Anatomical Landmarks and Branching Patterns of the Greater Auricular Nerve
Abstract
:Introduction
Methodology
Results
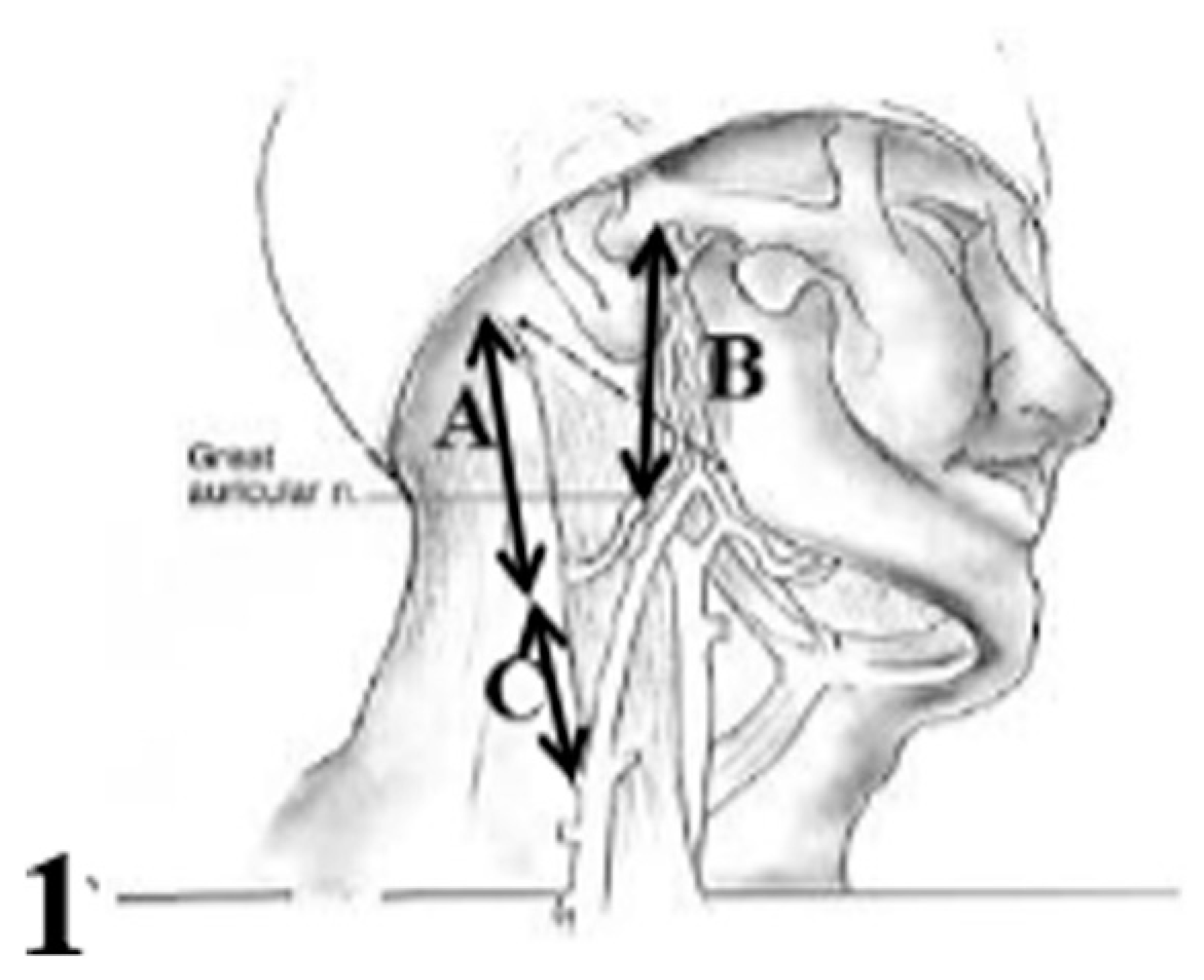
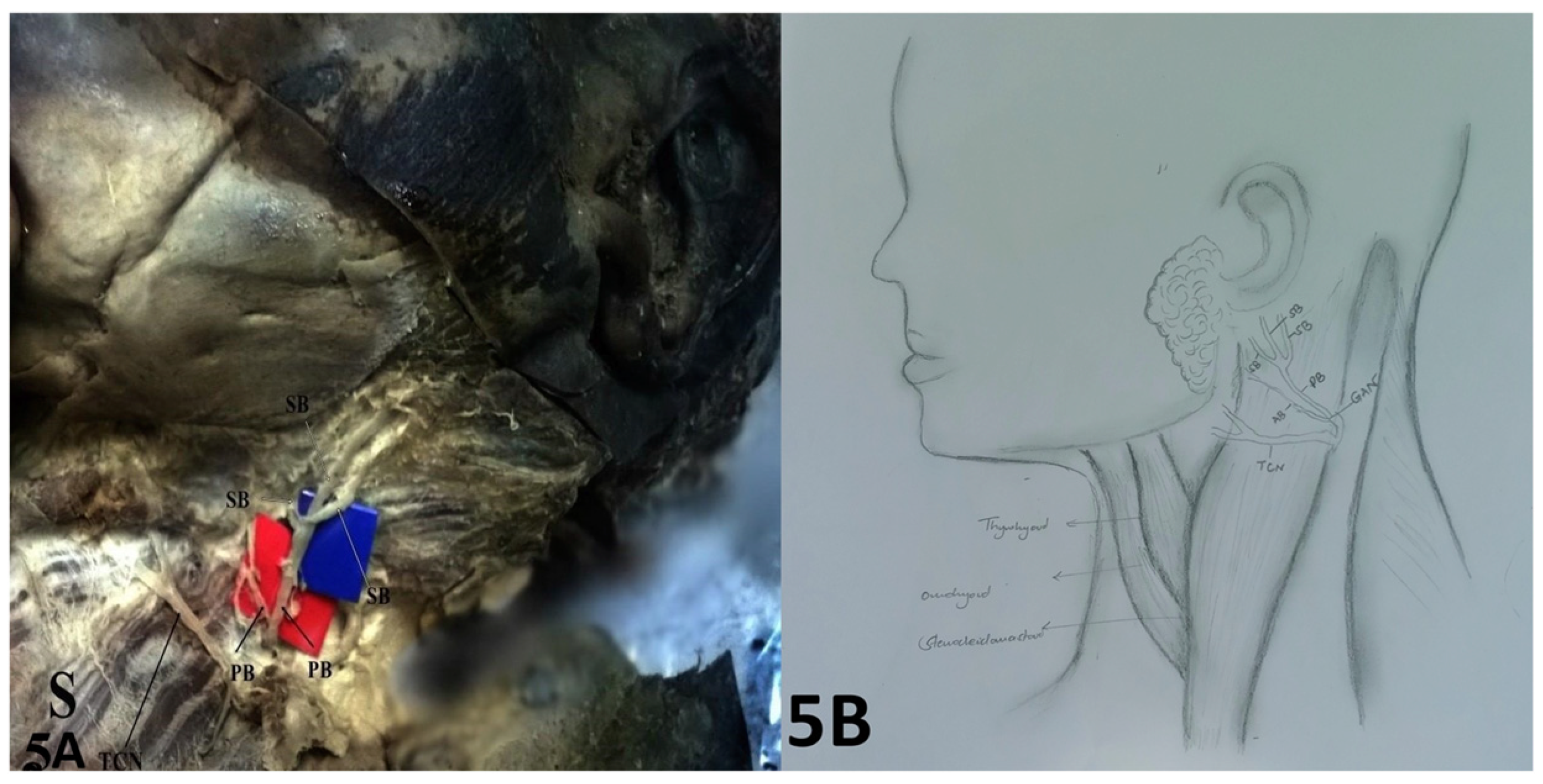
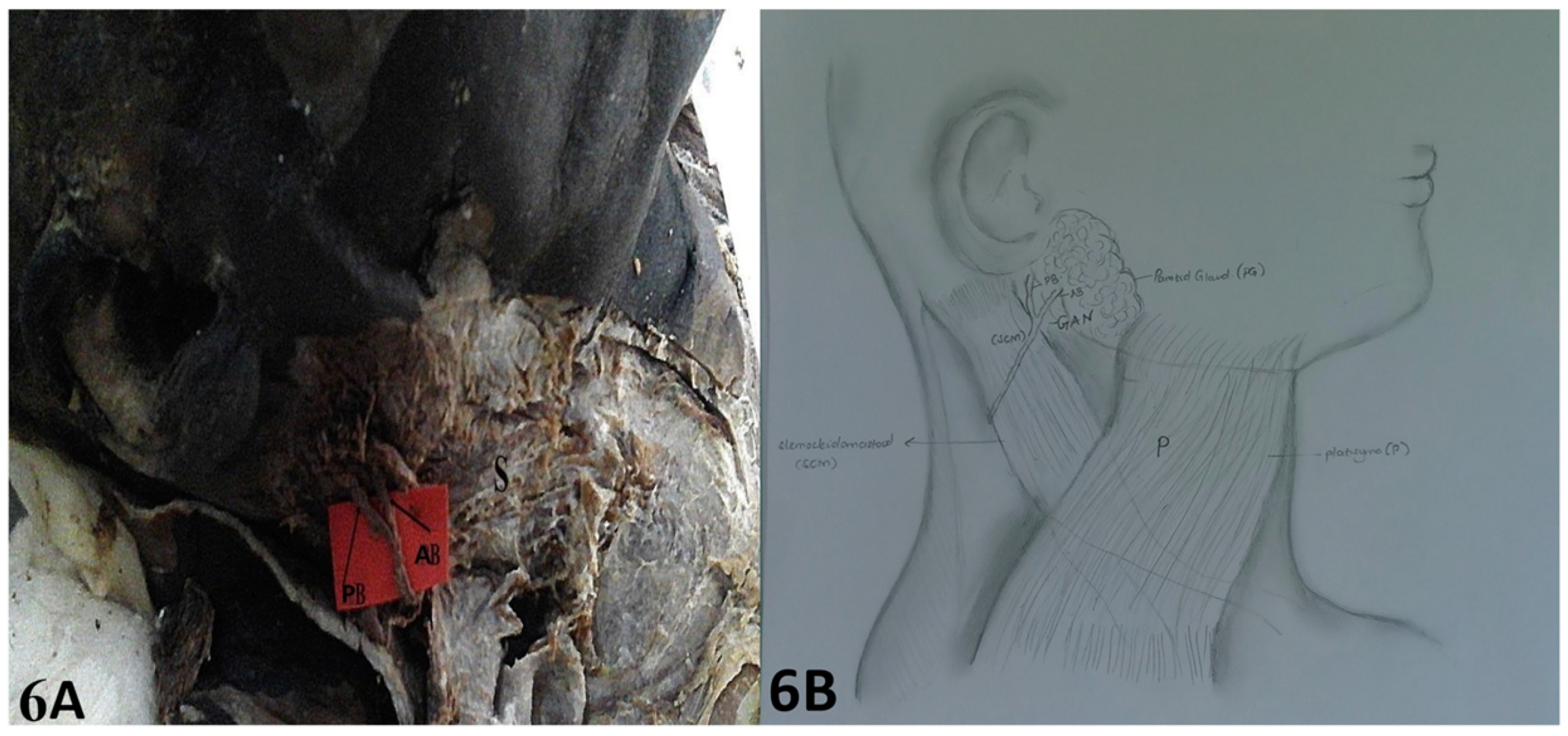
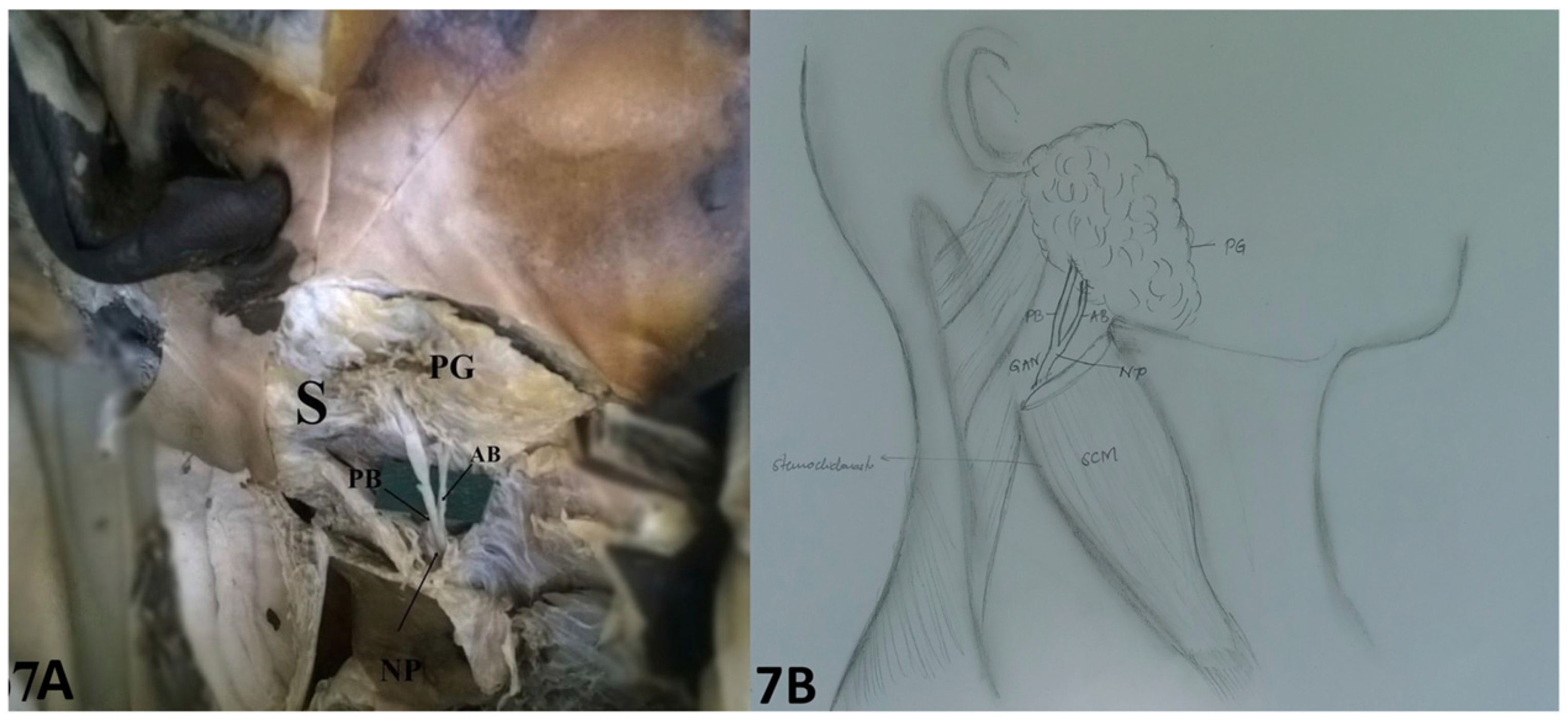
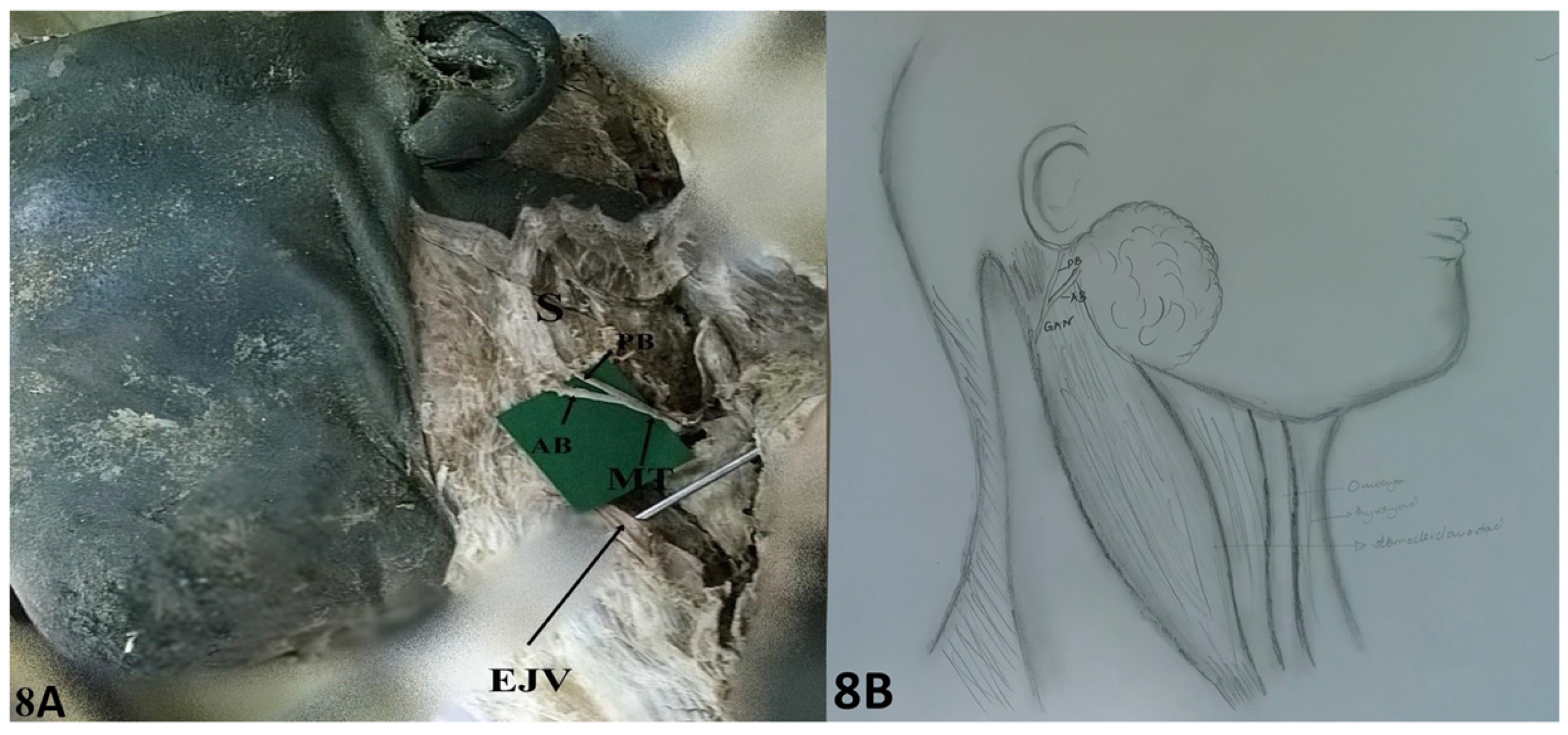
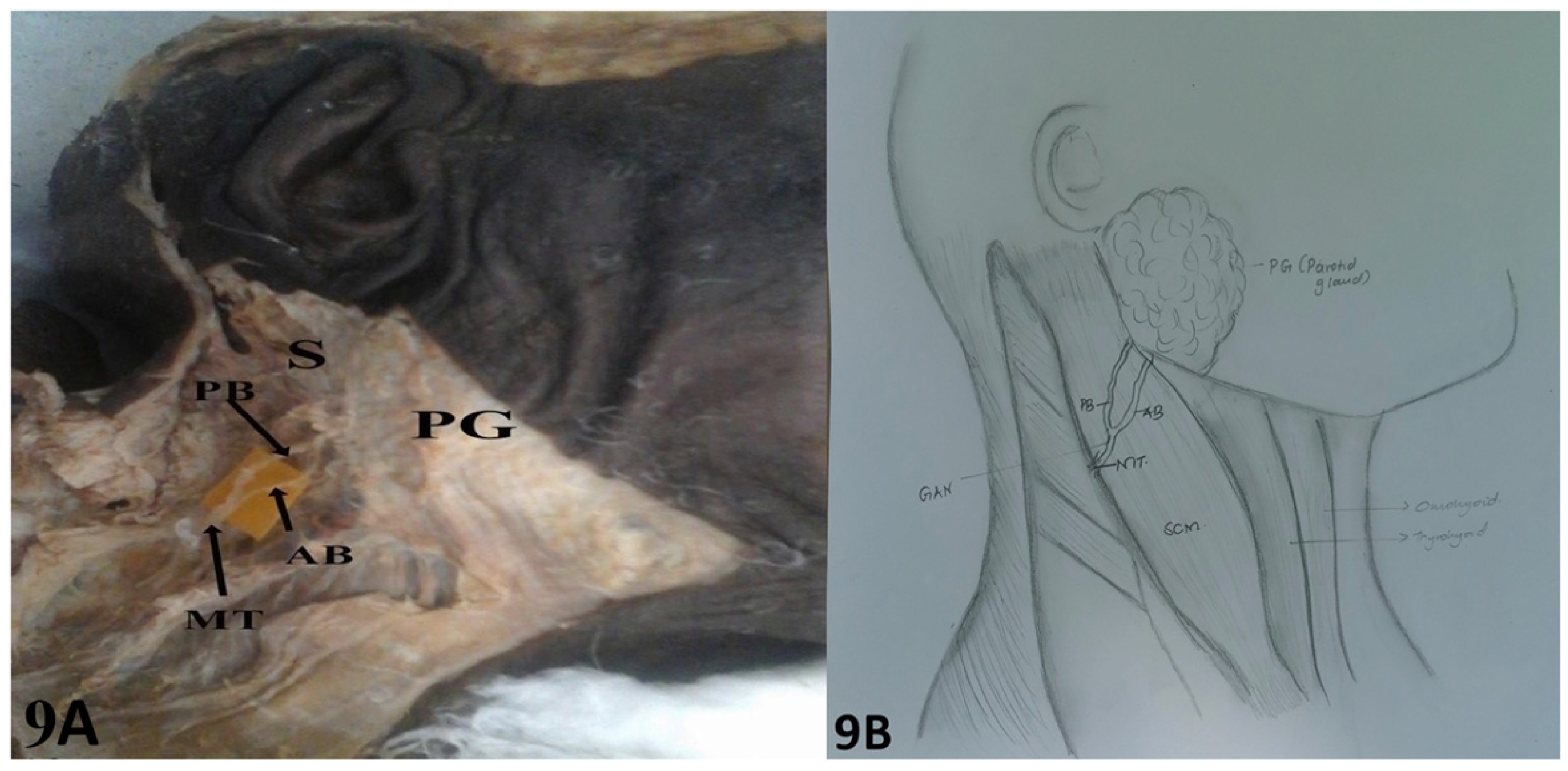
Anatomical Landmarks
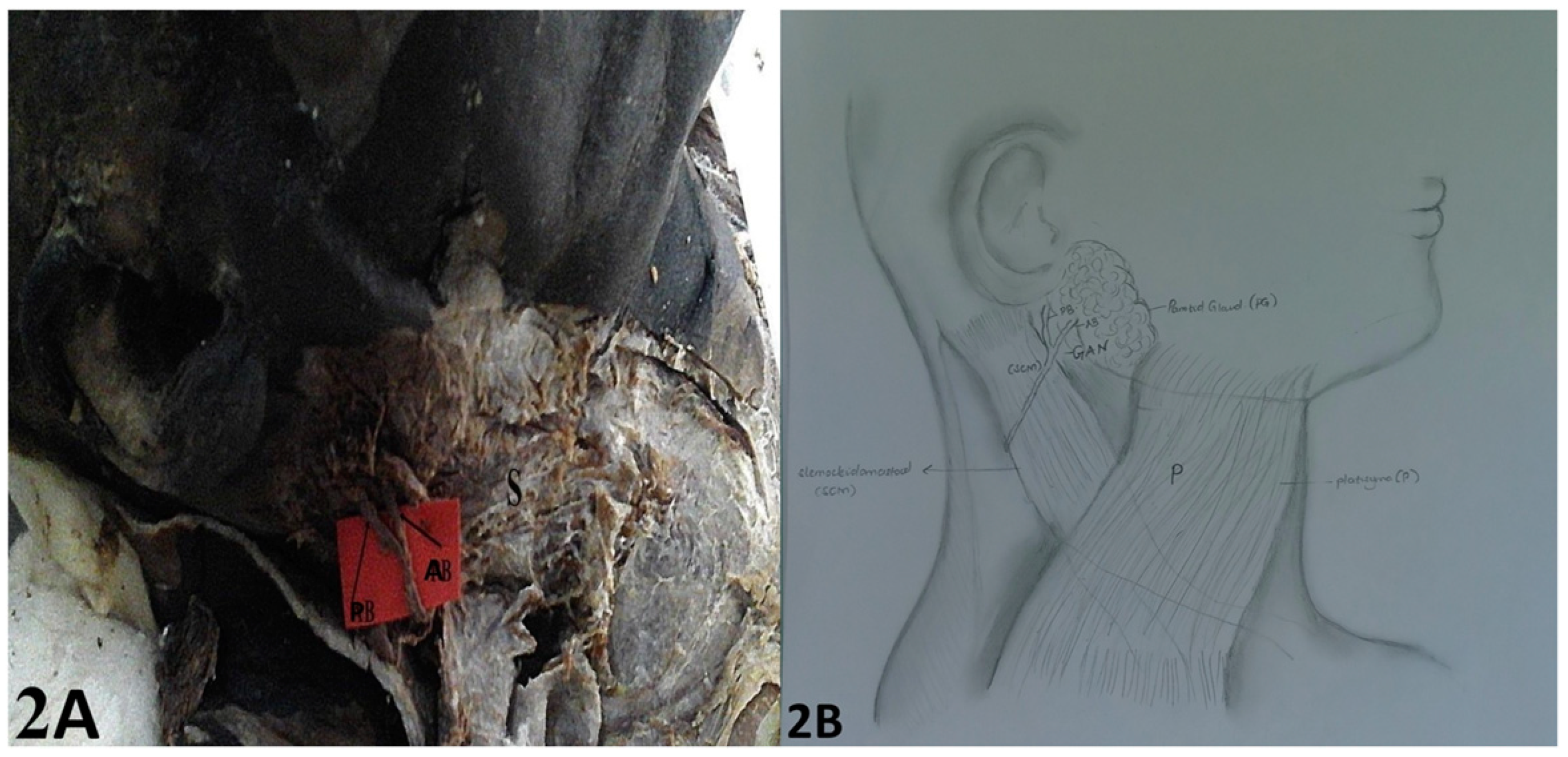
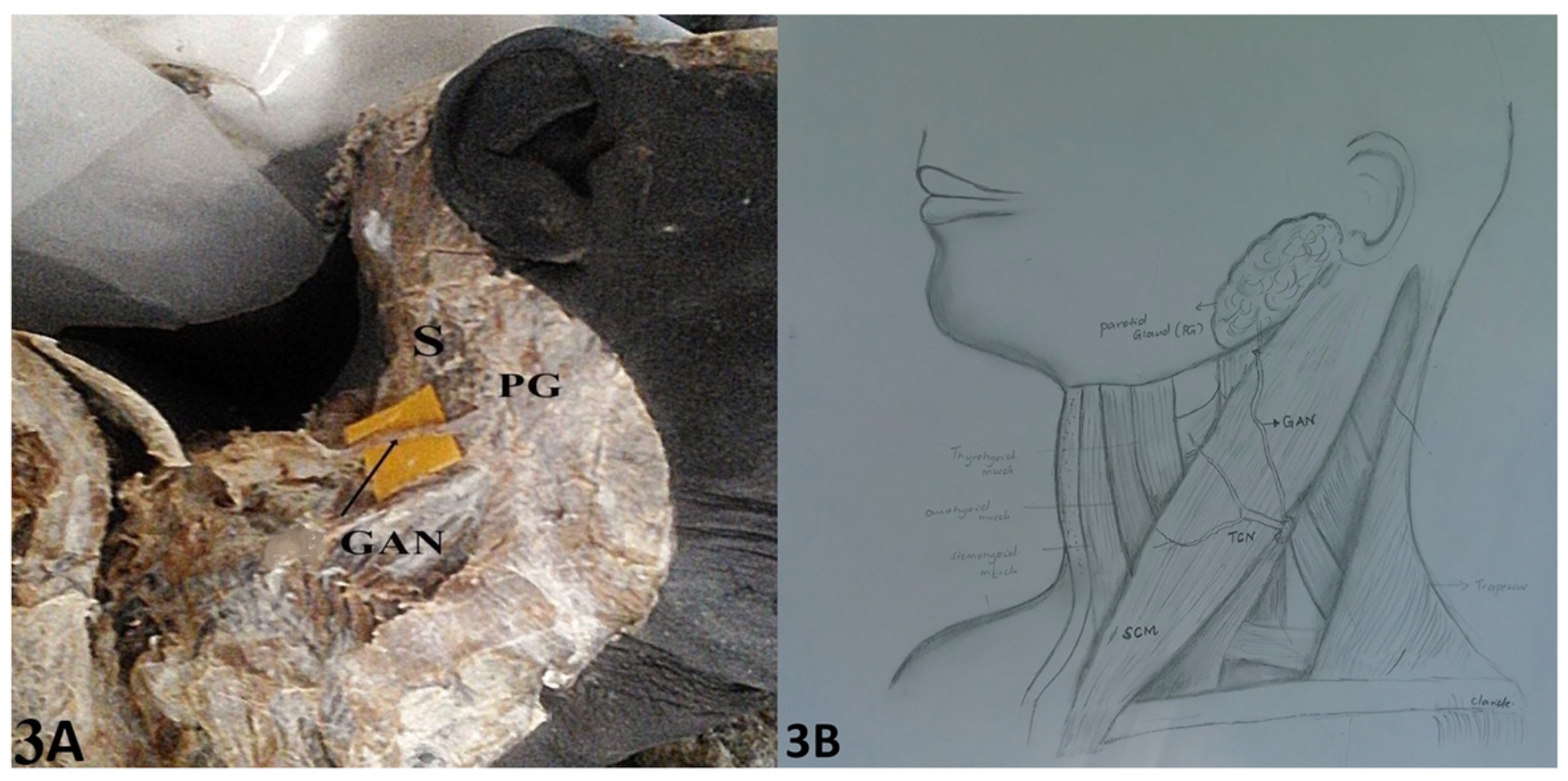
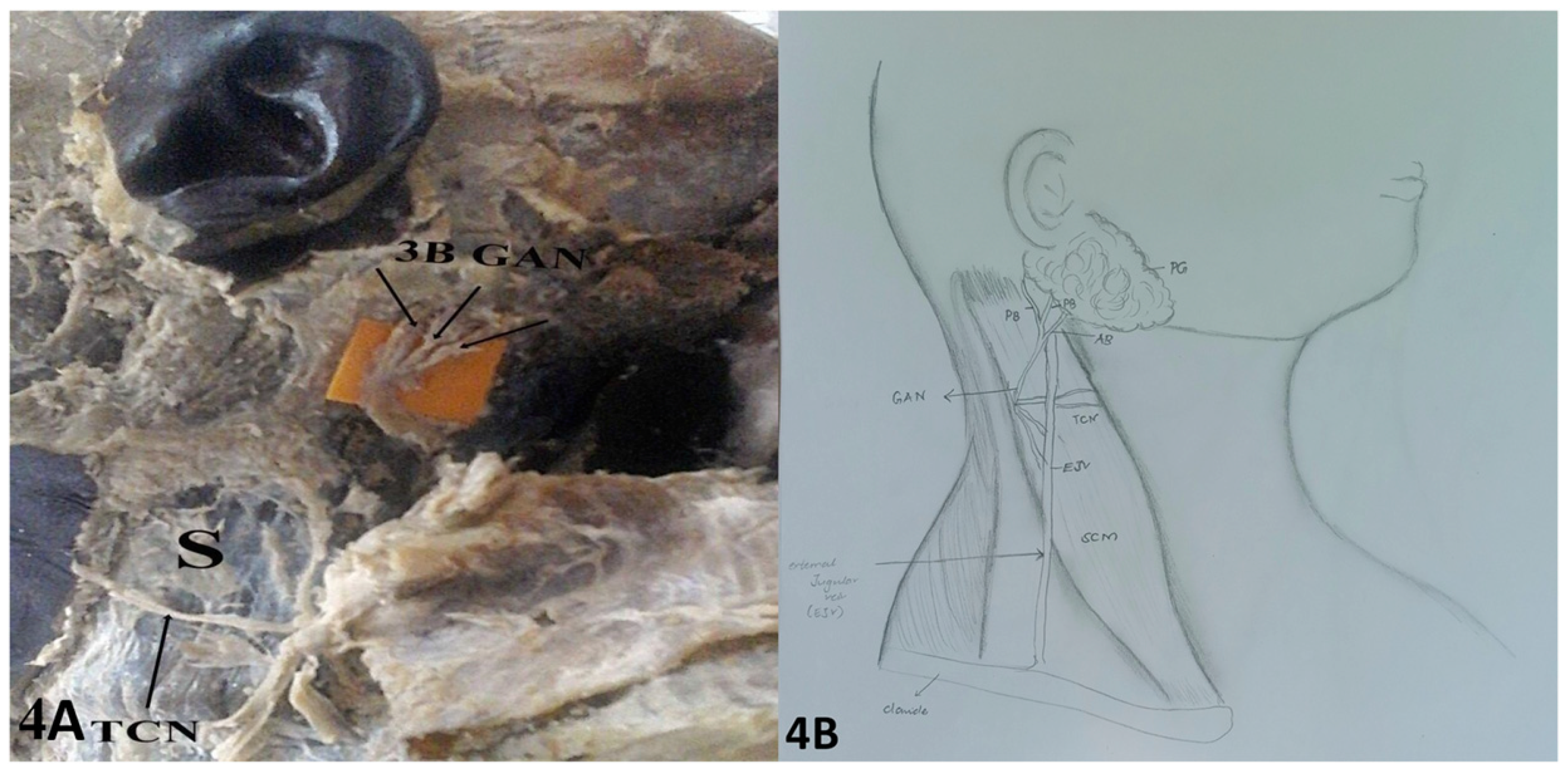
Branching Pattern of the GAN
Discussion
Anatomical Landmarks
Branching Patterns
Funding
Acknowledgments
Declaration of Conflicting Interests
References
- Gray, A.T. Atlas of Ultrasound-Guided Regional Anesthesia: Expert Consult – Online; Elsevier Saunders: Philadelphia, PA, USA, 2013; pp. 280–286. [Google Scholar]
- Gupta, C.; D’souza, A.S.; Raythe, B. Anatomical variations in the emergence of the cutaneous nerves from the nerve point in the neck and identification of the landmarks to locate the nerve point with its clinical implications: A cadaveric study on south indian human foetuses. J Clin Diagn Res JCDR. 2013, 7, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Borle, R.M. Textbook of Oral and Maxillofacial Surgery; Jaypee Brothers Medical Publishers (P) Ltd.: New Delhi, India, 2014; p. 715. [Google Scholar]
- Vidimos, A.T. Dermatologic Surgery; Elsevier Health Sciences: Edinburgh, PA, USA, 2009; p. 39. [Google Scholar]
- McKinney, P.; Katrana, D.J. Prevention of injury to the great auricular nerve during rhytidectomy. Plast Reconstr Surg. 1980, 66, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Ozturz, C.N.; Ozturk, C.; Huettner, F.; Drake, R.L.; Zins, J.E. A failsafe method to avoid injury to the great auricular nerve. Aesthet Surg J. 2014, 34, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Lefkowitz, T.; Hazani, R.; Chowdhry, S.; Elston, J.; Yaremchuk, M.J.; Wilhelmi, B.J. Anatomical landmarks to avoid injury to the great auricular nerve during rhytidectomy. Aesthetic Surg J Am Soc Aesthetic Plast Surg. 2013, 33, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Sand, T.; Becser, N. Neurophysiological and anatomical variability of the greater auricular nerve. Acta Neurol Scand. 1998, 98, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Zumeng, Y.; Zhi, G.; Gang, Z.; Jianhua, W.; Yinghui, T. Modified superficial parotidectomy: Preserving both the great auricular nerve and the parotid gland fascia. Otolaryngol -Head Neck Surg. 2006, 135, 458–462. [Google Scholar] [CrossRef] [PubMed]
- Pillay, P.; Partab, P.; Lazarus, L.; Satyapal, K.S. The great auricular nerve in fetuses. Int J Morphol. 2012, 30, 40–44. [Google Scholar] [CrossRef]
- Christensen, N.R.; Jacobsen, S.D. Parotidectomy. Preserving the posterior branch of the great auricular nerve. J Laryngol Otol. 1997, 111, 556–559. [Google Scholar] [CrossRef] [PubMed]
- George, M.; Karkos, P.D.; Dwivedi, R.C.; Leong, S.C.; Kim, D.; Repanos, C. Preservation of greater auricular nerve during parotidectomy: Sensation, quality of life, and morbidity issues. A systematic review. Head Neck. 2014, 36, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Marchese-Ragona, R.; De Filippis, C.; Marioni, G.; Staffieri, A. Treatment of complications of parotid gland surgery. Acta Otorhinolaryngol Ital. 2005, 25, 174–178. [Google Scholar] [PubMed]
- Colella, G.; Rauso, R.; Tartaro, G.; Biondi, P. Skin injury and great auricular nerve sacrifice after parotidectomy. J Craniofac Surg. 2019, 20, 1078–1081. [Google Scholar] [CrossRef] [PubMed]
- Hora´cio, J.; Aboudib, J.; Castro, C.C. Anatomical variations analysis of the external jugular vein, great auricular nerve, and posterosuperior border of the platysma muscle. Aesthetic Plast Surg. 1997, 21, 75–78. [Google Scholar]
- Murphy, R.; Dziegielewski, P.; O’Connell, D.; Seikaly, H.; Ansari, K. The great auricular nerve: An anatomic and surgical study. J. Otolaryngol. Head Neck Surg. 2012, 41 (Suppl 1), S75–S77. [Google Scholar] [PubMed]
- Sharma, V.; Surek, C.; Stephens, R.; Wright, B. What is the lobular branch of the great auricular nerve? Anatomical description and significance in rhytidectomy. Plast Reconstr Surg Glob Open. 2016, 4, 108. [Google Scholar] [CrossRef]

© 2023 by the author. The Author(s) 2023.
Share and Cite
Salim, S.B.; Amuti, T.; Butt, F. Anatomical Landmarks and Branching Patterns of the Greater Auricular Nerve. Craniomaxillofac. Trauma Reconstr. 2024, 17, 186-193. https://doi.org/10.1177/19433875231183032
Salim SB, Amuti T, Butt F. Anatomical Landmarks and Branching Patterns of the Greater Auricular Nerve. Craniomaxillofacial Trauma & Reconstruction. 2024; 17(3):186-193. https://doi.org/10.1177/19433875231183032
Chicago/Turabian StyleSalim, Swafiya Busaidy, Thomas Amuti, and Fawzia Butt. 2024. "Anatomical Landmarks and Branching Patterns of the Greater Auricular Nerve" Craniomaxillofacial Trauma & Reconstruction 17, no. 3: 186-193. https://doi.org/10.1177/19433875231183032
APA StyleSalim, S. B., Amuti, T., & Butt, F. (2024). Anatomical Landmarks and Branching Patterns of the Greater Auricular Nerve. Craniomaxillofacial Trauma & Reconstruction, 17(3), 186-193. https://doi.org/10.1177/19433875231183032



