Differences Between Patient and Surgeon Perspectives: A Long-Term Follow-Up of 180 Patients with Zygomaticomaxillary Complex Fractures Following Either Conservative or Surgical Treatment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Inclusion, and Exclusion
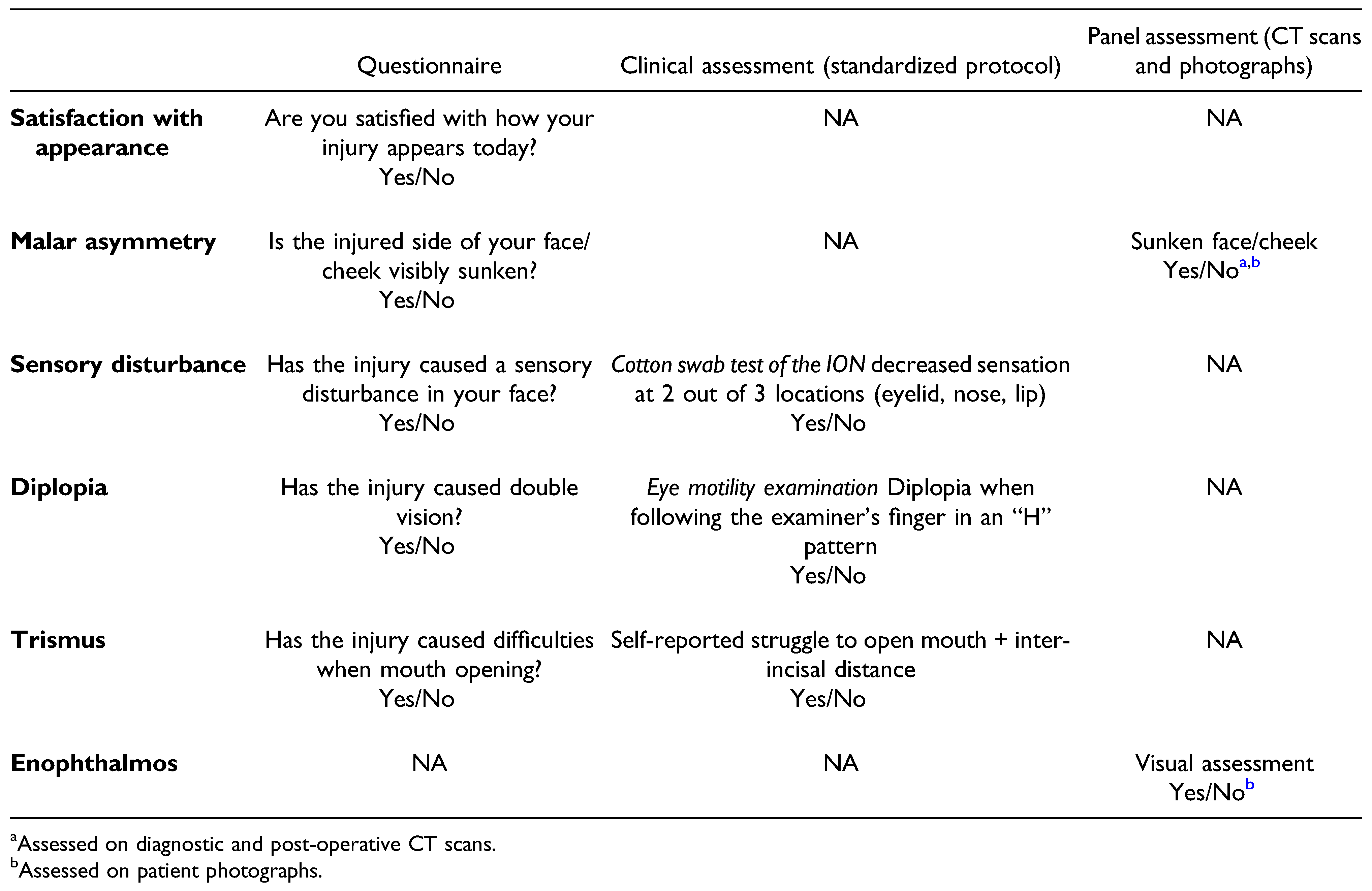
2.2. Follow-Up Clinical Examinations and Collection of Data
2.3. Review Panel Assessment
2.4. Statistical Analysis
3. Results
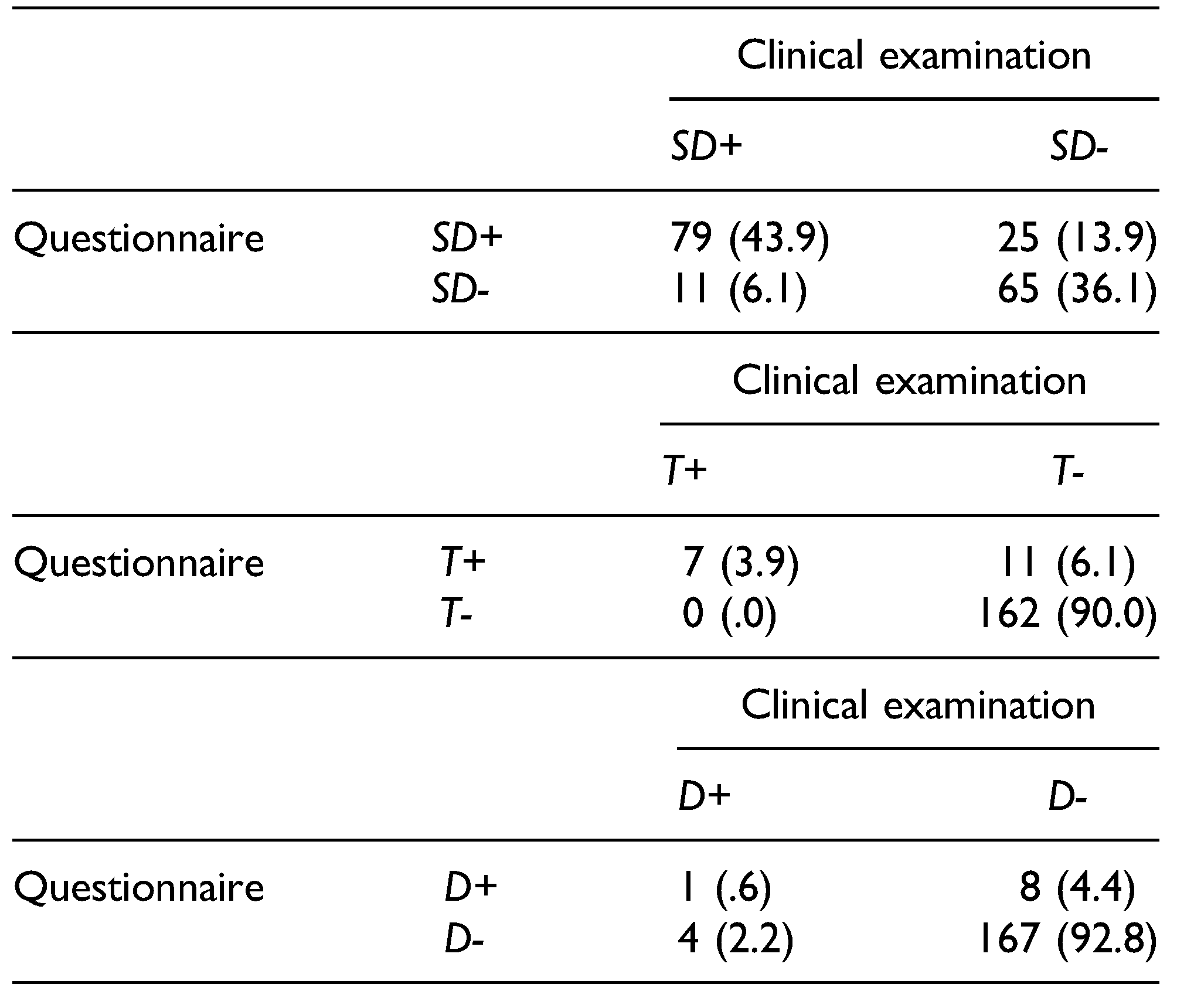
3.1. Sensory Disturbance, Trismus, and Diplopia
3.2. Malar Asymmetry
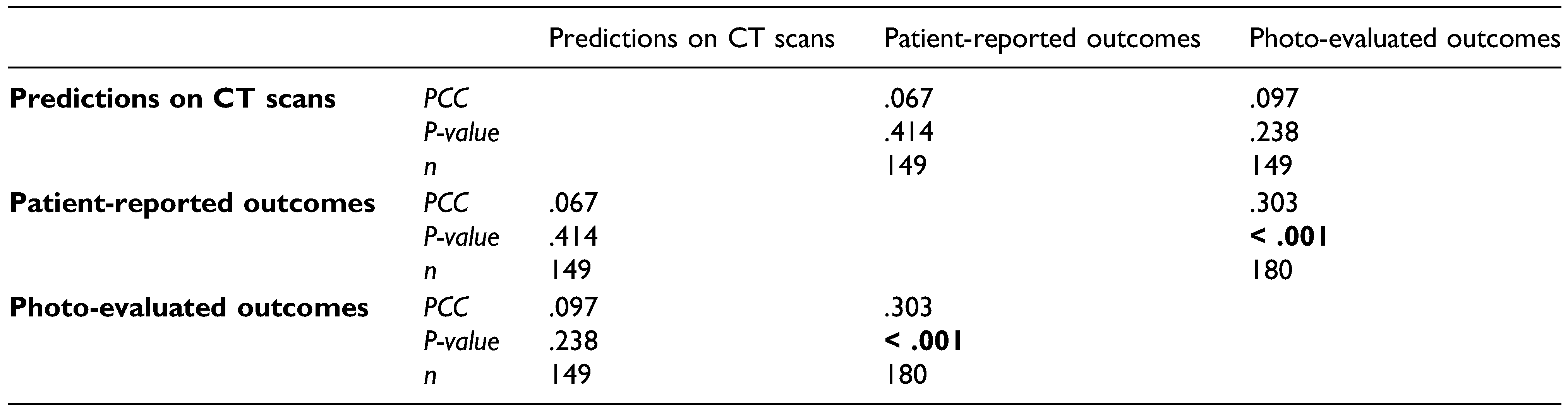
3.3. Patient Satisfaction
4. Discussion
4.1. Sequelae and Long-Term Patient Satisfaction
4.2. Patient Characteristics
4.3. Patient and Surgeon Perspectives
4.4. Strengths and Limitations
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Boffano, P.; Roccia, F.; Zavattero, E.; et al. European Maxillofacial Trauma (EURMAT) project: A multicentre and prospective study. J Cranio-Maxillo-Fac Surg. 2015, 43, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Brucoli, M.; Boffano, P.; Broccardo, E.; et al. The “European zygomatic fracture” research project: The epidemiological results from a multicenter European collaboration. J CranioMaxillo-Fac Surg. 2019, 47, 616–621. [Google Scholar] [CrossRef]
- Ellis, E.; Kittidumkerng, W. Analysis of treatment for isolated zygomaticomaxillary complex fractures. J Oral Maxillofac Surg. 1996, 54, 386–400. [Google Scholar] [CrossRef]
- Zingg, M.; Laedrach, K.; Chen, J.; et al. Classification and treatment of zygomatic fractures: A review of 1,025 cases. J Oral Maxillofac Surg. 1992, 50, 778–790. [Google Scholar] [CrossRef]
- Strong, E.B.; Gary, C. Management of zygomaticomaxillary complex fractures. Facial Plast Surg Clin North Am. 2017, 25, 547–562. [Google Scholar] [CrossRef] [PubMed]
- Birgfeld, C.B.; Mundinger, G.S.; Gruss, J.S. Evidence-based medicine: Evaluation and treatment of zygoma fractures. Plast Reconstr Surg. 2017, 139, 168e–180e. [Google Scholar] [CrossRef]
- Salma, R.G.; Almutairi, K.M.; Alalmai, M.I. The clinical course of diplopia associated with zygomaticomaxillary complex fractures before and after surgery. J. Oral Maxillofac. Surg. Med. Pathol. 2018, 30, 191–196. [Google Scholar] [CrossRef]
- Ling, X.F.; Yew, C.C.; Mohd Nazri, S.B.; Tew, M.M. Unilateral zygomatic complex fracture a comparison between nonsurgical treatment and surgical treatment. J Craniofac Surg. 2021, 32, e627–e630. [Google Scholar] [CrossRef]
- Ellis, E.; Perez, D. An algorithm for the treatment of isolated zygomatico-orbital fractures. J Oral Maxillofac Surg. 2014, 72, 1975–1983. [Google Scholar] [CrossRef]
- Back, C.P.; McLean, N.R.; Anderson, P.J.; David, D.J. The conservative management of facial fractures: Indications and outcomes. J Plast Reconstr Aesthetic Surg. 2007, 60, 146–151. [Google Scholar]
- Salentijn, E.G.; Boverhoff, J.; Heymans, M.W.; van den Bergh, B.; Forouzanfar, T. The clinical and radiographical characteristics of zygomatic complex fractures: A comparison between the surgically and non-surgically treated patients. J CranioMaxillo-Fac Surg. 2014, 42, 492–497. [Google Scholar]
- van Hout, W.M.; Van Cann, E.M.; Koole, R.; Rosenberg, A.J. Surgical treatment of unilateral zygomaticomaxillary complex fractures: A 7-year observational study assessing treatment outcome in 153 cases. J Cranio-Maxillo-Fac Surg. 2016, 44, 1859–1865. [Google Scholar]
- Basaran, K.; Saydam, F.A.; Pilancı, O.; Sagır, M.; Güven, E. Optimal treatment of zygomatic fractures: A single-center study results. Kulak Burun Bogaz Ihtis Derg. 2016, 26, 42–50. [Google Scholar]
- Rahman, R.A.; Ghazali, N.M.; Rahman, N.A.; Pohchi, A.; Razak, N.H.A. Outcome of different treatment modalities of fracture zygoma. J Craniofac Surg. 2020, 31, 1056–1062. [Google Scholar]
- Starch-Jensen, T.; Linnebjerg, L.B.; Jensen, J.D. Treatment of zygomatic complex fractures with surgical or nonsurgical intervention: A retrospective study. Open Dent J. 2018, 12, 377–387. [Google Scholar] [PubMed]
- Benoliel, R.; Birenboim, R.; Regev, E.; Eliav, E. Neurosensory changes in the infraorbital nerve following zygomatic fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005, 99, 657–665. [Google Scholar]
- Raghoebar, I.I.; Rozema, F.R.; de Lange, J.; Dubois, L. Surgical treatment of fractures of the zygomaticomaxillary complex: effect of fixation on repositioning and stability. A systematic review. Br J Oral Maxillofac Surg. 2022, 60, 397–411. [Google Scholar]
- Ribeiro, M.C.; Regalo, S.C.; Pepato, A.O.; et al. Bite force, electromyography, and mandible mobility during the 6-month period after surgical treatment for isolated fractures of the zygomatico-orbital complex. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011, 111, e1–e7. [Google Scholar]
- Kaukola, L.; Snall, J.; Roine, R.; Sintonen, H.; Thoren, H. Health-related quality of life of patients with zygomatic fracture. Med Oral Patol Oral Cir Bucal. 2017, 22, e636–e642. [Google Scholar]
- Lupi-Ferandin, S.; Glumac, S.; Poljak, N.; et al. Health-related quality of life in patients after surgically treated midface fracture: A comparison with the Croatian population norm. Therapeut Clin Risk Manag. 2020, 16, 261–267. [Google Scholar]
- Mishra, P.; Khan, P.; Salunkhe, S.M.; et al. Factors affecting quality of life in zygomatic fractures: An original research. J Pharm BioAllied Sci. 2022, 14 (Suppl. S1), S242–s244. [Google Scholar] [PubMed]
- Kurita, M.; Okazaki, M.; Ozaki, M.; et al. Patient satisfaction after open reduction and internal fixation of zygomatic bone fractures. J Craniofac Surg. 2010, 21, 45–49. [Google Scholar] [PubMed]
- Folkestad, L.; Aberg-Bengtsson, L.; Granstrom, G. Recovery from orbital floor fractures: A prospective study of patients’ and doctors’ experiences. Int J Oral Maxillofac Surg. 2006, 35, 499–505. [Google Scholar] [PubMed]
- af Geijerstam, B.; Hultman, G.; Bergstrom, J.; Stjarne, P. Zygomatic fractures managed by closed reduction: An analysis with postoperative computed tomography follow-up evaluating the degree of reduction and remaining dislocation. J Oral Maxillofac Surg. 2008, 66, 2302–2307. [Google Scholar]
- Salentijn, E.G.; Boffano, P.; Boverhoff, J.; van den Bergh, B.; Forouzanfar, T. The epidemiological characteristics of zygomatic complex fractures: A comparison between the surgically and non-surgically treated patients. Natl J Maxillofac Surg. 2013, 4, 214–218. [Google Scholar]
- Olate, S.; Lima, S.M.; Sawazaki, R.; Moreira, R.W.; de Moraes, M. Variables related to surgical and nonsurgical treatment of zygomatic complex fracture. J Craniofac Surg. 2011, 22, 1200–1202. [Google Scholar]
- Lehtinen, V.; Pyotsia, K.; Snall, J.; Toivari, M. Zygomatico-orbital fracture-dislocation in surgical treatment: Novel 3dimensional software automated analysis. J Oral Maxillofac Surg. 2020, 78, 1372–1381. [Google Scholar]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. The Author(s) 2008.
Share and Cite
Rahbin, S.; Sunnergren, O.; McBride, E.; Darabi, H.; Alinasab, B. Differences Between Patient and Surgeon Perspectives: A Long-Term Follow-Up of 180 Patients with Zygomaticomaxillary Complex Fractures Following Either Conservative or Surgical Treatment. Craniomaxillofac. Trauma Reconstr. 2024, 17, 39. https://doi.org/10.1177/19433875231208463
Rahbin S, Sunnergren O, McBride E, Darabi H, Alinasab B. Differences Between Patient and Surgeon Perspectives: A Long-Term Follow-Up of 180 Patients with Zygomaticomaxillary Complex Fractures Following Either Conservative or Surgical Treatment. Craniomaxillofacial Trauma & Reconstruction. 2024; 17(4):39. https://doi.org/10.1177/19433875231208463
Chicago/Turabian StyleRahbin, Samin, Ola Sunnergren, Ellen McBride, Hatef Darabi, and Babak Alinasab. 2024. "Differences Between Patient and Surgeon Perspectives: A Long-Term Follow-Up of 180 Patients with Zygomaticomaxillary Complex Fractures Following Either Conservative or Surgical Treatment" Craniomaxillofacial Trauma & Reconstruction 17, no. 4: 39. https://doi.org/10.1177/19433875231208463
APA StyleRahbin, S., Sunnergren, O., McBride, E., Darabi, H., & Alinasab, B. (2024). Differences Between Patient and Surgeon Perspectives: A Long-Term Follow-Up of 180 Patients with Zygomaticomaxillary Complex Fractures Following Either Conservative or Surgical Treatment. Craniomaxillofacial Trauma & Reconstruction, 17(4), 39. https://doi.org/10.1177/19433875231208463




