Infection and trauma are the two most common causes of temporomandibular joint (TMJ) ankylois [
1]. TMJ ankylosis can lead to disturbed growth of the mandible and maxilla on the affected side. This disturbance in growth can have serious sequelae. It may lead to an occlusal cant, a shift in the dental midline, and profound facial asymmetry. In addition, the maxillary and mandibular midlines are often not coincident and a transverse dental arch discrepancy is frequently found between the mandible and maxilla.
Fusion at the TMJ can restrict mouth opening. For those individuals severely affected: food has to be cut into small pieces, oral hygiene becomes difficult, and dental treatment is a challenge. Left untreated, TMJ ankylosis may lead to not only facial deformity but also to a compromised dentition that could result in pain, reduced oral intake, and poor oral health.
Facial deformity in childhood if not corrected early can have profound psychological effects on children and their families as the development of the facial disfigurement worsens in adolescence. Integration of the affected individual into mainstream society and obtaining a satisfactory education are two potential hurdles for such patients.
We report a young boy with unilateral TMJ ankylosis for whom treatment was done in two stages. The first operation involved release of the ankylosis and gap arthroplasty using a conchal graft secured to the condylar stump with BioGlue® (CryoLife, Inc., Kennesaw, GA). The second stage focused on the correction of the facial deformity and the restoration of function using unilateral distraction osteogenesis of the mandible.
Case Report
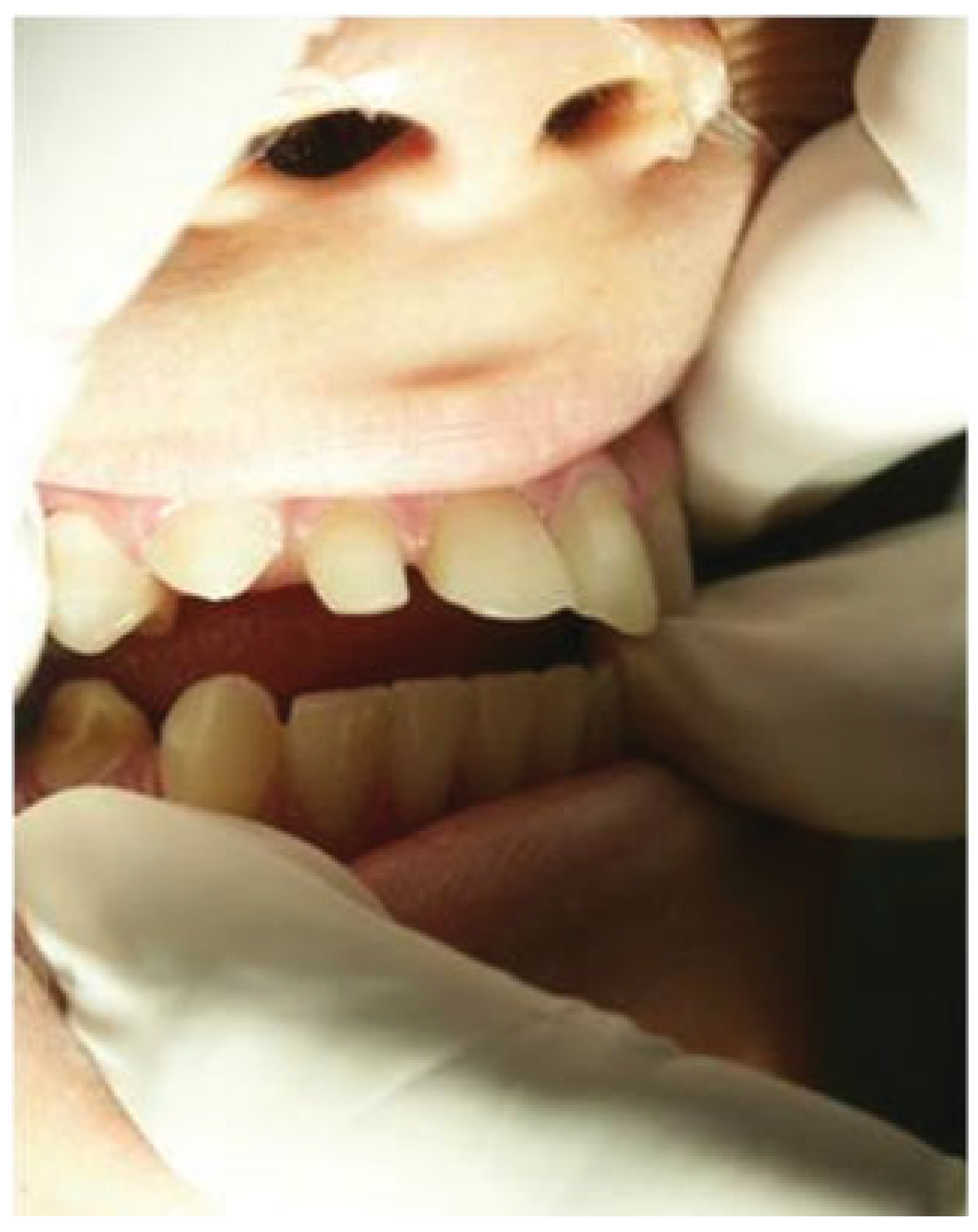
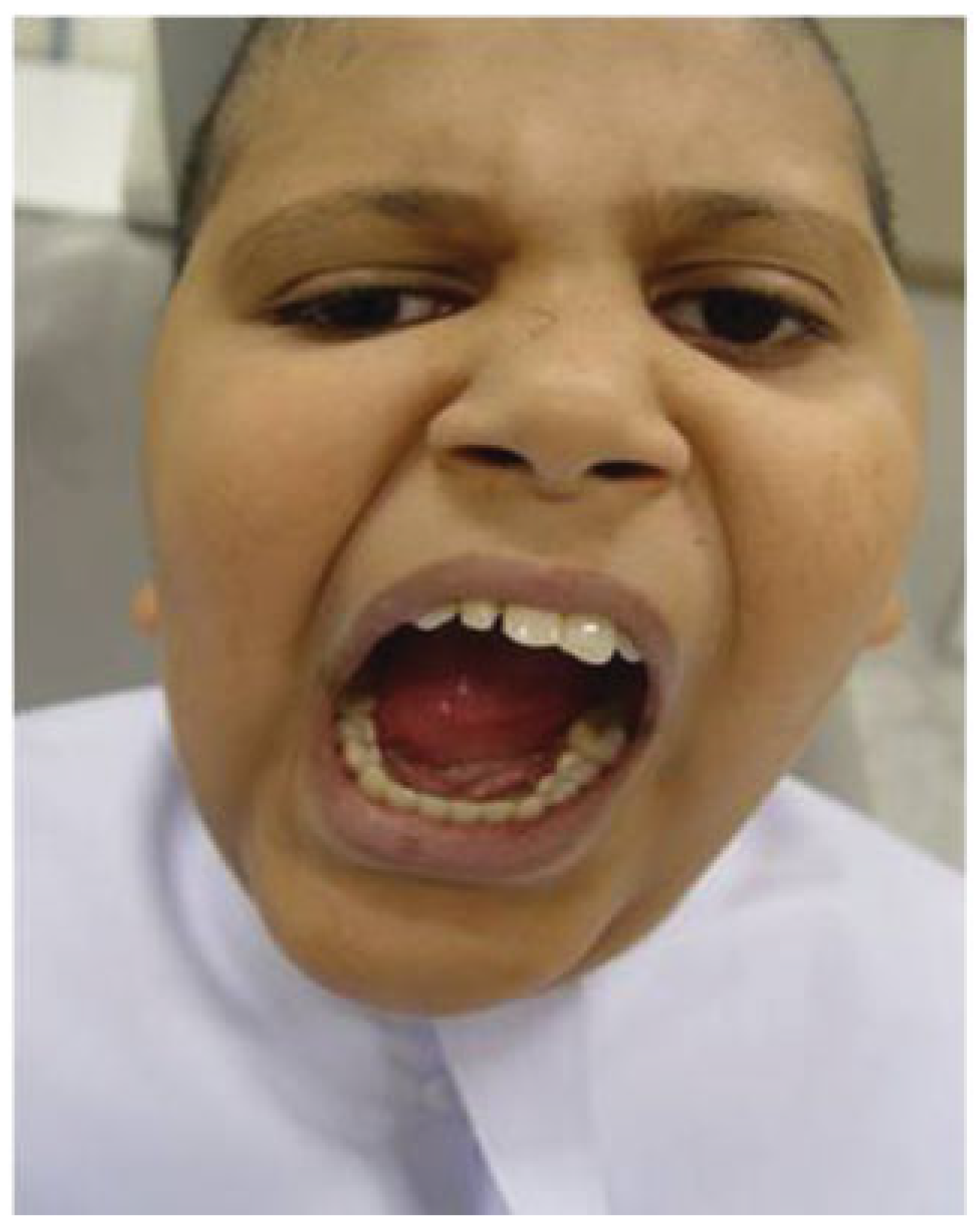
A young boy presented to the Maxillofacial Surgery Service with a severe limitation in mouth opening (
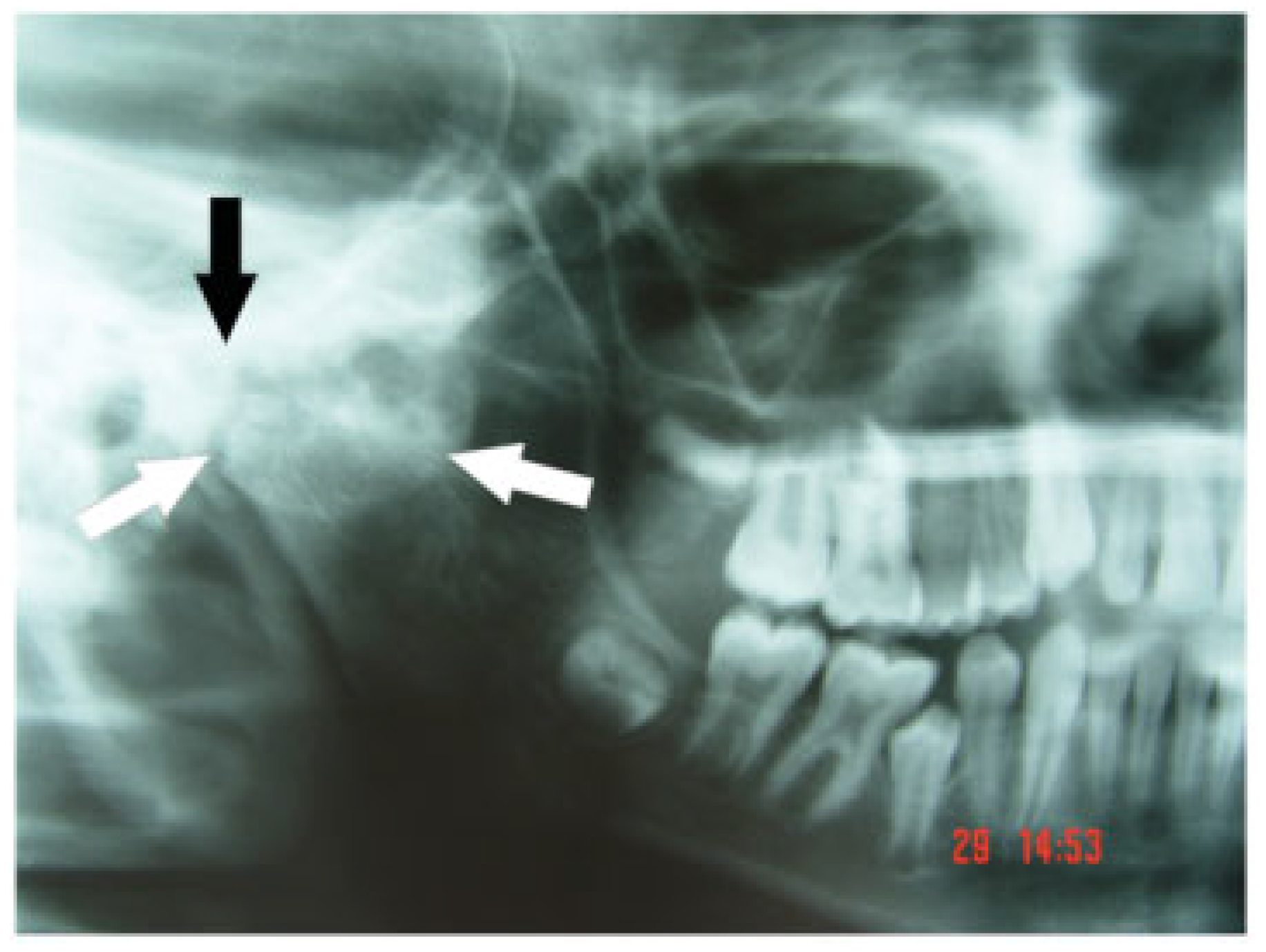
Figure 1). He had problems with eating and difficulty in maintaining oral hygiene. He displayed facial asymmetry with a shift of both his facial and dental midlines to the right. There was also an alteration of the occlusal cant of the maxilla with the left side being lower than the right. He had fallen as a child some years previously and fractured the right mandibular condyle. An orthopantomogram radiograph (OPG;
Figure 2) showed marked changes in TMJ anatomy and architecture on the affected right side and a hypertrophied right coronoid process.
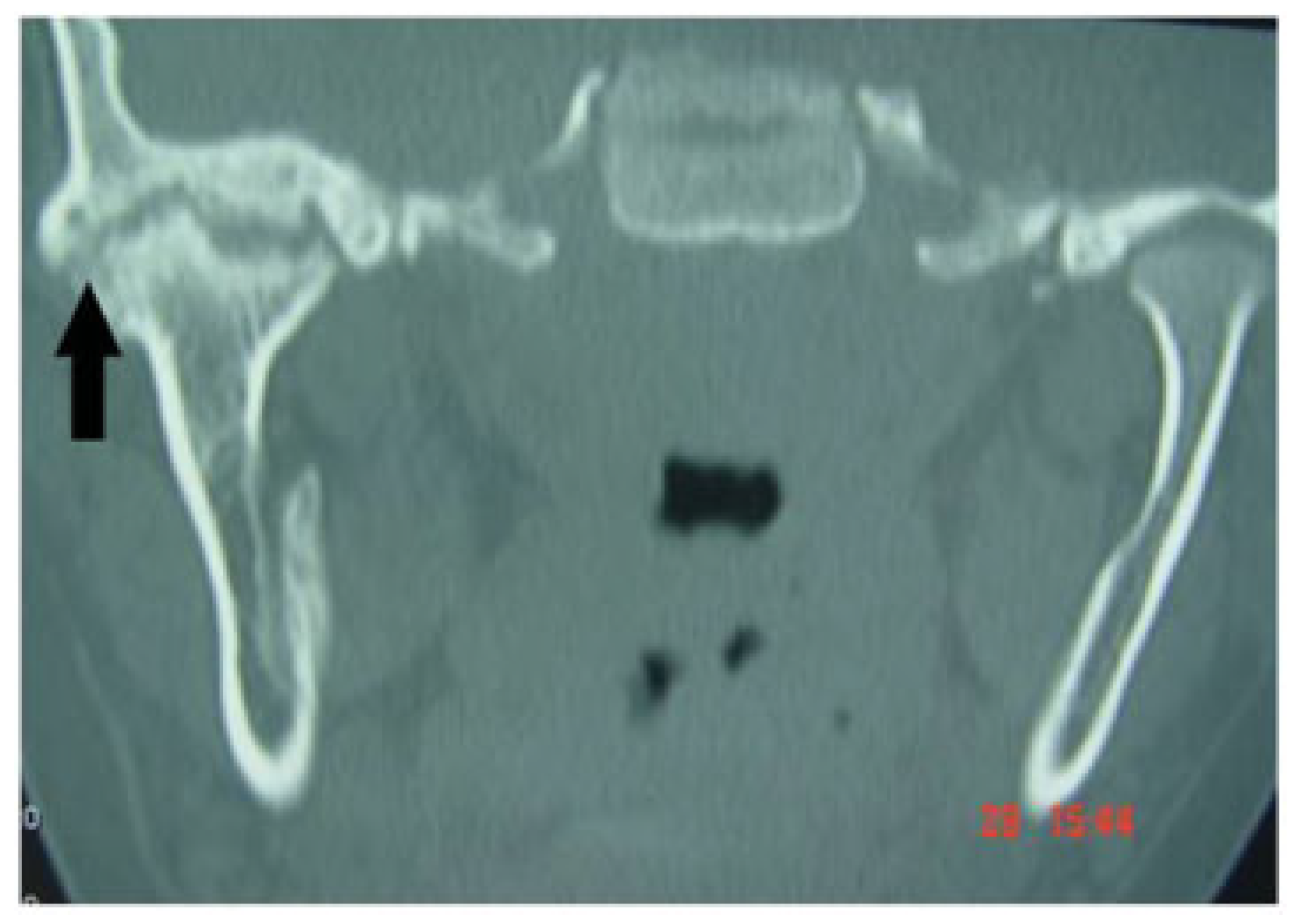
A computed tomography scan showed a mass of bone in the right TMJ region (
Figure 3). The fractured mandibular condyle had ankylosed with the skull base. Functional difficulties arose because the articulation at the right TMJ was restricted.
The plan of action for the young boy was to surgically release his ankylosis and do a gap arthroplasty using autogenous conchal cartilage under general anesthesia followed by extensive postoperative physiotherapy.
Surgical Technique—First Stage
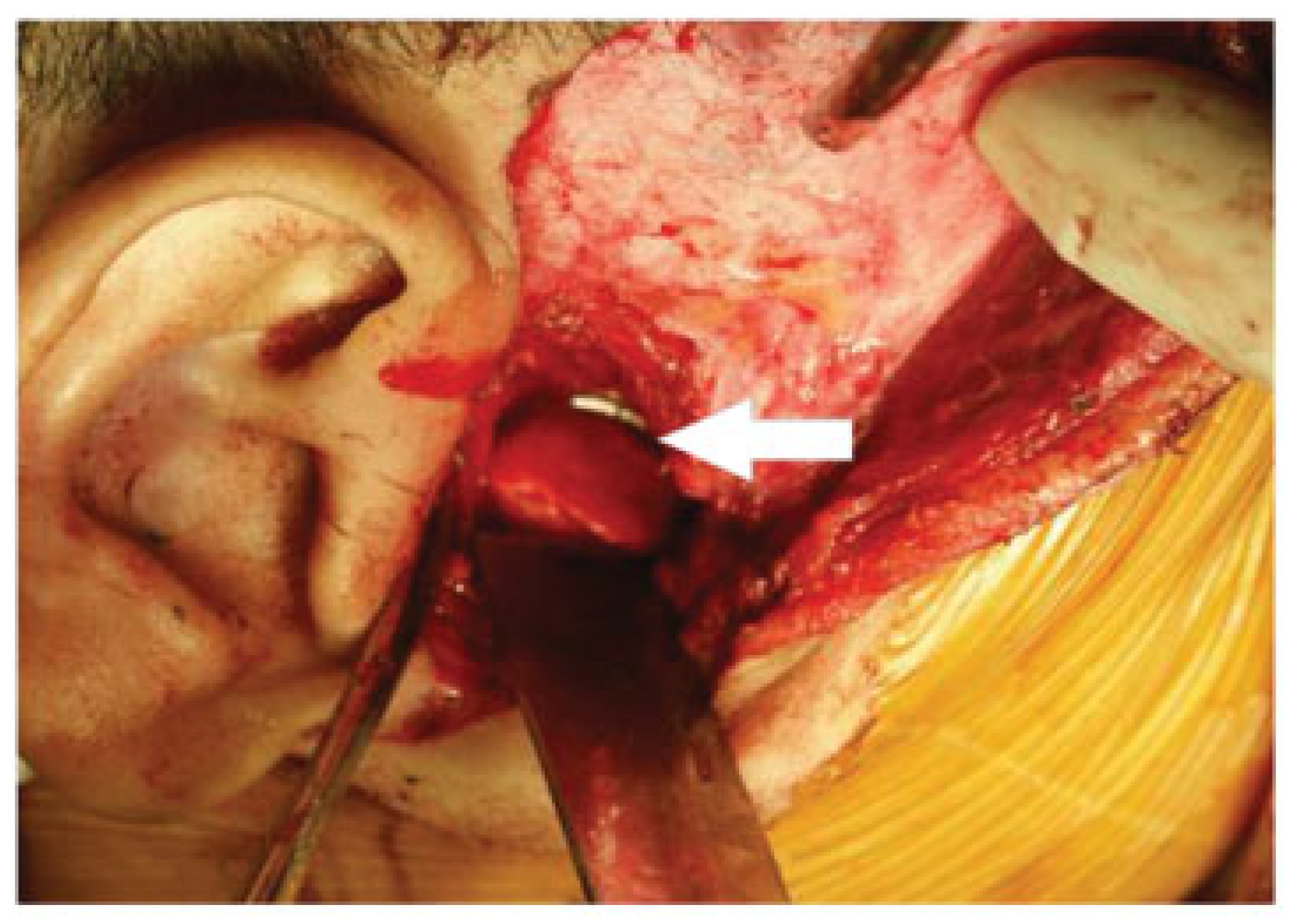
A modified preauricular approach to the TMJ was used [
2]. The temporalis fascia was split between the superficial and deep layers so that the plane of dissection would proceed beneath the temporal and zygomatic branches of the facial nerve. On arrival at the zygomatic arch, the periosteum was incised and the ankylotic bone accessed. The ankylosed bone was removed, taking care not to injure the maxillary artery that runs posterior to the neck of the condyle. A retractor was positioned directly behind the neck of the condyle to minimize the risk of injury. A coronoidectomy was not done. On release of the ankylosis, the mandible was manipulated to improve mouth opening.
A conchal graft was harvested from the ipsilateral ear via a posterior approach (
Figure 4A,B). The technique involved marking out with surgical ink the outline of the shape and size of the graft. Up to 50% of the conchal bowl can be removed without distorting the shape of the ear. The shape of the conchal bowl (
Figure 5) conforms closely to the shape of the residual condylar stump after TMJ release.
BioGlue
® adhesive was then applied to the condylar stump and conchal cartilage. It is made by mixing a cartridge of 10% glutaldehyde with one of 45% bovine serum albumin (BSA) in a double-barreled gun (
Figure 6). It was delivered to the operative site via a nozzle attached to the gun. The conchal graft was glued to the condylar stump. Not only did the conchal graft restore the contour of the condyle (
Figure 7), but it also served as a gap arthroplasty. The patient had rigorous postoperative physiotherapy to maintain the improved jaw opening (
Figure 8) that had been achieved from surgery. After discharge from the hospital and initial outpatient follow-up, the patient returned to his home country. He was not seen again for 2 years.
Follow-Up
The young boy returned 2 years later for follow-up. On inspection there was no recurrence of his ankylosis but his facial asymmetry had worsened. There had been very little if any forward mandibular growth on the side of his previous ankylosis. However, continued mandibular growth on the left side had increased the severity of the facial deformity. Indeed, the disparity in dental and facial midlines had gotten worse (
Figure 9). Of particular note was the exacerbation of his deviated chin position on mouth opening (
Figure 10). The left side of the mandible was longer than the right side and that the mandibular midline had shifted to the right.
The treatment options were waiting until the completion of growth before correction of the secondary facial deformity or immediately proceeding with surgery to reduce the facial disfigurement and doing definitive corrective surgery on cessation of growth. It was felt that delaying surgery could lead to further worsening of the dentofacial deformity, which could have profound psychological effects on the patient as he approached his teen years.
Early intervention could harness the potential of the patient’s own growth once skeletal and soft tissue balance have been restored, which in turn might lead to less surgery being required to correct the residual deformity on completion of growth. After much discussion between the family and clinicians, it was decided that unilateral mandibular distraction osteogenesis was the treatment of choice to restore facial symmetry.
Surgical Technique—Second Stage
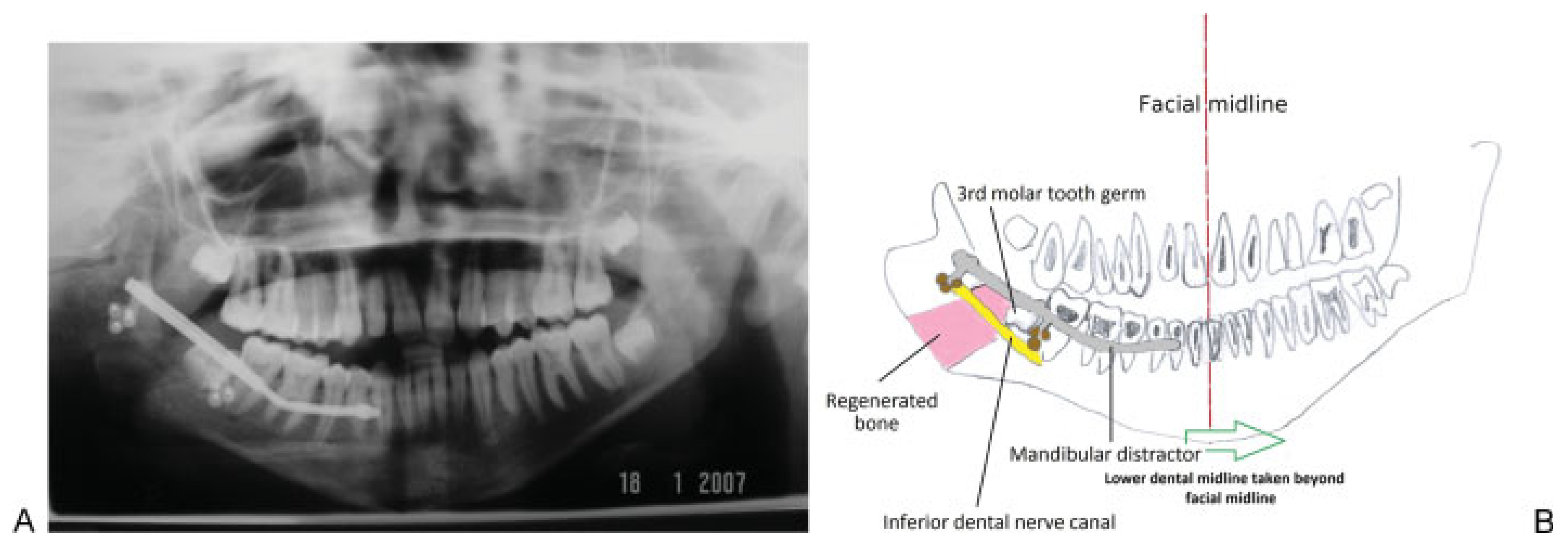
Preoperative assessment of the mandible prior to making the osteotomy cuts and placement of the distractor was assisted by the use of an OPG. The osteotomy cuts (
Figure 11) have been previously described [
3,
4].
As the patient was young, it was deemed important to ensure that both the boney cuts and placement of the screws to secure the distractor plate were positioned to avoid damage to the roots of the teeth and developing tooth germs (
Figure 12). A possible advantage of employing staggered buccal and lingual osteotomy cuts is that the width of the mandible is preserved as the callous is elongated as opposed to the formation of a narrow callous that might arise from a single vertical buccal-lingual osteotomy cut. However, the use of sagittal split osteotomy cuts results in a large surface area between the buccal and lingual plates for rapid healing to take place; consequently, distraction was started on the first postoperative day rather than on the fifth postoperative day with the standard vertical cut [
5].
A Zurich Pediatric Ramus Distractor (KLS Martin®, Tuttlingen, Germany) was placed across the osteotomy site. Distraction was achieved by turning the distractor rod with a screwdriver. Each turn represented 0.5-mm movement. The rod was turned twice daily. Progress with distraction was monitored both radiographically and clinically. Serial OPGs were used to radiographically follow progress.
Clinical evaluation consisted of watching for improvements in both the dental and facial midlines and whether the mandibular deviation associated with mouth opening improved. On completion of distraction, a post mandibular distraction osteogenesis OPG was taken (
Figure 13A). In anticipation of continued growth from the unaffected side and possible relapse, mandibular distraction was continued beyond the dental midline (
Figure 13B).
At the conclusion of distraction, the patient had an open bite on the right side (
Figure 14), which was gradually closed by encouraging passive eruption of the maxillary dentoalveolar segment through the selective grinding of the occlusal surfaces of a removable denture (
Figure 15). Not only had mandibular distraction reduced his asymmetry, (
Figure 16) but it had also corrected the deviation of his mandible on mouth opening (
Figure 17). There was no limitation in mandibular movement in right and left lateral excursion (sideway movements) and protrusion. Before the open bite could be completely closed the patient was lost to follow-up.
Discussion
Gap Arthroplasty
Surgical techniques to correct TMJ ankylosis vary. The initial surgical step involves the release of the ankylosis to ensure that there is free movement of the condylar stump. Traditionally, this is done is at the level of the TMJ. If the coronoid process is also part of the ankylosis, it too is removed (coronoidectomy).
To prevent reankylosis at the surgical site, synthetic material (Silastic; Dow Corning Corporation; Midland, MI) or autogenous tissue (full-thickness skin graft, temporalis, cartilage graft, or composite skin auricular cartilage graft) can be placed between the condylar stump and skull base (gap arthroplasty) [
6,
7,
8,
9]. The disadvantage of using Silastic for TMJ arthroplasty is the potential for a foreign body reaction to develop [
6]. One animal study investigating the use of autogenous conchal graft secured by wire to the glenoid fossa found that fibrous connective tissue formed between the superior surface of the graft and the articular surface of the glenoid fossa and also between the inferior surface of the graft and the articular surface of the condyle [
10]. In contrast, however, the technique we describe uses BioGlue
® to secure the conchal graft to the condylar stump. As a procedure it is both quick and simple. The graft requires no contouring and there is no need for sutures as it is glued to the condylar stump.
Is Coronoidectomy Always Necessary?
Coronoidectomy involves both the detachment of the temporalis muscle from the coronoid process and resection of the hypertrophied coronoid process. On release of TMJ ankylosis it would appear reasonable to do a coronoidectomy if the hypertrophied coronoid process was contributing to the ankylosis and restricting mouth opening. A hypertrophied coronoid process could also physically interfere with mouth opening. Coronoidectomy has been regarded as established practice for the treatment of TMJ ankylosis by several authors [
5,
11].
Should it therefore be considered routine after release of TMJ ankylosis? In some patients after release of unilateral TMJ ankylosis and coronoidectomy a huge swing of the mandible to the operated side is observed on mouth opening. This deviation may be due to an imbalance of forces acting on the right and left sides of the mandible as a result of partial removal of the temporalis coronoid process unit on one side. Whatever the cause, the deviation can be both unsightly and psychologically disturbing for the patient. It may even arouse comment from strangers and cause the patient social embarrassment. Deviation of the mandible on mouth opening may also be seen in internal derangement of the TMJ, but it is often not as severe as that observed following unilateral coronoidectomy.
Coronoidectomy may be unavoidable for some patients affected by unilateral TMJ ankylosis. However, in view of the possibility of a disfiguring jaw deviation arising from such surgery, it might be prudent to counsel patients about this potential scenario and consider deferment of coronoidectomy in selected patients.
Restoration of Symmetry—Choice of Technique
Gap arthroplasty does not correct the facial deformity. The options for restoring symmetry include costochondral graft, prosthetic TMJ, and mandibular ramus distraction osteogenesis. A costochondral graft is biocompatible and has inherent growth potential. However, it requires a donor site remote from the area of surgery. Growth is also unpredictable and could occur at any time leading to the possibility of a return of the facial asymmetry [
12,
13].
Unlike rib, a prosthetic TMJ has the advantage of not requiring a donor site. However, it does not grow with the patient. Its use is therefore generally contraindicated in children.
Mandibular distraction osteogenesis, however, can correct mandibular asymmetry without the need to harvest tissue from a donor site and the regenerated bone does not represent a foreign body as is the case with a TMJ prosthesis. The application of unilateral mandibular ramus distraction osteogenesis to provide mandibular elongation to restore symmetry can lead to a lateral open bite; however, if this is done in the growth phase, closure of the bite can be facilitated through passive eruption of the opposing maxillary dentoalveolar segment.
Simultaneous Gap Arthroplasty and Distraction Osteogenesis versus Staged Procedures
There have been reports of simultaneous gap arthroplasty and distraction to correct facial asymmetry as a result of unilateral TMJ ankylosis [
12,
14]. Doing these two distinct surgical steps at the same time certainly has the advantage of reducing overall treatment time, which would certainly appeal to patients and family. However, compliance with jaw exercises is considered essential to success after release of TMJ ankylosis and gap arthroplasty. Not being entirely focused on postoperative physiotherapy after ankylosis release because of concurrent distraction may compromise the gains in mouth opening and lead to relapse. Although the type of postoperative physiotherapy was not reported in the studies cited, conventional methods of jaw exercises usually employ wooden tongue spatulas or the TheraBite device (Atos Medical AB, Hornby, Sweden) to force the mandible down and stretch the muscles of mastication. These exercise regimens should be used with caution. The inadvertent application of downward forces on the side of distraction could not only dislodge the distractor, but also alter the direction of distraction through distortion of the callous.
In one study the recommended treatment plan for children with TMJ ankylosis was to defer distraction after TMJ ankylosis release for about a year to assess the response of the maxillomandibular complex on the affected side to ankylosis release [
1]. Planning could then be focused solely on distraction and the execution of the surgery. As yet, there is no consensus on whether children with TMJ ankylosis should undergo simultaneous gap arthroplasty and mandibular distraction or a staged reconstruction. Patients with complex facial deformity arising from unilateral TMJ ankylosis probably do not fall into a single treatment protocol. Indeed, planning by the craniofacial team should include not only case complexity, but issues related to compliance and individual family circumstances.
Tissue Adhesion
Tissue adhesion is the process by which surfaces stick together [
15]. Protein polymers are just one group of many tissue adhesives that have found clinical use as adjuncts to tissue repair with sutures. Other tissue adhesives include fibrinbased adhesives and cyanoacrylate and bone cements. BioGlue
® is a protein polymer tissue adhesive. It consists of 45% BSA solution and 10% glutaldehyde. Cross-linking of BioGlue
® occurs between lysine molecules of BSA and the aldehyde groups in glutaldehyde. Tissue adhesion occurs after the BSA, extracellular matrix, and cell surfaces have come into contact with glutaldehyde. Within 2 minutes of mixing the two components, maximum binding power is achieved. Albumin is a natural protein and the major component of BioGlue
®. It is broken down slowly in the body by proteolysis.
BioGlue
® has been recognized as a medical device by both the United States and European Union and is subject to Food and Drug Administration and European Union surveillance [
16]. Although it is United States Pharmacopeia class VI compliant and considered both biocompatible and nontoxic, caution should be exercised when using BioGlue
® in close proximity to nerves [
17].
BioGlue
® has been used to assist aortic resection repair and cardiac repair and for the prevention of cerebrospinal leaks in neurosurgery [
18,
19,
20]. Although fibrin-based adhesives have been used in head and neck surgery and maxillofacial surgery [
21,
22,
23], the application of protein polymers adhesives such as BioGlue
® for craniomaxillofacial surgery has not been reported.
Conchal grafts, however, have been reported for a variety of craniomaxillofacial applications. An earlier study reported the use of sutures to attach a composite skin– conchal graft to the condylar stump after TMJ ankylosis release, whereas Lei described a technique of placement of conchal cartilage as a free interpostional graft following ankylosis release [
7,
8].
Interestingly, the use of BioGlue® to secure the conchal graft to the condylar stump avoided the use of sutures. Conchal grafts can be harvested safely via a posterior approach without altering the shape of the ear. The inherent “caplike” shape of the graft allows it to easily confirm to the raw condylar stump without modification. The procedure can be done in a short period of time.
Conclusion
There are a variety of options available to treat unilateral TMJ ankylosis in childhood. The use of autogenous conchal cartilage for gap arthroplasty has many benefits over alloplastic material. The shape of the harvested conchal bowl conforms closely to the residual condylar stump after ankylosis release. The use of BioGlue® provides a quick and simple way to secure the conchal graft, further expanding the application of tissue adhesives in surgical practice.
The use of mandibular distraction osteogenesis with a sagittal split osteotomy cut to correct asymmetry and an acrylic plate to facilitate passive eruption of the maxillary teeth is nothing new. However, the multiple steps or procedures employed to treat this child including the absence of a coronoidectomy emphasize the importance to clinicians of not being too rigid and prescriptive in dealing with facial deformity. Protocols and guidelines can serve as an invaluable foundation to base our practice and should be regularly updated in light of new evidence and technology.
Ultimately, the success of surgery will be influenced not only by the technical skill of the craniofacial team, but other factors such as compliance, the timing of surgery, and the availability of resources.
Personalized surgery is very much a part of the personalized medicine of the future as patients and their families expect and demand individualized solutions to their problems. The management of unilateral TMJ ankylosis is no exception.