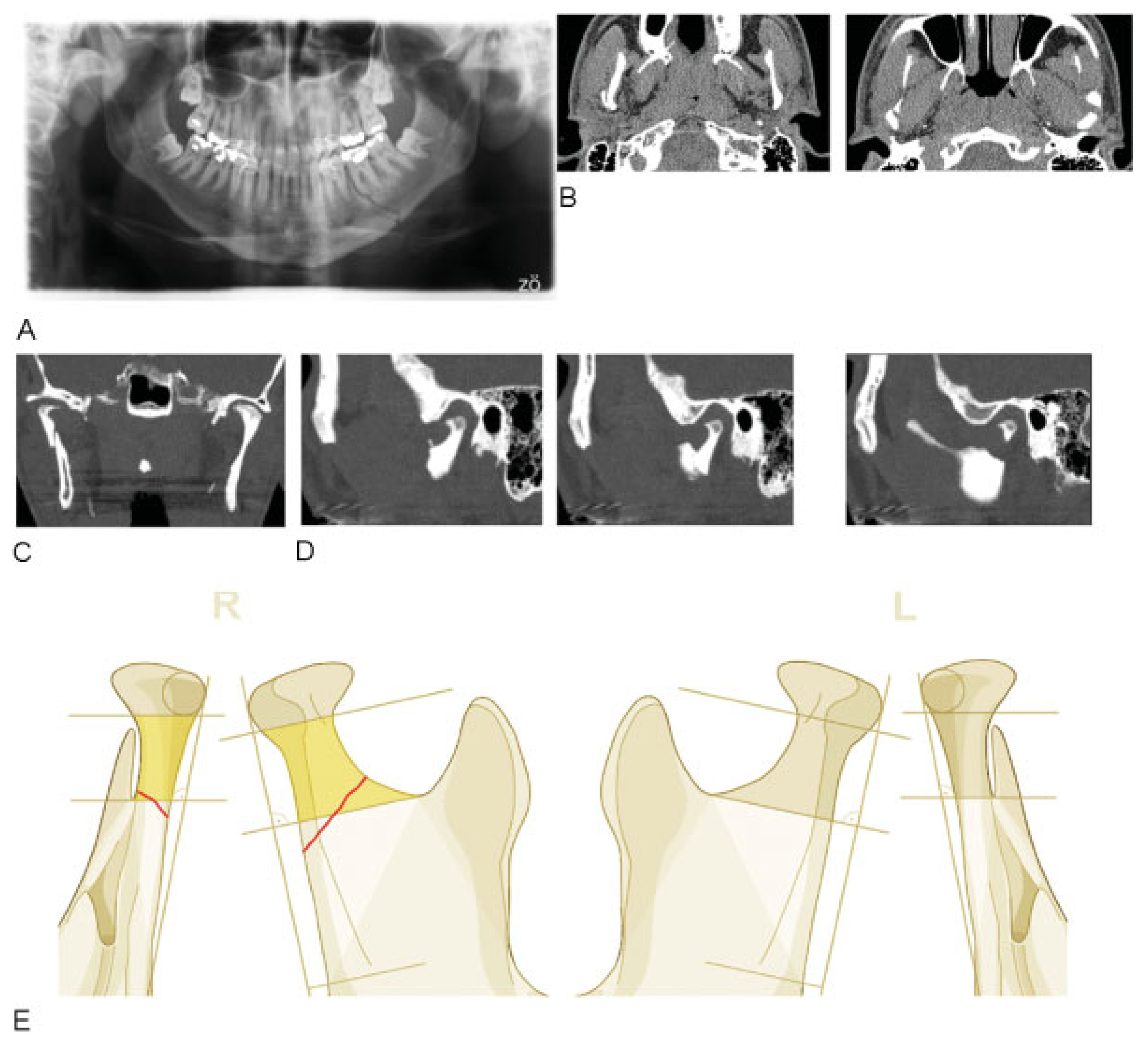
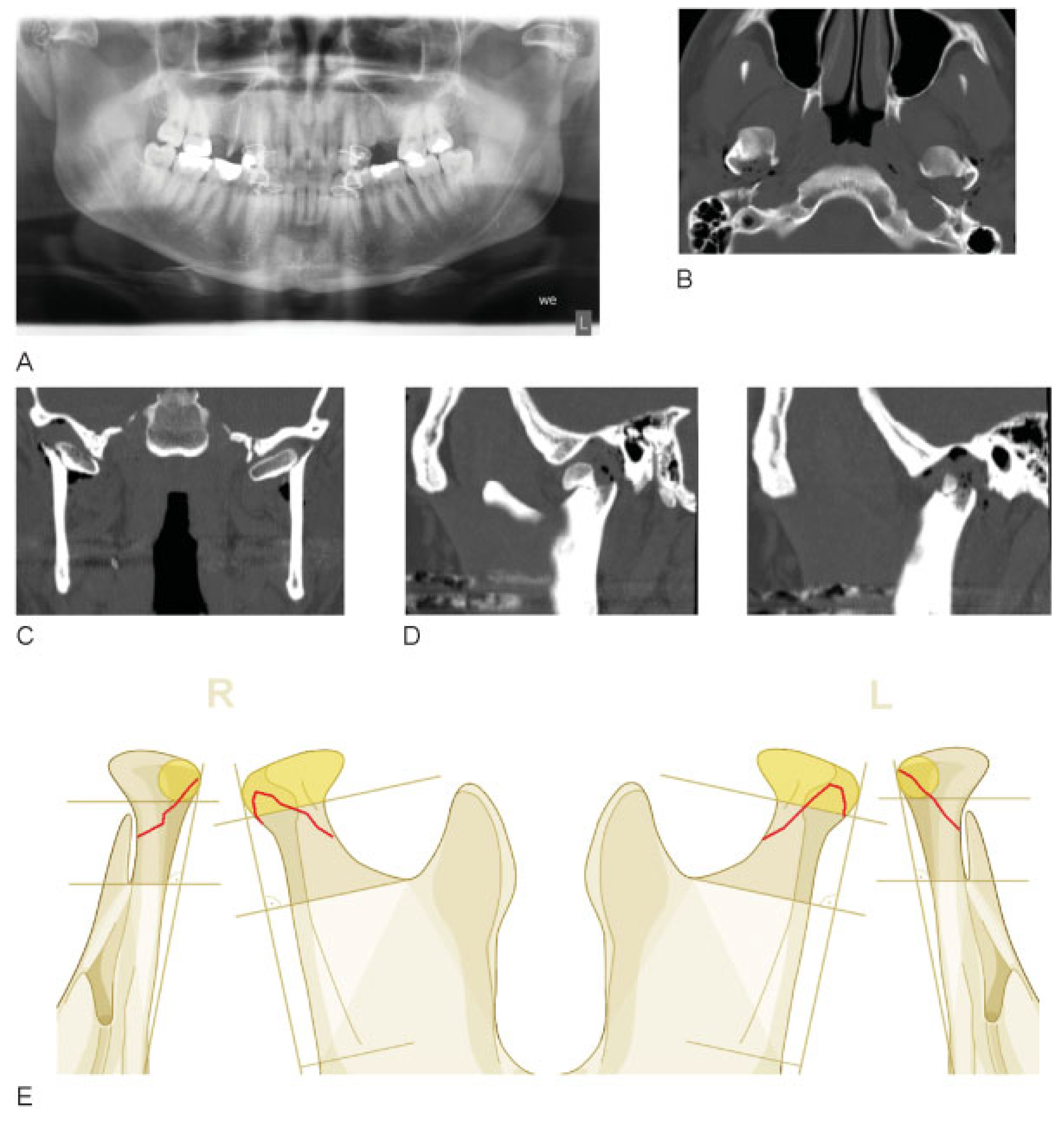
One of the early essential experiences during the assessment sessions was the necessity to demand a rather high level regarding the minimum requirements for diagnostic images. The classification group had agreed on CT scans (1–2 mm slices) in standard 2D format in axial, coronal, and sagittal reconstruction. In addition a panorex and open mouth Townes view with both condyles visible were to be provided (alternatively a 3D-CT reconstruction). For assessment of rotation of the condylar head an axial CT scan or axial cone beam CT (or radiographic axial skull base view) were mandatory. As conventional X-rays are progressively less available in case of modern CT diagnostics as an emergency room standard, especially panorex was often missing. Alternative up to date 3D reconstructions, however, were not suited for exact metric measurements, for example, assessing the loss of vertical ramus height. Alternatively, in CT sagittal scans, for example, measurement of vertical loss to some degree depends on the selected slices and thus, such as in 3D CT due to lack of measurement instruments of the Digital Imaging and Communications in Medicine (DICOM)-viewer, makes it difficult to define the Loukota line, which however is crucial for defining base and neck fractures and is unfortunately more or less basically panorex based. As panorex will be even less available in the future as a standard in trauma cases in favor of CT imaging, the Loukota line urgently needs a CT-based equivalent in the near future. A similar problem was also evident in an initial attempt to distinguish between high (viz. upper) versus low condylar neck fractures. However, due to high diagnosis inconsistency, the group participants agreed to remove this differentiation from the classification system. The differentiation of condylar neck fractures against condylar head fractures required clear definitions. It was generally agreed that panorex X-rays and 3D CT are required, and must be done on the AP view.
As soon as the fracture line involves the area above the condylar head reference, the fracture was defined as a head fracture, which was basically differentiated as within the pole zone or medial to the pole zone. Consensus was achieved that in case of fragmentation the clinically most relevant location (i.e., the lateral pole zone in head fractures) should be considered. This process was accompanied by more precise definitions of minor and major fragmentation (the latter one being synonymous with the classical meaning of the term “comminution”).
Some atypical fractures were responsible for disagreement among the group members, such as fractures with a vertical fracture pattern involving several levels of the condylar process (see borderline cases in the appendix case collection [
7]). Such fractures involving the condylar head and extending vertically to the condylar neck (potentially even involving the base) can be found in about 5 to 7% of all condylar head and neck fractures. [
27] The proposed coding system allows for unambiguous identification of these single fractures instead of a double fracture pattern of both head and neck. This is consistent with the rest of the mandibular system when fractures extend over several regions. [
2]
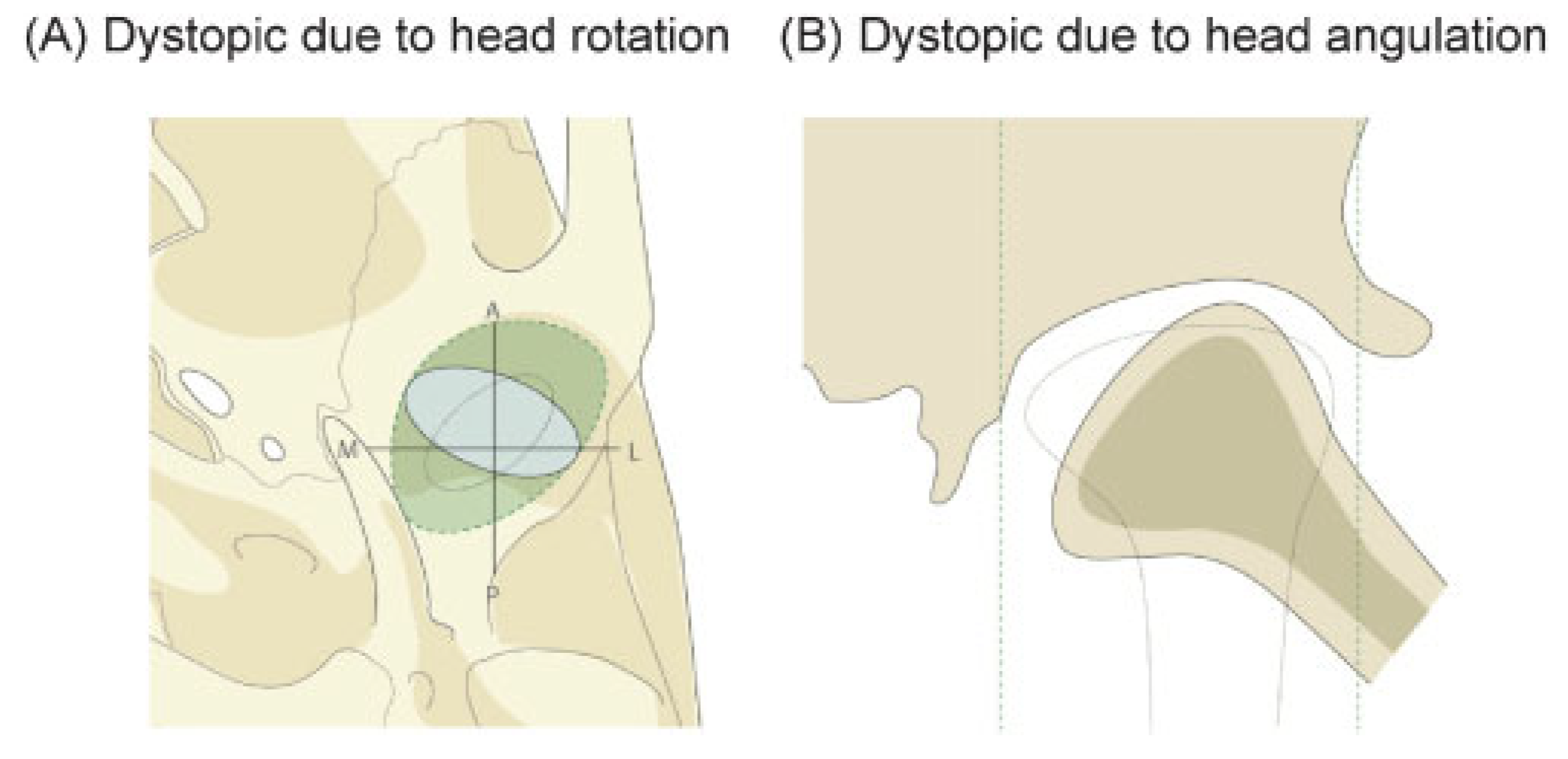
A displacement of the condylar head vis-à-vis the fossa has to be coded only once for each side. As far as alterations of the condyle to fossa relation are concerned, the group introduced an additional assessment of dystopic head to fossa relations, to allow an evaluation of late sequelae affecting the discoligamental function, for example, as a consequence of deviations even in undisplaced fractures or angulations of the head following fractures with displacement. Another much discussed problem was the precise definition of dislocation fractures. According to Wassmund [
28] and Gilhuus-Moe [
29] a dislocation fracture can be presumed, if the degree of angulation or fragment malposition is over 60 degrees, which nevertheless is not satisfyingly precise. During the working process we therefore defined anatomical landmarks based on axial, coronal, and sagittal CT views to give a more concise definition regarding complete or partial dislocation. One problem the group was not able to solve satisfyingly, yet, was the correct assessment of loss of vertical height in case of bilateral fractures. So far, there will remain a discrepancy between the assessments by for instance use of lateral overrides (i.e., performed according to the measurement procedure described in the brochure) and the overall loss of vertical height of the ramus due to rotational movements of the fragments, which cannot be calculated (
Figure 13). There remain major challenges for further classification of base versus neck fractures, which so far has been defined according to the panorex-based Loukota line (
Figure 1), [
4] with the location of the majority of the fracture line driving the diagnosis. According to this definition, however, there was a low rate of condylar neck fractures, with 55% of the assessed fractures of the condylar process having to be defined as base fractures against 12% in the neck subregion, that is, an odd of around 4:1 base to neck fractures. In addition, many fractures were considered as borderline cases as far as the differentiation between base and neck was concerned, resulting in cases being classified as base fractures, although participants would diagnose them as neck fractures from a clinical view point (see borderline cases in the appendix case collection [
7]). An alternative definition was thus proposed by giving more weight on the fracture lines located within the neck subregion, such as applying a one-third versus two-thirds rule (i.e., the fracture is defined as a neck fracture as soon as the fracture line runs more than one-third above the Loukota line) instead of the conventional 50 versus 50% rule. This proposal however remained to be fully evaluated.
In case of a new definition of the landmarks base versus neck (which should run more caudally according to the surgeons involved in the classification group) there might also be a better agreement in differentiating between the lower and upper neck region, which would also be of high clinical importance for the decision-making regarding the selection of approaches.