Abstract
Fractures of the pediatric craniofacial skeleton can be challenging to manage. The initial injury and subsequent treatment can cause long-term growth disturbances yielding problematic secondary deformities. This review considers the normal growth of the craniofacial skeleton and typical facial fracture presentations in children and discusses the potential long-term sequelae from these injuries and their management.
Craniofacial Skeletal Development
The craniofacial skeleton originates primarily from cells of neural crest origin. Cranial growth is driven by the underlying brain, and the sutures allow even expansion of the cranium. By the age of 5, the cranium has reached greater than 85% of the final adult size, although the most rapid growth occurs from birth to 2 years [1,2]. The growth of the orbit is similarly directed by its contents with 90% of the size of the orbit complete by age 5 [3,4]. Cranio-orbital injuries after the age of 5 should therefore have minimal long-term effects on growth.
The midfacial growth occurs forward from the skull base directed by the midline synchondroses of the sphenoid, ethmoid, and vomer [5,6]. This region directs nasal growth, which is slower to achieve full growth compared with the cranium and orbit. The height of the nose as measured by nasion to subnasale is ~30 mm at 1 year of age, just under 40 mm at 4 years, and fully grown in females at 12 years (46 mm) and in males at 15 years (50 mm) in a large cohort of North American children [7]. The nose undergoes a periods of more rapid growth around 4 to 5 years of age and at the time of puberty [8].
The mandible develops from neural crest cells of the first pharyngeal arch of Meckel’s cartilage by intramembranous ossification. The condylar region is cartilaginous and thought to be a significant growth center directing the elongation of the posterior border of the ramus [9] and causing the gonial angle to become more acute [10]. The muscular action of the pterygomasseteric complex when chewing is also thought to contribute to the development of the mandible [11]. Transverse width and anteroposterior growth are achieved by resorption of bone along the lingual border and deposition of new bone along the labial and buccal surfaces of the bone. Transverse width is highly developed with bigonial distances over 80% complete by age 1 year [7]. Height of the mandible is increased by deposition of new bone along the inferior border of the mandible and is only two-thirds complete by age 1 [7,11]. The mandible undergoes periods of faster growth, and if the growth centers are injured at this time, more significant growth disturbances may occur [12]. Mandibular growth is complete in females at age 14 to 16 years and males at age 18 to 20.
The paranasal sinuses develop at different rates. The frontal sinus pneumatizes from age 2 but is only radiologically identifiable at around 8 years of age [13]. The maxillary sinus can be seen radiologically at around 6 months.
Epidemiology of Facial Fractures in Children
Pediatric craniofacial skeletal injuries are relatively uncommon with pediatric patients consisting of less than 10% of all facial fracture cases [14]. Craniofacial skeletal fractures make up only 4.6% of all pediatric trauma presentations,15 but these patients tended to have higher injury severity scores with prolonged hospital admissions and higher morbidity/mortality [14]. Younger patients (<5 years) are less likely to sustain a fracture probably due to both the intrinsic elastic quality of bone in the young as well as social factors [12]. When fractures occur, young patients less than 5 years are more likely to have nasal and superior orbital injuries [15,16]. This is thought to be due to high cranial:facial proportions, starting from 8:1 at birth decreasing to 2:1 in the adult. Older pediatric patients have a higher incidence of mandibular fractures injuries due to the relative prominence of the lower jaw and of orbital floor injuries due to the aeration of the maxillary sinus.
The causes of injuries are primarily motor vehicle accidents, accounting for 35 to 50% of all fractures, followed by sports injuries, interpersonal violence, and falls [12,14,15,17,18]. It is more common to treat pediatric facial fractures conservatively compared with adults as the capacity to remodel is greater [12,16,19,20]. For fractures that require treatment, accurate reduction with or without fixation should be achieved earlier than in adults as children’s bones will heal much faster.
Long-Term Sequelae
There is a paucity of literature regarding the long-term complications following a pediatric facial fracture. It is uncommon for children to require secondary reconstructive surgery following a facial fracture with only 10 to 15% of patients requiring revisions [12,19,21,22].
Longer-term complications from pediatric facial fractures may be due to several factors:
- Damage to growth centers.
- Fracture malposition.
- Iatrogenic—either from soft tissue/periosteal stripping or due to fixation.
- Soft tissue injury and subsequent scar formation.
The resulting disturbance can either be overgrowth or undergrowth. Malposition of a fracture fragment such as an incompletely reduced parasymphyseal fracture may result in malocclusion. Underor overgrowth occurs from damage to the growth centers such as the condyle of the mandible or the nasal septum. In animal studies, the use of metal fixation can result in bony growth restriction [23]. This growth restriction is least with interfragmentary wiring and increases with the increasing volume of fixation used. In practice, there are few cases reported with titanium fixation that directly lead to undergrowth; the more likely complications result from loosening and plate migration through the growing skeleton [24,25]. It would seem prudent from these studies to minimize the amount of rigid fixation applied to the growing craniofacial skeleton and consider planned early removal to reduce potential complications.
The use of bioresorbable fixation is thought to lessen the chances of growth disturbances compared with titanium fixation [21]. The plates lose their strength after several months and are resorbed by 1 year, thus reducing the impact on growth. They do not require removal, which reduces iatrogenic soft tissue disruption.
Cranium
Cranial defects following trauma may be due to direct bony loss, subsequent bone flap loss, or growing skull fractures.
Growing skull fractures occur when there is disruption to the underlying dura as well as the bone during rapid brain growth (Figure 1). Bone is resorbed and a subsequent soft area develops. Growing skull fractures almost always occur in a child under 3 years and require reconstruction of the underlying dura with a dural patch and autogenous bone reconstruction [26].

Figure 1.
(A) Gap in dura from trauma allows herniation of arachnoid and pia mater. (B) Growing calvarial fracture from bony resorption and herniation of intracranial contents.
Significant head trauma may require the removal of a bone flap to decompress the brain. In our institution, the bone flap is frozen to maintain its integrity. Grant et al. [27] report a 50% reoperation rate following delayed replacement of the bone flap due to significant bony loss, which is consistent with our experience at the Hospital for Sick Children. Small defects are best reconstructed with autogenous bone, either split calvarium or rib. Large calvarial defects are best reconstructed with customized alloplastic constructs, either polyetheretherketone (PEEK), hydroxyapatite (in the form of a customized hard tissue reconstruction), or titanium. These alloplastic materials are well tolerated, have a low incidence of infection, are simple to position as they are already contoured to the defect, provide solid protection to the underlying brain, and importantly do not require a donor site (Figure 2). Successful application of the alloplastic construct requires careful preoperative planning to allow for the shape of the underlying brain not just contouring to the bony vault. Growth is not impeded if the reconstruction is performed in the school years as calvarial growth is nearly complete by age 5. At the Hospital for Sick Children, we perform alloplastic reconstruction of large cranial defects after age 5 to 7 to prevent the potential skull growth restriction, which can occur if performed at an earlier age.
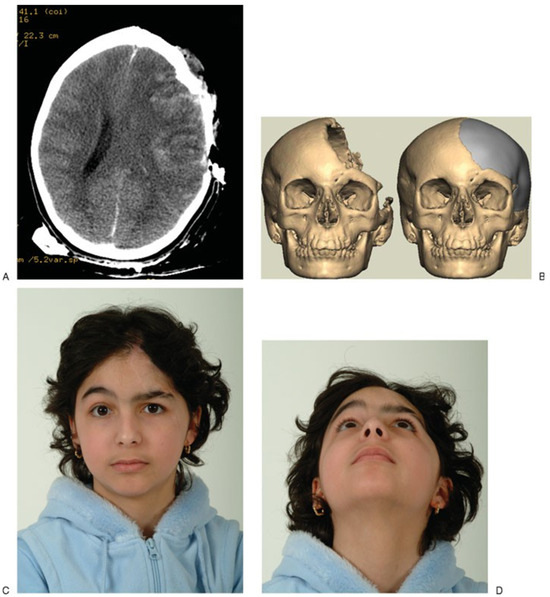
Figure 2.
(A) This 8-year-old patient sustained a significant open head injury from a motor vehicle accident requiring a decompressive craniotomy. An intermediate bone flap was raised and replaced a week later once the patient was considered stable. (B) Much of the replaced bone flap resorbed, leaving a large cranial defect. Following rehabilitation, the patient required an alloplastic reconstruction using polyetheretherketone (Synthes, Paoli, Pennsylvania). (C,D) The aesthetic outcome following bony reconstruction.
Craniofrontal Region
The fracture patterns in the craniofrontal area change as children age. The cranial:facial ratio decreases with decreasing incidence of frontal bone injuries [28] As the frontal sinus develops, injuries can occur to this structure. Longer-term problems from injuries in this area may be contour deformities of the bone (Figure 3) or complications arising from the frontal sinus such as mucoceles. At our institution, we have used bone substitutes including calcium hydroxyapatite constructs to contour bony defects but found delamination a significant problem in a small number of patients who required explantation of the material. Consequently, our preference is to use solid constructs such as porous polyethylene or PEEK once the fracture is well healed and there is no evidence of connection with the sinus.
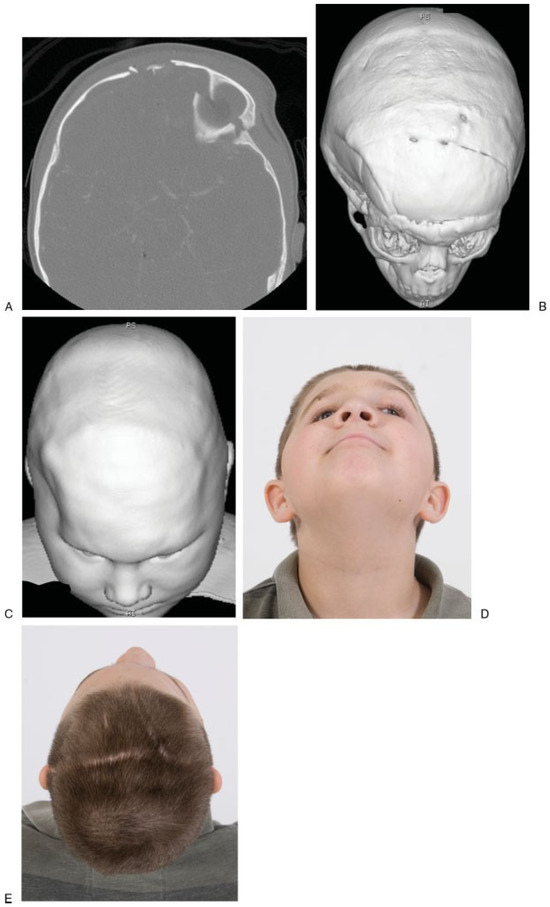
Figure 3.
(A) Fronto-orbital fracture in a 9-month-old boy accidentally run over by car tire. (B,C) At age 6 years, the patient had a significant right forehead/temporal depression that was managed operatively with a fronto-orbital advancement. (D,E) The aesthetic outcome at age 10 years.
In children who undergo fronto-orbital reshaping for craniosynostosis, it is well recognized that the frontal sinus may not develop due to the elevation of the bandeau (Figure 4). We would speculate that children sustaining a significant trauma to the glabella region might also have hypoplasia of the frontal sinus [29].
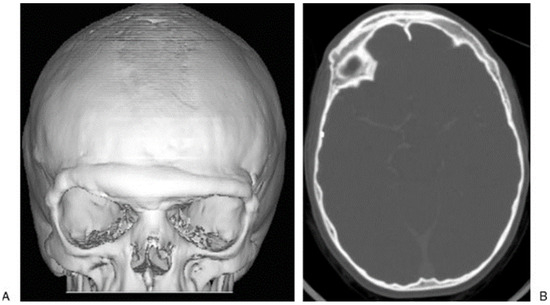
Figure 4.
(A,B) The lack of pneumatization of the frontal sinus following fronto-orbital advancement at age 6 months with follow-up scan at 12 years of age.
Frontal sinus mucoceles may present as a nasofrontal swelling or may cause globe dystopia. Treatment involves cranialization of the sinus, obliteration of the frontal ducts, and bony reconstruction as required.
Naso-Orbital-Ethmoidal Fractures and Nasal Fractures
Managing these fractures acutely can be challenging, with potential disruption of the medial canthus and depressed nasal bridge. The best opportunity to prevent secondary complications is accurate repositioning of the bony fragments and transcanthal wiring to stabilize the medial canthi. Longer-term sequelae may present as telecanthus if the medial canthus is able to drift laterally. The nasal bridge may be depressed, leading to a saddle nose deformity [6,22,30,31]. Treatment for this may require nasal dorsal augmentation with either autogenous grafts or alloplastic implants. Animal experiments suggest that damage to the cartilaginous portion of the nasoseptovomeral region can result in significant growth disturbance, and isolated nasal bony trauma results in less growth disturbance. This is consistent with observational studies as noted by a study of 57 children followed into adulthood who had sustained bony nasal fractures suggesting that it was uncommon for patients to require later corrective surgery [5]. However, isolated nasal fractures are common in children, and even simple injuries treated with a careful manipulation under anesthesia may still have long-term problems such as nasal deviation, dorsal hump, or obstructive breathing. Treatment involves septorhinoplasty at skeletal maturity.
Orbit
In children, superior orbital fractures are often treated conservatively [16,32]. Longer-term sequelae from larger defects can be potential encephalocele/growing skull fracture [33]. Management of this rare problem would involve bone grafting the floor of the anterior cranial fossa.
Orbital floor fractures occur once the maxillary sinus is sufficiently pneumatized (Figure 5). The ‘‘whiteeyed fracture’’ is a classic pediatric orbital fracture where intraorbital contents become trapped in the maxillary sinus following a fracture of the floor [34]. The bony floor may return to its original position [35,36]. Examination findings reveal diplopia on upward gaze, and computed tomography scan demonstrates the entrapped soft tissue. Although the inferior rectus is not directly trapped, the delicate fibrous tissues between it and the floor can be tethered in the fracture site [19]. The inferior rectus muscle can undergo fibrosis and scarring following this type of injury, possibly due to a Volkmann’s type of contracture. Early exploration is recommended. Usually the diplopia from this type of jury resolves over weeks to months, and if it does not resolve, strabismus surgery may be required.
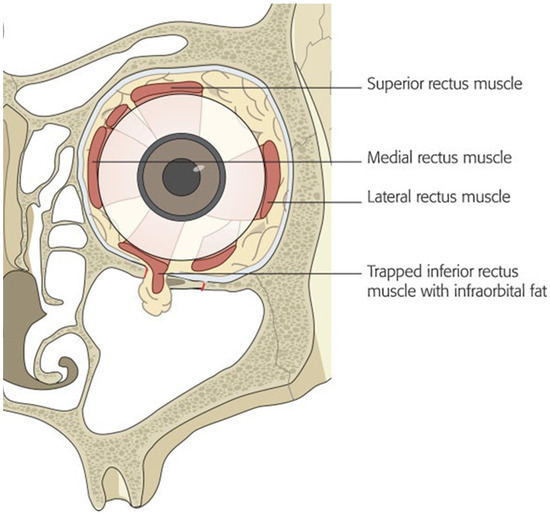
Figure 5.
Fracture of orbital floor allows herniation of periorbital fat and inferior rectus muscle. Strong periosteum and flexible bone in children and young adults allow the floor to return to its original position, trapping the intraorbital contents along the fracture line. This results in diplopia on upward gaze and nausea/vomiting from the oculovagal reflex.
Enophthalmos is less common in children than adults following orbital floor fracture. Treatment is similar to the adult population involving augmentation of the orbital floor [37].
Midfacial and Dentoalveolar Fractures
The classic Le Fort pattern of injuries are uncommon in children [14]. In the acute setting, accurate reduction of midfacial fractures can be challenging if the soft tissue is significantly disrupted or if there is significant bony comminution or bone loss. Midfacial fractures may be allowed to heal with a view to managing any subsequent problems secondarily. These problems may include malocclusion, tooth loss, and facial contour irregularities. Undergrowth of the maxilla is well described in patients who have had periosteal elevation in the process of repairing a cleft of the hard palate [38,39]. The periosteum provides the bone with a blood supply; it is osteoinductive and following elevation it can form a scar. Traumatic stripping of the periosteal tissues either from direct trauma or surgical repair may potentially cause growth disturbances. Malocclusion can be treated with orthodontics and orthognathic surgery as required. Permanent dentition loss may require osteointegrated implants, and contour issues may be addressed with onlay grafts or alloplasts (Figure 6).
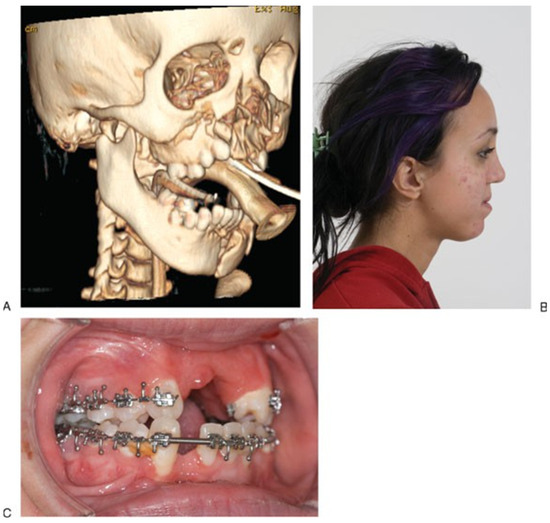
Figure 6.
(A) Midfacial and mandibular fracture following motor vehicle accident. (B,C) Subsequent midfacial hypoplasia and maxillary alveolar bone loss and class III relationship.
Mandibular Fractures
Mandibular fractures account for one-third of facial fractures in children and are more often treated conservatively compared with adults [12,20,40,41] Longer-term problems arising from mandibular fractures depend on the location at which the fracture occurs and the age of the patient at the time of the injury.
A primary growth center for the mandible is in the condyle, and injury to this area can result in growth disturbance and temporomandibular joint (TMJ) bony ankylosis. Several studies with intermediate-term follow-up have shown good results with conservative treatment of condylar fractures in children [20,42]. Intraarticular condylar head fractures that are displaced laterally are at greater risk of later bony ankylosis to the base of the zygoma [43]. Posttraumatic TMJ ankylosis may present with asymmetry, malocclusion, and limited mouth opening. If the injury occurs as an infant, there may be concomitant retrognathia (Figure 7). TMJ release may be indicated to treat ankylosis, and at the Hospital for Sick Children, this is performed once a patient is old enough to comply with physiotherapy, usually after 6 years of age. The principles of surgical release involve an external approach to the TMJ with excision of the bony block, contralateral bony or soft tissue release as needed, and autogenous reconstruction of the joint. Postoperative physiotherapy is commenced 1 week later and may involve the use of dynamic stretching devices as well as passive bite blocks for nighttime.
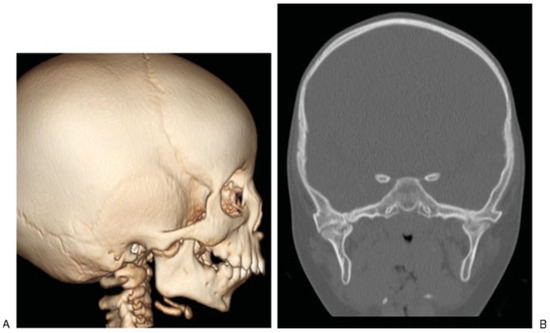
Figure 7.
(A,B) This patient was injured in a bus crash at age 6 months. Prior to the accident, there was normal mouth opening but over the subsequent 18 months, her mouth opening was reduced to 2 mm. The accident occurred in another country, and her first presentation was at age 2 years with temporomandibular ankylosis.
If the TMJ is functioning well but there has been disturbance to the growth potential of the mandible, facial asymmetry and/or malocclusion may occur. Treatment may be solely orthodontic or may involve orthognathic surgery (Figure 8). Long-term records of 88 children who sustained mandibular fractures and presented to the Hospital for Sick Children were retrospectively reviewed to assess the need for later orthodontic treatment or orthognathic surgery [12]. Results indicated that a pediatric mandibular fracture does not lead to a higher incidence of orthodontic treatment. Children younger than 4 years or older than 12 years rarely require orthognathic surgery to correct facial growth disturbances following mandibular fractures. In contrast, 22% of children aged 4 to 7 years and 17% of children aged 8 to 11 years required orthognathic surgery to correct facial growth disturbances following mandibular fractures. Condylar fractures were the most common site of mandibular fracture and led to facial asymmetry most frequently.
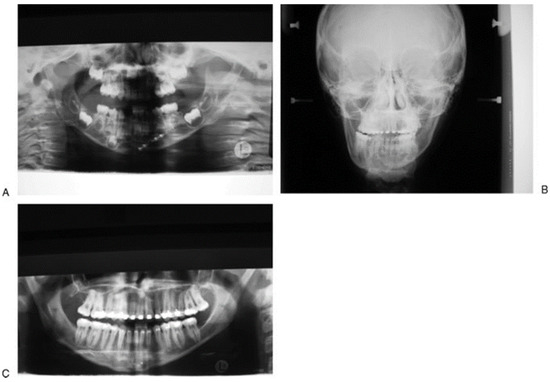
Figure 8.
(A) This 3-year-old patient sustained a left parasymphyseal fracture and right condylar head fracture following a fall down stairs. The parasymphyseal fracture was plated and she was mobilized on a soft diet. (B,C) Seven years later, she was noted to have mandibular asymmetry with the chin point deviating to the right side suggestive of right-sided undergrowth. Cephalometric analysis showed decreased height of the posterior ramus on the right side. She underwent bilateral sagittal split osteotomies to correct this asymmetry.
Achieving centric occlusion at the time of initial treatment is challenging in patients with mixed dentition and in the presence of multiple fracture sites. Maxillomandibular fixation should only be used for a relatively short period (2 weeks or less) in children as the bony union is much faster than adults and any longer period of fixation can lead to ankylosis. At the time of acute management it is critical to attempt to reduce an open bite deformity or significant cross-bite. A minor cross-bite may be due to soft tissue swelling and/or masseteric spasm and often improves with time. A persistent, mild crossbite can be corrected with orthodontics in the future and is preferable to acute operative intervention in some cases.
Loss of permanent dentition may result from direct injury to the erupted tooth or damage to tooth buds. Iatrogenic damage to tooth buds may occur during rigid fixation with screws. Bioresorbable fixation can be used, but we prefer the use of titanium plates and screws [44]. We remove them at 6 months to prevent long-term growth disturbance and to allow ease of removal before they become encased in bone. This is especially important in mandibular angle fractures where a plate may interfere with future mandibular osteotomies. A Champy-style plate may interfere with the eruption of the third molar if not removed early (Figure 9). Nerve injury at the time of injury or during bony reduction may persist long term, although children are less likely to be symptomatic than adults.
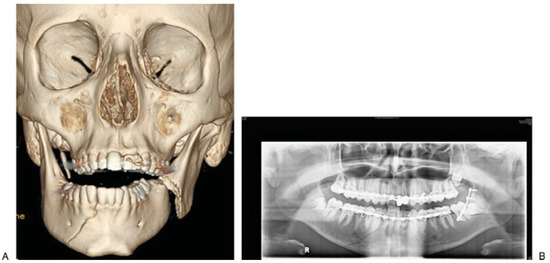
Figure 9.
(A,B) This patient sustained a blow to the right side of the face while playing ice hockey. There was an undisplaced right parasymphyseal fracture and a displaced angle fracture on the left side that was treated with a Champy-style plate. This will be removed to allow eruption of the third molar.
Conclusions
Pediatric facial fractures are relatively uncommon but represent a significant management problem when they do occur. It is important that clinicians involved in the care of these patients understand the differences between children and adult fracture patterns and understand the potential longer-term effects on the growth of the pediatric skeleton and how to manage these problems when they occur.
References
- Sgouros, S.; Goldin, J.H.; Hockley, A.D.; Wake, M.J.; Natarajan, K. Intracranial volume change in childhood. J. Neurosurg. 1999, 91, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Farkas, L.G.; Posnick, J.C.; Hreczko, T.M. Anthropometric growth study of the head. Cleft Palate Craniofac. J. 1992, 29, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Farkas, L.G.; Posnick, J.C.; Hreczko, T.M.; Pron, G.E. Growth patterns in the orbital region: A morphometric study. Cleft Palate Craniofac. J. 1992, 29, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Waitzman, A.A.; Posnick, J.C.; Armstrong, D.C.; Pron, G.E. Craniofacial skeletal measurements based on computed tomography: Part II. Normal values and growth trends. Cleft Palate Craniofac. J. 1992, 29, 118–128. [Google Scholar] [CrossRef]
- Grymer, L.F.; Gutierrez, C.; Stoksted, P. The importance of nasal fractures during different growth periods of the nose. J. Laryngol. Otol. 1985, 99, 741–744. [Google Scholar] [CrossRef]
- Sarnat, B.G. Normal and abnormal growth at the nasoseptovomeral region. Ann. Otol. Rhinol. Laryngol. 1991, 100, 508–515. [Google Scholar] [CrossRef]
- Farkas, L.G.; Posnick, J.C.; Hreczko, T.M. Growth patterns of the face: A morphometric study. Cleft Palate Craniofac. J. 1992, 29, 308–315. [Google Scholar] [CrossRef]
- Farkas, L.G.; Posnick, J.C.; Hreczko, T.M.; Pron, G.E. Growth patterns of the nasolabial region: A morphometric study. Cleft Palate Craniofac. J. 1992, 29, 318–324. [Google Scholar] [CrossRef]
- Ricketts, R.M. Planning treatment on the basis of the facial pattern and an estimate of its growth. Angle Orthod. 1957, 27, 14–37. [Google Scholar]
- Standring, S. (Ed.) Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 39th ed.; Churchill Livingston: London, UK, 2004. [Google Scholar]
- Enlow, D. Handbook of Facial Growth; WB Saunders: Philadelphia, PA, USA, 1982. [Google Scholar]
- Demianczuk, A.N.; Verchere, C.; Phillips, J.H. The effect on facial growth of pediatric mandibular fractures. J. Craniofac. Surg. 1999, 10, 323–328. [Google Scholar] [CrossRef]
- Yavuzer, R.; Sari, A.; Kelly, C.P.; et al. Management of frontal sinus fractures. Plast. Reconstr. Surg. 2005, 115, 79e–93e; discussion 94e–95e. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.C.; Amarante, J.M.; Silva, P.N.; et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast. Reconstr. Surg. 2005, 115, 1500–1508. [Google Scholar] [CrossRef] [PubMed]
- Imahara, S.D.; Hopper, R.A.; Wang, J.; Rivara, F.P.; Klein, M.B. Patterns and outcomes of pediatric facial fractures in the United States: A survey of the National Trauma Data Bank. J. Am. Coll. Surg. 2008, 207, 710–716. [Google Scholar] [PubMed]
- Messinger, A.; Radkowski, M.A.; Greenwald, M.J.; Pensler, J.M. Orbital roof fractures in the pediatric population. Plast. Reconstr. Surg. 1989, 84, 213–216; discussion 217–218. [Google Scholar]
- Alcalá-Galiano, A.; Arribas-García, I.J.; Martín-Pérez, M.A.; Romance, A.; Montalvo-Moreno, J.J.; Juncos, J.M.M. Pediatric facial fractures: Children are not just small adults. Radiographics 2008, 28, 441–461, quiz 618. [Google Scholar]
- Thorén, H.; Iso-Kungas, P.; Iizuka, T.; Lindqvist, C.; Törnwall, J. Changing trends in causes and patterns of facial fractures in children. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2009, 107, 318–324. [Google Scholar]
- Losee, J.E.; Afifi, A.; Jiang, S.; et al. Pediatric orbital fractures: Classification, management, and early follow-up. Plast. Reconstr. Surg. 2008, 122, 886–897. [Google Scholar]
- Strobl, H.; Emshoff, R.; Röthler, G. Conservative treatment of unilateral condylar fractures in children: A long-term clinical and radiologic follow-up of 55 patients. Int. J. Oral. Maxillofac. Surg. 1999, 28, 95–98. [Google Scholar]
- Eppley, B.L. Use of resorbable plates and screws in pediatric facial fractures. J. Oral. Maxillofac. Surg. 2005, 63, 385–391. [Google Scholar] [CrossRef]
- Singh, D.J.; Bartlett, S.P. Pediatric craniofacial fractures: Longterm consequences. Clin. Plast. Surg. 2004, 31, 499–518. [Google Scholar]
- Yaremchuk, M.J.; Fiala, T.G.; Barker, F.; Ragland, R. The effects of rigid fixation on craniofacial growth of rhesus monkeys. Plast. Reconstr. Surg. 1994, 93, 1–10; discussion 11–15. [Google Scholar] [PubMed]
- Baumeister, S.; Peek, A.; Friedman, A.; Levin, L.S.; Marcus, J.R. Management of postneurosurgical bone flap loss caused by infection. Plast. Reconstr. Surg. 2008, 122, 195e–208e. [Google Scholar] [PubMed]
- Bos, R.R.M. Treatment of pediatric facial fractures: The case for metallic fixation. J. Oral. Maxillofac. Surg. 2005, 63, 382–384. [Google Scholar] [PubMed]
- Rinehart, G.C.; Pittman, T. Growing skull fractures: Strategies for repair and reconstruction. J. Craniofac. Surg. 1998, 9, 65–72. [Google Scholar]
- Grant, G.A.; Jolley, M.; Ellenbogen, R.G.; Roberts, T.S.; Gruss, J.R.; Loeser, J.D. Failure of autologous bone-assisted cranioplasty following decompressive craniectomy in children and adolescents. J. Neurosurg. 2004, 100, 163–168. [Google Scholar] [CrossRef]
- Moore, M.H.; David, D.J.; Cooter, R.D. Oblique craniofacial fractures in children. J. Craniofac. Surg. 1990, 1, 4–7. [Google Scholar]
- Yaremchuk, M.J.; Posnick, J.C. Resolving Controversies related to the plate and screw fixation in the frowing craniofacial skeleton. J. Craniofac. Surg. 1995, 6, 525–538. [Google Scholar]
- Markowitz, B.L.; Manson, P.N.; Sargent, L.; et al. Management of the medial canthal tendon in nasoethmoid orbital fractures: The importance of the central fragment in classification and treatment. Plast. Reconstr. Surg. 1991, 87, 843–853. [Google Scholar]
- Sargent, L.A.; Rogers, G.F. Nasoethmoid orbital fractures: Diagnosis and management. J. Craniomaxillofac. Trauma. 1999, 5, 19–27. [Google Scholar]
- Clauser, L.; Dallera, V.; Sarti, E.; Tieghi, R. Frontobasilar fractures in children. Child’s Nerv. Syst. 2004, 20, 168–175. [Google Scholar]
- Mohindra, S.; Mukherjee, K.K.; Chhabra, R.; Gupta, R. Orbital roof growing fractures: A report of four cases and literature review. Br. J. Neurosurg. 2006, 20, 420–423. [Google Scholar] [CrossRef] [PubMed]
- Jordan, D.R.; Allen, L.H.; White, J.; Harvey, J.; Pashby, R.; Esmaeli, B. Intervention within days for some orbital floor fractures: The white-eyed blowout. Ophthal Plast. Reconstr. Surg. 1998, 14, 379–390. [Google Scholar] [CrossRef] [PubMed]
- Criden, M.R.; Ellis, F.J. Linear nondisplaced orbital fractures with muscle entrapment. J. AAPOS 2007, 11, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.; Lisman, R.D.; Simonton, J.; Della Rocca, R. Volkmann’s contracture of the extraocular muscles following blowout fracture. Plast. Reconstr. Surg. 1984, 74, 200–216. [Google Scholar] [CrossRef]
- Cole, P.; Boyd, V.; Banerji, S.; Hollier, L.H., Jr. Comprehensive management of orbital fractures. Plast. Reconstr. Surg. 2007, 120 (Suppl. S2), 57S–63S. [Google Scholar] [CrossRef]
- Liao, Y.-F.; Cole, T.J.; Mars, M. Hard palate repair timing and facial growth in unilateral cleft lip and palate: A longitudinal study. Cleft Palate Craniofac. J. 2006, 43, 547–556. [Google Scholar] [CrossRef]
- Wojtaszek-Slominska, A.; Renkielska, A.; Dobke, M.; Gosman, A.; Slominski, W. Orthodontic characteristics of maxillary arch deficiency in 5-year-old patients undergoing unilateral cleft lip and palate repair with and without early gingivoplasty. J. Craniomaxillofac. Surg. 2010, 38, 155–159. [Google Scholar] [CrossRef]
- Smartt, J.M., Jr.; Low, D.W.; Bartlett, S.P. The pediatric mandible: II. Management of traumatic injury or fracture. Plast. Reconstr. Surg. 2005, 116, 28e–41e. [Google Scholar] [CrossRef]
- Zimmermann, C.E.; Troulis, M.J.; Kaban, L.B. Pediatric facial fractures: Recent advances in prevention, diagnosis and management. Int. J. Oral. Maxillofac. Surg. 2006, 35, 2–13. [Google Scholar] [CrossRef]
- Landes, C.A.; Day, K.; Glasl, B.; Ludwig, B.; Sader, R.; Kovács, A.F. Prospective evaluation of closed treatment of nondisplaced and nondislocated mandibular condyle fractures versus open reposition and rigid fixation of displaced and dislocated fractures in children. J. Oral. Maxillofac. Surg. 2008, 66, 1184–1193. [Google Scholar] [CrossRef]
- He, D.; Ellis, E., III; Zhang, Y. Etiology of temporomandibular joint ankylosis secondary to condylar fractures: The role of concomitant mandibular fractures. J. Oral. Maxillofac. Surg. 2008, 66, 77–84. [Google Scholar] [CrossRef]
- Dorri, M.; Nasser, M.; Oliver, R. Resorbable versus titanium plates for facial fractures. Cochrane Database Syst. Rev. 2018, 5, CD007158. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2011 by the author. The Author(s) 2011.