Pediatric Facial Fractures: A Multi-Institutional Level 1 Trauma Center Analysis of Incidence, Interventions, and Outcomes
Abstract
Introduction
Facial Trauma in the Developing Child and Adolescent
Pediatric Consequences from Facial Trauma
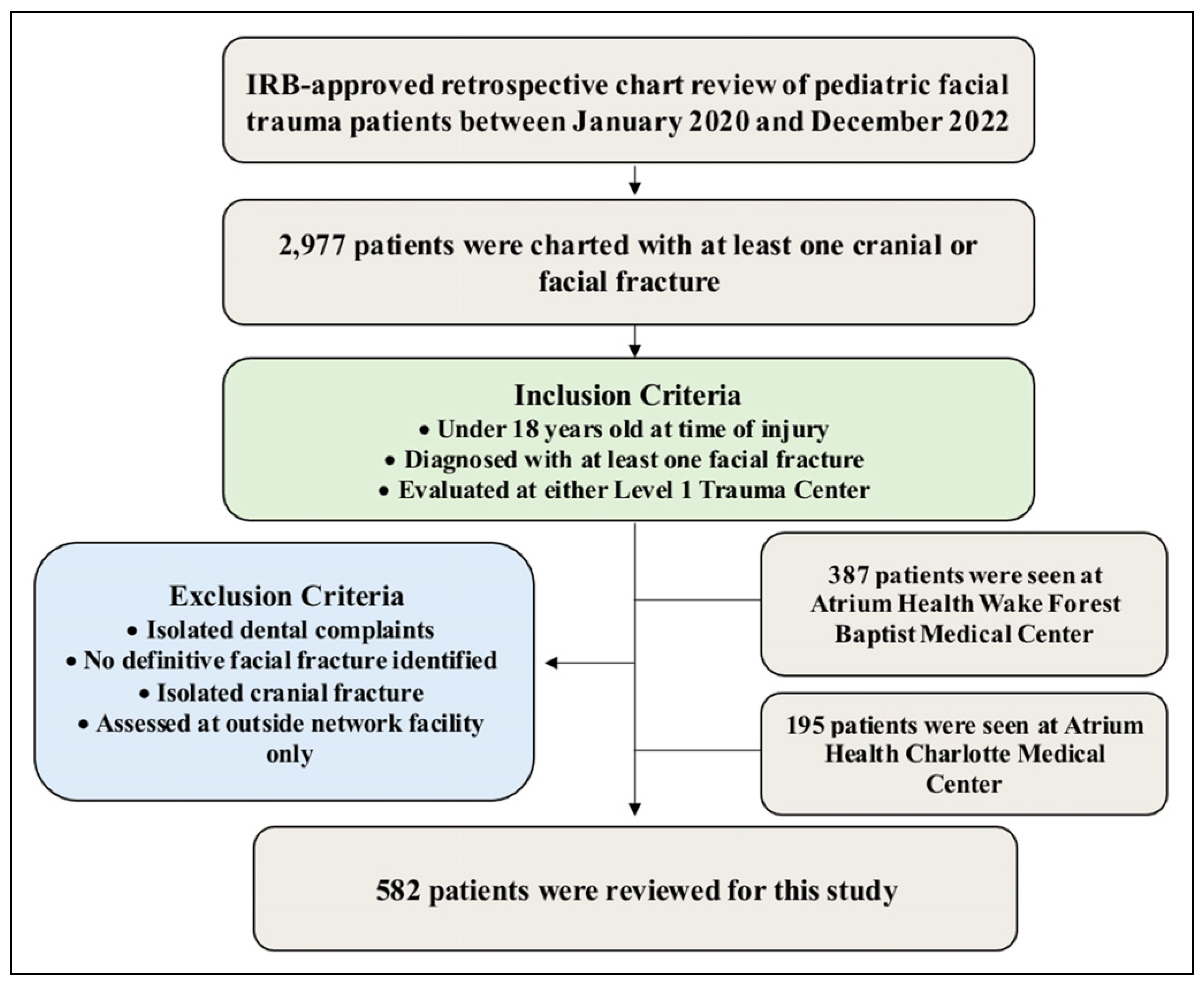
Methods and Materials
Data Acquisition
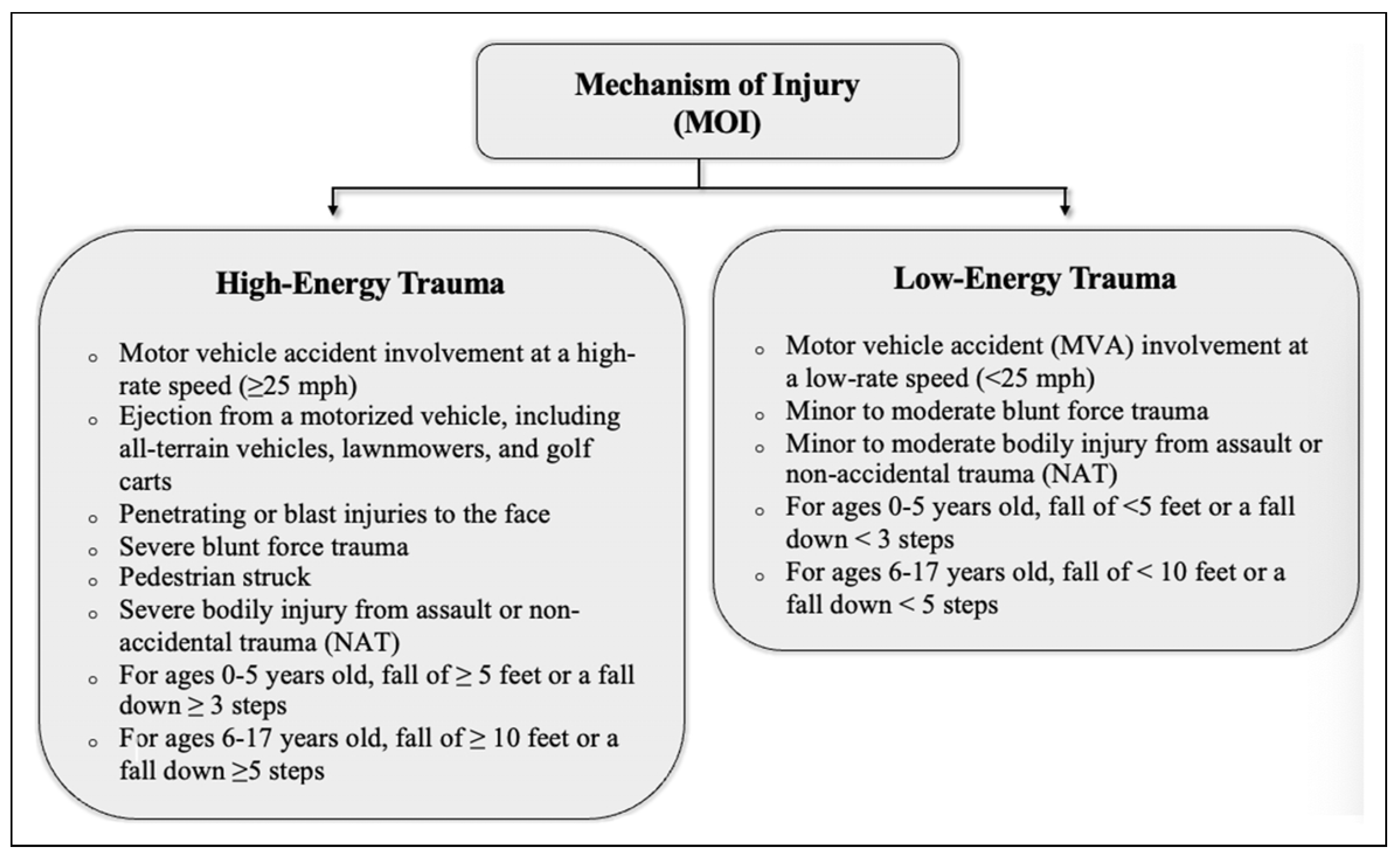
Trauma Type
Database Creation
Data Analysis
Results
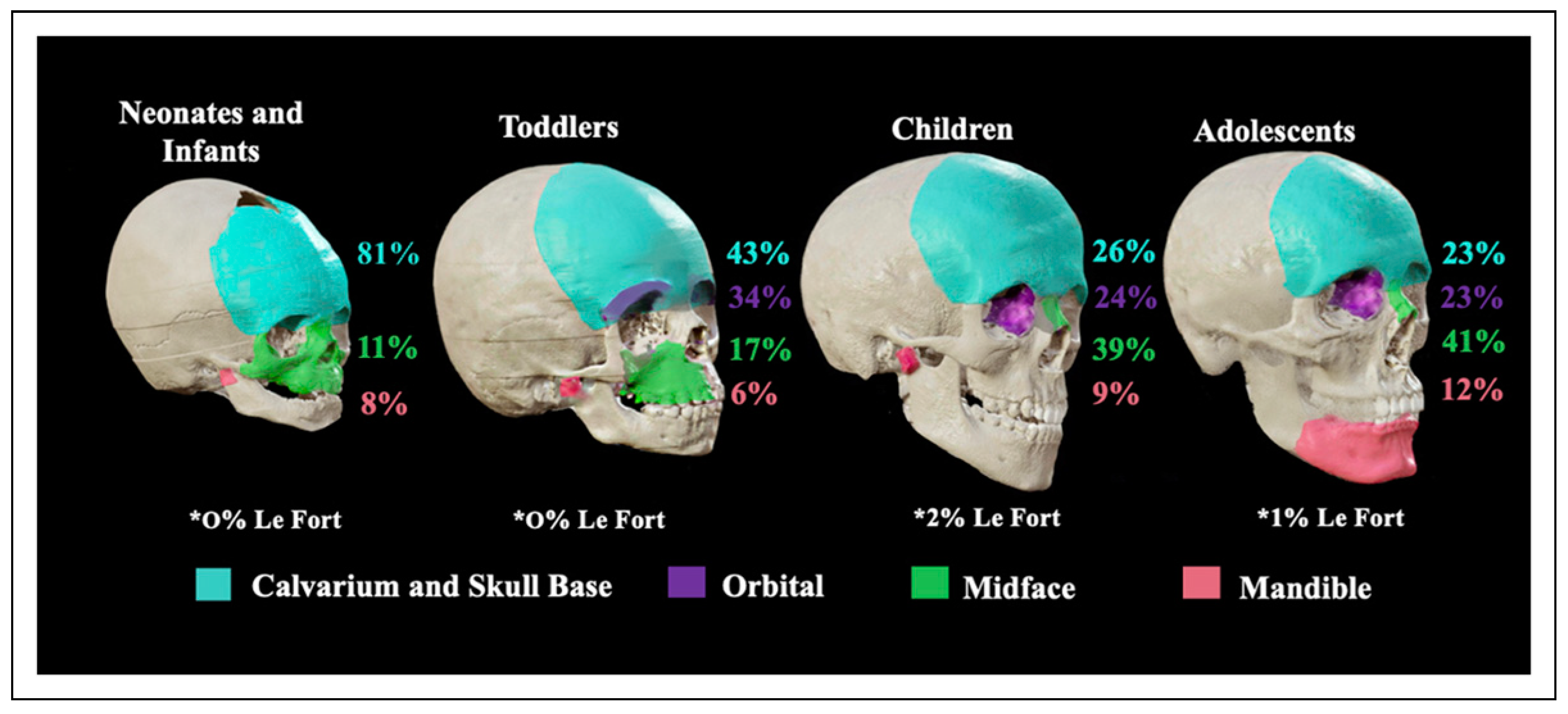
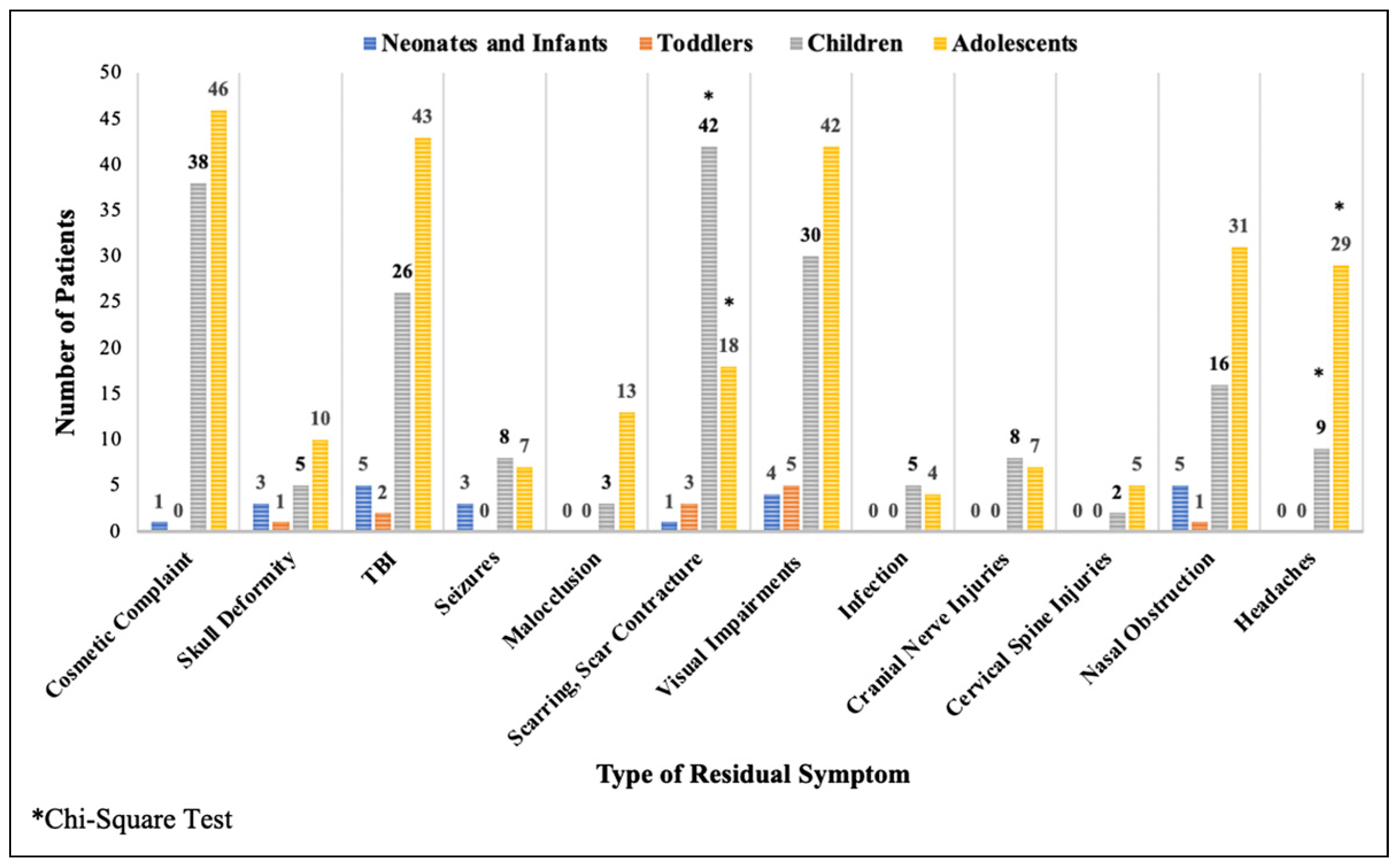
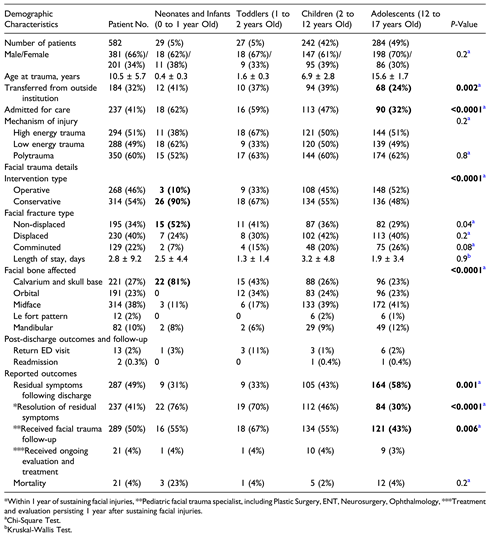
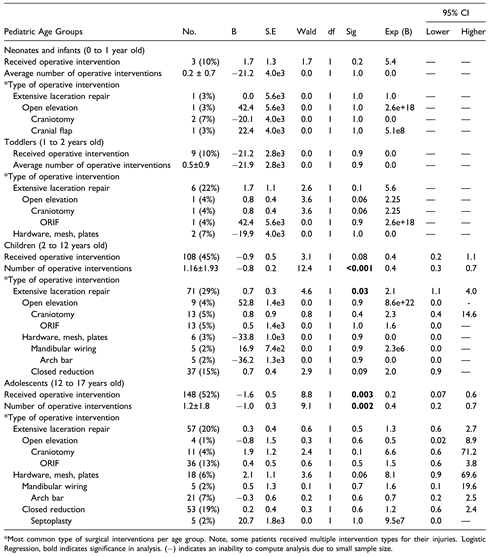
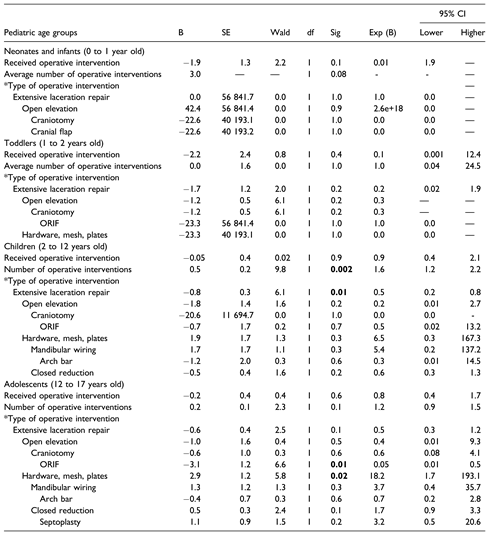
Pediatric Facial Fractures, Interventions, Management, and Outcomes by Age Group
Discussion
Analysis of Pediatric Facial Trauma
Future Directions
Limitations
Conclusion
Funding
Conflicts of Interest
Ethics Statement
- Ethics Approval
References
- Rogan, D.T.; Fang, A. Pediatric facial trauma. StatPearls. 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK558932/.
- Koch, B.L. Pediatric considerations in craniofacial trauma. Neuroimaging Clin N Am. 2014, 24, 513–529. [Google Scholar] [CrossRef] [PubMed]
- Cole, P.; Kaufman, Y.; Hollier, L.H., Jr. Managing the pediatric facial fracture. Craniomaxillofac Trauma Reconstr. 2009, 2, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Gentile, M.A.; McKinlay, A.A.; Stires, S.A. Pediatric maxillary and zygomatic fractures. In Pediatric Maxillofacial Trauma; Kushner, G.M., Jones, L.C., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2021; pp. 115–143. [Google Scholar] [CrossRef]
- Mukherjee, C.G.; Mukherjee, U. Maxillofacial trauma in children. Int J Clin Pediatr Dent. 2012, 5, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Sclafani, A.P.; Sclafani, M.S.; Long, S.; Losenegger, T.; Spielman, D.; Obayemi, A.; Cosiano, M.F.; Neuner, R.; Kacker, A.; Reeve, G.; et al. Injury Patterns in Pediatric Facial Fractures Unique to an Urban Environment. Facial Plast. Surg. 2021, 37, 564–570. [Google Scholar] [CrossRef] [PubMed]
- Giertych, B.; Morrow, V.R.; Rizwan, U.; Danby, G.C.B.; Lubicky, J.P.; Hobbs, G.; Grant, D.R. ATV-Related Trauma in the Pediatric Population. J. Pediatr. Orthop. 2023, 43, e669–e673. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, I.C.; Kordahi, A.M.; Paik, A.M.; Lee, E.S.; Granick, M.S. Pediatric facial fractures as a result of gunshot injuries: an examination of associated injuries and trends in management. J Craniofac Surg. 2014, 25, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Andrew, T.W.; Morbia, R.; Lorenz, H.P. Pediatric Facial Trauma. Clin. Plast. Surg. 2019, 46, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.C.; Le, T.M.T.; Oleck, N.C.; et al. Pediatric pedestrian facial fracture patterns and management following motor vehicle collisions. J Craniofac Surg. 2020, 31, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, I.C.; Kordahi, A.M.; Paik, A.M.; Lee, E.S.; Granick, M.S. Examination of Life-Threatening Injuries in 431 Pediatric Facial Fractures at a Level 1 Trauma Center. J. Craniofacial Surg. 2014, 25, 1825–1828. [Google Scholar] [CrossRef]
- Palmer, C. Major trauma and the injury severity score--where should we set the bar? Annu Proc Assoc Adv Automot Med 2007, 51, 13–29. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217501/. [PubMed]
- Wendling-Keim, D.S.; Hefele, A.; Muensterer, O.; Lehner, M. Trauma Scores and Their Prognostic Value for the Outcome Following Pediatric Polytrauma. Front. Pediatr. 2021, 9, 721585. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; et al. The REDCap consortium: building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Althammer, A.; Prückner, S.; Gehring, G.C.; Lieftüchter, V.; Trentzsch, H.; Hoffmann, F. Systemic review of age brackets in pediatric emergency medicine literature and the development of a universal age classification for pediatric emergency patients - the Munich Age Classification System (MACS). BMC Emerg. Med. 2023, 23, 77. [Google Scholar] [CrossRef]
- Juncar, R.I.; Moca, A.E.; Juncar, M.; Moca, R.T.; Țenț, P.A. Clinical Patterns and Treatment of Pediatric Facial Fractures: A 10-Year Retrospective Romanian Study. Children 2023, 10, 800. [Google Scholar] [CrossRef] [PubMed]
- Haruna, S.; Sawada, K.; Nakajima, T.; Moriyama, H. Relationship between pediatric sinusitis and middle turbinate pneumatization—ethmoidal sinus pyocele thought to be caused by middle turbinate pneumatization. Int. J. Pediatr. Otorhinolaryngol. 2005, 69, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Alvi, S.P.; Nasal, B.C. Fracture Reduction. National Library of Medicine. 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK538299/.
 |
 |
 |
 |
© 2024 by the authors. The Author(s) 2024.
Share and Cite
Hinson, M.; Wright, A.; Davidson, A.; Kogan, S.; Runyan, C. Pediatric Facial Fractures: A Multi-Institutional Level 1 Trauma Center Analysis of Incidence, Interventions, and Outcomes. Craniomaxillofac. Trauma Reconstr. 2024, 17, 45. https://doi.org/10.1177/19433875241272430
Hinson M, Wright A, Davidson A, Kogan S, Runyan C. Pediatric Facial Fractures: A Multi-Institutional Level 1 Trauma Center Analysis of Incidence, Interventions, and Outcomes. Craniomaxillofacial Trauma & Reconstruction. 2024; 17(4):45. https://doi.org/10.1177/19433875241272430
Chicago/Turabian StyleHinson, Madison, Avery Wright, Amelia Davidson, Samuel Kogan, and Christopher Runyan. 2024. "Pediatric Facial Fractures: A Multi-Institutional Level 1 Trauma Center Analysis of Incidence, Interventions, and Outcomes" Craniomaxillofacial Trauma & Reconstruction 17, no. 4: 45. https://doi.org/10.1177/19433875241272430
APA StyleHinson, M., Wright, A., Davidson, A., Kogan, S., & Runyan, C. (2024). Pediatric Facial Fractures: A Multi-Institutional Level 1 Trauma Center Analysis of Incidence, Interventions, and Outcomes. Craniomaxillofacial Trauma & Reconstruction, 17(4), 45. https://doi.org/10.1177/19433875241272430




