Abstract
Abstract: Study Design: The authors designed a 20-year cross-sectional study using the National Electronic Injury Surveillance System (NEISS) database. Objective: The purpose of the study is to determine the risk factors for hospital admission among individuals who suffer head and neck injuries secondary to trampoline use. Methods: The primary predictor variables were a set of heterogenous variables that were categorized into the forementioned study variable groups (patient characteristics and injury characteristics). The primary outcome variable was hospital admission. Multivariate logistic regression was used to determine independent risk factors for hospital admission. Results: The final sample consisted of 13,474 reports of trampoline injuries to the head and neck. Relative to females, males (OR 1.66, P < .05) were at an increased risk for hospital admissions. Fractures (OR 35.23, P < .05) increased the risk for hospital admissions relative to dental injuries. Concerning anatomical region of injury, neck injuries (OR 30.53, P < .05) were at an increased risk for hospital admissions. Conclusions: Injuries to the neck from trampoline jumping significantly increased the risk for admission. The severity of neck injuries from trampoline jumping is well established in the literature. Additionally, male sex and fractures were each risk factors for hospital admission. Given the rising prevalence of trampoline-related head and neck injuries over the past 2 decades, it is crucial for individuals to take the necessary precautions when jumping on a trampoline.
Introduction
The coiled springs of a trampoline can store elastic energy and provide a rebound force that can propel an individual to supraphysiological heights. Built by the gymnasts George Nissen and Larry Griswold, the trampoline was designed to train tumblers. It was later used by fighter pilots and astronauts to enhance their spatial orientation. Their popularity continued to increase as trampolines were eventually distributed commercially for recreational use [1]. Trampolining ultimately went on to be inducted as a sport in the Olympics during the 2000 Sydney games [2].
A trampoline’s potential for danger was first studied in 1956 by Zimmerman et al [3]. Several studies thereafter went on to investigate whole body injuries secondary to trampoline use [4,5,6,7] with some studies limiting their study sample to the pediatric population [8,9,10,11]. A recent statewide study has reported head injuries to be 4.76% of all trampoline-related injuries [12]. Nevertheless, there have been no studies in the literature to date that specifically investigated head and neck injuries secondary to trampoline use. Trampoline-related injuries to the neck that have been reported are limited to case reports and series [13,14,15,16,17].
The purpose of the present study is to answer the following, “among individuals who suffer head and neck injuries secondary to trampoline use, what are the risk factors for hospital admission?” We hypothesized that injuries to the neck would be a risk factor for admission. The authors sought to: (1) identify the prevalence of head and neck injuries from trampoline use across the calendar years studied; (2) explore the specific mechanisms of injury associated with trampoline use; (3) describe the different types of injuries and the anatomical region of injury; (4) compare the admission rates across all study variables; and (5) determine independent risk factors for hospital admission.
Materials and Methods
Study Design and Sample Selection
This is a 20-year cross-sectional study conducted using the National Electronic Injury Surveillance System (NEISS), which is maintained by the Consumer Product Safety Commission (CPSC). The NEISS acquires data from a cohort of 100 hospitals, which were selected from all hospitals with 24-hour emergency departments containing at least 6 beds in the United States. This dataset is publicly available and contains reports of injuries from consumer products or sports and recreational activities. From January 2000 through December 2019, reports categorized under the code 1233 (trampoline; activity/apparel/equipment) were archived. Reports were excluded if they did not have the term “trampoline” in the narrative or if their mechanism of injury was not specified. Reports were also excluded if the injury did not occur in the head and neck region, which was defined using the following NEISS body part codes: 75, head; 76, face; 77, eyeball; 88, mouth; 94, ear; and neck, 89. Figure 1 illustrates how the regions of the head and neck as defined by the NEISS. The mouth includes the lips, tongue, and teeth while the face includes the eyelid area, nose, and forehead.
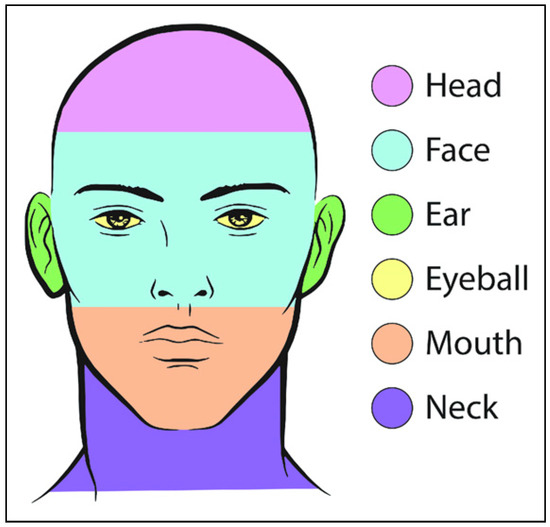
Figure 1.
Regions of the head and neck as defined by the NEISS.
Variables
Study variables consisted of patient and injury characteristics. Patient characteristics included age, gender (male and female), and race (White, Black, and Asian). Injury characteristics included season of injury (winter, spring, summer, and fall), diagnosis, anatomical region of injury (head, face, eyeball, mouth, ear, and neck), setting of injury, mechanism of injury, and hospital admission (yes or no).
Diagnosis was a nominal categorical variable (concussion, contusion/abrasion, fracture, hematoma, laceration, dental, brain injury, and strain/sprain). The NEISS database entails 2 diagnoses variables (diagnosis 1 and diagnosis 2) for each entry. Diagnosis 1 represents the most severe diagnosis associated with the product/activity: it was considered in our analysis. Hematoma represents an external head injury. Brain injury represents any of the forementioned insults to brain tissue, such as brain lacerations and brain contusions. Dental represents both tooth fractures and avulsions. Setting of injury was a binary variable (home and place of recreation or sports). In addition to a house, home includes exterior elements such as porch, patio, yard, and garden. Place of recreation or sports include playgrounds, amusement parks, and sports fields.
Mechanism of injury obtained from the provided injury narratives and was grouped into 6 classes: (1) collision with the ground; (2) collision with another person (intentional); (3) collision with another person (accidental); (4) collision with trampoline structure; (5) hyperextension injury; and (6) other. Hyperextension injury was defined as an injury sustained during the upward jumping motion. Other injuries consisted of various miscellaneous mechanisms of injury such as “patient bit lip/tongue while jumping on trampoline” and “patient struck own knee while jumping on trampoline.”
Patients were considered admitted if they were held for observation, treated and admitted, or treated and transferred. Patients were not considered admitted if they were examined and released or if they left without being seen. The primary predictor variables were a set of heterogenous variables that were categorized into the forementioned study variable groups above (patient characteristics and injury characteristics). The primary outcome variable was hospital admission.
Data Analyses
Descriptive statistics were calculated for all study variables. Univariate analyses (chi-square or Fisher exact) were conducted to determine associations of the primary predictor variables and the outcome variable. Predictor variables with a significant (P < .05) or near-significant associations (P < .05) with the outcome variable were further analyzed via multivariate logistic regression model to determine independent risk factors of admissions. A P-value of less than .05 was considered statistically significant. All statistical calculations were performed using SPSS version 25 for Mac (IBM Corp, Armonk, N.Y., USA). As per our medical center policy, research involving the analysis of de-identified data from publicly available datasets does not require institutional review board approval.
Results
The total number of trampoline injuries reported in the NEISS from 2000 to 2019 was 65,152. After filtering for injuries to the head and neck exclusively, there were 13,665 cases remaining. After excluding for cases where the reported mechanism of injury was not specified or the injury was in fact not due to the act of jumping on a trampoline (eg, boy was jumping on trampoline and threw piece of wood at friend outside), our final sample consisted of 13,474 cases. A majority of the patients were under the age of 18 (93.1%). More than half of the sample consisted of males (64.3%). With regards to race, 86% of the patients were white. The most frequently injured anatomical region was the head (34.6%). The most common diagnosis was laceration (32.8%). Overall, 88.7% the injuries took place in the patient’s home. Falling on the trampoline was the most common mechanism of injury (52.6%).
The calendar year where the greatest number of trampoline injuries occurred was 2017 (863 injuries), while the fewest quantity of injuries transpired in 2001 (509 injuries). The increase in the number of injuries from 2000 to 2019 was significant (P < .05) (Figure 2).
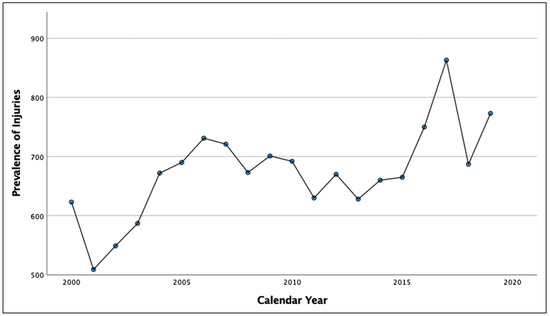
Figure 2.
Prevalence of patients with trampoline injuries presenting to US emergency departments, 2000–2019.
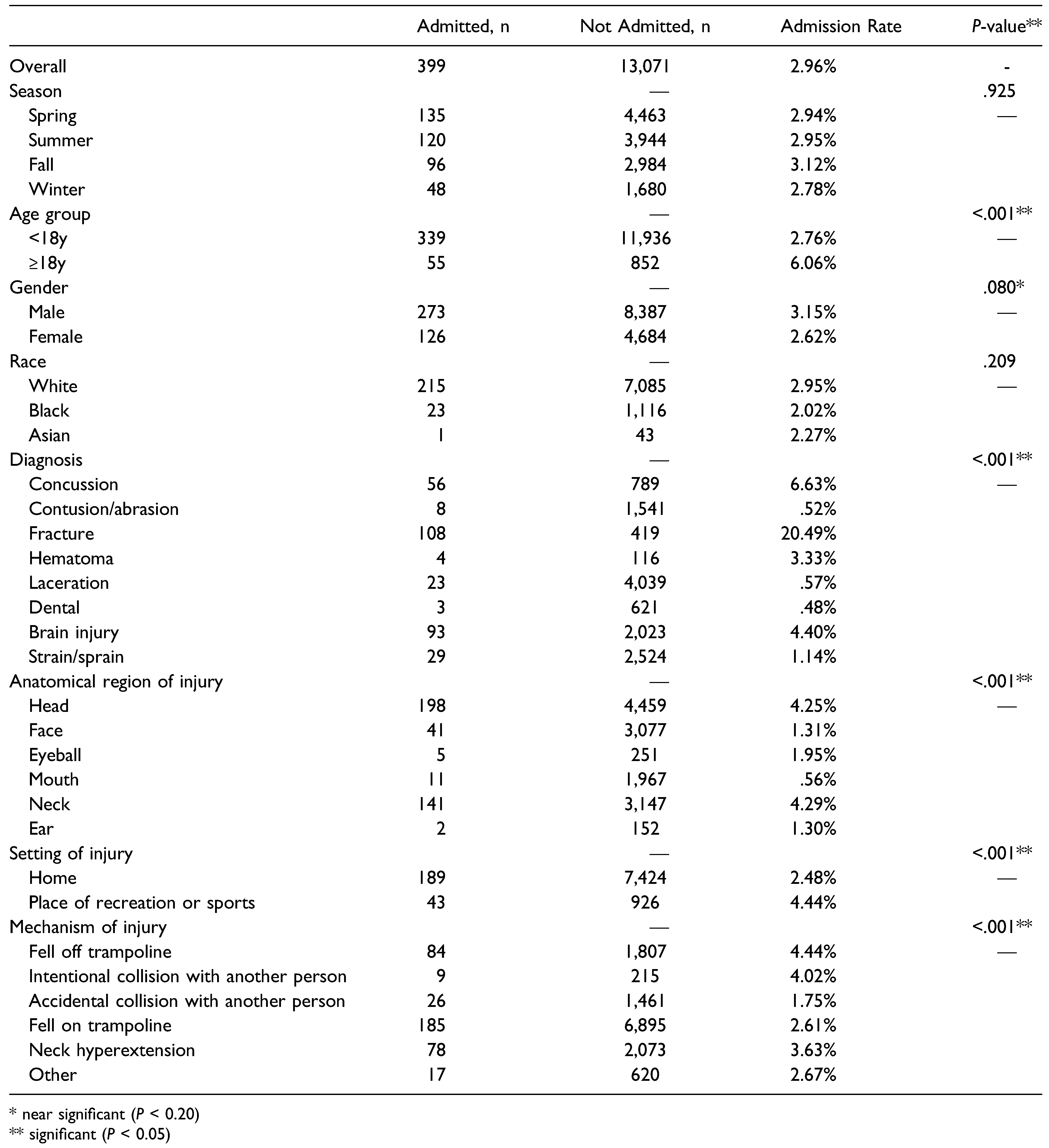
When examined across hospital admissions (Table 1), age group, diagnosis, anatomical region of injury, setting of injury, and mechanism of injury were all significant predictors (P < .05) of admissions and, hence, were further analyzed via logistic regression. Gender was a near significant predictor (P < .20) of admissions and was also analyzed via logistic regression. Because race is a biologically relevant variable, it was added to the logistic regression model regardless of its statistical significance.

Table 1.
Admission Rate Stratified by Season, Patient Demographics, Injury Characteristics, and Mechanism of Injury.
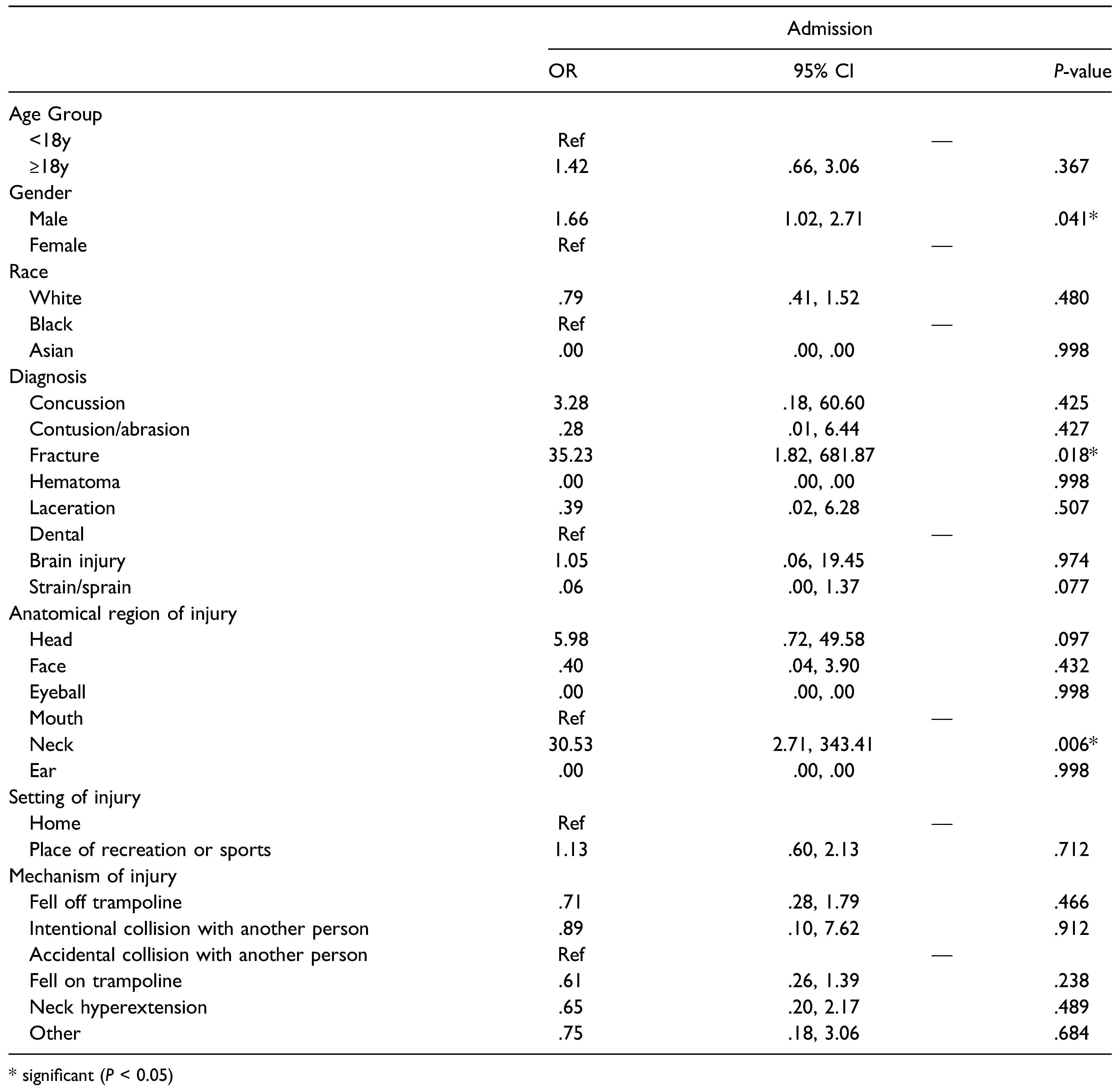
Table 2 illustrates the results of our multivariate logistic regression model. Relative to females, males (OR 1.66, P < .05) were at an independently increased risk of hospital admissions. Regarding diagnosis, fractures (OR 35.23, P < .05) were at an independently increased risk of hospital admissions relative to dental injuries. Concerning anatomical region of injury, neck injuries (OR 30.53, P < .05) were at an independently increased risk of hospital admissions.

Table 2.
Multivariate Logistic Regression for Odds of Admission.
Discussion
The purpose of this study was to identify risk factors for hospital admission among individuals who suffer head and neck injuries secondary to trampoline use. Ultimately, we rejected the null hypothesis—injuries to the neck were a risk factor for admission. Additionally, male patients and patients who suffered fractures were each at independently increased risk for hospital admission.
The prevalence of trampoline-related head and neck injuries increased across the 20-year study period. Trampoline-related injuries have been on a continuous rise decades before our study period. In a descriptive epidemiologic study of injuries secondary to trampoline use in New Zealand, Chalmers et al. determined a statistically significant 3-fold increase in the incidence of hospitalizations from 1979 to 1988. Thereafter, in a retrospective analysis of trampoline-related injuries among children, Smith et al. discovered that the number of yearly injuries almost doubled form 1990 (n = 29,600) to 1995 (n = 58,400). We suggest 2 possibilities for this increase in trampoline related head and neck injuries. The general increase in access and availability of owning a trampoline in a private home may contribute to the increase in total number of injuries over the 20-year period being studied or possibly the rising adoption of risky maneuvers by individuals while jumping on a trampoline.
Patients who sustained an injury to the neck were over 30 times more likely to be admitted. Neck injuries from trampolines are severe, being a major cause of neurological sequelae, such as sensory deficits, torticollis, motor weakness, severe paralysis (ie, quadriplegia), and Horner’s syndrome [13,14,15,16,17,18,19,20]. Neck injuries can also be severe enough to result in death [14,20].
Leonard et al. retrospectively analyzed patients under 18 years who presented with a cervical spine injury between 1995 and 2006. Seven patients met the inclusion criteria, all of whom were hospitalized for an average of 9.5 days, except for one who succumbed to their injuries. All 6 admitted patients required comprehensive imaging, including x-rays, computed tomographic scans and magnetic resonance imaging, and 3 required surgeries for spinal stabilization. Four patients had enduring neurological deficits at the time of discharge.
Another study presented their experience with 16 cases of spinal injuries from trampolines. The majority of the patients had lower cervical spinal fractures from landing erroneously on their head. Ultimately, 14 patients (87.5%) developed paralysis. Injuries were seen in both proficient and novice athletes and was not a factor in sustaining injuries. Silver et al. hypothesized that an instructor’s lack of supervision was an important factor in injury since the athletes performed riskier maneuvers in their absence. They also suggested that an instructor’s inexperience with the trampoline was another important factor in injury, where some instructors would advance athletes prematurely and progress to advanced techniques beyond their ability. Last, the authors believed that many athletes did not fully comprehend the dangers and potentially devastating injuries associated with a trampoline.
Patients who sustained fractures were over 35 times more likely to be admitted. This result confirmed a previous retrospective study by Lee et al. on patients under 18 years of age who suffered whole body trampoline-related injuries. The authors determined that, among other factors, patients who suffered fractures were over 18 times more likely to get admitted. Similarly, a study that compared backyard trampoline injuries with trampoline park injuries determined that fractures accounted for the majority of hospital admissions for both types of trampolines. Fractures of the skull, particular the cranial vault and skull base, can damage the neurologic system. Depressed cranial vault fractures can have an infection rate upwards of 10 and a 15% incidence of late epilepsy. Frontobasal fractures can injure the upper cranial nerves, the paranasal sinuses, and cavernous sinuses.
Further, CSF rhinorrhea results in 4 to 48% of frontobasal fractures and pneumocephalus in 10 to 50% [21]. As was discussed earlier, fractures of the cervical vertebrae secondary to trampolining are well documented, most of which are associated with devastating consequences ranging from sensory deficits to quadriplegia.
Injuries at trampolines located within places of sports/recreation were associated with higher rates of admission than injuries at home trampolines. However, injuries at sports/recreation trampolines were not an independent risk factor for hospital admissions. According to the NEISS, places of sports/recreation include parks. Mujadi et al. conducted a meta-analysis to determine risk factors for trampoline injuries that necessitate surgical therapy. The authors determined that park trampolines increased the risk for injuries requiring surgery by more than 2-fold relative to home trampolines.
Sex was a risk factor for hospital admissions—males were 1.7 times more likely to be admitted relative to females. This result conflicted with a meta-analysis that explored the risk factors for trampoline injuries requiring surgery. Mujadi et al. determined that females were 1.5 times more likely to sustain a trampoline-related injury requiring surgery relative to males. This disparity with the results of our study could be because Mujadi et al. did not limit the anatomical region of injury to the head and neck, including injuries to the entire body. The most common region of injury in the meta-analysis was the lower extremity (42%) likely due to falling on the trampoline (30%).
Although these are conflicting reports it is not relevant in practice. The potentially devastating injuries necessitate strict safety and trainings regardless of sex.
The rates of hospital admission were significantly different among the mechanisms of injury studied, with falling off the trampoline having the highest rate. However, no particular mechanism of injury proved to be an independent risk factor for admission. Conversely, Lee et al. determined that falling was an independent risk factor for hospital admission among pediatric patients with trampoline-related injuries. Their study included all regions of the body that were injured. They noted that falls are especially injurious to the extremities, which are often the first point of contact with a trampoline structure or ground to break a fall and protect the head. Studying this subset of patients may have elucidated an independent risk factor in the population of South Koreans they studied.
Several positions on trampoline use and recommendations to prevent injuries have been posed over the years. As early as 1977, The American Academy of Pediatrics (AAP) recommended that trampolines be completely banned since trampoline-related injuries were the leading cause of spinal cord injuries with subsequent paralysis [22]. However, years later, the AAP revised their position on trampoline use in their paper “Trampoline II.” The organization approved the use of trampolines under certain circumstances with multiple restrictions, such as the strict presence of a spotter whenever the trampoline is in use [23]. The rate of trampoline injuries increased following this new position by the AAP. In 1999, the AAP further revised their position on trampoline use. In addition to the restrictions postulated in Trampoline II, the APP does not permit trampoline use as part of routine physical education classes in school [24]. Not content with the APP latest position on trampolines, several authors support a complete ban on trampoline use among children. In contrast, other authors favor a more lenient stance on trampolines for the health benefits associated with trampoline use. The authors cite that physical inactivity is associated with many diseases and disorders, which represents a greater health hazard to children than the risk of injury [5].
This study is not without limitations. We had no insight into the specifications of the trampoline at hand, such as its size and the presence of safety nets. Another limitation is that the NEISS records data on a single emergency department visit, not providing follow-up data that allows for longitudinal analysis. The NEISS also did not reliably provide insight into other details that complete context of the trampoline-related injury, such as the presence of parental supervision (for children) or a spotter (for adults), the number of people simultaneously jumping on the trampoline, and the person’s experience and skill level with the trampoline. Withstanding these limitations, our study uses the NEISS database which is nationally representative sample of hospitals throughout the US and is not confined to a certain region or state, enhancing the external validity and generalizability of our results.
In summary, injuries to the neck from trampoline jumping significantly increased the risk for admission. This result is consistent with the literature, which contains several reports that reflect the severity of neck injuries and their neurological sequelae from trampoline jumping. Additionally, male patients and patients who suffered fractures were each at independently increased risk for hospital admission. Given the increase in the prevalence of trampoline-related head and neck injuries over the past 2 decades, it is important for individuals to take the necessary precautions when jumping on a trampoline. This includes jumping within one’s own technical capacity, avoiding risky maneuvers, and (for pediatric patients) adequate supervision by parents and caregivers.
Supplementary Materials
Supplemental material for this article is available online.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
The study would like to acknowledge Eric Litman and Maria Yanez for deciphering the mechanism of injury from the narratives for each NEISS entry.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Wikipedia. Trampoline. 2022. https://en.wikipedia.org/wiki/ Trampoline#First_modern_trampolines.
- International Olympic Committee. GYMNASTICS History of Trampoline at the Olympic Games . 2017. https://stillmed.olympic.org/media/Document%20Library/OlympicOrg/Factsheets-Reference-Documents/Games/OG/History-of-sports/Reference-document-Gymnastics-Trampoline-History-at-the-OG.pdf.
- Zimmerman, H.M. Accident experience with trampolines. Res Q Am Assoc Health Phys Educ Recreat. 1956, 27, 452–455. [Google Scholar] [CrossRef]
- Ashby, K.; Pointer, S.; Eager, D.; Day, L. Australian trampoline injury patterns and trends. Aust N Z J Publ Health. 2015, 39, 491–494. [Google Scholar] [CrossRef] [PubMed]
- Nysted, M.; Karlsson, J.; Drogset, J.O. Trampoline injuries. Br J Sports Med. 2006, 40, 984–987. [Google Scholar] [CrossRef] [PubMed]
- Muljadi, J.A.; Chaijenkij, K.; Arirachakaran, A.; Kongtharvonskul, J. Comparative surgical risk between type of trampoline (size and place) and type of patients (age and sex) in trampoline related injury: a systematic review and indirect meta-analysis. BMC Sports Sci Med Rehabil. 2020, 12, 37. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, D.J.; Hume, P.A.; Wilson, B.D. Trampolines in New Zealand: A decade of injuries. Br J Sports Med. 1994, 28, 234–238. [Google Scholar] [CrossRef]
- Lee, G.; Kim, D.K.; Park, J.W.; Kwak, Y.H.; Jung, J.Y. Trampoline-related injuries in children: A nationwide cross-sectional study in South Korea. Clin Exp Emerg Med. 2020, 7, 190–196. [Google Scholar] [CrossRef]
- Wootton, M.; Harris, D. Trampolining injuries presenting to a children’s emergency department. Emerg Med J. 2009, 26, 728–731. [Google Scholar] [CrossRef]
- Shankar, A.; Williams, K.; Ryan, M. Trampoline-related injury in children. Pediatr Emerg Care. 2006, 22, 644–646. [Google Scholar] [CrossRef]
- Rao, D.P.; McFaull, S.R.; Cheesman, J.; Do, M.T.; Purcell, L.K.; Thompson, W. The ups and downs of trampolines: Injuries associated with backyard trampolines and trampoline parks. Paediatr Child Health. 2019, 24, e19–e25. [Google Scholar]
- Sullivan, M.C.; Morgan, M.E.; Bradburn, E.; Perea, L.L. Trampoline injuries in a statewide trauma system. Am Surg. 2022, 88, 419–423. [Google Scholar] [CrossRef]
- Maranich, A.M.; Hamele, M.; Fairchok, M. Atlanto-axial subluxation: A newly reported trampolining injury. Clin Pediatr (Phila). 2006, 45, 468–470. [Google Scholar] [PubMed]
- Leonard, H.; Joffe, A.R. Children presenting to a Canadian hospital with trampoline-related cervical spine injuries. Paediatr Child Health. 2009, 14, 84–88. [Google Scholar] [PubMed]
- Brown, P.G.; Lee, M. Trampoline injuries of the cervical spine. Pediatr Neurosurg. 2000, 32, 170–175. [Google Scholar]
- Silver, J.R.; Silver, D.D.; Godfrey, J.J. Trampolining injuries of the spine. Injury. 1986, 17, 117–124. [Google Scholar]
- Ellis, W.G.; Green, D.; Holzaepfel, N.R.; Sahs, A.L. The trampoline and serious neurological injuries. JAMA. 1960, 174, 1673–1677. [Google Scholar]
- Smith, G.A. Injuries to children in the United States related to trampolines, 1990-1995: a national epidemic. Pediatrics. 1998, 101, 406–412. [Google Scholar]
- Torg, J.S.; Das, M. Trampoline-related quadriplegia: review of the literature and reflections on the American Academy of Pediatrics’ position statement. Pediatrics. 1984, 74, 804–812. [Google Scholar]
- Rapp, G.F.; Nicely, P.G. Trampoline injuries. Am J Sports Med. 1978, 6, 260–271. [Google Scholar] [PubMed]
- Fonseca, RJ. Oral & Maxillofacial Trauma, 4th ed.; Saunders: St. Louis, MO, USA, 2013. [Google Scholar]
- American Academy of Pediatrics, C.o.A.a.P.P. Trampolines. Pediatrics. 1977, 28, 5. [Google Scholar]
- American Academy of Pediatrics CoAaPPaCoPAoPF, Recreation, and Sports. Trampolines II. Pediatrics. 1981, 67, 438.
- Trampolines at home, school, and recreational centers. American Academy of Pediatrics. Committee on Injury and Poison Prevention and Committee on Sports Medicine and Fitness. Pediatrics. 1999, 103, 1053–1056. [Google Scholar]
© 2022 by the author. The Author(s) 2022.