Abstract
Study design: Retrospective case series. Objective: Alloplastic temporomandibular joint replacement has been established as a standard technique for end- stage temporomandibular (TMJ) pathologies. Joint replacement when there are extensive mandibular defects remains a challenging clinical problem. Custom-made extended temporomandibular joint replacement is a feasible option but there is limited information about this emerging technique. Methods: Included were all patients undergoing extended TMJ-replacements (TMJe), all operatrions were carried out by the senior author. Surgical technique was either single stage or two stage protocol. Surgical details and pitfalls and outcome of more than 2 years follow-up with reference to thirteen including twelve patients were recorded. Results: The most common diagnosis was ameloblastoma of the mandibular ramus. Single stage or two stagge regime were carried out depending on resection requirements and involvement of teeth. Improved mouth opening of more than 30mm was achieved in 10 of 12 patients. One patient with previous TMJ replacement reported temporary weakness of the facial nerve, which resolved after 10 months. Conclusions: The authors suggest a simplified anatomically based single-stage or two-stage regime, with both regimes achieved excellent anatomic reconstruction, facial appearance and function with low surgical morbidity. Custom-made extended temporomandibular joint protheses appear an advanced and reliable solution for reconstruction of combined complex mandibular defects including the temporomandibular joint. If surgical clearance of the pathology can be achieved, a single-stage regime is favoured.
Introduction
Alloplastic temporomandibular joint replacement has become a safe and standard technique for a range of end-stage diseases of the temporomandibular joint. In the UK, guidelines for the indication of joint replacement surgery are available [1]. Excellent functional long-term results can be achieved with regards to pain and function [2,3]. However, management of the joint in ablative surgery remains controversial with currently no standardized approach.
Results are highly variable, and a broad range of complications has been described [4] Free tissue transfer [5,6,7] may be combined with an alloplastic joint prosthesis [8] or autologous techniques chosen, using the fibular head [9] or the second metatarsal for TMJ-reconstruction [10].
Advantages for the usage of free tissue transfer remain availability, good biocompatibility and adaptability as the graft can be fashioned according to the requirements. In contrast, the second donor side extends surgical time and risks. Bone healing requires rigid fixation with IMF, which delays physical therapy [11].
Alloplastic joint replacement does not require a donor side. Involving large mandibular defects custom-made implants that conform the exact anatomic situation are required and require some time for manufacturing. Current studies show alloplastic TMJ replacement devices have a lifespan of at least ten to 20 years [12,13,14]. Postoperative joint infection is reported to be low, estimated between 1.5 to 2.7%. Meticulous measures to prevent and detect infections are paramount [15].
A specific classification system for extended total temporomandibular replacements was recently suggested by Elledge et al. [16]. It includes a fossa component from F0 to F5 and a condyle/mandible component from M0 to M4 according to the extent of the defect.
Very few reports and studies are available in the literature. The biggest case series to date includes four cases by Westermark and his team, who reported good results in Goldenhar syndrome and hemifacial microsomia [17] and five cases in a very recent publication by Mommaerts et al. [18].
Here, the authors report of thirteen extended temporomandibular joint replacements (TMJe) conducted on twelve patients with at least 2 year follow-up. Our aims of this case series with retrospective follow-up are to report our experience and observations on this surgery as well as difficulties and complications, which may help to guide future surgeries to prevent pitfalls.
Patients and Methods
All operations were carried out by the same surgeon (LC). Data was extracted from the records including age, gender, diagnosis, Elledge classification, operative details, complications, postoperative mouth opening and follow-up (see Table 1). Written consent for publication of clinical photographs was obtained. Ethical approval for the retrospective data collection was not required. The audit project was registered on the Trust database with the project number 12166.

Table 1.
Case series: Clinical and treatment detail.
Resection was carried out either with simultaneous insertion of TMJe (single-stage regime) from an extraoral approach, or in 2 operations with the resection of the pathology from intraoral in an initial operation, and subsequent insertion of TMJe in a second operation.
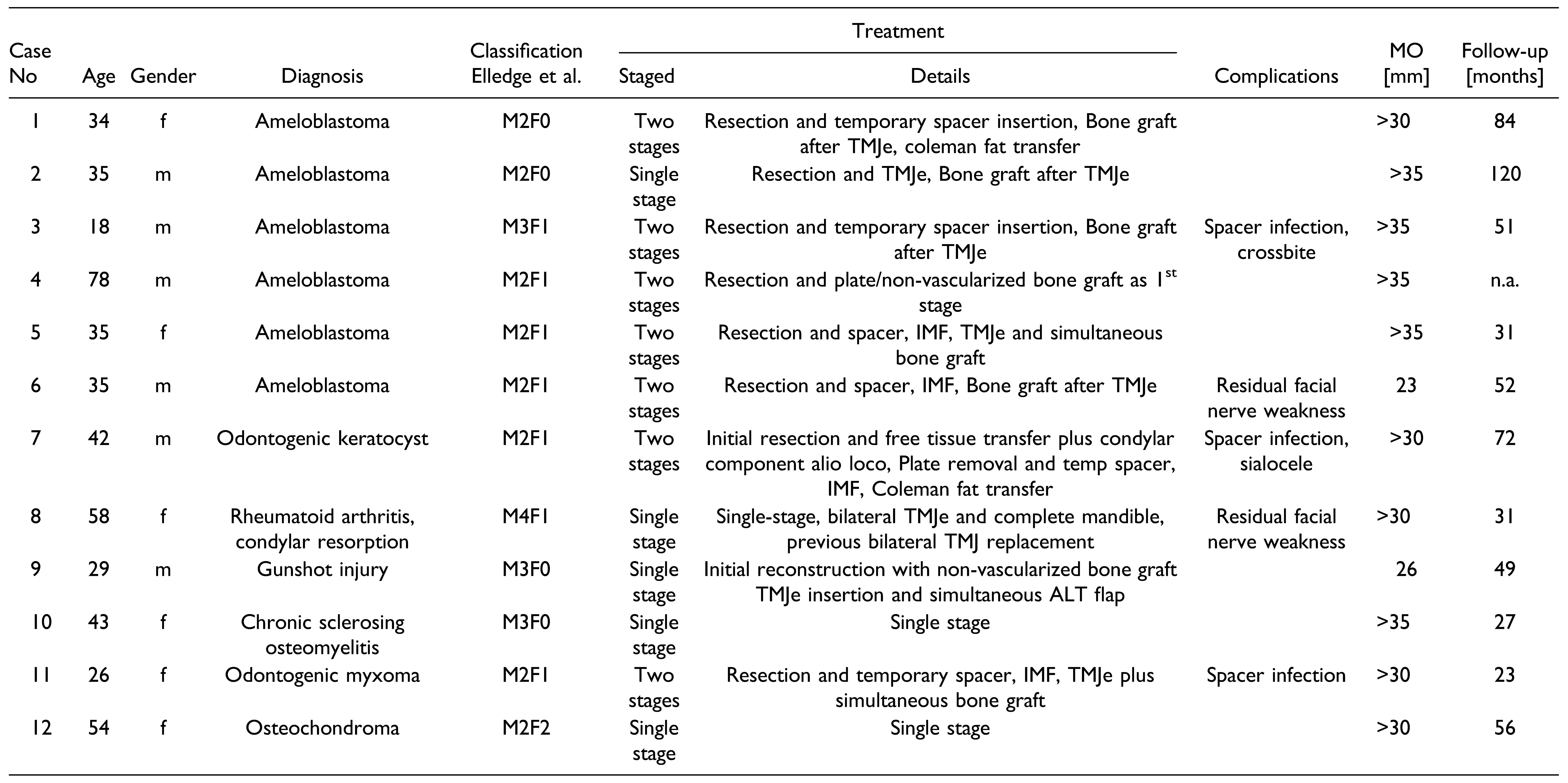
In case of a two-stage regime an intraoperative manufactory of a spacer was carried out. In this case, resection was conducted via an intraoral approach leaving the pre- auricular soft tissue untouched for later reconstructive surgery. Preoperatively, a sterilized silicon casting mould using a mirrored 3D-printed model of the mandible was produced (see Figure 1, Figure 2, Figure 3 and Figure 4). This facilitated the intraoperative manufacturing of a spacer using bone cement (BonOs®, Ostartis, Dieburg, Germany). The spacer was fixed using osteosynthesis.
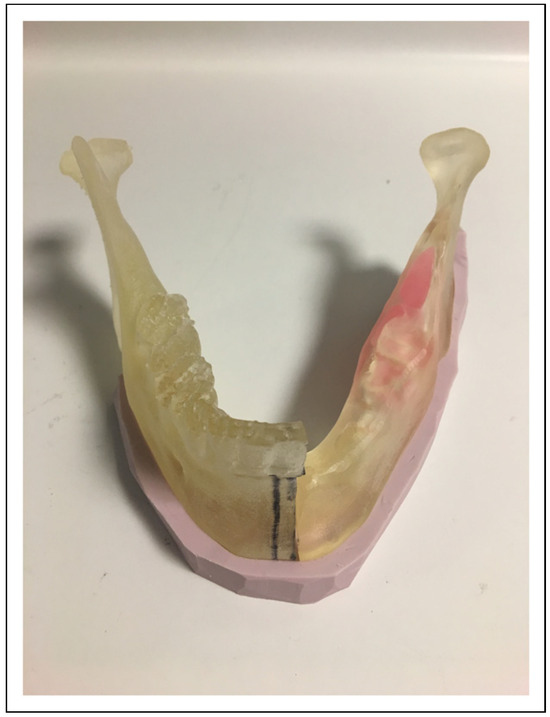
Figure 1.
A 3D-printed model was produced mirroring the unaffected side.

Figure 2.
Silicon impression material was used to manufacture a casting mould. An opening was designed for the nozzle to insert BonOs® using the application device.
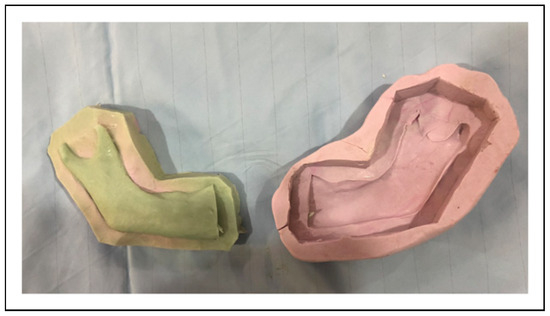
Figure 3.
Intraoperative Manufacturing of temporary spacer, sterilized casting mould is filled with BonOs®.

Figure 4.
The temporary spacer coming off the casting mould and the spacer after fine adjustment, ready for insertion and fixation with Osteosynthesis.
After confirmation of pathology and sufficient margins, the final design of the TMJe was confirmed and produced.
In both protocols, insertion of the TMJe was carried out via extraoral approach (see Figure 5, Figure 6, Figure 7 and Figure 8). The custom-made prostheses for extended TMJ replacement used for the patients were manufactured from either TMJ Concepts (www.tmjconcepts.com, Ventura, CA) or Zimmer Biomet (zimmerbiomet.com, Warsaw, IN).
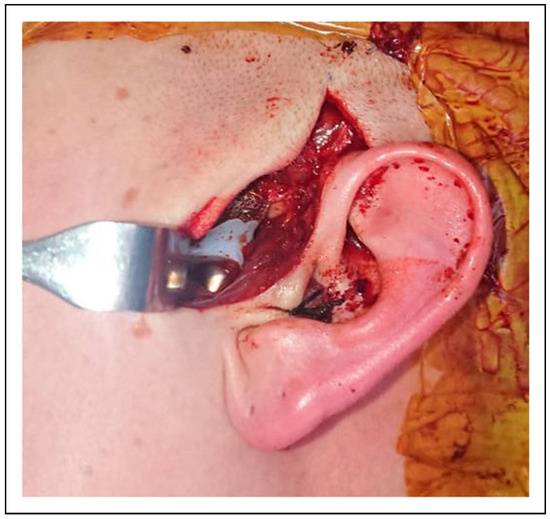
Figure 5.
Insertion of TMJe is carried out via a small preauricular incision.
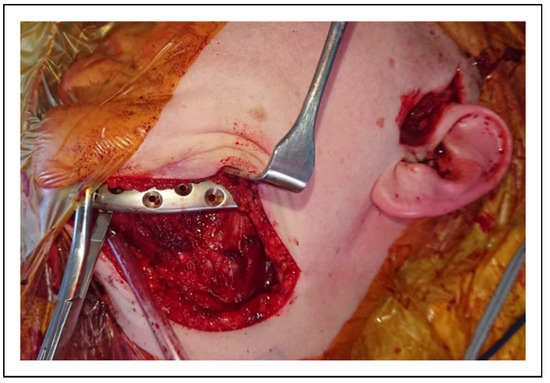
Figure 6.
A second small submandibular incision is made for fixation of the mandibular component. In case of a single-stage management, the resection of the pathology is carried out from extraoral without breaching the intraoral mucosa. In a two-stage protocol, resection and spacer insertion are carried out via intraoral approach, for removal of spacer and insertion of TMJe an extraoral approach is used.
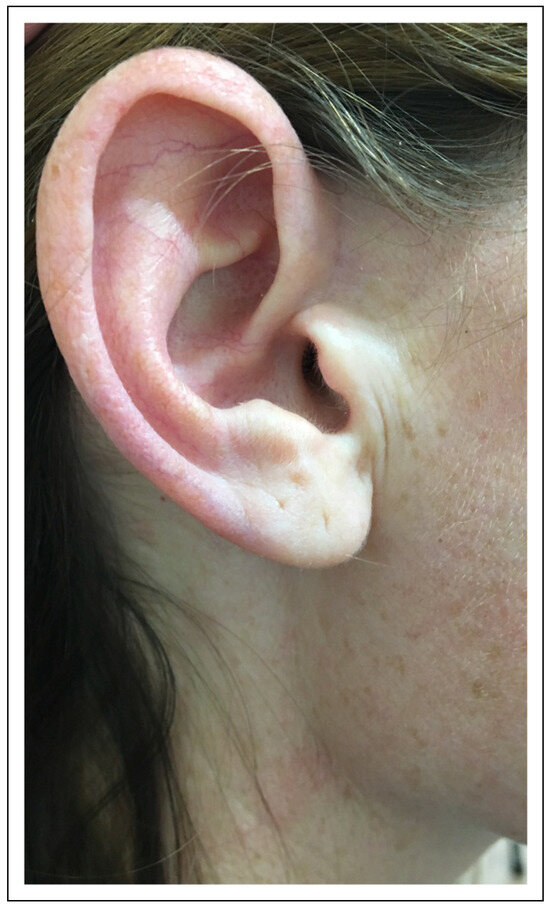
Figure 7.
Healing usually shows minimal visible scarring preauricular.

Figure 8.
The incision on the chin if needed, a skin crease may be used to leave an inconspicuous scar.
All patients were followed up at least for 2 years to date. No recurrence of the initial pathology was observed
Results
The group comprised six male and six female patients, with an average age of 40.6 years.
The most common diagnosis for unilateral TMJe replacement included ameloblastoma of the mandibular ramus in six patients. Further diagnoses included gunshot injury, odontogenic keratocyst, odontogenic myxoma chronic sclerosing osteomyelitis and osteochondroma (see Table 1). One patient underwent bilateral TMJe replacement with complete mandibular replacement for failing metal-work and extensive bone resorption following a previous temporomandibular joint replacement.
Seven patients were treated using the two-stage regime. Five patients received the TMJe at the time of resection (single-stage regime).
Non-vascularized bone graft for dental rehabilitation was carried out in five cases, of which 2 were carried out at the time of TMJe insertion. Two patients underwent Coleman fat transfer for contour optimization at a later stage.
Mouth opening of more than 30 mm was achieved except in 2 cases. One patient reported temporary weakness of facial muscles after bilateral TMJe M4F1 following reoperation after a previous bilateral TMJ replacement. After 10 months it had largely resolved.
Case Examples
- Two-stage regime with simultaneous bone graft, patient 5
A 35-year-old female presented with an extensive ameloblastoma in the right mandible (Figure 9 and Figure 10). The resection resulted in an M2F1 defect (Figure 11), and a spacer was inserted from an intraoral approach. Tight elastics and an NG tube were inserted. The second stage was carried via an extraoral approach for insertion of the TMJe and simultaneous bone graft (Figure 12). The patient is disease free and did not require further corrective surgery with good cosmesis (Figure 13 and Figure 14) and mouth opening (Figure 15).

Figure 9.
OPG of a patient 5 with a right mandibular ameloblastoma.

Figure 10.
Patient 5, 3D CT reconstruction of the right ramus shows the extend of the lesion.

Figure 11.
Patient 5, Intraoperative specimen of the right ramus including condylar head from an intraoperative approach. Insertion of spacer in the same operation was carried out. Postoperatively tight IMF was applied, and an NG tube was inserted.
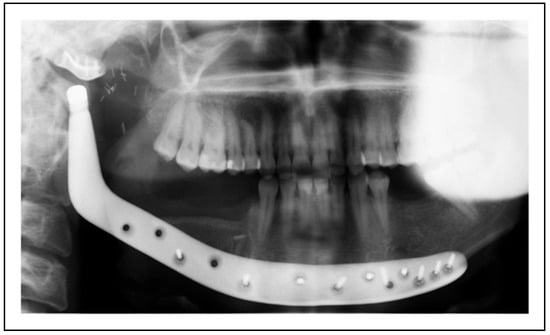
Figure 12.
Patient 5: Postoperative OPG after removal of the spacer and insertion of the TMJe with simultaneous bone graft.
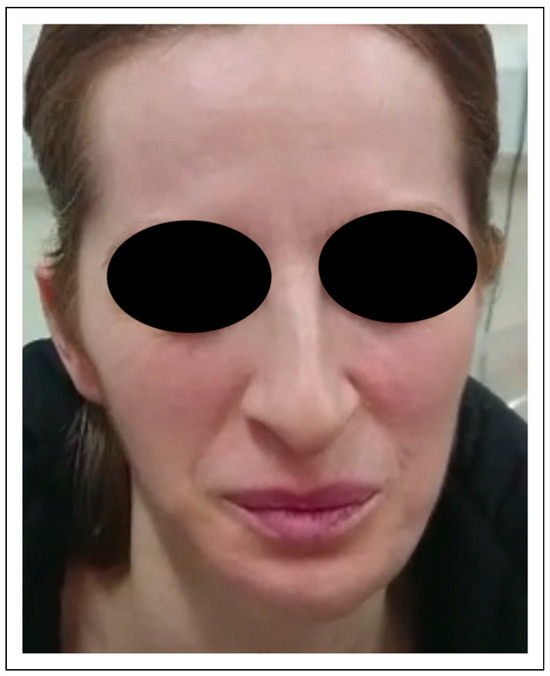
Figure 13.
Facial view 3 months postoperatively, the patient showed good facial symmetry.
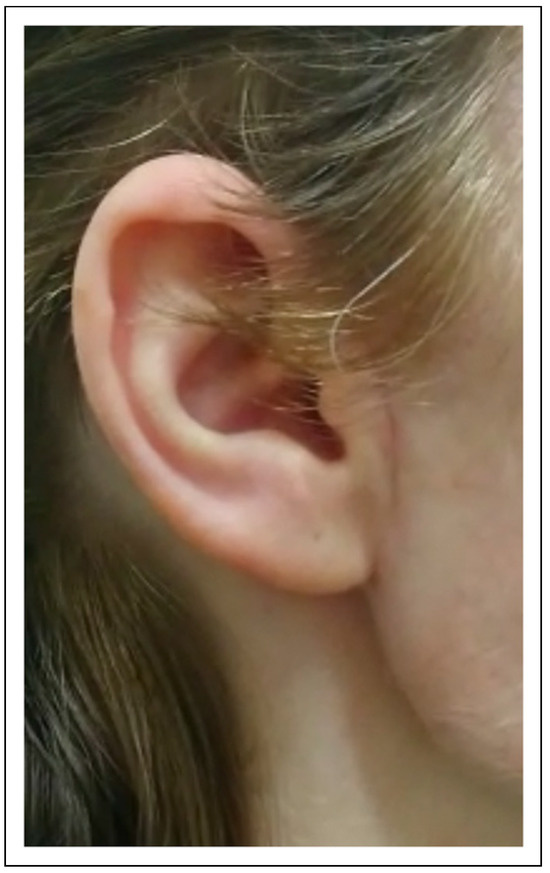
Figure 14.
Patient 5 right preauricular area with a minimally visible scar.
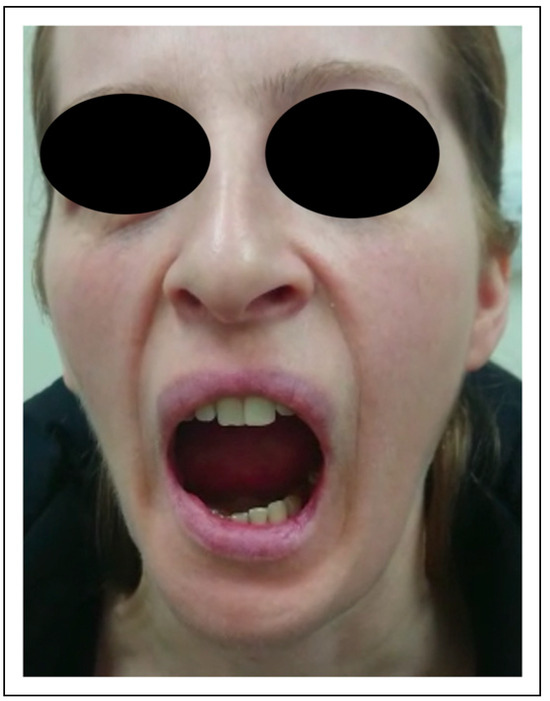
Figure 15.
Patient 5 with unrestricted mouth opening.
Two-Stage Regime, Patient 1
A 34-year-old female patient had previously undergone enucleation for Ameloblastoma elsewhere. She presented with an extensive recurrence in the left mandible including the ramus (Figure 16). The resection was undertaken from intraoral, with a second stage for custom-made TMJe for M2F0 defect (Figure 17). Postoperative OPG (Figure 18) and 3D CT (Figure 19) show the TMJe in situ with good occlusion. The patient underwent further bone graft and coleman fat transfer and the result shows good facial symmetry (Figure 20, Figure 21 and Figure 22) and good mouth opening without deviation (Figure 23).

Figure 16.
Patient 1 was referred with recurrence of an ameloblastoma of the left mandible. The patient had previously undergone enucleation.
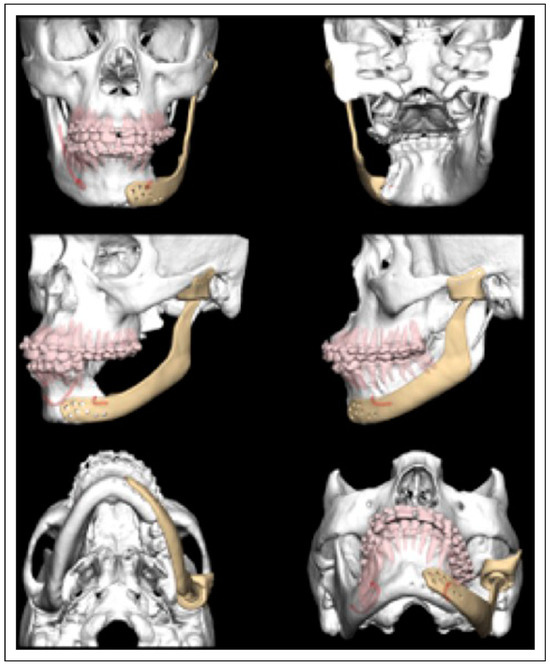
Figure 17.
Patient 1, preoperative planning for insertion of the TMJe.
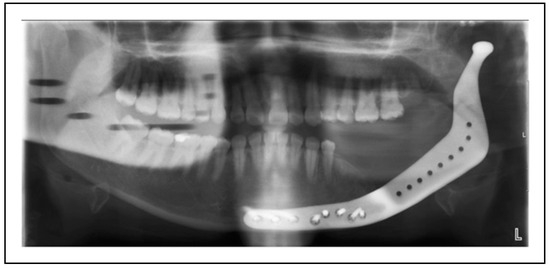
Figure 18.
Patient1, postoperative OPG of the TMJe for the left mandibular ramus and TMJ.

Figure 19.
3D CT reconstruction of Patient 1.

Figure 20.
Patient 1, the postoperative facial view shows good symmetry of the contour and facial soft tissues.

Figure 21.
Patient 1, facial profile.
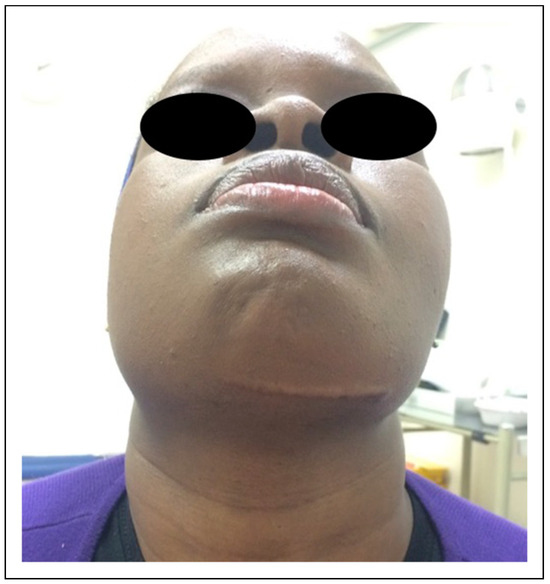
Figure 22.
Patient 1, view from below shows good symmetry.
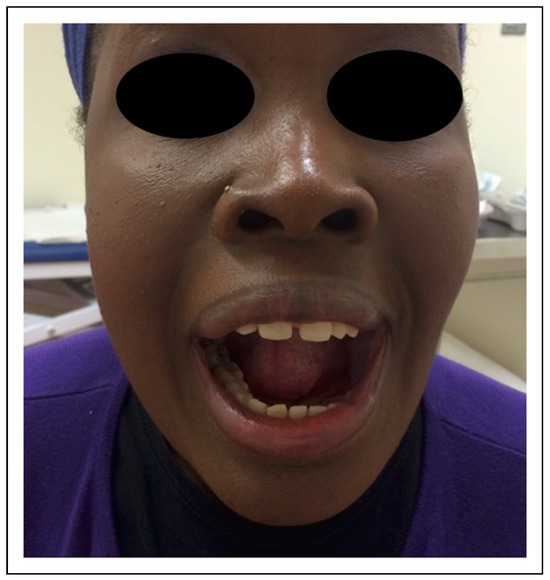
Figure 23.
Patient 1: Good mouth opening without deviation postoperatively.
Single-Stage Regime, Patient 10
A forty-three-year-old female was treated for long-term chronic sclerosing osteomyelitis in the left mandible with wide excision (M3F0) from extraoral. No teeth were involved in the resection area (Figure 24). Therefore, a single-stage regime using an extraoral approach was chosen. Surgery achieved good mouth opening and good occlusion (Figure 25, Figure 26 and Figure 27).
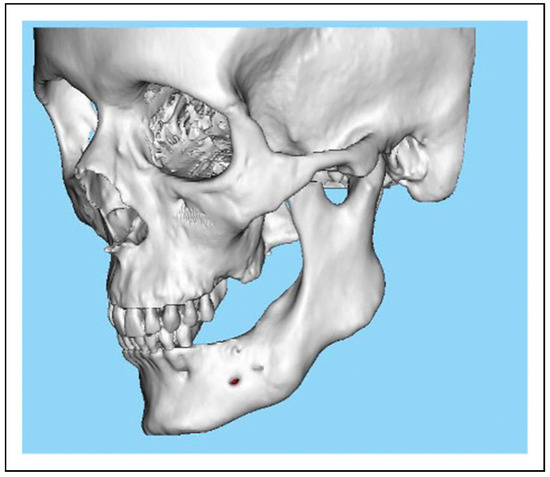
Figure 24.
Patient 10. TMJe for chronic sclerosing osteomyelitis of the left mandible. The patient was edentulous in the area of resection. Therefore, a single-stage treatment was favoured.
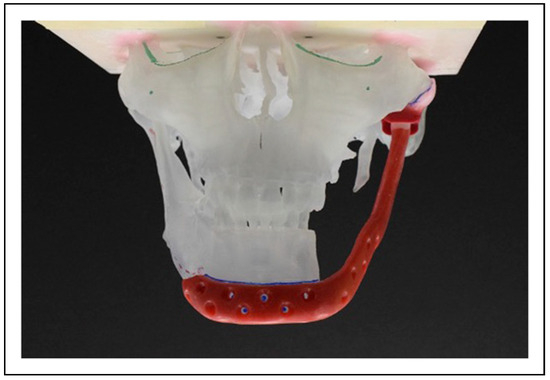
Figure 25.
The planning included a M3F0 TMJe for replacement of the left TMJ and ramus and body of the left side.
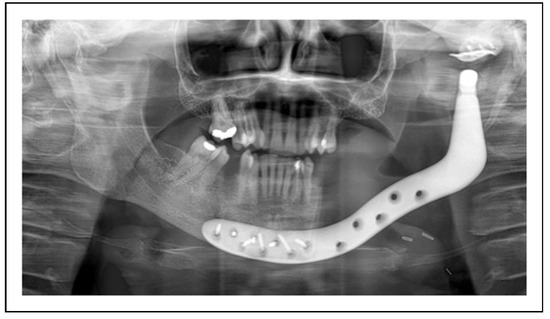
Figure 26.
Patient 10. Postoperative orthopantomogram.

Figure 27.
Patient 10. PA view of the postoperative TMJe.
Bilateral TMJ Replacement With Complete Replacement of the Mandible, Patient 8
A 58-year-old female was referred for treatment of end- stage failure of bilateral temporomandibular joint (TMJ) replacements. The patient had, some 30 years previously, undergone a bilateral sagittal split osteotomy and genioplasty, but within 2 years had presumed ischaemic necrosis of both proximal segments. Bilateral stock prostheses were secured by a combination of screws and circumferential wiring, but there was progressive necrosis of the remaining bone, and loosening of the metalwork. Her symptoms included pain, reduced mouth opening and intercurrent infections. Her further past medical history included rheumatoid arthritis (Figure 28).

Figure 28.
Patient 8. Orthopantomogram of the preoperative situation. Long-term rheumatoid arthritis and failing bilateral TMJ.
3D scanning and modelling was undertaken (Figure 29 and Figure 30), some of the exposed metalwork was removed 2 weeks before definitive surgery, and intraoral wounds closed, and allowed to heal. The patient underwent simultaneous removal of the failing bilateral prostheses (Figure 31Figure 32Figure 33Figure 34 and Figure 35), and a one-piece custom-made bilateral TMJ replacement with an extended component for total alloplastic mandibular replacement (Biomed, zimmerbiomet.com, Warsaw, IN, Figure 32) was placed.
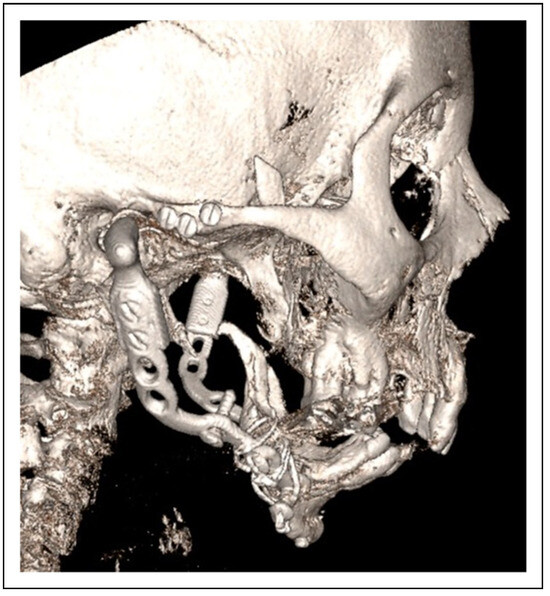
Figure 29.
Patient 8: Preoperative CT-3D reconstruction of the clinical situation showing the metal work failure and resorption of the mandible.
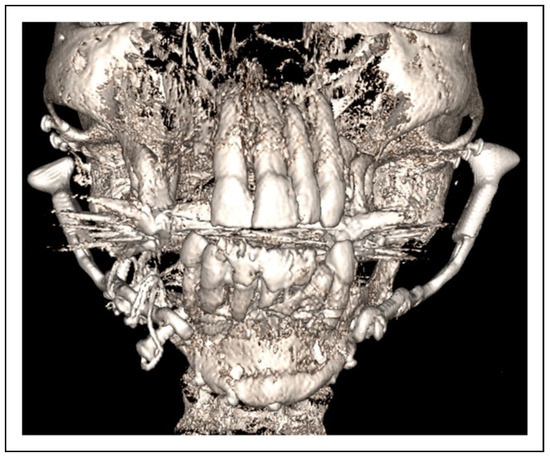
Figure 30.
Patient 8: Coronal view of 3D CT. Only a small part of the anterior mandible was left and planned to be integrated into the TMJe.

Figure 31.
Patient 8. The approach was carried out via the previous incision. Of note the retruded chin before resection of the TMJ.

Figure 32.
Patient 8: The TMJe for bilateral TMJ replacement and the complete mandible.
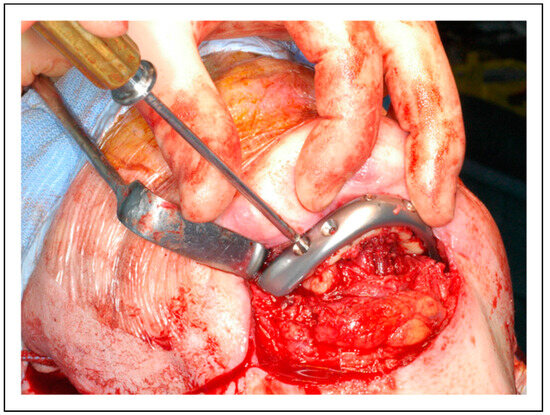
Figure 33.
Patient 8: The design included screw holes in the anterior aspect to integrate the remaining bone of the chin including the lower incisors.
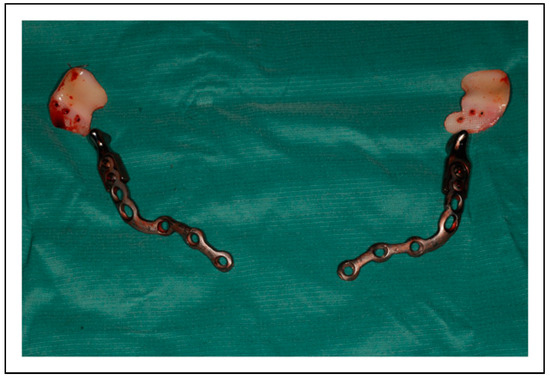
Figure 34.
Patient 8. The resected metalwork from the previous TMJ replacement.

Figure 35.
Patient8. The immediate postoperative view shows a significantly improved facial profile.
Her immediate postoperative progress was satisfactory (Figure 36), and she was discharged on day six. The patient remains pain-free 18 months post-op, with interincisal opening of greater than 30 mm, and has a stable, albeit only anterior, occlusion. A significant right-sided facial nerve weakness resolved over some months.
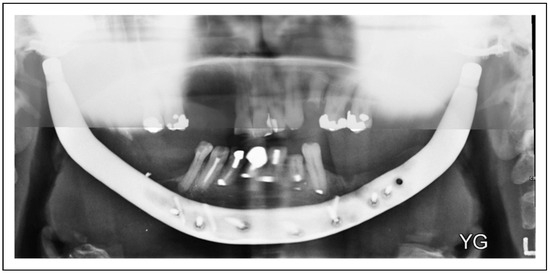
Figure 36.
Patient 8. Postoperative Orthopantomogram of the custom-made device spanning the complete mandible and including both temporomandibular joints.
Discussion
This case series includes thirteen custom-made extended temporomandibular joint replacements in twelve patients, and is, to the best of our knowledge, the largest case series to date. A single-stage protocol and a two-stage protocol are now considered in treatment planning. Factors crucial to the choice of protocol are the underlying pathology and extent of the lesion, and the need for confirmation of completeness of the resection prior to insertion of the prothesis. In the case of a benign pathology achievement of surgical clearance of the pathology, the authors favour a single-stage protocol.
If histopathological clearance of the disease is required, the area of the resection requires a temporary reconstruction. The authors used an intraoral approach and a two-stage protocol. A temporary joint replacement with a BonOs® spacer was carried out at the time of resection, preserving height and space for the TMJe. The authors observed some extended healing time, which required intermaxillary fixation for up to 3 months. Case reports using a custom 3D temporary spacer in 2 stage repair have also been described in the literature [19]. Alternatively, a temporary titanium plate could be considered. But this could lead to shrinkage of the surrounding soft tissue and could make future transplant more challenging. However, risks of fluid collection, intraoral breakdown and infection remain. Untimely removal of the spacer may lead to collapse of tissue space, which complicates the insertion of TMJe, and may raise the risks of a facial nerve injury.
For satisfactory functional and aesthetic reconstruction of mandibular defects including the temporomandibular joint, several aspects must be addressed. Firstly, the complete resection of the underlying pathology and, secondly, the reconstruction of the continuity of the mandible including lost teeth as well as the long-term function of the joint.
In cases with no involvement of significant amounts of the mandible, standard temporomandibular joint replacement is a well-established and standardized treatment [1,3,13]. Long-term results from Westermark and colleagues on 111 patients over 20 years demonstrated improvements in several parameters, pain, jaw function, diet score, incisal opening and quality of life. They did not report the need for device replacement due to material failure [14].
Reconstructive solutions using free tissue transfer are well established, and good and stable results are reported. However, disadvantages include donor side morbidity and long reconstructive surgery; longer hospital stays and potential failure of reconstruction need mentioning. Options for autologous joint reconstruction include using the head of the fibula, rigid fixation of the condylar head or no reconstruction. Long-term complications may include joint instability, bone height loss or ankylosis [9,20].
However, the combination of mandibular pathologies extending into the condyle, requiring resection of the condylar head adds several problems that must be addressed. No standardized protocol has become available to date. This may be due to the relatively low number of cases, difficulty with regards to time for planning, and availability and costs of devices.
Further consideration needs to be addressed with regards to good viable soft tissue cover, when inserting large alloplastic mandibular implants, as a larger surface may lead to a higher chance of infection long term. Previous radiation therapy should be considered critical, when planning these cases [17]. Addressing a significant soft tissue defect successfully using combined free tissue transfer has been reported previously [17]. Weight and length of the device may contribute to wear and potential device fracture long-term, which has not been observed in this series. Vertical suspension of the pterygomasseteric sling is recommended using 2-0 PDS to support the mandible until scar formation has occurred.
Another important consideration is allergy or hypersensitivity to the metals in joint prosthesis, with nickel, cobalt and chromium being the most common sensitizing metals, which may lead to premature removal of the device [21]. Hypersensitivity in temporomandibular joint replacement is observed significantly more frequently in metal-on-metal prostheses than metal-on-UMWPE [22].
Vega et Meara suggested a classification based on the time in which the reconstruction is going to be performed [23].
Based on the experience of the presented case series, and in addition to the above classification system, which is based exclusively on the timing of the repair, the authors suggest a simplified algorithm for reconstruction, that additionally takes involved tissues into account and offers an anatomically based treatment algorithm for decision making (Figure 37).
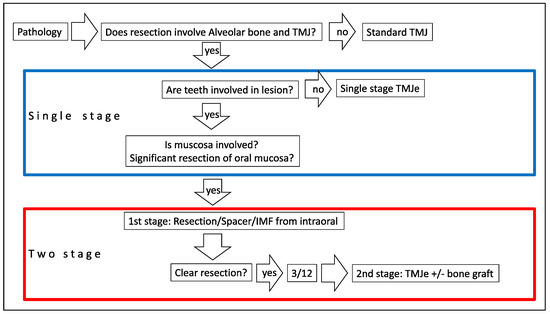
Figure 37.
Treatment algorithm for single-stage or two-stage TMJe.
Single-Stage Procedure
If a complete resection with sufficient margins can be safely achieved, a single-stage protocol is favoured. The extraoral approach allows resection of the pathology and insertion of the TMJe. The device can be designed to the anticipated extent of resection. The planning should also include options for osteosynthesis, if a simultaneous bone graft is planned.
Two-Stage Procedure
Pathologies involving teeth or periodontal tissues or mucosa, should be addressed in 2 stages. Initially, resection of the pathology including teeth and mucosa should be carried out from an intraoral approach. It may be combined with a small preauricular incision, if required. Using a temporary spacer following resection allows confirmation of the final histopathological diagnosis and resection margins. The anatomic space for the implant is maintained and allows function and height of the mandible.
The authors use tight intermaxillary fixation for up to 3 months and liquid diet to allow intraoral healing. The extraoral tissues can be kept untouched for the second operation, when the spacer is taken out extraorally and the TMJe inserted. The pterygomasseteric sling is fixed on the device. When designing the prosthesis, planning should include further drill holes applied to the body and angle region. The authors initially carried out the block bone graft as a secondary procedure. Advancing this new technique to the next level in recent cases, a non-vascularized bone graft was carried out at the time of TMJe insertion. This allows earlier dental rehabilitation and reduces risk of infection of the implant and facial nerve injury by eliminating a second procedure.
The Authors Recommend
- If a spacer is used, it should be designed slightly smaller than the original mandible.
- Application of tight intermaxillary fixation at this stage for up to 3 months.
- Strict avoidance of solid, or insertion of a nasogastric tube may be considered.
- If pathology allows management as single stage is favoured.
- If dental rehabilitation is planned, simultaneous bone grafting at the time of TMJe insertion is recom- mended and should be considered in the planning of the device.
Conclusion
Extended temporomandibular joint replacement (TMJe) is a safe and reliable technique for reconstruction of combined complex defects involving the mandible and the tempo- romandibular joint. Careful case selection, meticulous planning and surgical technique are paramount.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval
This retrospective audit project was registered on the Trust da- tabase with the project number 12166 from Guy`s and St Thomas NHS Foundation Trust.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Sidebottom, A.J.; surgeons, U.T.r.; Maxillofacial, S.; British Association of O. Guidelines for the replacement of temporomandibular joints in the United Kingdom. Br. J. Oral Maxillofac. Surg. 2008, 46, 146–147. [Google Scholar] [CrossRef] [PubMed]
- Mercuri, L.G.; Wolford, L.M.; Sanders, B.; White, R.D.; Hurder, A.; Henderson, W. Custom CAD/CAM total temporomandibular joint reconstruction system: Preliminary multicenter report. J. Oral Maxillofac. Surg. 1995, 53, 106–115, discussion 15-6. [Google Scholar] [CrossRef] [PubMed]
- Mercuri, L.G. Subjective and objective outcomes in patients reconstructed with a custom-fitted alloplastic temporomandibular joint prosthesis. J. Oral Maxillofac. Surg. 1999, 57, 1427–1430. [Google Scholar] [CrossRef]
- Bredell, M.; Gratz, K.; Obwegeser, J.; Gujer, A.K. Management of the temporomandibular joint after ablative surgery. Craniomaxillofac. Trauma. Reconstr. 2014, 7, 271–279. [Google Scholar] [CrossRef]
- Hidalgo, D.A. Fibula free flap: A new method of mandible reconstruction. Plast. Reconstr. Surg. 1989, 84, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Disa, J.J.; Cordeiro, P.G. Mandible reconstruction with microvascular surgery. Semin. Surg. Oncol. 2000, 19, 226–234. [Google Scholar] [CrossRef]
- Petrovic, I.; Baser, R.; Blackwell, T.; et al. Long-Term Functional and Esthetic Outcomes after Fibula Free Flap Reconstruction of the Mandible; Head & Neck: Hoboken, NJ, USA, 2019. [Google Scholar]
- Zaid, W.Y.; Alshehry, S.; Zakhary, G.; Yampolsky, A.; Kim, B. Use of Vascularized myo-osseous fibula free flap to reconstruct a hemimandibular defect with a concomitant skull defect arising from stock condylar prosthesis displacement into the middle cranial fossa. J. Oral Maxillofac. Surg. 2018, 77, 1316.e1–1316.e12. [Google Scholar] [CrossRef]
- Chao, J.W.; Rohde, C.H.; Chang, M.M.; Kutler, D.I.; Friedman, J.; Spector, J.A. Oral rehabilitation outcomes after free fibula reconstruction of the mandible without condylar restoration. J. Craniofac. Surg. 2014, 25, 415–417. [Google Scholar] [CrossRef]
- Taristano, A.; Battaglia, S.; Ramieri, V. , et al. Short-term outcomes of mandibular reconstruction in oncological patients using a CAD/CAM prosthesis including a condyle supporting a fibular free flap. J. Cranio-Maxillo-Fac. Surg. 2017, 45, 330–337. [Google Scholar] [CrossRef]
- Mercuri, L.G. Costochondral graft versus total alloplastic joint for temporomandibular joint reconstruction. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 335–342. [Google Scholar] [CrossRef]
- Mercuri, L.G.; Edibam, N.R.; Giobbie-Hurder, A. Fourteen-year follow-up of a patient-fitted total temporomandibular joint reconstruction system. J. Oral Maxillofac. Surg. 2007, 65, 1140–1148. [Google Scholar] [PubMed]
- Leandro, L.F.; Ono, H.Y.; Loureiro, C.C.; Marinho, K.; Guevara, H.A. A ten-year experience and follow-up of three hundred patients fitted with the Biomet/Lorenz Microfixation TMJ replacement system. Int. J. Oral Maxillofac. Surg. 2013, 42, 1007–1013. [Google Scholar] [PubMed]
- Wolford, L.M.; Mercuri, L.G.; Schneiderman, E.D.; Movahed, R.; Allen, W. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: The Technedica/TMJ Concepts device. J. Oral Maxillofac. Surg. 2015, 73, 952–960. [Google Scholar]
- Mercuri, L.G. Prevention and detection of prosthetic temporomandibular joint infections-update. Int. J. Oral Maxillofac. Surg. 2019, 48, 217–224. [Google Scholar]
- Elledge, R.; Mercuri, L.G.; Speculand, B. Extended total temporomandibular joint replacements: A classification system. Br. J. Oral Maxillofac. Surg. 2018, 56, 578–581. [Google Scholar] [CrossRef]
- Westermark, A.; Heden, P.; Aagaard, E.; Cornelius, C.P. The use of TMJ Concepts prostheses to reconstruct patients with major temporomandibular joint and mandibular defects. Int. J. Oral Maxillofac. Surg. 2011, 40, 487–496. [Google Scholar] [PubMed]
- Mommaerts, M.Y.N.I.; Dorobantu, M.; De Meurechy, N. Extended total temporomandibular joint replacement with occlusal adjustments: Pitfalls, patient-reported outcomes, subclassification, and a new paradigm. Ann. Maxillofac. Surg. 2020, 10, 73–79. [Google Scholar]
- Green, J.M., 3rd; Lawson, S.T.; Liacouras, P.C.; Wise, E.M.; Gentile, M.A.; Grant, G.T. Custom anatomical 3D spacer for temporomandibular joint resection and reconstruction. Craniomaxillofac. Trauma. Reconstr. 2016, 9, 82–87. [Google Scholar]
- Gonzalez-Garcia, R.; Naval-Gias, L.; Rodriguez-Campo, F.J.; Martinez-Chacon, J.L.; Gil-Diez Usandizaaga, J.L. Vascularized fibular flap for reconstruction of the condyle after mandibular ablation. J. Oral Maxillofac. Surg. 2008, 66, 1133–1137. [Google Scholar]
- Merritt, K.; Brown, S.A. Distribution of cobalt chromium wear and corrosion products and biologic reactions. Clin. Orthop. Relat. Res. 1996, 329 (Supp 1), S233–S243. [Google Scholar]
- Wolford, L.M. Factors to consider in joint prosthesis systems. Bayl. Univ. Med. Cent. Proc. 2006, 19, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Vega, L.a.M.D. Mandibular Replacement Utilizing TMJ TJR Devices. In Temporomandibular Joint Total Joint Replacement—TMJ TJR; Mercuri, L.G., Ed.; Springer: Cham/Heidelberg, New York, Dordrecht, London, 2016. [Google Scholar]
© 2022 by the authors. Multimed Inc.