Isolated Orbital Fracture—Treatment and Outcomes in a Single Tertiary Care Centre
Abstract
Introduction
Materials and methods
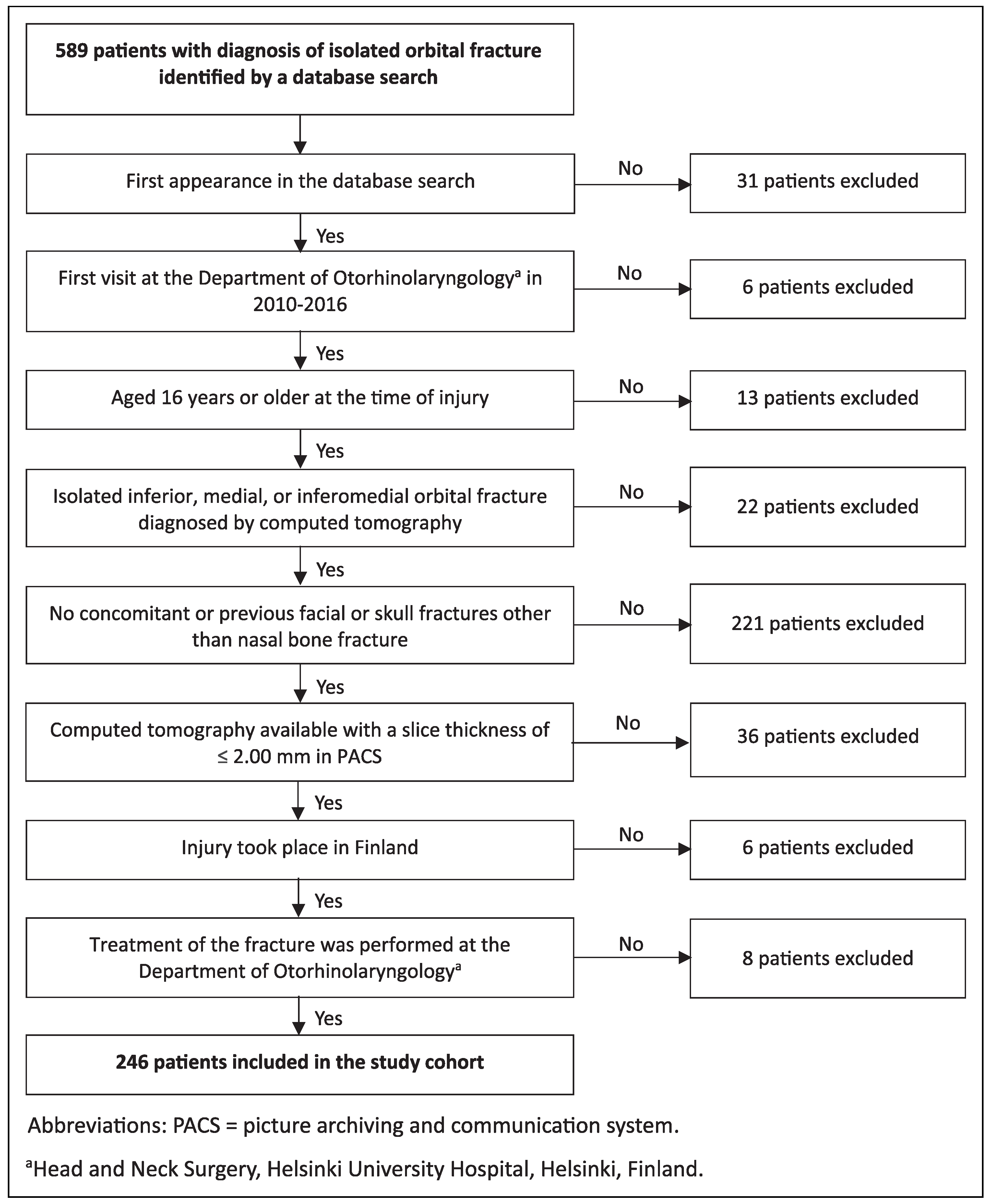
Study Design and Patient Selection
Inclusion Criteria
Study Variables
Statistical Methods
Ethical Considerations
Results
Patient Inclusion
Demographics and Injury Aetiology
Treatment Modality, Surgical Approach, and Reconstruction Material
Location of Fracture
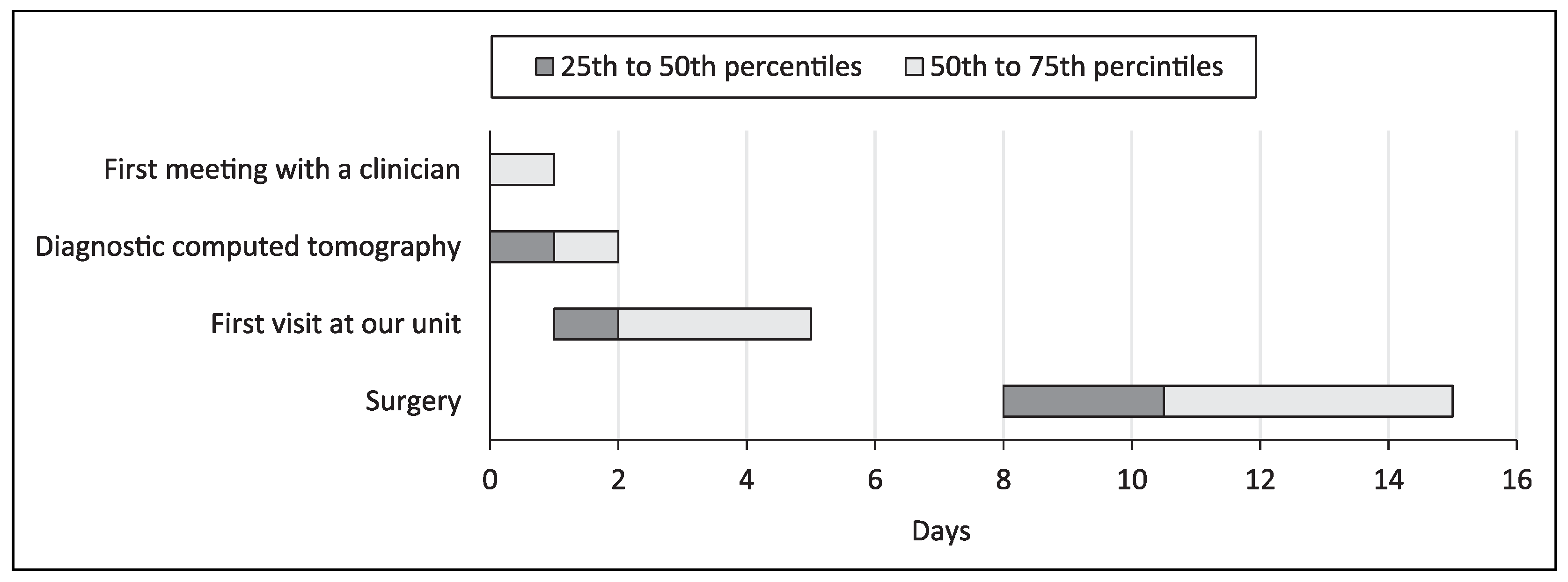
Time Intervals in the Care Pathway
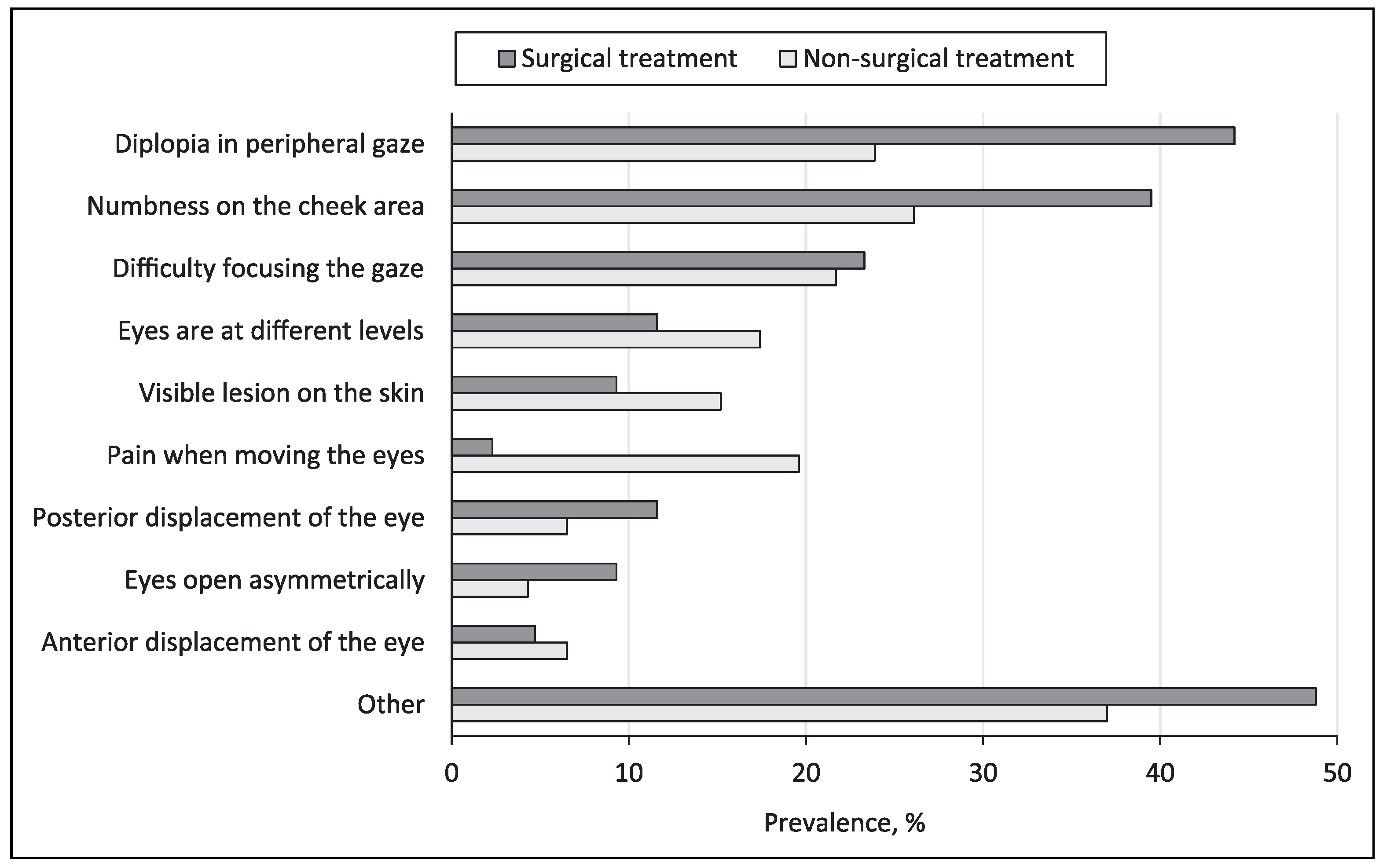
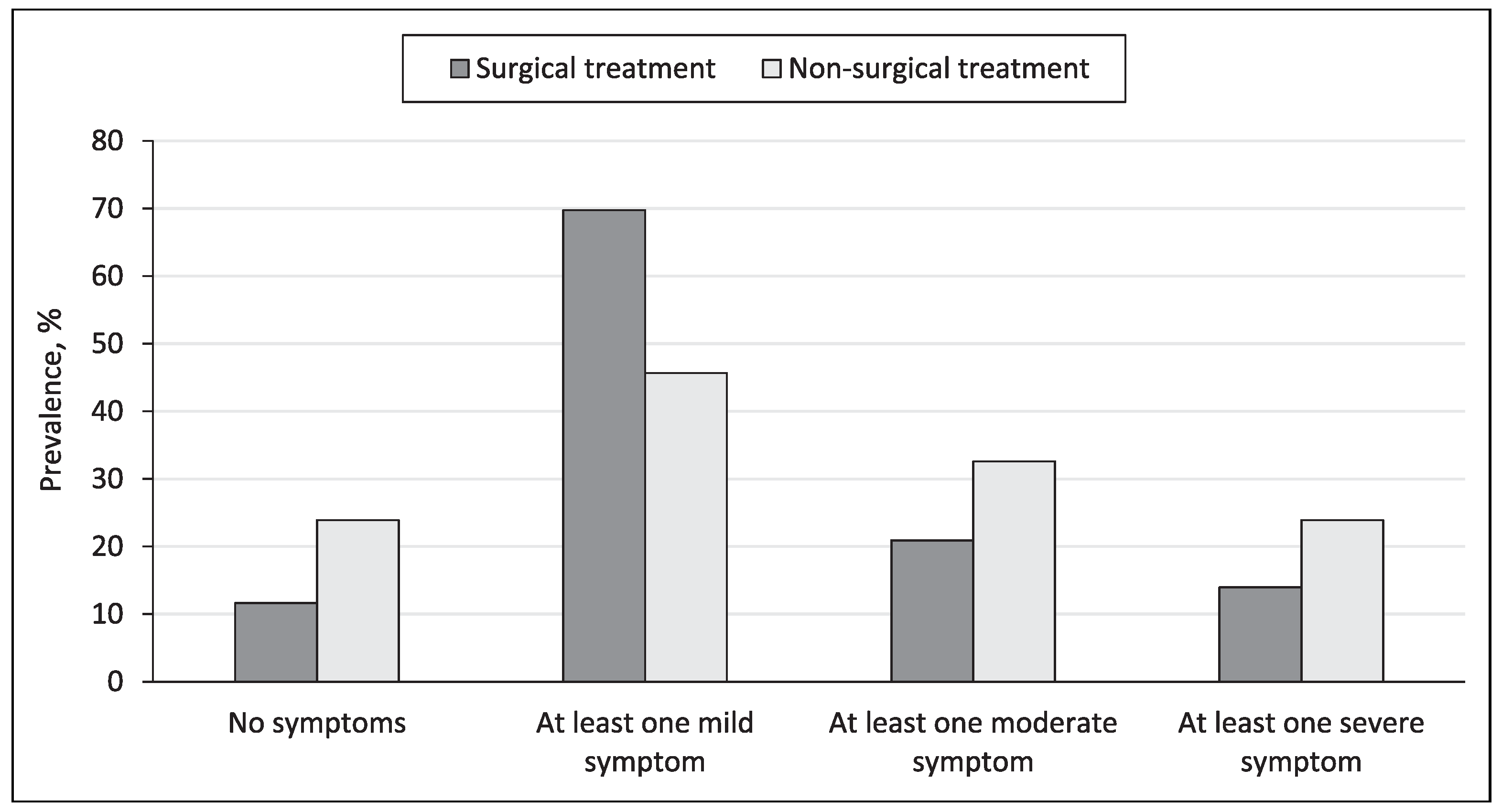
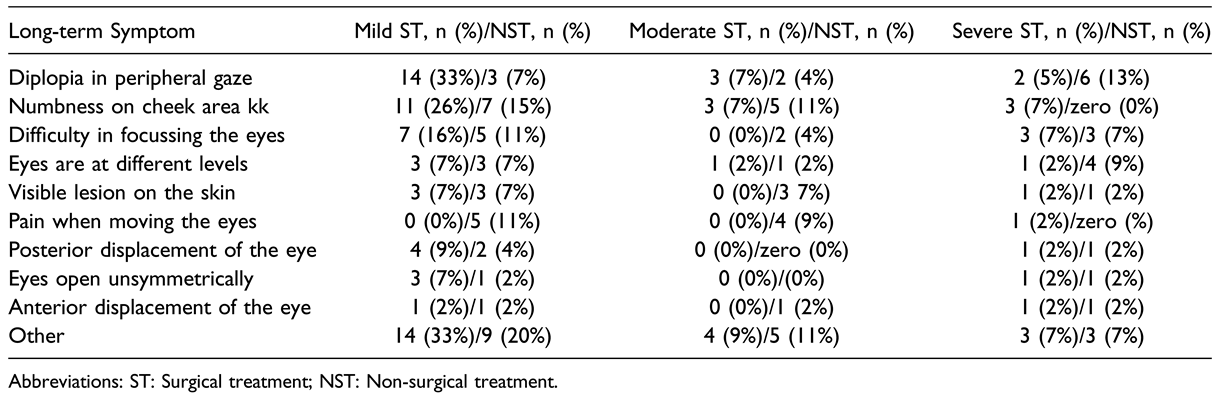
Questionnaire and Long-Term Symptoms
Discussion
Conclusion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Arangio, P.; Vellone, V.; Torre, U.; Calafati, V.; Capriotti, M.; Cascone, P. Maxillofacial fractures in the province of Latina, Lazio, Italy: Review of 400 injuries and 83 cases. J Cranio-Maxillofac Surg Off Publ Eur Assoc Cranio-Maxillofac Surg. 2014, 42, 583–587. [Google Scholar] [CrossRef]
- Bonitz, L.; Wruck, V.; Peretti, E.; Abel, D.; Hassfeld, S.; Bicsák, Á. Long-term evaluation of treatment protocols for isolated midfacial fractures in a German nation-wide craniomaxillofacial trauma center 2007-2017. Sci Rep. 2021, 11, 18291. [Google Scholar] [CrossRef]
- Ahmad, F.; Kirkpatrick, N.A.; Lyne, J.; Urdang, M.; Waterhouse, N. Buckling and hydraulic mechanisms in orbital blowout fractures: Fact or fiction? J Craniofac Surg. 2006, 17, 438. [Google Scholar] [CrossRef] [PubMed]
- Burnstine, M.A. Clinical recommendations for repair of isolated orbital floor fractures: An evidence-based analysis. Ophthalmology. 2002, 109, 1207–1210. [Google Scholar] [CrossRef] [PubMed]
- Dubois, L.; Dillon, J.; Jansen, J.; Becking, A.G. Ongoing debate in clinical decision making in orbital fractures: Indications, timing, and biomaterials. Atlas Oral Maxillofac Surg Clin North Am. 2021, 29, 29–39. [Google Scholar] [CrossRef]
- Dubois, L.; Steenen, S.A.; Gooris, P.J.J.; Mourits, M.P.; Becking, A.G. Controversies in orbital reconstruction--II. Timing of posttraumatic orbital reconstruction: A systematic review. Int J Oral Maxillofac Surg. 2015, 44, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Cole, B.L.; Tran, A.Q. Controversies in ophthalmology: Timing of isolated orbital floor fracture repair. Int Ophthalmol Clin. 2022, 62, 63–67. [Google Scholar] [CrossRef]
- Wood, J.; Adeoye, J. Literature review to create evidence based care pathway for isolated adult orbital blowout fractures. Strabismus. 2021, 29, 120–124. [Google Scholar] [CrossRef]
- Basta, M.N.; Rao, V.; Roussel, L.O.; Crozier, J.W.; Liu, P.Y.; Woo, A.S. Refining indications for orbital floor fracture reconstruction: A risk-stratification tool predicting symptom development and need for surgery. Plast Reconstr Surg. 2021, 148, 606. [Google Scholar] [CrossRef]
- Scolozzi, P. Reflections on a patient-centered approach to treatment of blow-out fractures: Why the wisdom of the pastmust guide our decision-making. J Plast Reconstr Aesthetic Surg JPRAS. 2022, 75, 2268–2276. [Google Scholar] [CrossRef]
- Alinasab, B.; Borstedt, K.J.; Rudström, R.; et al. New algorithm for the management of orbital blowout fracture based on prospective study. Craniomaxillofacial Trauma Reconstr. 2018, 11, 285–295. [Google Scholar] [CrossRef]
- Soliman, L.; Sawicki, N.; Sobti, N.; Swartz, S.; Rao, V.; Woo, A.S. Re-Evaluating the timing of surgery after isolated orbital floor fracture. Plast Reconstr Surg Glob Open. 2023, 11, e4973. [Google Scholar] [CrossRef]
- Kersten, R.C.; Vagefi, M.R.; Bartley, G.B. Orbital “blowout” fractures: Time for a new paradigm. Ophthalmology. 2018, 125, 796–798. [Google Scholar] [CrossRef] [PubMed]
- Gooris, P.J.J.; Jansen, J.; Bergsma, J.E.; Dubois, L. Evidence-based decision making in orbital fractures: Implementation of a clinical protocol. Atlas Oral Maxillofac Surg Clin North Am. 2021, 29, 109–127. [Google Scholar] [CrossRef] [PubMed]
- Wevers, M.; Strabbing, E.M.; Engin, O.; Gardeniers, M.; Koudstaal, M.J. CT parameters in pure orbital wall fractures and their relevance in the choice of treatment and patient outcome: A systematic review. Int J Oral Maxillofac Surg. 2022, 51, 782–789. [Google Scholar] [CrossRef] [PubMed]
- Billig, A.B.; Dengler, J.; Hardisty, M.; Chew, H.F.; Kiss, A.; Fialkov, J.A. Are we overoperating on isolated orbital floor fractures? Plast Reconstr Surg. 2023, 152, 629–637. [Google Scholar] [CrossRef]
- Pyötsiä, K.; Lehtinen, V.; Toivari, M.; Puolakkainen, T.; Lowery Wilson, M.; Snäll, J. Three-dimensional computer-aided analysis of 293 isolated blowout fractures which radiological findings guide treatment decision? J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2021, 79, 2306–2318. [Google Scholar] [CrossRef]
- Jansen, J.; Dubois, L.; Maal, T.J.J.; et al. A nonsurgical approach with repeated orthoptic evaluation is justified for most blowout fractures. J Cranio-Maxillo-fac Surg Off Publ Eur Assoc Cranio-Maxillo-fac Surg. 2020, 48, 560–568. [Google Scholar] [CrossRef]
- Senese, O.; Boutremans, E.; Gossiaux, C.; Loeb, I.; Dequanter, D. Retrospective analysis of 79 patients with orbital floor fracture: Outcomes and patient-reported satisfaction. Arch Craniofacial Surg. 2018, 19, 108–113. [Google Scholar] [CrossRef]
- Rajantie, H.; Kaukola, L.; Sna¨ll, J.; Roine, R.; Sintonen, H.; Thore´n, H. Health-related quality of life in patients surgically treated for orbital blow-out fracture: A prospective study. Oral Maxillofac Surg. 2021, 25, 373–382. [Google Scholar] [CrossRef]
- Brucoli, M.; Arcuri, F.; Cavenaghi, R.; Benech, A. Analysis of complications after surgical repair of orbital fractures. J Craniofac Surg. 2011, 22, 1387–1390. [Google Scholar] [CrossRef]
- Lubamba, G.P.; Dai, X.; Song, Z.; et al. Assessment of quality of life in patients treated for orbital fractures. J Stomatol Oral Maxillofac Surg. 2023, 25, 101486. [Google Scholar] [CrossRef]
- Hartwig, S.; Nissen, M.C.; Voss, J.O.; et al. Clinical outcome after orbital floor fracture reduction with special regard to patient’s satisfaction. Chin J Traumatol Zhonghua Chuang Shang Za Zhi. 2019, 22, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Kasaee, A.; Mirmohammadsadeghi, A.; Kazemnezhad, F.; Eshraghi, B.; Akbari, M.R. The predictive factors of diplopia and extraocular movement limitations in isolated pure blowout fracture. J Curr Ophthalmol. 2017, 29, 54–58. [Google Scholar] [CrossRef]
- Braaksma-Besselink, Y.; Jellema, H.M. Orthoptic evaluation and treatment in orbital fractures. Atlas Oral Maxillofac Surg Clin North Am. 2021, 29, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.C.; Ma, L.; Wu, S.Y.; Yang, F.R.; Tsai, Y.J. Orbital blow-out fractures in children: Characterization and surgical outcome. Chang Gung Med J. 2010, 33, 313–320. [Google Scholar] [PubMed]
- Matteini, C.; Renzi, G.; Becelli, R.; Belli, E.; Iannetti, G. Surgical timing in orbital fracture treatment: Experience with 108 consecutive cases. J Craniofac Surg. 2004, 15, 145. [Google Scholar] [CrossRef]
- Christensen, B.J.; Zaid, W. Inaugural survey on practice patterns of orbital floor fractures for American oral and maxillofacial surgeons. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2016, 74, 105–122. [Google Scholar] [CrossRef]
- Cohen, L.M.; Shaye, D.A.; Yoon, M.K. Isolated orbital floor fracture management: A survey and comparison of American oculofacial and facial plastic surgeon preferences. Craniomaxillofacial Trauma Reconstr. 2019, 12, 112–121. [Google Scholar] [CrossRef]
- Francomacaro, S.E.; Bregman, J.A.; Vakharia, K.T.; Grumbine, F.L. The utility of postoperative computed tomography imaging following isolated orbital blowout fracture repair. Craniomaxillofacial Trauma Reconstr. 2020, 13, 198–204. [Google Scholar] [CrossRef]
- Taxis, J.; Ungerboeck, L.; Gehrking, M.R.; et al. Two-dimensional post-traumatic measurements of orbital floor blowout fractures underestimate defect sizes compared to threedimensional approaches. Tomogr Ann Arbor Mich. 2023, 9, 579–588. [Google Scholar] [CrossRef]
- Pitak-Arnnop, P.; Witohendro, L.K.; Tangmanee, C.; et al. Assessing effectiveness of endoscope-assisted medial orbital wall fracture repair vs. no surgery using benefit-risk metrics and literature review. J Stomatol Oral Maxillofac Surg. 2023, 124, 101267. [Google Scholar] [CrossRef] [PubMed]
- Alafaleq, M.; Roul-Yvonnet, F.; Schouman, T.; Goudot, P. A retrospective study of pure medial orbital wall fracture management. J Fr Ophtalmol. 2019, 42, 592–596. [Google Scholar] [CrossRef]
- Sung, Y.S.; Chung, C.M.; Hong, I.P. The correlation between the degree of enophthalmos and the extent of fracture in medial orbital wall fracture left untreated for over six months: A retrospective analysis of 81 cases at a single institution. Arch Plast Surg. 2013, 40, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Mo, Y.W.; Ryu, D.H.; Shin, H.K.; Lee, W.J. Prediction of enophthalmos in medial orbital wall fracture: Suggested coordinate plane for making surgical decisions. J Craniofac Surg. 2023, 34, 1185–1190. [Google Scholar] [CrossRef]
- Snell, B.J.; Flapper, W.; Moore, M.; Anderson, P.; David, D.J. Management of isolated fractures of the medial orbital wall. J Craniofac Surg. 2013, 24, 291–294. [Google Scholar] [CrossRef]
 |
 |
© 2024 by the author. The Author(s) 2024.
Share and Cite
Maunula, M.K.K.; Blomgren, K.; Sinkkonen, S.T.; Nyman, K.; Tapiovaara, L.K. Isolated Orbital Fracture—Treatment and Outcomes in a Single Tertiary Care Centre. Craniomaxillofac. Trauma Reconstr. 2024, 17, 68. https://doi.org/10.1177/19433875241247370
Maunula MKK, Blomgren K, Sinkkonen ST, Nyman K, Tapiovaara LK. Isolated Orbital Fracture—Treatment and Outcomes in a Single Tertiary Care Centre. Craniomaxillofacial Trauma & Reconstruction. 2024; 17(4):68. https://doi.org/10.1177/19433875241247370
Chicago/Turabian StyleMaunula, Mirko K. K., Karin Blomgren, Saku T. Sinkkonen, Kristofer Nyman, and Laura K. Tapiovaara. 2024. "Isolated Orbital Fracture—Treatment and Outcomes in a Single Tertiary Care Centre" Craniomaxillofacial Trauma & Reconstruction 17, no. 4: 68. https://doi.org/10.1177/19433875241247370
APA StyleMaunula, M. K. K., Blomgren, K., Sinkkonen, S. T., Nyman, K., & Tapiovaara, L. K. (2024). Isolated Orbital Fracture—Treatment and Outcomes in a Single Tertiary Care Centre. Craniomaxillofacial Trauma & Reconstruction, 17(4), 68. https://doi.org/10.1177/19433875241247370




