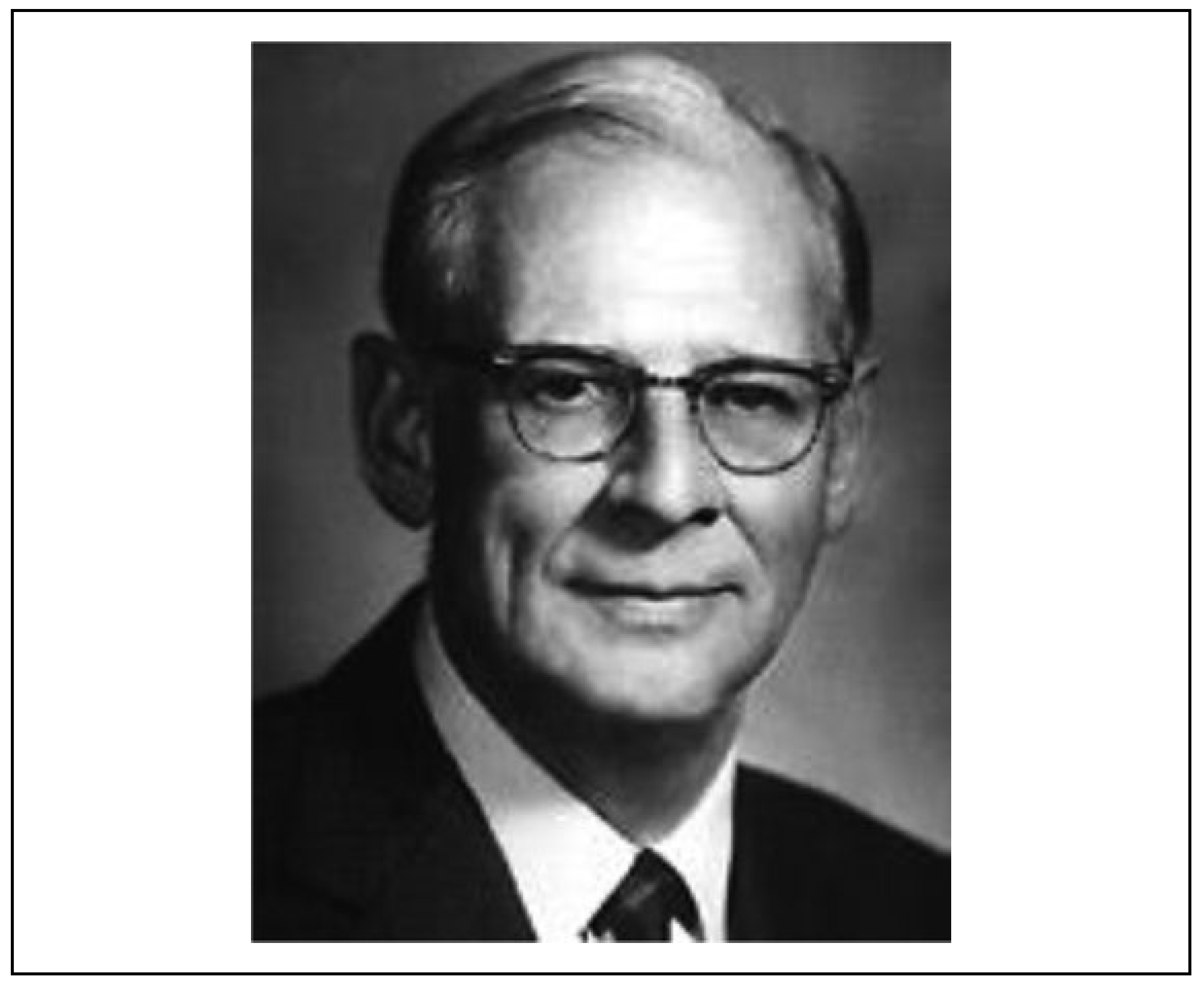
Resolution of Vertical Gaze Following a Delayed Presentation of Orbital Floor Fracture With Inferior Rectus Entrapment: The Contributions of Charles E. Iliff and Joseph S. Gruss in Orbital Surgery
Abstract
:Introduction
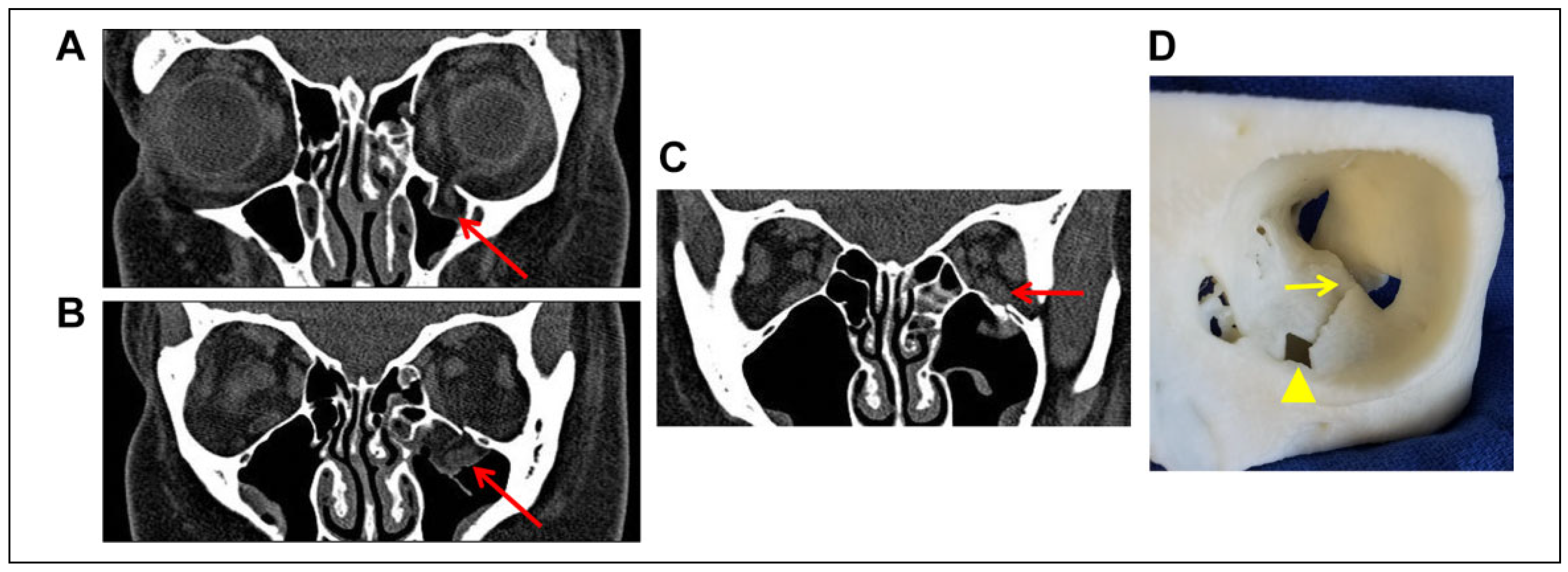
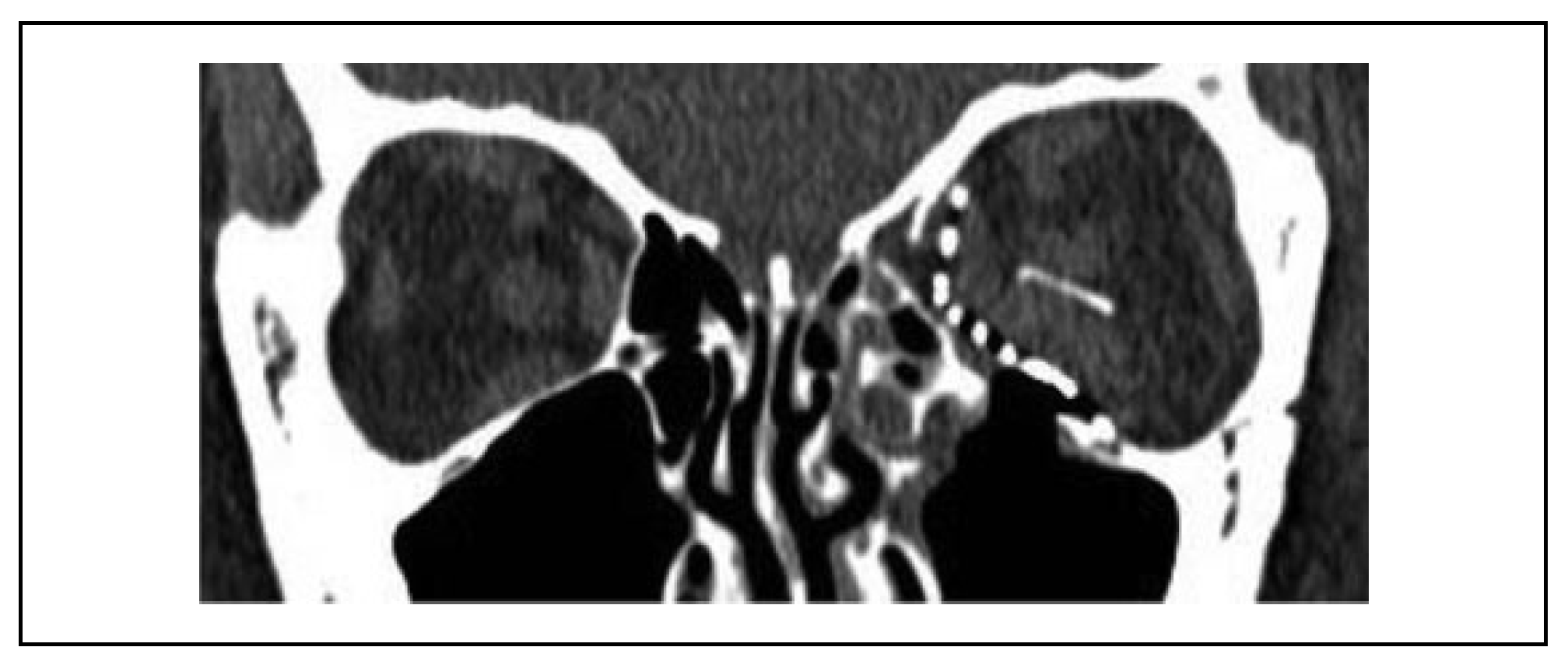
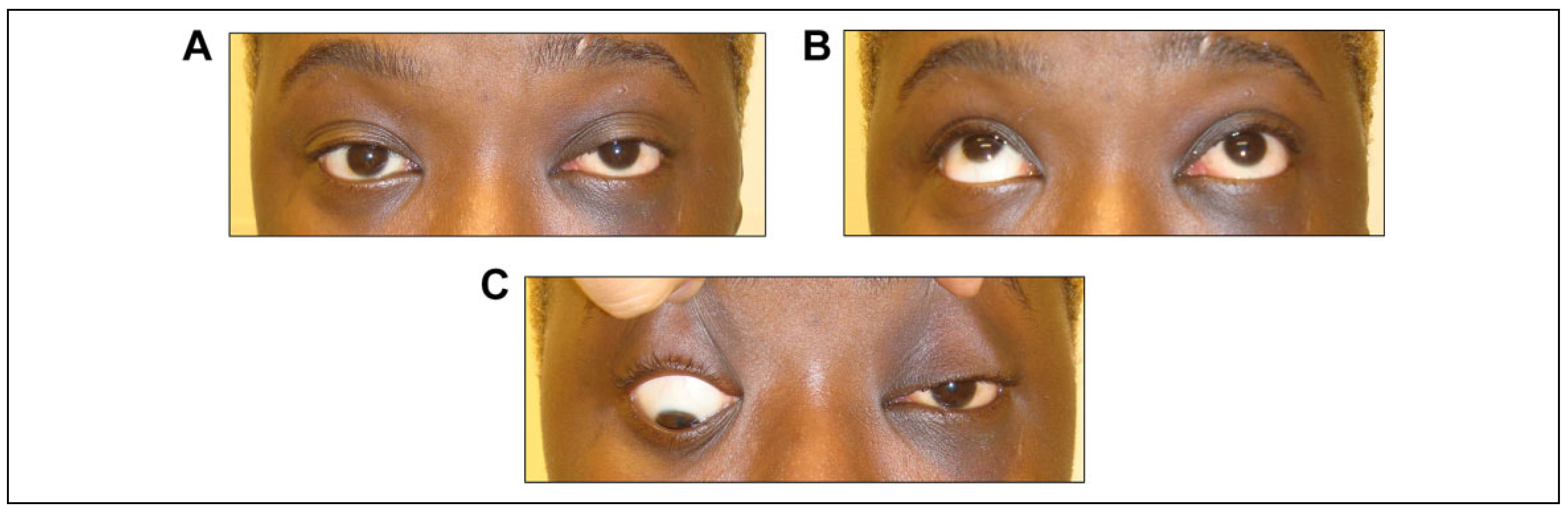
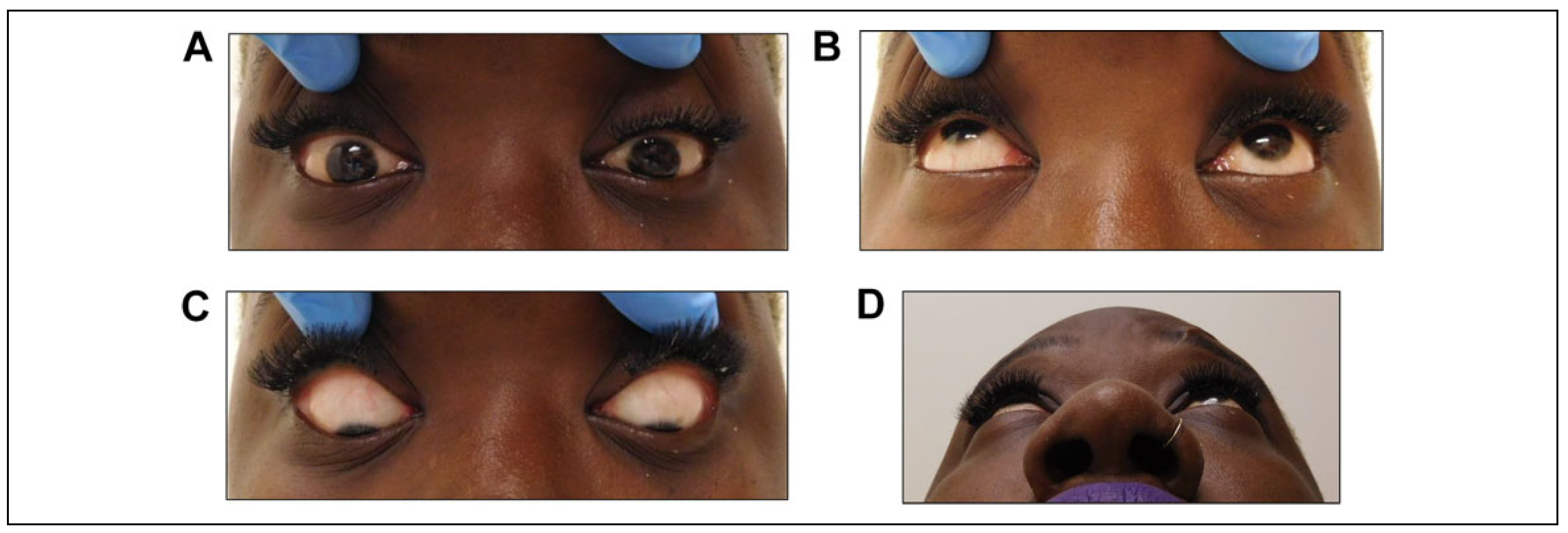
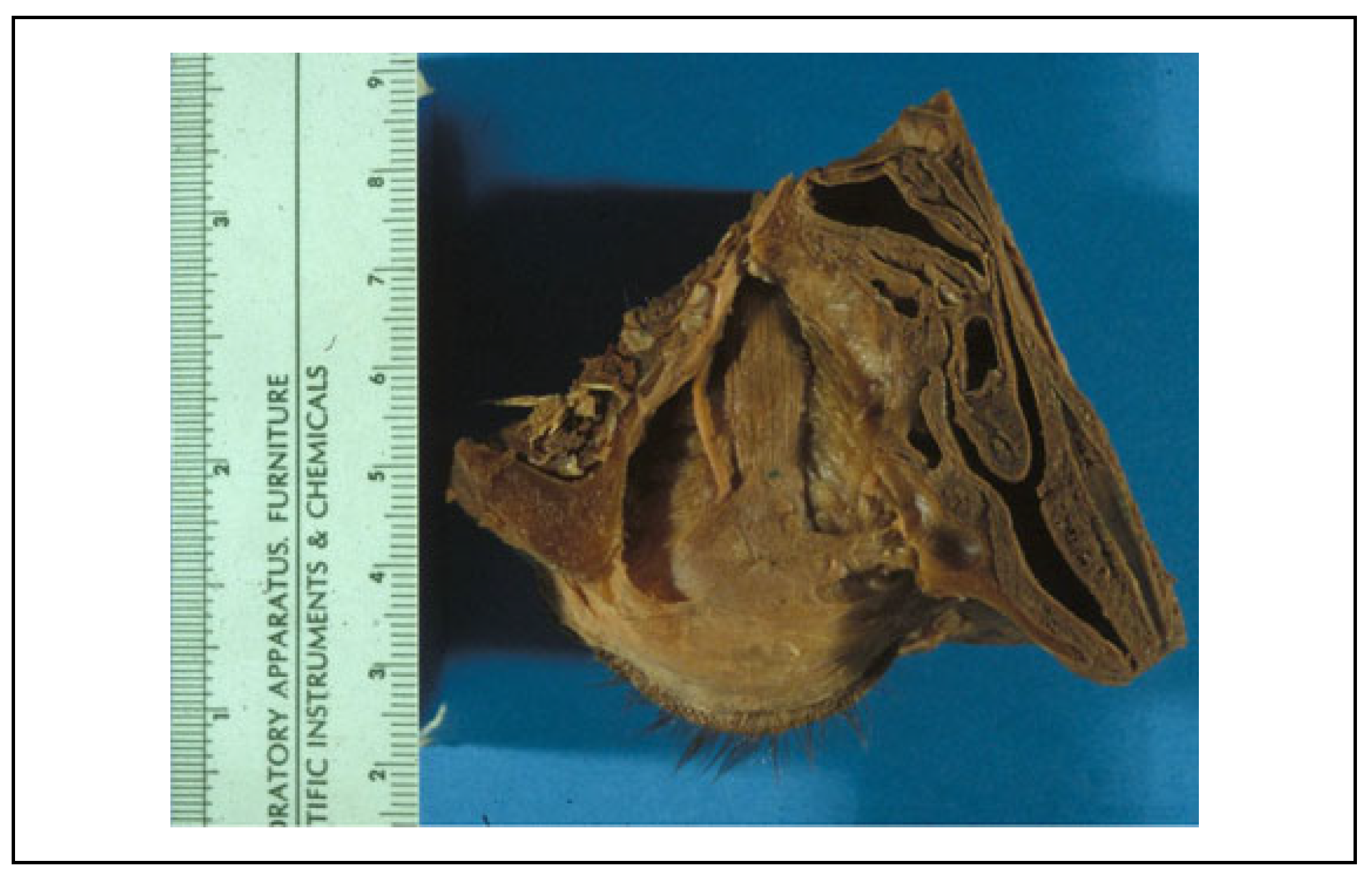
Case Report
Discussion
Funding
Conflicts of Interest
Authors’ Note
References
- Grant, J.H.; Patrinely, J.R.; Weiss, A.H.; Kirney, P.C.; Gruss, J.S. Trapdoor fracture of the orbit in a pediatric population. Plast Reconstr Surg. 2002, 109, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Iliff, N.; Manson, P.; Katz, J. Mechanisms of extraocular muscle injury in orbital fractures. Plast Reconstr Surg. 1999, 103, 787–799. [Google Scholar] [CrossRef]
- Manson, P.; Iliff, N.; Robertson, B. Trapdoor fracture of the orbit in a pediatric population. Plast Reconstr Surg. 2002, 109, 490–495. [Google Scholar]
- Bansagi, Z.C.; Meyer, D.R. Internal orbital fractures in the pediatric age group: characterization and management. Ophthalmology 2000, 107, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Jordan, D.R.; Allen, L.H.; White, J. Intervention within days for some orbital fractures: the white-eyed blowout opthal. Plast Reconstr Surg. 1998, 14, 379–390. [Google Scholar] [CrossRef]
- Egbert, J.E.; May, K.; Kersten, R.C.; Kulwin, D.R. Pediatric orbital floor fracture: direct extraocular muscle involvement. Ophthalmology 2000, 107, 1875–1879. [Google Scholar] [CrossRef]
- Soll, D.B.; Polley, B.J. Trapdor variety of the blowout fracture of the orbital floor. Am J Ophthalmology. 1965, 60, 269–272. [Google Scholar] [CrossRef]
- Erling, B.; Iliff, N.; Robertson, B.; Manson, P. A practical look at the mechanism of orbital blow out fractures, with a revisit to the work of Raymond Pfeiffer. Plast Reconstr Surg. 1999, 103, 1313–1316. [Google Scholar] [CrossRef]
- Fujino, T. Experimental blow out fracture of the orbit. Plast Reconstr Surg. 1974, 54, 81–82. [Google Scholar] [CrossRef]
- Fujino, T.; Makino, K. Entrapment mechanism and ocular injury in orbital blowout fracture. Plast Reconstr Surg. 1980, 65, 571–576. [Google Scholar] [CrossRef]
- Merville, L.C.; Gitton, E. An unusual form of isolated fracture of the orbital floor: “valve fracture”. Therepeutic Problems. Rev Stomatol Chir Maxillofac. 1985, 86, 165–170. [Google Scholar] [PubMed]
- Thiagarajah, C.; Kersten, R.C. Medial blowout fracture. Craniomaxillofac Trauma Reconstr. 2009, 2, 135–139. [Google Scholar] [PubMed]
- Tse, R.; Allen, L.; Matic, D. The white eyed medial blowout fracture. Plas Recon Surg. 2007, 119, 277–286. [Google Scholar]
- Kwon, J.H.; Moon, J.H.; Kwon, M.S.; Cho, J.H. The differences of blowout fracture of the inferior orbital wall between children and adults. Arch Otolaryngol Head Neck Surg. 2005, 131, 723–727. [Google Scholar] [PubMed]
- Kum, C.; McCulley, T.J.; Yoon, M.K.; Hwang, T.N. Adult orbital trapdoor fracture. Ophthal Plast Reconstr Surg. 2009, 25, 486–487. [Google Scholar]
- Criden, M.R.; Ellis, F.J. Linear nondisplaced orbital fractures with muscle entrapment. J AAPOS. 2007, 11, 142–147. [Google Scholar]
- Zavattero, E.; Roccia, F.; Benech, R.; et al. Orbital trapdoor fracture. J Craniofac Surg. 2015, 26, e6–e8. [Google Scholar] [PubMed]
- Kersten, R.C. Persistent upgaze restriction after orbital fracture repair. Craniomaxillofac Trauma Reconstr. 2016, 9, 268–270. [Google Scholar]
- Kersten, R.C.; Vogeli, M.R.; Brantley, G.B. Orbital “Blowout” fractures; time for a new paradigm. Ophthalmology 2018, 125, 796–7698. [Google Scholar]
- Marin, P.; Love, T.; Carpenter, R.; Iliff, N.; Manson, P. Complications of orbital reconstruction: misplacement of bone grafts within the intramuscular cone. Plas Reconst Surg. 1998, 101, 1323–1327. [Google Scholar]
- Alinasab, B.; Ryott, M.; Stjarne, P. Still No reliable consensus in the management of blow-out fractures. Injury 2014, 45, 197–202. [Google Scholar] [PubMed]
- Smith, B.; Lisman, R.D.; Semanta, J.; Della Rocca, R. Volkman’s contracture of the extraocular muscles following blowout fracture. Plast Reconstr Surg. 1984, 74, 200–216. [Google Scholar] [PubMed]
- Sires, B.S.; Stanley, R.B., Jr; Levine, L.M. Oculocardiac reflex caused by orbital floor trapdoor fracture: an indication for urgent repair. Arch Ophthalmol. 1998, 116, 955–956. [Google Scholar]
- Dubois, L.; Steenen, S.A.; Gooris, P.J.J.; et al. Controversies in orbital reconstruction II. timing of post-traumatic orbital reconstruction: a systematic review. Int J Oral Maxillofac Surg. 2015, 44, 433–440. [Google Scholar] [PubMed]
- Burt, B.; Jamieson, M.; Slone, B. Medial wall fracture induced pneumoorbita mimicking inferior rectus entrapment. Am J Emerg Med. 2010, 28, 119. [Google Scholar]
- Coon, D.; Kosztowski, M.; Mahoney, N.R.; Mundinger, G.S.; Grant, M.P.; Redett, R.J. Principles for management of orbital fractures in the pediatric population: a cohort study of 150 patients. Plast Reconstr Surg. 2016, 137, 1234–1240. [Google Scholar]
- Broyles, J.M.; Jones, D.; Bellamy, J.; et al. Pediatric orbital floor fractures: outcome analysis of 72 children with orbital floor fractures. Plast Reconstr Surg. 2015, 136, 822–828. [Google Scholar]
- Losee, J.E.; Afifi, A.; Jiang, S.; et al. Pediatric orbital fractures: classification, management, and early follow-up. Plast Recon Surg. 2008, 122, 886–897. [Google Scholar]
- Hink, E.M.; Wei, L.A.; Durairaj, V.D. Clinical features and treatment of pediatric orbital fractures. Opthal Plas Recon Surg. 2014, 30, 124–131. [Google Scholar]
- Hatton, M.; Watkins, L.M.; Rubin, P.A. Orbital fractures in children opthal. Plas Recon Surg. 2001, 17, 174–179. [Google Scholar]
- Brucoli, M.; Arcuri, F.; Cavenaghi, R.; Benech, A. Analysis of complications after surgical repair of orbital fractures. J Craniofacial Surg. 2011, 22, 1387–1390. [Google Scholar]
- Yang, J.W.; Woo, J.E.; Am, J.H. Surgical outcomes of trapdoor fracture in children and adolescents. J Craniomaxillofac Surg. 2015, 43, 444–447. [Google Scholar] [PubMed]
- Ethunandan, M.; Evans, B.T. Linear trapdoor or “white-eye” blowout fracture of the orbit: Not restricted to children. Br J Oral Maxillofac Surg. 2011, 49, 142–147. [Google Scholar] [PubMed]
- Koornneef, L. New insights in the human orbital connective tissue. Result of a new anatomical approach. Arch Ophthalmol. 1977, 95, 1269–1273. [Google Scholar]
- de Man, K.; Wijngaarde, R.; Hes, J.; de Jong, P.T. Influence of age on the management of blow-out fractures of the orbital floor. Int J Oral Maxillofac Surg. 1991, 20, 330–336. [Google Scholar]


| Grading of gaze limitation | Percentage of movement remaining |
|---|---|
| —1 | 75 |
| —2 | 50 |
| —3 | 25 |
| —4 | No movement beyond midline |
 |
© 2020 by the author. The Author(s) 2020.
Share and Cite
Gowda, A.U.; Manson, P.N.; Iliff, N.; Grant, M.P.; Nam, A.J. Resolution of Vertical Gaze Following a Delayed Presentation of Orbital Floor Fracture With Inferior Rectus Entrapment: The Contributions of Charles E. Iliff and Joseph S. Gruss in Orbital Surgery. Craniomaxillofac. Trauma Reconstr. 2020, 13, 253-259. https://doi.org/10.1177/1943387520965804
Gowda AU, Manson PN, Iliff N, Grant MP, Nam AJ. Resolution of Vertical Gaze Following a Delayed Presentation of Orbital Floor Fracture With Inferior Rectus Entrapment: The Contributions of Charles E. Iliff and Joseph S. Gruss in Orbital Surgery. Craniomaxillofacial Trauma & Reconstruction. 2020; 13(4):253-259. https://doi.org/10.1177/1943387520965804
Chicago/Turabian StyleGowda, Arvind U., Paul N. Manson, Nicholas Iliff, Michael P. Grant, and Arthur J. Nam. 2020. "Resolution of Vertical Gaze Following a Delayed Presentation of Orbital Floor Fracture With Inferior Rectus Entrapment: The Contributions of Charles E. Iliff and Joseph S. Gruss in Orbital Surgery" Craniomaxillofacial Trauma & Reconstruction 13, no. 4: 253-259. https://doi.org/10.1177/1943387520965804
APA StyleGowda, A. U., Manson, P. N., Iliff, N., Grant, M. P., & Nam, A. J. (2020). Resolution of Vertical Gaze Following a Delayed Presentation of Orbital Floor Fracture With Inferior Rectus Entrapment: The Contributions of Charles E. Iliff and Joseph S. Gruss in Orbital Surgery. Craniomaxillofacial Trauma & Reconstruction, 13(4), 253-259. https://doi.org/10.1177/1943387520965804



