Introduction
Orbital trauma has significant implications for overall health and quality of life. Complications of orbital trauma include vision loss, precipitation of oculocardiac reflex, impaired extraocular motion, and other concurrent injuries [
1]. Orbital injuries pose distinctive challenges at various life stages. In childhood, orbital injuries are more likely to cause neurologic damage due to decreased protection from developing bones [
2]. Adolescents, particularly males, face an increased risk of orbital injuries, often due to factors such as increased risk-taking behaviors and life stressors [
3]. Working-age adults are susceptible to orbital injuries related to their occupations or lifestyles, with socioeconomic status influencing the likelihood of such incidents [
4]. In older adulthood, the risk of certain injuries, such as those resulting from falls, rises due to declining physical function and the presence of chronic health conditions [
5]. Recognizing and mitigating these unique risk factors at different stages of life is critical for crafting tailored preventive measures, allocating healthcare resources, and ensuring prompt recognition and treatment for orbital injuries across all age groups.
Understanding these factors is especially important in the most vulnerable groups, namely elderly adults. Though there is extensive literature regarding trauma in patients aged 65 years and older, much of it focuses on injuries to the head, hip, and extremities. There remains a dearth of research investigating orbital trauma in geriatric populations. A retrospective study by Toviari et al found that associated non-facial injuries, especially brain injuries were more common in elderly adults with zygomatico-orbital fractures [
6]. It has also been shown that elderly adults who sustained craniofacial trauma had increased length of hospital stay, increased incidence of death during hospitalization, and increased use of post-discharge resources like rehabilitation services [
7].
Utilizing 10 years of data from the National Electronic Injury Surveillance System (NEISS) database, this study aims to compare the epidemiology of consumer productrelated orbital injuries across different life stages: young children, adolescents, working adults, and elderly adults. Such information can provide healthcare providers and policymakers the data to create targeted preventive measures and interventions to mitigate the risk of orbital injuries and enhance patient outcomes.
Methods
This study was IRB exempt because it utilized existing data that are publicly available and deidentified. Consent was not collected since all patients represented were from a deidentified database. Research was conducted in accordance with the Declaration of Helsinki.
This study reports a retrospective analysis of patient data from the National Electronic Injury Surveillance System (NEISS) collected by the Consumer Product Safety Commission (CPSC) from 2013 to 2022 in the United States. The NEISS is a nationally representative probability sample collected from 100 US hospital emergency departments that reports data on consumer product-related injuries. The included hospitals all have at least 6 beds and provide 24-hour emergency care. Of note, licensed automobiles are not reported in the NEISS. National estimates of orbital injuries can be extrapolated from the NEISS data based on the provided sample weights. The NEISS includes information extracted from medical charts, including patient demographics (i.e. age, sex, and race) and injury information including body part injured, diagnosis, location where the injury occurred, product involved, and a narrative of the injury event. Orbital injuries were identified by searching the narrative reports for the term “orbital” and other common misspellings.
The study sample was categorized by life stage: young children aged 0-5 year-olds (y/o), adolescents aged 6-17 y/ o, working adults 18-64 y/o, and elderly adults 65 + y/o. Yearly incidence was calculated using national estimates of orbital injuries from the NEISS and intercensal/postcensal national population estimates reported by year from the US Census Bureau [
8].
Comparative analyses were performed to assess differences in the epidemiologic characteristics of orbital injuries by age. Demographics, injury location, products involved, and disposition were compared between age groups.
Statistical Analysis
Microsoft Excel (Mac V16.83) was used for all analyses, and P-values <0.01 were considered statistically significant. Pearson’s chi-squared tests were used to compare proportions between groups. Demographic data (age, sex, race) were represented as percentiles by subdividing the population based on identifying characteristics.
Results
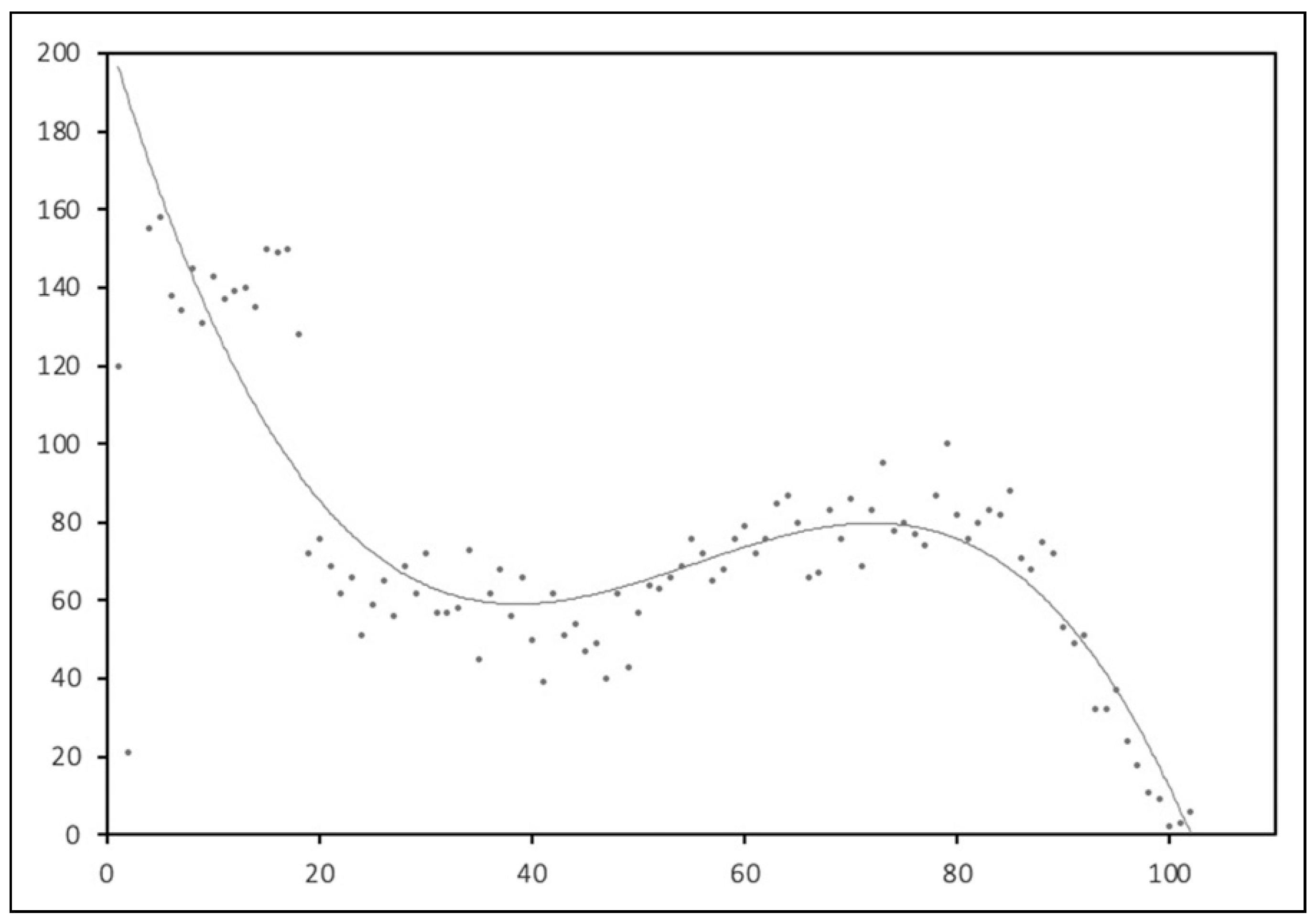
Among the 7846 orbital injuries reported in the NEISS from 2013-2022: 973 (12.4%) occurred in the 0-5 age group; 1680 (21.4%) in the 6-17 age group; 2970 (37.6%) in the 18-64 age group; and 2223 (28.3%) in the 65+ age group. The number of orbital injuries with respect to age had a bimodal distribution, with the highest frequency in young patients followed by another peak around age 80 (
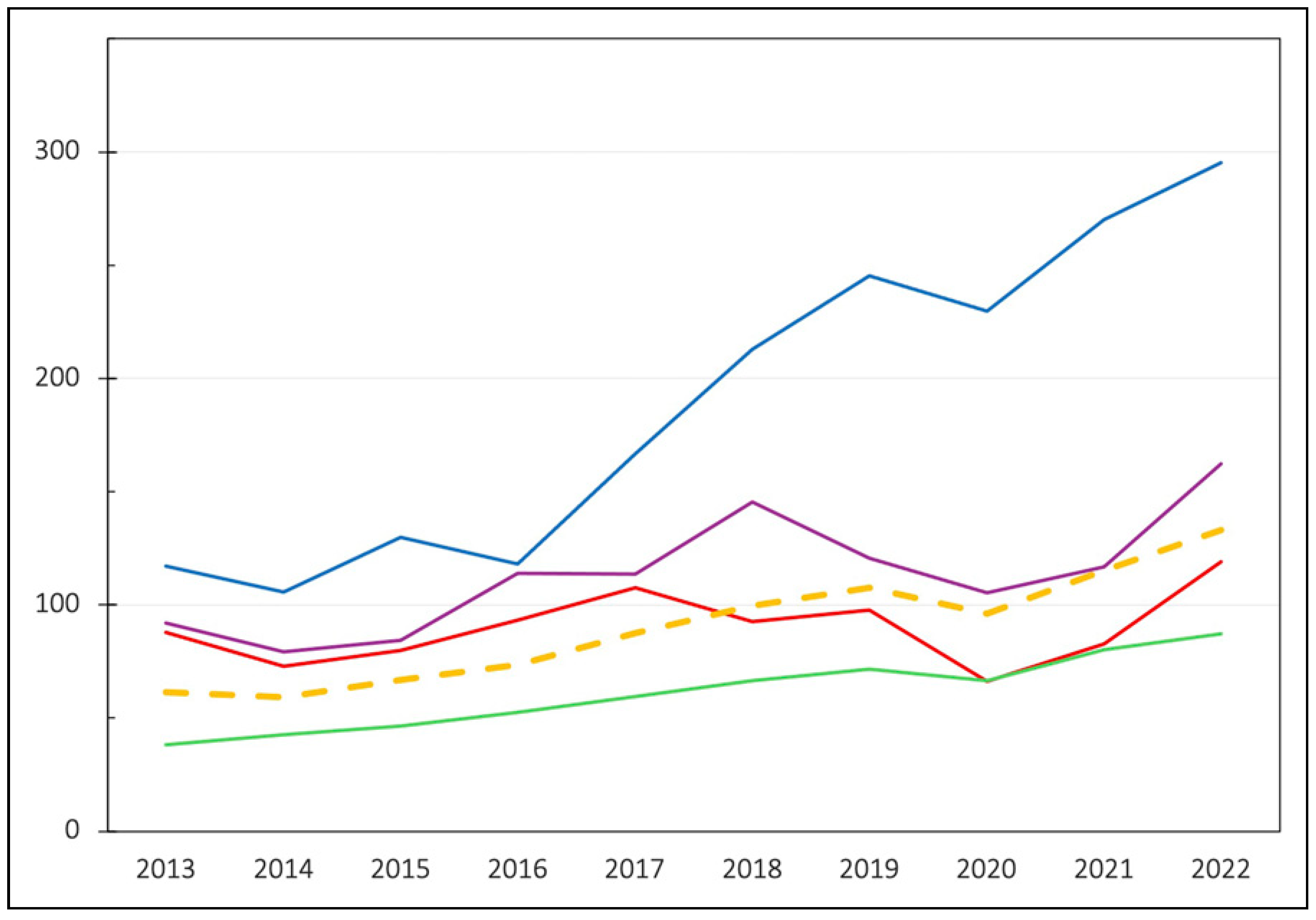
Figure 1). The yearly incidence using national estimates more than doubled over the study period, from 61.3 orbital injuries per million person-years in 2013 to 133.0 injuries per million person-years in 2022 (
Figure 2). On average, year to year incidence increased by 8.4% in 0-5 y/o, 5.8% in 6-17 y/o, 9.8% in 18-64 y/o, and 12.1% in 65 + y/o during the study period.
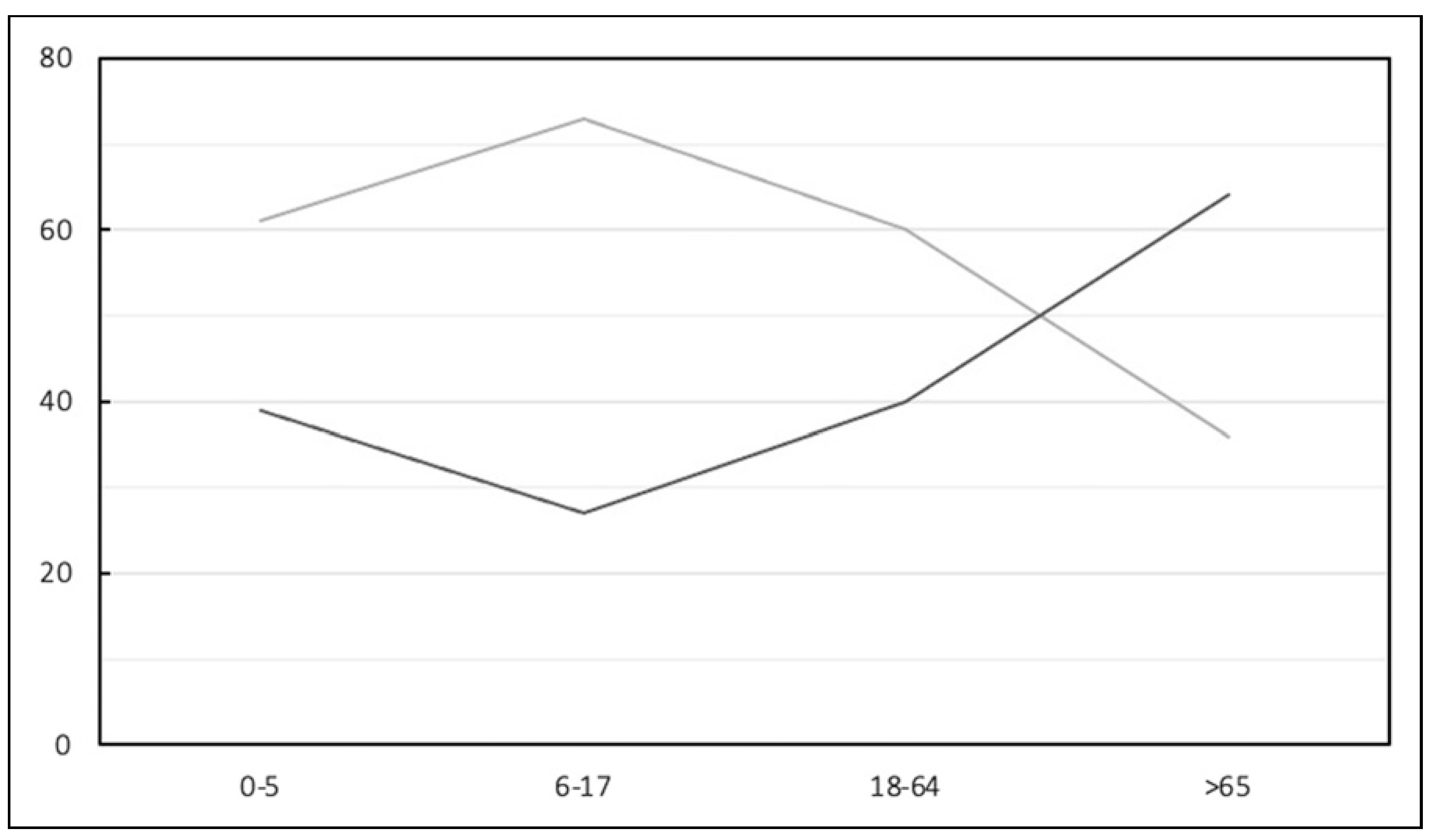
Males made up 56.2% of the cohort overall. There were statistically significantly fewer males in the >65 group (
P < 0.001) and more males in the 617 group (
P < 0.001) compared to the other age groups (
Figure 3). The majority of patients with orbital injuries were white (53.8%) followed by African American (13.4%). The proportion of injuries in white patients increased with age, with the highest number occurring in the 65+ age group (49.5% in the 0-5 age group vs 61.2% in the 65+ age group,
P < 0.001). The opposite trend was observed in African Americans, with a decrease in proportion of injuries observed with increasing age (19.5% in the 0-5 age group vs 8.6% in the 65+ age group,
P < 0.001). Patients whose race was reported as “other” also saw a decrease in injuries with age (7.4% in the 0-5 age group vs 1.3% in the 65+ age group,
P < 0.001).
Injury location was different between the age groups: 617 y/o were more frequently injured at places of sport (0-5 to 65+: 5.2% vs 43.8% vs 13.3% vs 1.8%,
P < 0.001), whereas 0-5 y/o and 65 + y/o were more likely to sustain injuries at home (0-5 to 65+: 60.6% vs 19.3% vs 34.9% vs 58.9%, < 0.001) (
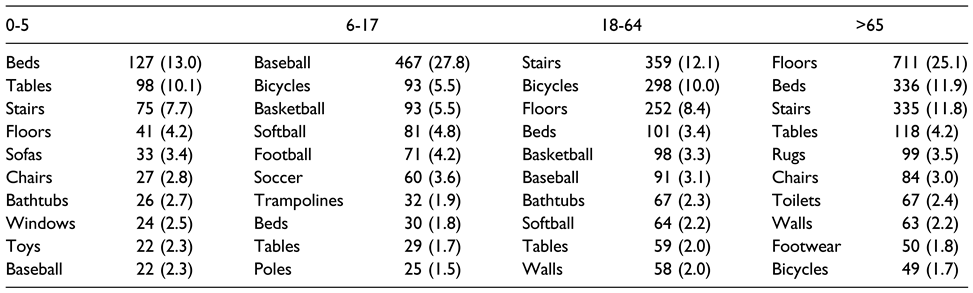
Figure 4).The top 10 products involved in orbital injuries for each age group are reported in
Table 1. Like the injury location results, a majority of the top 10 products for 6-17 y/o were sports-related, while both the 0-5 and 65+ age groups were more commonly injured by household products. The 18-64 group was injured by a mixture of products. Alcohol involvement was most frequently reported in the 18-64 age group (0-5 to 65+: 0.0% vs 0.1% vs 14.9% vs 4.0%,
P < 0.001).
Fractures were the most common type of injury across all age groups (40.6%), with the highest rate observed in the 18-64 age group; internal organ injuries were most common in the 65+ age groups, (
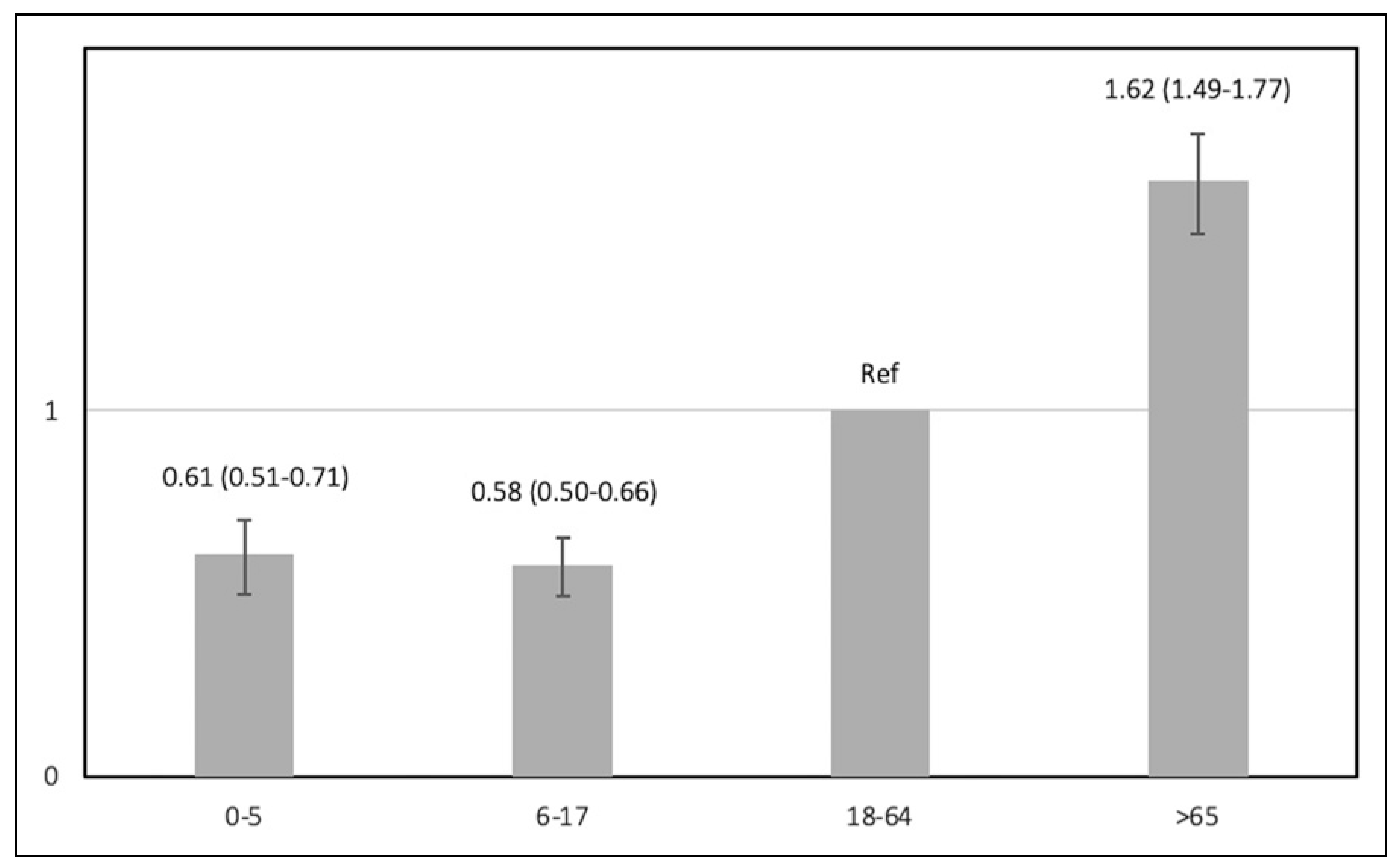
Figure 5). Disposition was also different between age groups. Overall, 24.2% of patients were admitted, with 0-5 y/o and 6-17 y/o having a lower risk of being admitted compared to 18-64 y/o, while 65 + y/o had a higher risk of being admitted (
Figure 6).
Discussion
Orbital trauma can have a significant burden on patients and the healthcare system. This study examines 7846 orbital injuries documented in the NEISS over the past decade. Distinct patterns and risk factors associated with orbital injuries were recognized between the different life stages. There was a bimodal peak in the occurrence of orbital injuries with respect to age, with the first, and higher peak in injuries noted between the ages of 0-20 years and the second peak at age 80 years. This is in concurrence with previously reported data [
9]. The incidence of orbital injuries more than doubled over the past decade in all age groups. A prior study found that the incidence of orbital floor fractures increased by 50% from 2006-2017 [
10]. The current study shows an even more rapid rise from 2013-2022, with the incidence more than doubling. Interestingly, several prior studies examining ocular traumas—including one that analyzed the NEISS—have found an opposite trend, with the incidence decreasing over time [
11,
12,
13] These authors suggest that ocular injuries have decreased due improved safety awareness and stricter eye protection standards. The results of the current study suggest that improved safety measures may not protect against the high-force mechanisms implicated in orbital injuries. While incidence did increase in all life stages, the most dramatic rise was seen in elderly adults, suggesting that preventative interventions are most needed in this group.
Individuals aged 65 and older were most likely to sustain injuries at home from common household products, possibly due to factors such as reduced mobility, sensory and proprioceptive changes, and side-effects of polypharmacy. Of the top ten products causing injury in elderly adults, most may be extrapolated to be involved with falls or causing falls. Fall prevention measures and initiatives to create homes with built-in safety features may help to mitigate the increasing rates of orbital trauma amongst elderly adults. Elderly adults also had a significantly higher risk of being admitted to the hospital, suggesting that their injuries were generally more severe. Young children aged 0-5 years were also more frequently injured by household items, reflecting the nature of their surroundings and developmental stage. Previous works have suggested that people at the extremes of the age are prone to blunt orbital injuries from falling onto flat surfaces due to morphologically “less prominent eyes.” Young children have underdeveloped orbits while older adults have decreased orbital contents due to aging, consequently leading to distortion of the orbital rim and walls during impact [
14]. This may explain why internal organ injury—most likely to the globe or brain—were more common in these age groups in this study. However, fractures were more common in older adults, likely due to more elastic bone in children and decreases in bone-mineral density with age.
In contrast, location and product data suggest orbital injuries in adolescents are most often sports-related, likely due to increased physical activity and participation in sports. Working adults exhibited a mixed pattern of injuries, reflecting the diverse range of activities and lifestyles within this demographic. These results are consistent with prior studies that have demonstrated a wide range of mechanisms of injury in 18-64 year old age group, including but not limited to assault, alcohol-related incidents, motor vehicle accidents, and sports [
15,
16].
Among elderly adults, this study showed that females were more common than males. Across all other age groups, males were more common. This trend has previously been seen with other injuries, where females are more likely to sustain falls as well as maxillofacial trauma in older age groups [
17,
18,
19]. This trend may be because there are generally a higher proportion of females than males in geriatric populations [
20]. Males made up the majority of patients in all other age groups, with the highest proportion seen in 6-17 y/o. Adolescent males exhibit more risk-taking behaviors and violence than adolescent females, which may explain this result [
3,
21].
Racial/ethnic differences in orbital injuries were also observed, aligning with existing literature on fracture risk and injury patterns among different populations. Specifically, the proportion of orbital injuries in white patients was found to increase with age, while the opposite trend was observed in Black patients. A previous study that identified this trend in overall fractures suggests that Black populations have a decreased life expectancy compared to white populations, potentially explaining the lower representation of Black patients in the older age groups (Bao et al. 2023) [
22]. Anatomic differences in orbital morphology have also been documented, with certain populations being more prone to specific types of fractures. For example, Asians and AfroCaribbeans are more likely to suffer fractures to the medial wall of the orbit, while Caucasians are more prone to fractures of the orbital floor [
23]. These anatomical variations, coupled with socioeconomic factors, could contribute to the disparities in injury patterns seen in our study. Further research is needed to fully elucidate the underlying mechanisms driving racial/ethnic disparities in orbital injury epidemiology.
Alcohol involvement notably manifested most frequently among individuals aged 18-64, aligning with established research indicating that this demographic tends to exhibit more risk-taking behaviors and increased susceptibility to alcohol-induced impairments in coordination, balance, and judgment [
24,
25,
26]. This vulnerability among younger adults may be due to increased engagement in activities characterized by elevated risk, such as physical altercations and high-risk sports, thereby increasing their likelihood of sustaining alcohol-related injuries. In contrast, this study found a much smaller proportion of alcohol-related injuries in elderly adults. Previous studies have indicated that older adults may exhibit greater caution and lower overall alcohol consumption rates, contributing to fewer alcohol-related injuries in this age group [
27,
28]. While age-related changes to alcohol metabolism and tolerance may result in higher blood alcohol concentrations in older adults for a given amount of alcohol consumed, behavioral changes towards exhibiting more caution appear to temper these physiologic effects [
28].
This study had some limitations. The NEISS is national database, which makes it vulnerable to coding errors or variation in coding practices between institutions. Only patients who sought medical care in the emergency setting were included. Therefore, those who experienced orbital injuries but did not seek medical care are not represented within this study. Furthermore, this study may have limited applicability to populations outside the US given that several studies in the past have shown great variation in orbital trauma amongst different countries with varying socioeconomic climates. Finally, since licensed motor vehicles are not included in the NEISS, this significant source of trauma is not reported in this study’s results. Previous research has found that among patients with ocular injuries, motor vehicle accidents are more common in younger patients in their 30s [
4]. Another study found that patients with orbital floor fractures sustained in motor vehicle accidents were more likely to be hospitalized than those injured through other mechanisms [
10]. More research is still needed on the epidemiology of orbital injuries caused by motor vehicle accidents. Despite these limitations, the NEISS is a nationally representative database, making the results of this study generalizable to the population of the United States. Furthermore, several key differences in epidemiological characteristics between the life stages were identified, which can help guide future preventative health measures and better guide clinical practice.