Tomographic Evaluation of Bone Height Between the Mandibular Canal and the Inferior Cortex of the Mandible Related to Bicortical Screws Fixation
Abstract
:Introduction
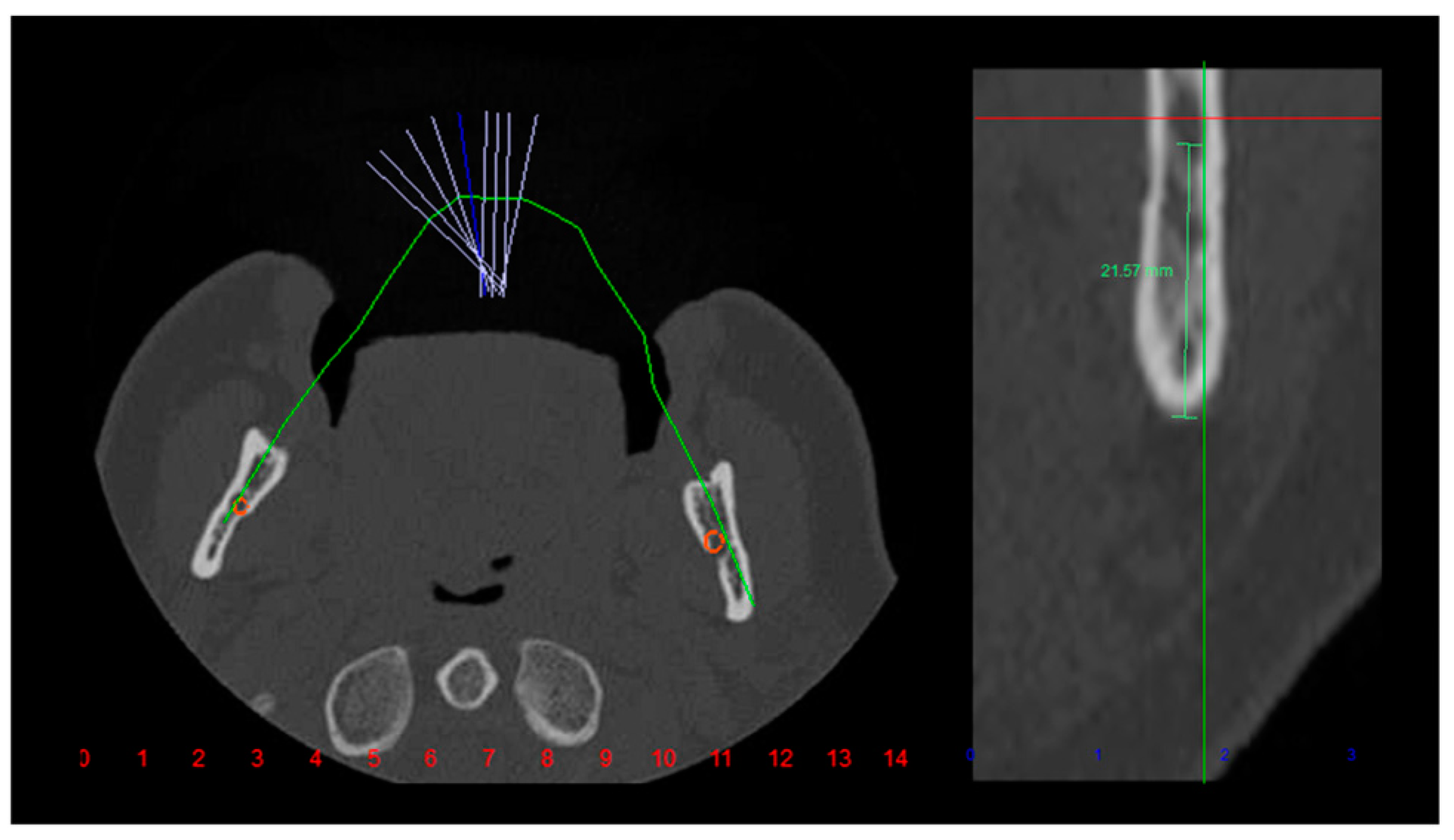
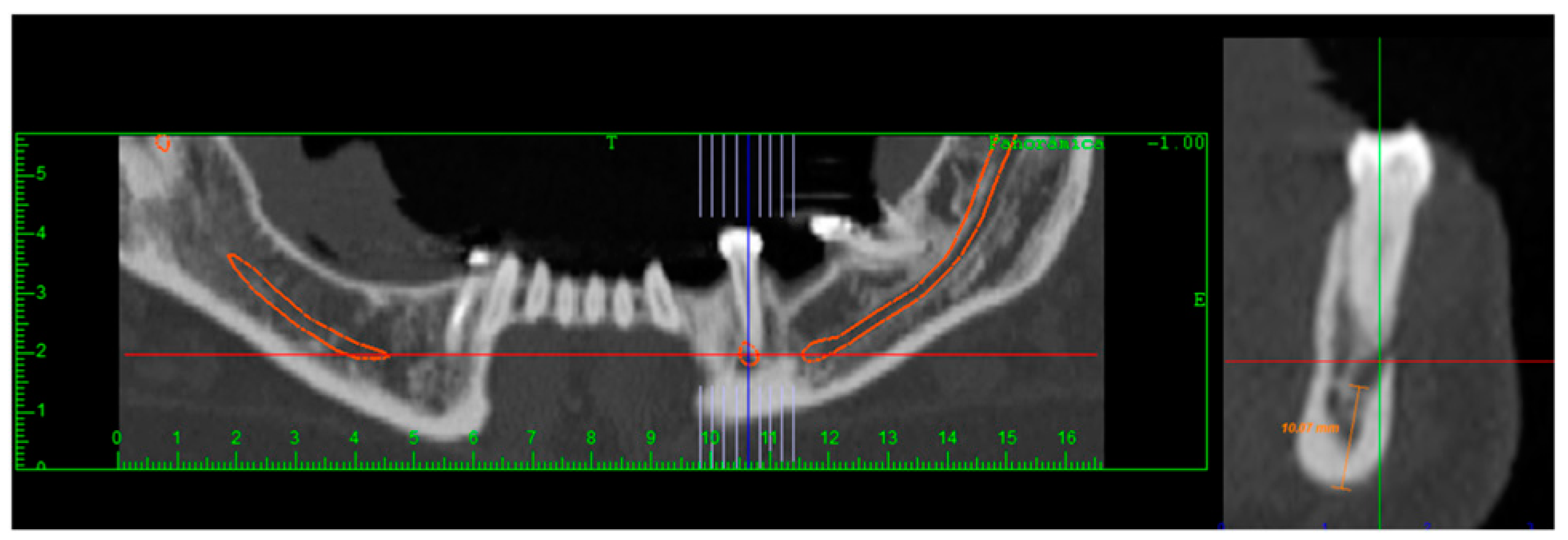
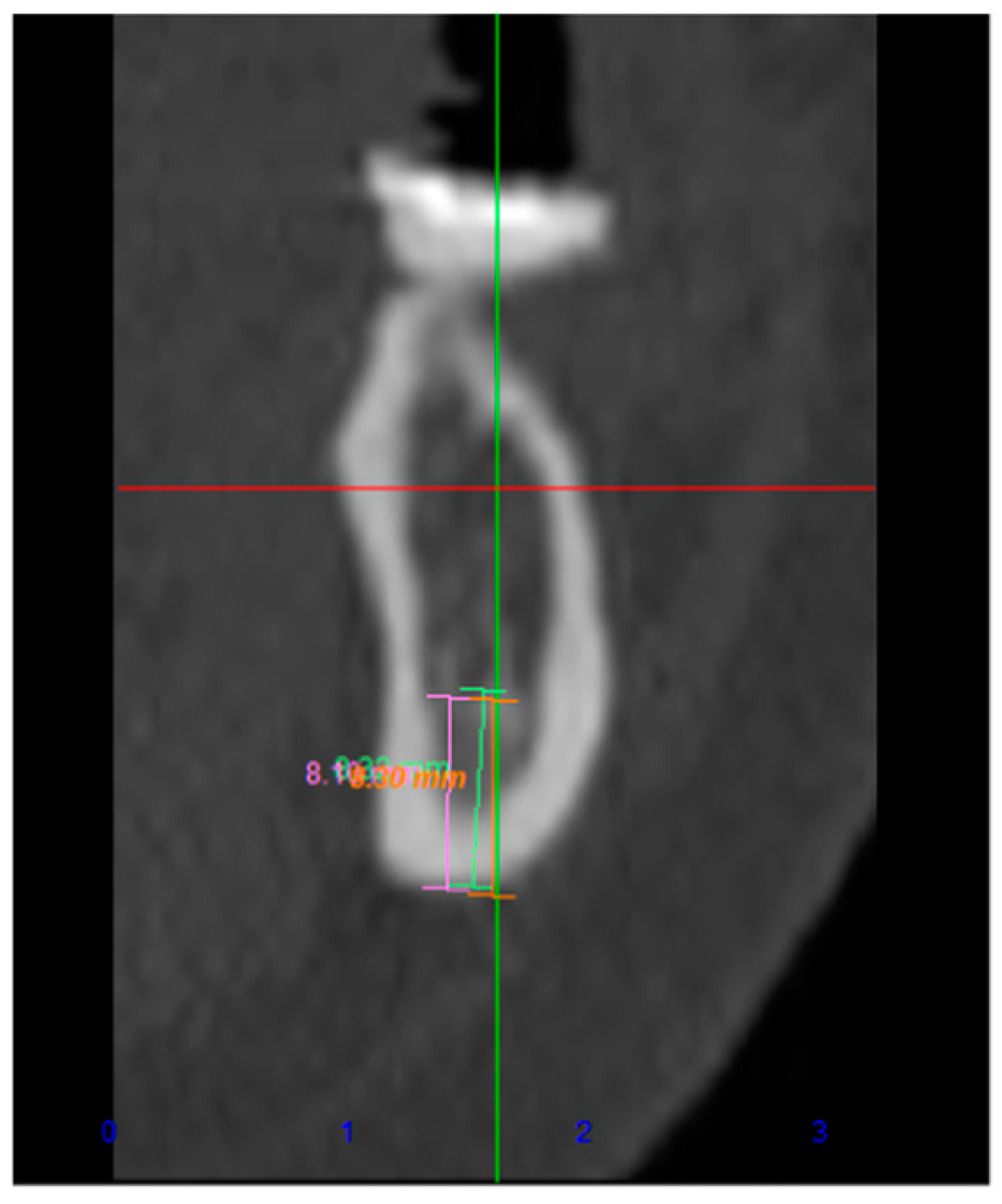
Materials and Methods
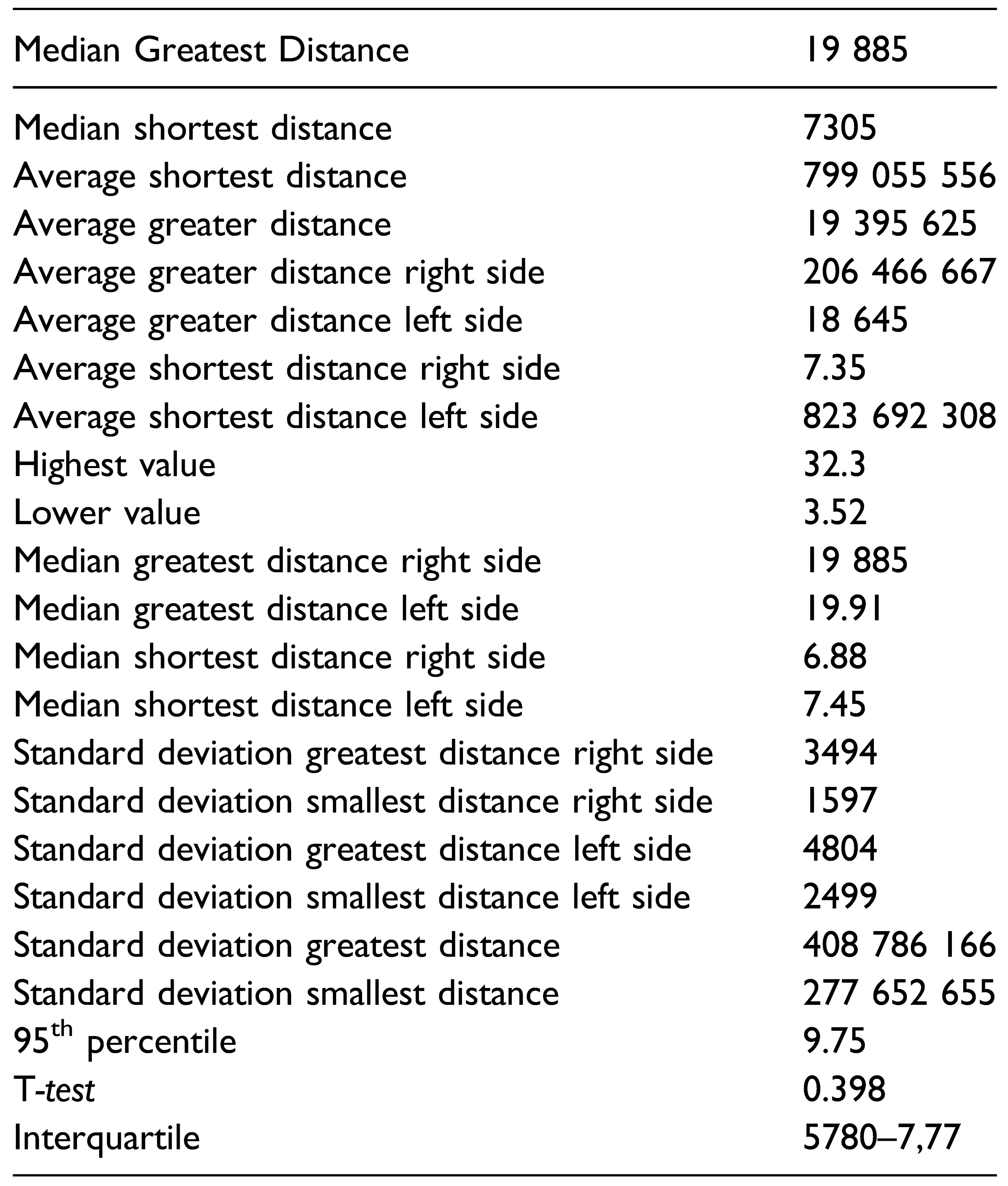
Results
Discussion
Conclusions
Funding
Declaration of Conflicting Interests
References
- Ellis, E., 3rd; Dean, J. Rigid fixation of mandibular condyle fractures. Oral Surg Oral Med Oral Pathol. 1993, 76(1), 6–15. [Google Scholar] [CrossRef]
- Cutright, B.; Quillopa, N.; Schubert, W. An anthropometric analysis of the key foramina for maxillofacial surgery. J Oral Maxillofac Surg. 2003, 61(3), 354–357. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.H.; Goddard, A.L.; Dodson, T.B. Inferior alveolar nerve canal position: a clinical and radiographic study. J Oral Maxillofac Surg. 2007, 65(3), 470–474. [Google Scholar] [CrossRef]
- Liu, T.; Xia, B.; Gu, Z. Inferior alveolar canal course: a radiographic study. Clin Oral Implants Res. 2009, 20(11), 1212–1218. [Google Scholar] [CrossRef]
- Kocaelli, H.A.; Arikan, H.; Kaptan, F.; Kayahan, B.; Haznedaroğlu, F. Management of the perforations due to miniplate application. J Endod. 2006, 32(5), 482–485. [Google Scholar] [CrossRef] [PubMed]
- Hillerup, S. Iatrogenic injury to the inferior alveolar nerve: etiology, signs and symptoms, and observations on recovery. Int J Oral Maxillofac Surg. 2008, 37(8), 704–709. [Google Scholar] [CrossRef] [PubMed]
- Seemann, R.; Schicho, K.; Wutzl, A.; et al. Complication rates in the operative treatment of mandibular angle fractures: a 10-year retrospective. J Oral Maxillofac Surg 2010, 68(3), 647–650. [Google Scholar] [CrossRef]
- Bede, S. Mandibular fractures in Iraq: an epidemiological study. Craniomaxillofac Trauma Reconstr. 2015, 8(01), 59–63. [Google Scholar] [CrossRef]
- Lo, L.J.; Wong, F.H.; Chen, Y.R. The position of the inferior alveolar nerve at the mandibular angle:: an anatomic consideration for aesthetic mandibular angle reduction. Ann Plast Surg. 2004, 53(1), 50–55. [Google Scholar] [CrossRef]
- Hernandez, L.C.; Montoto, G.; Puente Rodriguez, M.; Galban, L.; Martinez, V. Bone map’ for a safe placement of miniscrews generated by computed tomography. Clin Oral Implants Res. 2008, 19(6), 576–581. [Google Scholar] [CrossRef]
- Simonton, J.D.; Azevedo, B.; Schindler, W.G.; Hargreaves, K.M. Ageand gender-related differences in the position of the inferior alveolar nerve by using cone beam computed tomography. J Endod. 2009, 35(7), 944–949. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, J.; Marin, C.; Homsi, N.; et al. Tomographic evaluation of mandibular thickness on premolar and molar regions related to monocortical screws. Craniomaxillofac Trauma Reconstr. 2016, 9(02), 105–108. [Google Scholar] [CrossRef] [PubMed]
 |
© 2023 by the author. The Author(s) 2023.
Share and Cite
Fares, R.D.; Leal, J.V.B.; da Silva Areas, M.Z.; da Rocha, H.V.; de Moraes, S.L.C.; Homsi, N.; da Silva, J.R. Tomographic Evaluation of Bone Height Between the Mandibular Canal and the Inferior Cortex of the Mandible Related to Bicortical Screws Fixation. Craniomaxillofac. Trauma Reconstr. 2024, 17, 181-185. https://doi.org/10.1177/19433875231213892
Fares RD, Leal JVB, da Silva Areas MZ, da Rocha HV, de Moraes SLC, Homsi N, da Silva JR. Tomographic Evaluation of Bone Height Between the Mandibular Canal and the Inferior Cortex of the Mandible Related to Bicortical Screws Fixation. Craniomaxillofacial Trauma & Reconstruction. 2024; 17(3):181-185. https://doi.org/10.1177/19433875231213892
Chicago/Turabian StyleFares, Raissa Dias, João Victor Borges Leal, Manuella Zanela da Silva Areas, Hernando Valentim da Rocha, Sylvio Luiz Costa de Moraes, Nicolas Homsi, and Jonathan Ribeiro da Silva. 2024. "Tomographic Evaluation of Bone Height Between the Mandibular Canal and the Inferior Cortex of the Mandible Related to Bicortical Screws Fixation" Craniomaxillofacial Trauma & Reconstruction 17, no. 3: 181-185. https://doi.org/10.1177/19433875231213892
APA StyleFares, R. D., Leal, J. V. B., da Silva Areas, M. Z., da Rocha, H. V., de Moraes, S. L. C., Homsi, N., & da Silva, J. R. (2024). Tomographic Evaluation of Bone Height Between the Mandibular Canal and the Inferior Cortex of the Mandible Related to Bicortical Screws Fixation. Craniomaxillofacial Trauma & Reconstruction, 17(3), 181-185. https://doi.org/10.1177/19433875231213892




