Abstract
Study Design: Face and content validation of a surgical simulation model. Objective: Open reduction and internal fixation in displaced subcondylar mandibular fractures is standard care. This requires an extraoral (eg: retromandibular, transparotideal) or intraoral approach. An intraoral approach requires further training since specialized instrumentation such as the 90° screwdriver system and endoscopes might be needed. Currently, no simulation models are available for training residents in intraoral reduction and fixation of subcondylar mandibular fractures. Therefore, we present a validated simulation model for intraoral treatment of subcondylar mandibular fractures. Methods: Based on a computer tomography data set, we designed and printed a 3D model of a mandible with a unilateral subcondylar fracture. To simulate intraoral work depth, it was positioned inside a dental phantom. We tested the model by a group of experts (n = 8), simulating intraoral reduction and fixation of a unilateral subcondylar fracture, using a 90° screwdriver system, a 1.0 subcondylar plate (lambda), and 5-6 mm screws. We assessed Face and Content validity by survey. Results: We provided an open-source printable fracture model. Printing costs were approximately US $10. Experts “Agreed” the model resembling the real scenario and its use for training intraoral reduction and fixation of subcondylar mandibular fractures. Conclusions: We developed a low cost, reproducible, open-source simulator for subcondylar mandibular fractures. Face and Content validity was achieved through evaluation by a group of experts.
Introduction
Proper management of subcondylar mandibular fractures has been a subject of debate for many years. Open reduction might be challenging, with risks including sialocele, facial nerve palsy, bleeding, hematomas, insufficient reduction, and malunion of bone fragments. There is no consensus on the gold standard treatment on various patterns of condylar and subcondylar mandibular fractures. Recently, the indication for surgery has undergone a paradigm shift. [1,2,3,4] Advances in 3D modeling, anatomical plates, endoscopy, and 90° screwdriver systems made surgery more predictable by giving surgeons tools to achieve better outcomes. [5,6,7]
The COVID-19 pandemic brought challenges to surgery residency programs because of low exposure to their specialty’s daily duties. But this scenario gave more attention to simulation tools. Patient care needs a resident with experience and proper exposure to various treatments, resulting in better surgical outcomes, less hospitalization time, and complications. Despite existing considerable literature describing the use of simulation in surgical specialties and anesthesiology residents, there is insufficient information in oral and maxillofacial surgery (OMS) programs. [5,6,7,8,9] Programs on OMS need to evaluate the reality of clinical work with the importance of better outcomes, low risk, and proficiency-based training that simulation can provide. Simulation gives the occasion to evaluate specific educational objectives consistent with a program’s strengths and ensure that residents gain experience in non-frequent and high complexity procedures making learning conducive to all levels. Current residency programs with plans of executing simulation education might need a change in ideology, where the learner is the educational focus, ensuring that errors are used as teaching points, with the benefit of previous exposure and experience before real treatments. Further, it promotes competency based on validated measurements. [5,6,9,10]
The OMS residency program at Pontificia Universidad Católica de Chile is developing and implementing simulation with the institution’s Medicine School and Simulation Training Center into the curriculum of residency training.
The aim of our study was to develop and validate a low cost, reproducible simulator for an intraoral approach for open reduction and internal fixation of subcondylar man-dibular fractures.
Materials and Methods
Model Design
After signing informed consent, a head and neck computer tomography scan of a random patient was modified using a 3D software (Meshmixer 3.5). A subcondylar fracture was designed using a linear osteotomy from the sigmoid notch to the subcondylar area of the right side of the mandible. Figure 1 and Figure 2 shows the printed 3D model of the mandible fracture with filaments of Polylactic acid (PLA). Figure 3 shows the model inside a dental phantom to simulate intraoral work depth.

Figure 1.
Printed mandibular three-dimensional model with right mandibular subcondylar fracture.

Figure 2.
Dental Phantom with inserted fracture model for intraoral internal fixation of the subcondylar fracture with the 90° screwdriver and subcondylar plate systems.

Figure 3.
Subcondylar fracture with osteosynthesis performed (subcondylar lambda plate).
Osteosynthesis Systems
Plates and screws of the “Matrix Mandible subcondylar plates system” (DePuy Synthes) were used. We performed open reduction and internal fixation with the 90° screwdriver system, 1.0 subcondylar plates (lambda), and 5–6 mm screws (DePuy Synthes). Traditional maxillofacial surgery instruments were used.
Evaluation: Face and Content Validity
A group of 8 expert maxillofacial surgeons tested the simulation model for subcondylar fractures performing reduction and fixation in the simulator, followed by answering a face and content validity questionnaire to evaluate the realism of the model and its utility in surgical training for maxillofacial residents.
Face validity evaluates if the surgical simulator has a high degree of reality. Content validity describes the extent to which a simulator teaches the skills required for a successful surgical procedure.
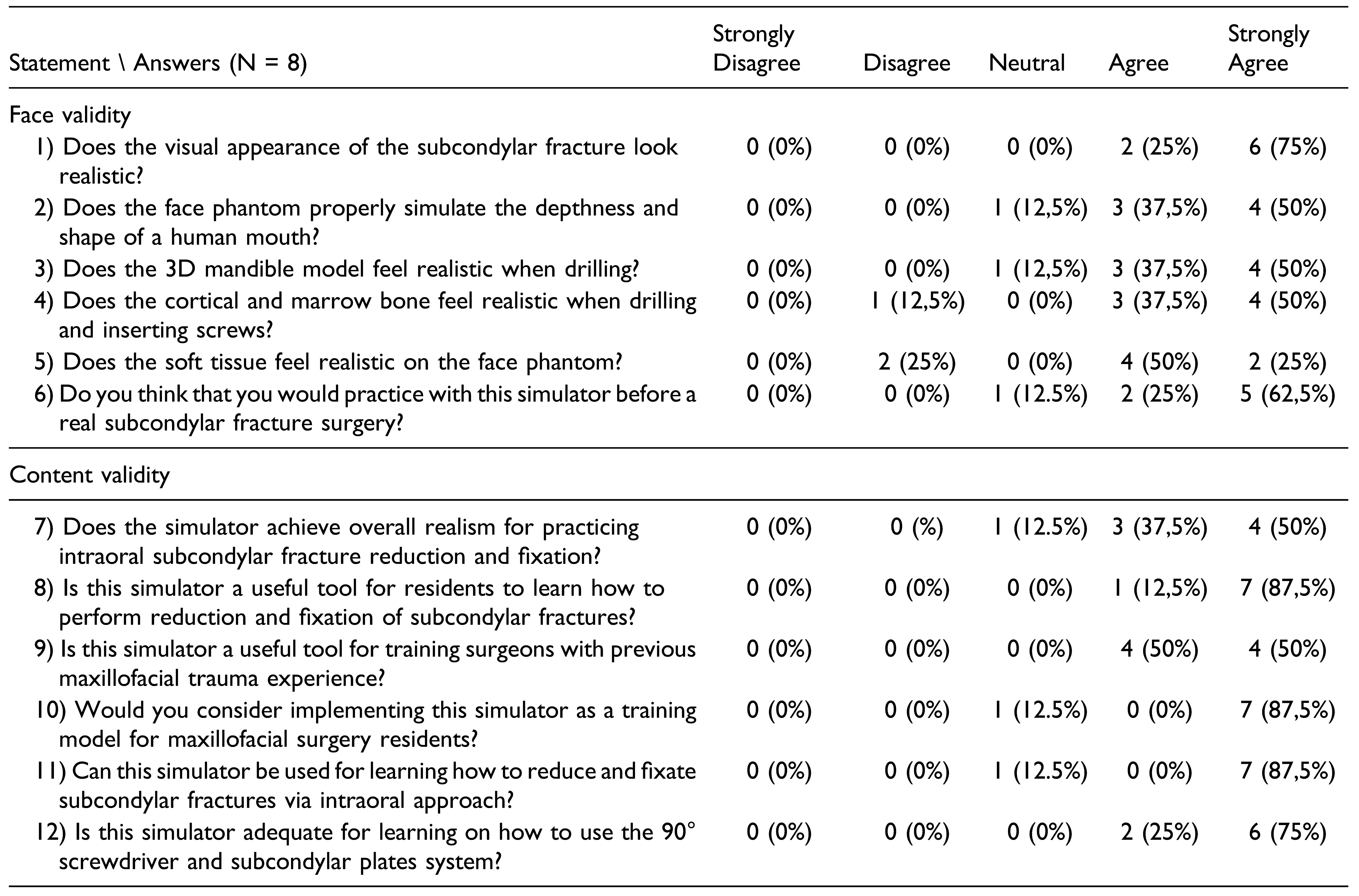
All experts considered eligible were trained oral and maxillofacial surgeons in Chile and have experience in treating maxillofacial trauma. After testing the subcondylar fracture simulation model, performing reduction and fixation of the fractures, all participants completed a Likert face and content validity questionnaire. The survey was conducted among the experts using Google Forms (Google Inc, California, US). Survey Form is enclosed in Table 1, and results were analyzed in Microsoft Excel v.18 (Microsoft Corporation, Washington, US). Descriptive statistics were used.

Table 1.
Likert Survey of Face and Content Validity.
Results
Model Development
The segmented mandible in Figure 1 is accessible as a Standard Tessellation Language-File (stl-file) for 3D printing at the National Institutes of Health 3D print exchange website (https://3dprint.nih.gov). The 3D subcondylar mandibular fracture model was printed in polylactid acid (PLA) and inserted in a dental phantom. Cost for printing the 3D model using PLA was approximately US $10.
Face and Content Validation
Table 2 shows the results of the Likert survey assessing face and content validity describing the realistic degree of this model and to which extent it can teach the skills required for the surgical intervention.

Table 2.
Likert Survey Assessing Face and Content Validity Results.
Face Validation Results
A total of 6 (75%) experts strongly agreed and 2 (25%) agreed that the visual appearance of the simulator looked realistic, 4 (50%) experts strongly agreed that the dental phantom simulated deepness and shape of a human mouth, 3 (37.5%) agreed and 1 (12.5%) experts remained neutral, 4 (50%) experts strongly agreed that the 3D mandible felt realistic when drilling, 3 (37.5%) agreed and 1 (12.5%) experts remain neutral. Regarding if bone marrow and cortical bone feels realistic when drilling and screwing, 4 (50%) experts strongly agreed, 3 (37.5%) experts agreed and 1 (12.5%) expert disagreed, 2 (25%) experts strongly agreed that the soft tissue felt realistic on the dental phantom, 4 (50%) experts agreed and 2 (25%) disagreed, 5 (62.5%) experts strongly agreed and 2 (25%) agreed on practicing with this subcondylar simulation model before a real surgery.
Content Validation Results
Half of the experts 4 (50%) strongly agreed and 3 (37.5%) experts agreed the simulator achieving overall realism for practicing subcondylar fracture reduction and fixation, whereas 1 (12.5%) expert disagrees, 7 (87.5%) experts strongly agreed, and 1 (12.5%) expert agreed the simulator being a useful tool for training residents and teaching them how to perform reduction and fixation of subcondylar fractures. After testing the simulator, 4 (50%) experts strongly agreed and 4 (50%) agreed the simulator being useful for training surgeons with previous maxillofacial trauma experience. Seven (87.5%) experts strongly agreed on implementing the simulator as a training model for maxillofacial surgery residents, meanwhile 1 (12.5%) expert remained neutral on the matter. Also, seven (87.5%) experts strongly agreed the simulator being usable to learn how to reduce and fixate subcondylar fractures via intraoral approach.
This simulator was found adequate for learning how to use the 90° screwdriver system and the subcondylar plates system, with 6 (75%) experts strongly agreeing and 2 (25%) of them agreeing.
Discussion
Oral and maxillofacial surgery programs have increased their interest in simulation as a part of their learning curve for residents. New simulation models have been designed and validated in several surgical specialties, where new learning programs based in simulation training have shown to improve abilities, shorten the learning curve, and reduce complications, giving the residents more confidence in surgical practice. This requires transferring what has been learned from the simulation model to the operating room, through a validated educational tool. [11,12]
Literature supports results and reduction of clinical costs when a procedure is performed by surgeons with this method of learning, in comparison to professionals with little experience, which in some cases could be applied to the reality during the pandemic. [5,6,9,12]
The acquisition of surgical and therapeutic experience is not an easy task; however, the use of simulators could contribute to the transfer of knowledge and skills from the theory to the patient. However, this requires an adequate validation process. [12,13,14,15,16,17,18,19,20,21,22]
Surgical simulation courses have become crucial for resident training and board certification with an exponential increase in development of new simulation models. As they showed improvement in technical skills, confidence and transferability of the acquired skills to the operating room. [10,13] In total, 79% of trainees report that simulation training would be beneficial in surgery providing them better technical preparation and confidence towards the trained procedure. [18] This study designed and examined the realism and usefulness of a novel subcondylar fracture simulating model. The expert testing group agreed the simulation model being highly realistic and usable in training maxillofacial surgery residents.
On this model, 28%% of the experts agreed and 62.5% strongly agreed with the validation process. The present model would be a good tool for training residents in the future but needs experienced surgeons teaching proper techniques and surgical steps. Regarding the material used for bone simulation, PLA showed good performances in other maxillofacial simulation models because of its low cost, biodegradability, non-toxicity, and with more similarity to bone than other materials while drilling at low temperature with continuous cooling. A disadvantage is lack of simulation of the difference in drilling sensation between cortical and cancellous bone and it may melt at higher temperatures. [13] In our study, experts reported the bone drilling sensation feeling realistic overall. From all experts, 87.5% strongly agreed that this simulator is a useful tool for training residents and teaching them how to perform reduction and fixation of subcondylar fractures, and also strongly agreed on implementing this simulator as a training model for maxillofacial surgery residents.
However, additional soft tissues and cortical perforation sensation may be further developed with other materials. Further research must aim at assessing construct validity and clinical skill transferability as some simulation models lacked transferability to the operating room. [18,19,20,21,22]
Conclusions
In the context of COVID-19 pandemic, surgical simulation courses have become crucial for training residents. This study describes the design and validation of a subcondylar fracture simulation model, its usefulness on training maxillofacial surgery residents and how realistic it is when comparing with real patients. We present a low cost, reproducible, realistic subcondylar fracture simulation model, adequate for training maxillofacial surgery residents in subcondylar fractures. Evaluated scores correspond to a high evaluation level, and all participants characterized the simulation model as realistic and with high teaching potential for maxillofacial surgery residents.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank Johnson & Johnson (DePuy Synthes) for their collaboration with the “90o screwdriver system for minimally invasive drilling and screw insertion” and “Matrix Mandible sub-condylar plates system.”
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Dayalan, N.; Kumari, B.; Khanna, S.; et al. Is open reduction and internal fixation sacrosanct in the management of subcondylar fractures: A comparative study. J Pharm BioAllied Sci. 2021, 13, S1633–S1636. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E.; Throckmorton, G.S. Treatment of mandibular condylar process fractures: Biological considerations. J Oral Maxillofac Surg. 2005, 63, 115–134. [Google Scholar] [CrossRef]
- Singh, V.; Bhagol, A.; Goel, M.; Kumar, I.; Verma, A. Outcomes of open versus closed treatment of mandibular subcondylar fractures: A prospective randomized study. J Oral Maxillofac Surg. 2010, 68, 1304–1309. [Google Scholar] [CrossRef]
- Hackenberg, B.; Lee, C.; Caterson, E.J. Management of subcondylar mandible fractures in the adult patient. J Craniofac Surg. 2014, 25, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Jacobo, O.M.; Giachero, V.E.; Hartwig, D.K.; Mantrana, G.A. Threedimensional printing modeling: Application in maxillofacial and hand fractures and resident training. Eur J Plast Surg. 2018, 41, 137–146. [Google Scholar] [CrossRef]
- Coffey-Zern, S.; Calvi, R.M.; Vorrasi, J.S.; Meara, D.J. Incorporating simulation into oral and maxillofacial surgery residency education and training: Christiana care’s method. J Oral Maxillofac Surg. 2015, 73, 1244–1245. [Google Scholar] [CrossRef]
- Milburn, J.A.; Khera, G.; Hornby, S.T.; Malone, P.S.C.; Fitzgerald, J.E.F. Introduction, availability and role of simulation in surgical education and training: Review of current evidence and recommendations from the association of surgeons in training. Int J Surg. 2012, 10, 393–398. [Google Scholar] [CrossRef]
- Zargaran, A.; Hirniak, J.; Zargaran, D. Oral and maxillofacial surgical simulation: Efficacy for medical students. Br J Oral Maxillofac Surg. 2020, 58, 1251–1254. [Google Scholar] [CrossRef]
- Meara, D.J.; Zern, S.C. Simulation in craniomaxillofacial training. Curr Opin Otolaryngol Head Neck Surg. 2016, 24, 376–380. [Google Scholar] [CrossRef]
- Christophel, J.J.; Park, S.S.; Nogan, S.J.; Essig, G.F. A facial trauma simulation course for evaluation and treatment of facial fractures. JAMA Facial Plastic Surgery. 2017, 19, 464–467. [Google Scholar] [CrossRef]
- Ahmed, N.; McVicar, I.H.; Mitchell, D.A. Simulation-based training in maxillofacial surgery: Are we going to be left behind? Br J Oral Maxillofac Surg 2019, 57, 67–71. [Google Scholar] [CrossRef]
- Shah, S.; Aydin, A.; Fisher, R.; Ahmed, K.; Froghi, S.; Dasgupta, P. Current status of simulation-based training tools in general surgery: A systematic review. International Journal of Surgery Open. 2021, 38, 100427. [Google Scholar] [CrossRef]
- Skertich, N.J.; Schimpke, S.W.; Lee, T.; et al. Pediatric surgery simulation-based training for the general surgery resident. J Surg Res. 2021, 258, 339–344. [Google Scholar] [CrossRef]
- Monje Gil, F.; Hernandez Vila, C.; Moyano Cuevas, J.L.; Lyra, M.; Pagador, J.B.; Sanchez Margallo, F.M. Validation of a simulator for temporomandibular joint arthroscopy. Int J Oral Maxillofac Surg. 2016, 45, 836–841. [Google Scholar] [CrossRef]
- Buckley, C.E.; Kavanagh, D.O.; Traynor, O.; Neary, P.C. Is the skillset obtained in surgical simulation transferable to the operating theatre? Am J Surg. 2014, 207, 146–157. [Google Scholar] [CrossRef]
- Werz, S.M.; Zeichner, S.J.; Berg, B.I.; Zeilhofer, H.F.; Thieringer, F. 3D printed surgical simulation models as educational tool by maxillofacial surgeons. Eur J Dent Educ. 2018, 22, e500–e505. [Google Scholar] [CrossRef] [PubMed]
- Elledge, R.; Speculand, B.; Green, J.; Attard, A. Training in surgery of the temporomandibular joint: Perceptions of trainees in oral and maxillofacial surgery in the United Kingdom. Br J Oral Maxillofac Surg. 2016, 54, 941–945. [Google Scholar] [CrossRef]
- Bertin, H.; Huon, J.F.; Praud, M.; et al. Bilateral sagittal split osteotomy training on mandibular 3-dimensional printed models for maxillofacial surgical residents. Br J Oral Maxillofac Surg. 2020, 58, 953–958. [Google Scholar] [CrossRef]
- Farnworth, L.R.; Lemay, D.E.; Wooldridge, T. A comparison of operative times in arthroscopic ACL reconstruction between orthopaedic faculty and residents: the financial impact of orthopaedic surgical training in the operating room. Iowa Orthop J. 2001, 21, 31–35. [Google Scholar]
- Deutsch, E.S.; Wiet, G.J.; Seidman, M.; et al. Simulation activity in otolaryngology residencies. Otolaryngol Head Neck Surg 2015, 153, 193–201. [Google Scholar] [CrossRef]
- Naples, R.; French, J.C.; Han, A.Y.; Lipman, J.M.; Awad, M.M. The impact of simulation training on operative performance in general surgery: Lessons learned from a prospective randomized trial. J Surg Res. 2022, 270, 513–521. [Google Scholar] [CrossRef]
- Navia, A.; Tejos, R.; Canahuate, S.; et al. MicrosimUC: Validation of a low-cost, portable, do-it-yourself microsurgery training kit. J Reconstr Microsurg. 2022, 38, 409–419. [Google Scholar] [CrossRef]
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).