
Welcome to FACE AHEAD, organized by AO CMF. FACE AHEAD is designed to be one of the most important gatherings of young surgeons active in the treatment of craniomaxillofacial lesions from all over the world. It is with great regret that, due to concerns over COVID-19, FACE AHEAD 2020 had to be postponed by a year.
We are determined and committed to conduct FACE AHEAD on March 25–27, 2021 in Barcelona.
FACE AHEAD gives the accepted abstract submitters the option to publish their work in this supplement to the Craniomaxillofacial Trauma & Reconstruction Journal even though the in-person meeting had to be postponed to 2021.
This supplement contains 40 carefully selected abstracts in the following areas:
Trauma
Oncology
Reconstruction
Facial deformity surgery
Cleft lip and palate
Aesthetic surgery
Temporomandibular joint (TMJ) disorders
Oral surgery/implants
Orthognathic surgery
3-D planning
Other
We are committed to offering you FACE AHEAD 2021 with exactly what we had promised you for 2020. You will get another chance to publish your contributions and present the progress of your scientific work in a year’s time. We are convinced that the oral and e-poster presentations along with the symposia, will encourage lively discussions among participants and generate new ideas to help advance CMF care. We hope to see you in Barcelona at FACE AHEAD 2021 for three exciting days from 25–27 March 2021.
- Gregorio Sánchez Aniceto, Chair
- Sabine Girod
- Mike Leung
- Satyesh Parmar
- FACE AHEAD Organizing Committee
TOPIC: TRAUMA
EP02
Treatment of Atrophic Mandible Fractures
- Ricardo Cienfuegos
- Centro Médico ABC, Mexico City, Mexico
Abstract
- Objectives: Fractures of the atrophic mandible have been historically treated in various ways, from intermaxillary fixation to internal fixation with plates and screws. Since there is poor bone quality, some cases require bone grafts. Computed tomography (CT) scanning makes it possible to assess the lack of cancellous bone at the fracture site, and thus the need for bone grafts, as well as for locked or nonlocked plates. Besides, the Luhr classification serves as a guide to select the type of treatment.
- Methods: The authors analyzed the outcomes 6 months after surgery in a retrospective series of 19 patients with atrophic mandible fractures treated with plates and screws, placed according to the principle of load bearing. Locked systems were used in some cases, and non-locked systems in others. For patients in Luhr classes II and III, cancellous bone grafts were used to improve osteogenic response. Grafts were taken from the proximal third of the tibia, after computed tomographic assessment.
- Results: Postoperative progress was generally uneventful. Oral intake with purees was resumed 24 hours after surgery, as well as ambulation. Fracture healing at six months was seen in 17 patients. One patient died before the 6-month time point as the result of a stroke; bone healing had been underway before death. Delayed union was diagnosed 3 months after surgery in another patient who refused secondary treatment.
- Conclusions: Treatment of fractures in atrophic mandibles with plates and screws according to the load-bearing principle is a reliable procedure. CT scan findings and the Luhr classification provide useful guidance regarding the use of bone grafts and the type of plates and screws, in order to achieve the best outcomes. This treatment makes it possible to resume oral intake early, whereas no gait disturbances were seen related to graft taking.
EP07
Abstract
- Purpose: There are risks of postoperative ectropion or entropion under transconjunctival and subciliary approaches to orbital floor fractures. This study evaluates the endoscopic approach to orbital floor fractures.
- Materials and methods: From 2016 to 2018, 13 cases of orbital floor fractures were repaired endoscopically. Under navigation system and preoperative planning, an endoscopic approach was used to repair orbital floor fractures. All the risks of complication were evaluated.
- Results: There were 7 male and 6 female patients, and the age was 24.6 years. There was no ectropion or entropion. Post-operation, no enophthalmus, optic neuropathy, diplopia was noted.
- Conclusion: Under navigation system and pre-operation planning, the endoscopic approach is a safe, viable technique for orbital floor fracture repair. It offers improved visualization, anatomic fracture repair, no risk of postoperative eyelid complications, and good clinical results.
EP09
The Value of Endoscopy in Treating Unilateral Subcondylar Mandible Fractures
- Samia Saied1,2, Osma Mouhammed2, Mohamed Eloteify2, Karim Massoud3
- 1Sohag University Hospital, Sohag, Egypt. 2Aswan University, Aswan, Egypt. 3Ain-Shams University, Cairo, Egypt
Abstract
- Using endoscopic-assisted technique for fixation of subcondylar fractures is accepted by many surgeons. Our aim is to find the benefits of using endoscopy in fixing of unilateral subcondylar fractures over mandibulomaxillary fixation. A total of 30 patients with mandibular subcondylar fractures are included and divided in two groups randomly. The first group was treated conservatively with mandibulomaxillary fixation while the second group was treated by transoral endoscopic-assisted open reduction and internal fixation. Postoperative facial bone computed tomography for all patients was done, and the patients were followed for 6 months postoperatively. The endoscopic group showed overall equal or even better results than the conservatively treated group. Although, endoscopicassisted open reduction and internal fixation is a challenging approach, it is considered a consistent technique for treating subcondylar fractures.
EP13
Prophylactic Antibiotic Prescription on Open Reduction Internal Fixation of Fractured Mandible
- Jie Luo
- Queen Victoria Hospital, East Grinstead, United Kingdom
Abstract
- Introduction and Aim: Scottish Intercollegiate Guidelines Network published a guideline on antibiotic prophylaxis surgery recommending antibiotic prophylaxis for open reduction internal fixation (ORIF) of compound mandibular fractures; however, the duration should not be more than 24 hours. From recent clinical observation, it seemed to be routine practice to give a course of antibiotics on discharge for most of the patients who were treated with ORIF mandibular fracture. The aim of the study was to audit prophylactic antibiotic prescription habit on ORIF fracture mandible in our busy Maxillofacial Regional Referral Centre, Queen Victoria Hospital, East Grinstead, United Kingdom, for the year 2018.
- Methods: 50 ORIF fractured mandible cases were randomly selected from all the cases (122 cases) which were preformed between January 2018 and September 2018. We excluded pathological fractures; recorded pre-, perio-, and postoperative antibiotics prescriptions; assessed the length of time between injury and surgery; patients’ factors (medical and social history), surgeons’ experience level, and postoperative complications.
- Results: All the patients were given preoperative antibiotics. Co-amoxiclav appeared to be the first line management and, for patients with penicillin allergies, clindamycin was given instead. Of the patients, 86% were given antibiotics postoperatively with various dosages and durations. There was no obvious correlation between length or type of antibiotics and post-operative complications.
- Conclusion: Patients who had preexisting periodontal disease with smoking habit and partially erupted wisdom tooth in the line of fracture contributed to most of postoperative complications. There are further opportunities for reducing antibiotic prescriptions with the aim of lowering the risk of developing antibiotic resistance.
TOPIC: OTHER
EP21
Audit of OMFS Elective and Emergency Operative Notes
- Aiysha Mahmood, Janhvi Shah, Sukhpreet Dubb, Arun Majumdar
- Luton and Dunstable Hospital, Luton, United Kingdom
Abstract
- Introduction and aims: A significant variability was noted across operation notes in an oral and maxillofacial (OMFS) department between surgeons. The Royal College of Surgeons (RCS) publishes ideal parameters that should be included within an operation note to improve patient safety.
- This audit aimed to investigate how well operation notes matched standards set by the Royal College of Surgeons in order to improve information governance, communication and patient safety following an operative procedure.
- Methods: A retrospective analysis was performed on all general anesthetic procedures performed by the OMFS department and compared to the Royal College of Surgeons guidance. The first cycle recorded 136 operations, 22 elective (16%) and 114 emergency (84%) over 2 months. The second cycle examined 154 operations, 28 elective (18%) and 126 emergency (81%) over 2 months.
- Results and conclusions: There was general improvement across most recorded parameters between the first and second cycles respectively; time increased from 13% to 40%, elective/emergency increased from 1% to 19%, named anesthetist increased from 32% to 85%, and key operative findings improved from 66% to 90%. Parameters not improved at audit closure included recording additional procedures (30% to 15%), anticipated blood loss (11% to 4%) and operative diagnosis reduced from 75% to 64%.
- In conclusion, most operative note documentation parameters had improved; however, further changes are needed to improve patient safety and may include the use of proformas and induction presentations.
EP22
Audit of Cone Beam CT Referrals Meeting the Gold Standard for Wisdom Tooth Exodontia Based on OPG Examination
- Aiysha Mahmood, Janhvi Shah, Sukhpreet Dubb, Chi-Hwa Chan
- Luton and Dunstable Hospital, Luton, United Kingdom
Abstract
- Objectives: Cone beam computed tomography (CBCT) is used by the oral and maxillofacial surgery (OMFS) department for management of wisdom tooth exodontia. This audit aimed to highlight whether CBCT referrals for proximity of wisdom teeth to the inferior dental nerve prior to exodontia met the gold standard guidelines based on orthopantomogram (OPG) examinations.
- Methodology: The European Commission Guidelines for Dental and Maxillofacial Radiology state the three indications to consider a CBCT from an OPG are “darkening” of the root, interruption of the ID canal wall and diversion of the canal. Retrospective analysis was undertaken for CBCT referrals for wisdom tooth exodontia over 1 year (46 cases), a 3 month period to implement changes, and then reaudited over a 1 year period.
- Results: Of all referred cases, 78% met the gold standard for referral with the remaining 22% referred based on nonsignificant OPG indications including deflected root (15%), narrowed canal (13%) and bifid roots (10%). In 16% of patients a change in management resulted from CBCT scanning including coronectomy (4%), delay (2%) or cancellation (6%). A forced choice proforma, education and posters of indications were implemented. Following 3 months, a reaudit was carried out over 1 year (65 cases) with 87% meeting the gold standard with 7% undergoing a change in management including a coronectomy (4%) or cancellation (3%).
- Conclusions: Our results demonstrated an increase in the number of referrals based on evidence-based signs on OPG for CBCT for wisdom tooth exodontia with a reduction in patients delaying or canceling their procedures.
TOPIC: ORTHOGNATHIC SURGERY
EP25
The Stability of Anterior Open Bite After Orthognathic Surgery
- Islam Ellabban, Sarah Germain, Anthony Paaterson
- North Cumbria University Hospitals NHS Trust, Carlisle, United Kingdom
Abstract
- Objectives:
- Assess the degree of stability for patients who had an orthognathic surgery for anterior open bite.
- To assess the success rate.
- Analyze the surgical movements and cause for relapse.
- Methods: Retrospective analysis for the patients who had an orthognathic surgery for anterior open bite. This was done via comparing the lateral cephalometric X-rays and dental models done immediately after surgery (T1), one year postoperatively (T2) and 2 years postoperatively (T3). A sample of 11 patients was identified to fit the inclusion criteria. The sample can be described as having a pretreatment anterior open bite of at least −3 mm to −6.5 mm. All of the patients received combined orthodontic and orthognathic therapy via the same surgeon.
- Three factors were taken in consideration when comparing results:
- Overbite (models and lateral cephalometric X-ray)
- Lower anterior facial height: total anterior facial height
- Maxillomandibular plane angle
- Results: 73% of patients remained to experience a positive overbite after 2 years following the surgical procedure. 27% of patients experienced a relapse and had an overall negative overbite in the 2 years following the surgical procedure. The 27% of patients who endured a relapse had a high pretreatment maxillomandibular plane angle, which were at least 38 to 45.4, whereas the average of all the patients was 36.4. 66% of the patients who endured a relapse had a range of 3–3.5 mm maxillary posterior impaction compared to the patients with positive overbite, who had an average of 4.3 mm impaction.
- Conclusion: 73% of the patients remained with a positive incisal overbite in the 2 year follow-up. Patients with a high maxillomandibular plane angle associated with minimal impaction movements are at a higher risk of developing a relapse in their anterior open bites.
EP26
Failure of All Fixation Devices Used for A Le Fort I Osteotomy in A Patient with Obstructive Sleep Apnea and Severe Parafunctional Habits
- Zahid Lalani
- Houston Methodist Hospital, Houston, United States
Abstract
- Over the past three decades, craniofacial fixation has evolved significantly as a result of improved understanding of the biology of bone healing, advances in material science, and engineering of devices. As these advances have evolved, so have the complications that are seen with their use in craniofacial surgery. Reduction in size of fixation devices while maintaining structural strength, integrity and the ability to withstand physiologic forces in the craniofacial skeleton has been a driving force in this evolution.
- As the number of adult patients being diagnosed with obstructive sleep apnea has increased, so have the number of cases of maxillomandibular advancement to increase the airway space as a counter to the sole use of continuous positive airway pressure (CPAP) devices. A number of these individuals have significant parafunctional habits that are partly attributed to a protrusive position of the mandible to increase their airway. Use of the fixation devices traditionally used for orthognathic surgery in this patient cohort exposes the devices to a significantly higher physiologic force than they were likely designed to withstand. Fracture of isolated fixation devices in patients with craniofacial osteotomies has been reported in literature as a complication. However, there are no reported cases in literature where all devices in a patient have failed due to severe parafunctional habits.
- We present the case report of a heretofore unreported and unusual complication in a patient who underwent maxillomandibular advancement for increasing airway space for obstructive sleep apnea. Four 3-D midfacial fixation plates fractured due to fatigue secondary to severe parafunctional habits leading to nonunion of the midfacial osteotomy requiring additional surgery.
- The goal of this presentation is to engender a conversation and see if there are other surgeons who have encountered such a complication and to design fixation devices that can withstand higher physiologic forces in patients who need them.
EP27
A New Education Alternative in Orthognathic Mandibular Osteotomy: Air-Dried Clay Model
- Erol Kozanoğlu, Bora Edim Akalın, Hayri Ömer Berköz, Soner Karaal, Nermin Mammadova, Erman Ak, Ahmet Faruk Yücel, Ufuk Emekli
- Istanbul University Istanbul Faculty of Medicine, Department of Plastic Reconstructive and Aesthetic Surgery, Istanbul, Turkey
Abstract
- Objectives: Orthognathic surgery is a key element of craniomaxillofacial surgery. The aim of this study is to evaluate the effectiveness of a low-cost model that is produced from air-dried clay in orthognathic mandibular osteotomy.
- Methods: An air-dried clay mold was prepared from a human mandibula model and seventeen partial mandibular models (MM-17) were produced for the sagittal split ramus osteotomy surgery (SSRO). The operations were performed by four surgeons with orthognathic surgery experience of at least three years. Each surgeon operated on four models. The completion times of corticotomies and SSROs, the presence and time of MM-17 fractures, the similarity points of MM-17 cortex and medulla with the human mandible, the mandibular representation point of MM-17 and educational compatibility point of MM-17 were recorded for each model.
- Results: The cost of one MM-17 was EUR 0.5. The corticotomies were completed in an average of 126.75 (110– 150) seconds. The mean cortical resistance point was 8.75/10 (8–10). Three SSROs were completed in an average of 288 (205–401) seconds. The ratios of outer and inner cortical fractures were 60% and 40% respectively. The mean medullar resistance similarity point was 5/10 (4–6). The mean mandibular representation point of MM-17 was 5.25/10 (4–7). The mean orthognathic mandibular osteotomy educational compatibility point of MM-17 was 8.25 (7–10).
- Conclusion: Air dried clay is mechanically similar to the mandibular cortex and MM-17 is the first air-dried clay mandibular education model. Although MM-17 does not enable a complete SSRO, it is an appropriate and low-cost alternative in orthognathic mandibular corticotomy education. Surgical instrument usage capabilities such as drilling and osteotomizing may be improved on MM-17 before patient-based applications.
TOPIC: ORAL SURGERY/IMPLANTS
EP30
New Strategies of Immediate Alveolar Ridge Preservation After Tooth Extraction
- Nikolay Redko, Alexey Drobyshev, Sergey Shamrin, Andrey Miterev
- Moscow State University of Medicine and Dentistry, Moscow, Russian Federation
Abstract
- Objectives: The most effective method of treatment adentia is dental implantation. The main difficulty in carrying out this manipulation is the resorption of the alveolar ridge after extraction of the teeth. The aim of our study is to evaluate the effectiveness of using bone-grafting materials for alveolar ridge preservation following atraumatic tooth extraction.
- Methods: 87 patients underwent tooth extraction. 27 patients were treated by using natural bovine bone substitute (NBBS). In 32 cases autologous dentin matrix (ADM) of the extraction teeth was used, and in 28 cases plasmarich growth factors (PRGF) was used for alveolar ridge preservation.
- After 12 ± 4 weeks an implantation was made. Clinical and 3-dimensional radiological assessments were performed at day 0, 3 months, and 9 months postoperative. Before and after treatment intraoral scanning was also done for all patients
- Results: There were no clinical differences in general wound healing between the groups, but better healing was in the group with using PRGF. Analysis of the results of three groups showed a significant difference of level of bone resorption; less resorption was in groups with use of NBBS (14.6% in height, 13.3% in width) and with use of ADM (16.3% in height, 15.2% in width). Comparison between groups showed a significant difference of bone resorption at 3 and 9 months. All dental implantations were successfully made in the follow-up period. The primary stability of dental implants was 71 ISQ (from 63 to 79 ISQ). The primary morphological analysis of the trepan biopsies revealed significantly more trabecular bone formation in ADM group, and a lot of blood vessels in the newly formed bone when using PRGF.
- Conclusions: We can recommend comparing use of ADM and NBBS with collagen membrane or platelet rich plasma.
TOPIC: FACIAL DEFORMITY SURGERY
EP31
Guided Control Over Malpositioned Proximal (Condyle Bearing) Segments in Reoperative Mandibular Reconstruction Cases
- Mohamed Ghorab
- Cairo University Oral and Maxillofacial Surgery Department, Cairo, Egypt
Abstract
- Objectives: Virtual planning and 3-D printing in head and neck reconstruction is becoming a diverse field with several methods described and reported. However, some of it is inaccessible to certain surgeons due to costs or complexity of the virtual planning steps. In this series of cases, we describe a simple method of controlling mandibular segments intraoperatively without the need for intermaxillary fixation. A 3-D-printed “U-shaped” guide is used to hold mandibular segments in planned position. Such a guide allows control over the proximal segment position, where the condyle bearing segment is malpositioned with no teeth in the segment to relate it to the maxilla. The objectives of this study are: to describe the design of a simple guide to reposition and align the malpositioned proximal segment in mandibular reoperative reconstruction cases and to assess the accuracy of the guide by superimposing the outcome over the planned position.
- Methods: A 3-D virtual model based on the patient’s Digital Imaging and Communiations in Medicine (DICOM) data is created and the mandibular segments are isolated and virtually repositioned. The non-toothbearing malpositioned proximal segment is seated into the fossa and hinge rotated to match the contralateral side. A guide that connects and holds mandibular segments together is created. Postoperative 3-D models are created, and surface registration is performed to compare the outcome with the plan.
- Results: Reconstruction was successful in all reported cases with regain of normal mandibular contour. Further, and in the absence of intermaxillary fixation, the occlusion relationship was satisfactory. After surface comparison of planned and outcome positions of the mandibular segments using stable reference points, the mean deviation is 0.57 mm with maximum deviation 2.1 mm.
- Conclusions: This study confirms the accuracy of utilizing a simple custom-made guide in repositioning malpositioned proximal mandibular segments in the absence of intermaxillary fixation.
EP34
Comparison of Noninvasive Methodologies to Assess Mouth Opening Following Lipotransfer Techniques to Reverse Oral Fibrosis
- Michelle Griffin1, Aya Bakir2,3, Bryan Chew4, Christopher Denton5, Peter Butler1,6
- 1UCL Centre for Nanotechnology and Regenerative Medicine, Division of Surgery and Interventional Science, University College London, London, United Kingdom. 2Department of Plastic Surgery, Royal Free London NHS Foundation Trust Hospital, London, United Kingdom. 3Plastic and Reconstructive Surgery Department, Faculty of Medicine, Ain Shams University, Cairo, Egypt. 4Department of Plastic Surgery, Royal Free London NHS Foundation Trust Hospital, London, United Kingdom. 5Institute of Immunity and Transplantation, University College London, London, United Kingdom. 6Charles Wolfson Centre for Plastic & Reconstructive Surgery, London, United Kingdom
Abstract
- Objectives: The restrictions to the mouth opening as a result of skin fibrosis, scarring, etc., cause severe impairments to the patient’s self-image and quality of life. Monitoring the effect of the surgical intervention for patients with facial fibrosis is limited due to the limited tools to assess mouth opening in these patients. The currently available method is the mouth handicap in systemic sclerosis (MHISS) score which mainly targets scleroderma patients. However, such questionnaires can be time consuming and thus we aimed to examine whether there are alternative methods that can assess mouth opening to monitor facial fibrosis.
- Methods: Currently reported techniques for measuring mouth opening include performing two-dimensional photographs and measuring the maximum mouth opening length using software analysis tools. To evaluate the currently reported alternative tools (Vernier calipers, paper cone, OptraGate lip retractor and TheraBite®) for our intervention for facial fibrosis, we assessed the tool within a cohort of 20 patients with diffuse scleroderma and 20 age- and sex-matched controls. We compared the regression of each tool to the MHISS score for both control and intervention patients. Furthermore, we assessed whether any of the tools could detect differences with the control and scleroderma patients.
- Results: Analysis demonstrated that the tools had varied association to the MHISS score. The highest correlation to the MHISS score was the paper-cone measurement and the OptraGate system with the least being the TheraBite® system. In addition, the OptraGate and the paper cone detected significant difference between the control and scleroderma patients. Furthermore, the paper cone is significantly cheaper than the OptraGate which is important for the clinician and institution when considering evaluation tools for implementation.
- Conclusion: In conclusion, using a paper cone is of value to measuring mouth opening. Assessment using a paper cone is easy to implement for both the clinician and patient.
TOPIC: RECONSTRUCTION
EP35
Role of Fasciocutaneous Supraclavicular Artery Flap in Reconstruction of the Maxillofacial Soft Tissue Defects
- Muhammad Farooq1, Tahir Ullah2, Zafar Khan3
- 1Department of Oral & Maxillofacia Surgery, Bannu Medical College, Bannu, Pakistan. 2Lady Reading Hospital, Peshawar, Pakistan. 3College of Dentistry, University of Jouf, Sakaka, Saudi Arabia
Abstract
- Background: Maxillofacial soft tissue defects have many causes and the resulting functional and aesthetic defects are addressed out of necessity to improve quality of life. Simplicity of procedure, best functional and aesthetic outcome and least possible donor site morbidity are the minimum requirements of a good reconstruction option. The supraclavicular-artery-based flap is an extremely reliable local flap. Its thin pliable skin gives good color and texture match for the maxillofacial region, with minimal donor site morbidity.
- Objectives: The purpose of this study was to determine the role of supraclavicular artery flap in maxillofacial soft tissue reconstruction.
- Methods: This study was carried out on thirty patients with soft tissue defects in the maxillofacial region. At postoperative visits, they were evaluated for functional and cosmetic outcomes and donor site morbidity.
- Results: A 93.3% success rate was found in this study while 6.7% of the cases showed distal necrosis. Almost all of the patients were satisfied with their cosmetics in the last follow-up visits. Movements of the shoulder of the donor site and mouth opening at the recipient site were in the normal range. Donor site was primarily closed in 23 cases and there was no hypertrophic scar.
- Conclusions: The results of this study seem to suggest that fasciocutaneous supraclavicular artery flap can be considered as a useful reconstructive option in the shallow defects of the lower third of the face.
TOPIC: ONCOLOGY
EP45
Non-Hodgkin Lymphoma of the Parotid Gland
- Tiberiu Tamas¸1, Adela Tamas¸2, Sebastian Stoia1, Cristian Dinu1, Grigore Baciut3, Mihaela Baciut3
- 1Emergency County Hospital Cluj-Napoca, Romania, Oral and Maxillofacial Surgery Department, Cluj Napoca, Romania. 2The Oncology Institute ‘Prof. Dr. Ion Chiricuta’ Cluj-Napoca, Cluj Napoca, Romania. 3University of Medicine and Pharmacy “Iuliu Hatieganu” Cluj-Napoc, Romania
Abstract
- Objectives: The aim of this study was to evaluate the incidence of parotid lymphoma, the impact of associated pathology in disease development and the therapeutic role of the surgical approach.
- Methods: We retrospectively analyzed 362 cases of parotid gland tumors operated on in our department from 2012–2018; only nine were diagnosed with parotid lymphoma. We focused on the demographical data, age, associated pathology, histologic type, lactate dehydrogenase (LDH) levels, complete blood count and the treatment option.
- Results: 6 women and 3 men (females to males: 2:1) with ages varying from 29 to 84 years (median age of 59.9 years) were included, with confirmed diagnosis from an excisional biopsy followed by radiation or/and chemotherapy. The most common hystological type was the diffuse large B-cell lymphoma (n = 5), followed by mucosa-associated lymphoid tissue (MALT) lymphoma (n = 2), follicular type (n = 1) and Burkitt lymphoma (n = 1). All cases were stage I and II (Ann Arbor staging system). As for associated pathologies, one patient with Sjögren syndrome has developed parotid lymphoma after six years. Cardiovascular pathology under medication was correlated in six cases and type II diabetes in 4 cases. A simultaneous squamous cell carcinoma and a lymphoma affected the same parotid gland. The complete blood count (CBC) was lower in 4 cases and the LDH level was higher in 3 cases. In all cases, the tumor was clinically described as a painless elastic mass.
- Conclusions: Non-Hodgkin lymphoma (NHL) of the parotid gland is a rare tumor, with the most frequent subtypes: diffuse large B-cell lymphoma and the MALT lymphoma. Higher levels of LDH and lower values of CBC are helpful in diagnosis guidance. The risk is increased from two to ten times by the Sjögren syndrome and type II diabetes. The role of surgery is limited to the diagnosis and the treatment must be selected by histologic subtype and stage of lymphoma.
EP46
Diagnostic Value of Ultrasonography in Assessment of Cervical Lymph Node Metastasis in Patients with Oral and Oropharyngeal Cancer
- Sebastian Stoia1, Tiberiu Tamas¸1, Adela Tamas¸2, Manuela Lenghel3, Cristian Dinu1, Grigore Băciuț1
- 1Emergency County Hospital, Oral and Maxillofacial Surgery Department, Cluj-Napoca, Romania. 2The Oncology Institute “Prof. Dr. Ion Chiricuță,’ Cluj-Napoca, Romania. 3Department of Radiology, Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania
Abstract
- Objectives: The purpose of this study was to evaluate the accuracy of preoperative ultrasonography in detection of metastatic cervical lymph nodes in patients with oral cancer.
- Methods: We retrospectively analyzed the recorded data of patients diagnosed with oral and oropharyngeal cancer who underwent preoperative bilateral neck ultrasonography and benefited from surgical treatment, including neck dissection, in our department between 2013 and 2019. 51 patients were included in this study. The results obtained after performing the neck ultrasonography, operated by a single examiner, were compared and correlated with the histopathological report obtained after neck dissection and presented in terms of sensitivity, specificity, predictive values and accuracy. We have also analyzed the distribution of the primary cancer site.
- Results: Ultrasonography showed a sensitivity of 92%, a specificity of 82%, a predictive positive value of 86%, a predictive negative value of 90% and an overall accuracy of 88.2% in detecting cervical lymph node metastasis from oral and oropharyngeal cancer. The floor of the mouth was the most frequent cancer site (45%) followed by the tongue (27%), the base of the tongue (10%), retromolar trigone (8%), gum of the alveolar process (8%) and cheek mucosa (2%).
- Conclusion: Ultrasonography can be considered a reliable and valuable diagnostic tool in detection of lymph node metastasis in patients with oral and oropharyngeal cancer. It is a noninvasive, inexpensive, easily accessible examination that can be used in combination with computed tomography or magnetic resonance imaging to improve or support its accuracy in the diagnosis, staging and treatment planning of patients with oral and oropharyngeal cancer.
TOPIC: TEMPOROMANDIBULAR JOINT (TMJ) DISORDERS
EP51
A New Non-Metallic Anchor for TMJ Discopexy: More User-Friendly and Better Outcome
- Mohamed Klink
- Privat, Lebanon
Abstract
- Among all temporomandibular joint (TMJ) problems that we treat, the anterior disc displacements are the most challenging ones. Due to the limited mouth opening, as well as the unbearable pain and headache felt by the patient, we found ourselves adopting several treatments aiming to reduce the meniscus and relief the pain. Numerous treatments have been indicated for TMJ problems: splint, arthrosynthesis, arthroscopy, botox injection. These treatments have succeeded in relief of pain in some cases. However, most of them were revealed to be ineffective, showing recidivism or meniscus displacement along with the recurrence of the symptoms. With time, medical equipment companies have been developing arthroscopic tools and anchors for orthopedic indications. With the technological medical progress, small fragment anchors have been introduced to the market. Some craniomaxillofacial (CMF) surgeons grabbed this opportunity and used these small anchors to treat TMJ disc displacement. Results of discopexy with anchors seem promising, and patients are relieved from the symptoms. The last anchor used in TMJ discopexy studies is the Mitek, which is a metallic anchor. The new anchor that I have been using for my patients is the Conmed TruShot with Y-Knot, which is an all-suture anchor, non-metallic. It is a very user-friendly system, easy to apply, more stable, less pull-out risk, with minimal bone removal, perfect for the tiny TMJ. Results shown on my patients are satisfying so far, with a good mouth opening, and most importantly pain relief.
EP52
Management of an Iatrogenic Subcondylar Fracture at Coronoidectomy
- Bora Edim Akalın, Erol Kozanoğlu, Ufuk Emekli
- Istanbul Faculty of Medicine, Istanbul, Turkey
Abstract
- Objectives: In this case report, causes and management of an iatrogenic subcondylar fracture during a coronoidectomy process for a bilateral coronoid process hyperplasia is presented.
- Methods: A 19-year-old female patient with progressed restricted jaw motion diagnosed as bilateral coronoid hyperplasia underwent bilateral coronoidectomy. During the left coronoidectomy process, an iatrogenic left subcondylar fracture occurred although the coronoid process had been held with a wire and a bone hook was hooked to the mandibular notch before the bone was cut with an oscillating saw. The condylar segment was reduced properly, and the facelift approach was used for fixation with two miniplates.
- Results: The patient was followed for eight months after the operation. There was no sequelae of the condyle fracture and the interincissive distance was measured 45 mm.
- Conclusion: For a coronoidectomy operation, preparation for a subcondylar fracture reduction and fixation should be done; this preparation should be before the coronoidectomy operation and should include the required equipment and the patient’s informed consent. Furthermore, the osteotomy should be done delicately, and the mandibular notch should be visualized to keep the condyle intact.
TOPIC: 3-D PLANNING
EP54
Combining the Use of Artificial Intelligence (AI) and 3-D Printing to Achieve Accuracy in Reduction and Stabilization of Complex Craniomaxillofacial Fractures
- Samer Abdelsamie1,2,3, Pooja Sukumar1
- 1Temple University Hospitals, Philadelphia, United States. 2St. Christopher’s Hospital For Children, Philadelphia, USA. 3Crozer-Chester Medical Center, Chester, United States
Abstract
- Objectives: The surgical management of complex facial fractures is challenging and time consuming. We highlight the benefits of combining AI and 3-D printing to achieve optimal surgical outcomes, reduce operating time, and improve patient satisfaction. We present a workflow for using AI and 3-D planning in the management of complex facial fractures.
- Methods: Literature related to AI applications in the field of craniofacial surgery, virtual surgical planning, and 3-D printing were reviewed. The team then completed multiple complex craniofacial trauma reconstruction cases using the proposed workflow. In all cases, 1 mm thick computed tomography (CT) scans were obtained and virtual reduction of fractured segments was completed in three dimensions. Based on this analysis, stereolithographic splints were 3-D printed and inserted intraoperatively. In a second case, custom-made fixation plates were fabricated. The same protocol was used in a third case to fabricate a custom prosthesis to replace severely comminuted bony segments. Postoperative CT scans were then obtained to evaluate accuracy of bony reduction.
- Results: AI and 3-D printing facilitated the fabrication of intraoperative and postoperative splints which modeled the desired outcome for bony reduction in patients with complex midface and mandible fractures. The splints were utilized during surgery to help sequence the steps in reconstruction. The splints were also helpful to stabilize the palatal vault and prevent distraction along fracture lines. Accurate reduction of all fractured segments was achieved, and facial contours were restored.
- Conclusion: The workflow proved to be a powerful tool for managing complex cases and allows surgeons to manage complex craniomaxillofacial fractures in a structured and consistent manner. The use of virtual surgical planning can help achieve high-quality anatomical reduction and fracture stabilization. Thereafter, optimal facial height, width and contours are observed clinically. The ultimate outcome is reduction in operating time, reduced complications, shorter hospital stays, and improved surgeon confidence.
EP55
Custom-made Composite Implants for Treatment of Large Craniomaxillofacial Defects in the Go¨ ttingen Minipig Model
- Bettina Mannerström1, Ahmed Abushahba1, Roman Kornilov1, Kasper Dienel2, Bas van Bochove2, Johanna Snäll1, Risto Kontio1, Roy Björkstrand3, Jouni Partanen3, Jukka Seppälä2, Riitta Seppänen-Kaijansinkko1
- 1Oral and Maxillofacial Diseases, University of Helsinki and Helsinki University Hospital, Helsinki, Finland. 2Department of Chemical and Metallurgical Engineering, School of Chemical Engineering, Aalto University, Espoo, Finland. 3Department of Mechanical Engineering, School of Engineering, Aalto University, Espoo, Finland
Abstract
- Objectives: Fabrication of custom-made composite implants using stereolithography (SLA) has emerged as a promising alternative for the reconstruction of large bone defects. In this study we investigated the applicability of an SLA fabricated composite implant of photo-crosslinked poly trimethylene carbonate (PTMC) polymer containing 35wt% β-TCP for the reconstruction of a large continuous defect in the minipig mandible. The biodegradable and biocompatible PTMC degrades by surface erosion, thereby maintaining structural mechanical integrity over time, while the β-TCP component provides the implant osteoconductive properties.
- Methods: To investigate SLA-fabricated implants, a functional workflow for the production of custom-made implants was developed in a Go¨ ttingen minipig model. Firstly, molars M1–M2 were removed unilaterally in the mandible, and the animals were computer tomography (CT) imaged for designing and manufacturing of custommade composite implants and titanium plates. In the second phase, after 7 weeks of healing, a continuous defect (length 2.5 cm, volume ~9 cm3) was created. The defect was reconstructed with composite implants and a customized titanium plate. As controls, equal numbers of animals were allocated to 3 control groups (n = 3/group); plain PTMC, empty defect and autologous bone. The animals were noninvasively followed up 6 weeks and 4 months postimplantation by CT, and at termination time point 6 months post-implantation, by CT and micro-CT and by collection of histological samples.
- Results: The preliminary results show that SLA-fabricated implants (with or without TCP) were biocompatible and well-tolerated, showing evidence of bone ingrowth and remodeling already at 6 weeks post-implantation. Bone accumulation was continuous in all groups throughout the study. The study is currently at endpoint, with final results yet to be analyzed.
- Conclusions: This study indicates that a functional workflow of fabricating custom-made implants by SLA is achievable and could expedite the process from imaging to implantation, thereby reducing the cost and time of reconstructive surgery in a clinical setting.
EP58
Use of 3-D Printing and Virtual 3-D Imaging to Aid Mandibular Reconstruction: Experience and Methodology at Our Centre and Comparison with Standard Methods of Reconstruction
- Samarth Gupta, Pradeep Goil
- SMS Hospital Jaipur, Jaipur, India
Abstract
- Introduction: Free fibula flap is now regarded as the gold standard for reconstruction following oncological mandibular resection. This is owing to the uniform bicortical thickness, density, long vascular pedicle and less donor site morbidity of the fibular graft. However, the results are confounded due to inappropriate estimate of defect or inappropriate angulation of osteotomy. 3-D printing has been a tool which is being vastly employed in various specialties in the field of medicine. It can hence be an effective tool to help in preplanning osteotomies and implant designs.
- Methods: Patients were categorized in two groups, one of which underwent conventional free fibula flap and the other group consisted of those where 3-D printing was used. The study was conducted over the span of 4 years from 2016–2019. Aesthetic and functional outcome was measured by patient-given sheets as well as preoperative and postoperative 3-D scans. Furthermore, the mean operative time was also measured in both of these groups.
- Results: Comparative study of 3-D scans and the score sheets clearly demonstrated the better functional and aesthetic outcome of 3-D printing. The modality also helped reduce surgeons’ mean operative time where total surgery time was 3.0 ± 0.37 hours in the cases group 5.60 ± 0.3 hours in the control group.
- Conclusion: 3-D printing and virtual 3-D imaging have the potential to improve the quality of mandibular reconstruction, giving better aesthetic and functional outcome. Besides, it also reduces the operative time and gives us a chance to use preoperatively designed, patient-customized implants. 3-D printing obviates the need for speculation and gives exact measurements in all dimensions. We believe that this tool should be incorporated often in free fibula flaps for mandibular reconstruction.
EP64
In-Hospital 3-D Printing Facility for Mandibular Reconstruction Using Fibula Flap: An Italian Experience
- Claudia Borbon1, Andrea Novaresio2, Emanuele Zavattero1, Guglielmo Ramieri1
- 1Città della Salute e della Scienza Hospital, Division of Maxillofacial Surgery, Torino, Italy. 2Politecnico di Torino, Department of Management and Production Engineering, Torino, Italy
Abstract
- Objectives: Recently, computer-assisted surgery has had a positive impact on the accuracy and quality of the mandibular resection and reconstruction using fibula flap. Cutting guides produced using computer-aided design (CAD) and computer-aided manufacturing (CAM) technologies aim to increase the benefits to patients by improving the accuracy and shortening the operating time. The aim of this study was to explore whether the production of in-hospital, low-cost surgical cutting guides would be possible and to assess different cutting guide shapes to facilitate the surgery and the application with surgical drilling instruments.
- Methods: The study included 8 patients who underwent a partial resection of the mandible from July 2017 to March 2019. Using free CAD software, we designed surgical cutting guides for the mandible and fibula and used these to perform virtual mandibular segmental osteotomies and fibula transplants in these 8 model surgeries. The cutting guides were determined by the surgeon, considering clinical aspects of intraoperative feasibility. The mandible, the fibula and the guides were printed using a 3-D printer.
- Results: Sixteen virtual osteotomies were performed using free software. 22 jigs were designed using the described procedure. At least 8 hours were necessary for designing and printing the mandibular and the fibular cutting guides. The fit of the guides was excellent for all the operations. The footprint of the jigs was satisfactory for all cases.
- Conclusions: We demonstrated that virtual planning and the 3-D printing of jigs for mandibular reconstruction is reliable with the aid of an in-hospital 3-D laboratory and a short learning curve. We also demonstrated that different jigs with different shapes could easily be produced with benefit during surgery compared to those produced by commercial companies.
EP65
CAD/CAM and Computer-Assisted Piezoelectric Surgery for Treating Intraosseous Facial Hemangiomas
Miriam Estero, Alicia Dean, Francisco Alamillos, Susana Heredero
Hospital Universitario Reina Sofía, Córdoba, Spain
Abstract
- Objectives: Intraosseous hemangiomas are uncommon (0.5 to 1% of all intraosseous tumors), more frequent in females and most likely in the fourth decade of life. The most common etiology is believed to be prior trauma to the area. Generally located in the vertebral skeleton, they can also present in the calvarium and facial bones. In the head, the most common site is the parietal bone, followed by the mandible, malar and zygomatic regions. The objective of this work is to present our experience treating these lesions using computer-aided design/computer-aided manufacturing (CAD/CAM) and computer-assisted piezoelectric surgery, and to describe their clinical and radiological characteristics.
- Methods: This is a clinical series of patients treated in our department between June 2017 and May 2019. Preoperative planning was done using iPlan 3.0 (BrainLab®). Custom-made polyetheretherketone (PEEK) implants were designed according to the specific defects predicted in each patient. Intraoperative navigation (BrainLab® Kolibri navigation system) was used to guide resections as planned. Osteotomies were performed with piezoelectric surgery and continuous three–dimensional tracking of the piezoelectric device in real time.
- Results: The study sample comprised 3 females and 1 male, with an average age of 49 years old (range, 36–56). 3 hemangiomas were located in the orbital region and 1 in the malar region. In all cases, patients presented inflammation of the area, and 2 presented dystopia. None of them reported a history of facial trauma. Embolization prior surgery was performed in 2 patients. Minor adjustments were needed in order to better adapt the PEEK prostheses to the final defects.
- Conclusions: Virtual planning facilitates preoperative design and manufacture of PEEK prostheses that can be adapted to the defect right after the resection. Computerassisted piezoelectric surgery makes it possible to perform osteotomies according to the preoperative planning, easing the prosthesis adaptation during the surgery.
TOPIC: AESTHETIC SURGERY
EP66
The Submandibular Incision: Changing Lanes
- Amr Ghanem
- Ain Shams University, Cairo, Egypt. British University in Egypt, Cairo, Egypt
Abstract
- The submandibular incision has been a valuable tool in head and neck surgery since 1934. It has been advocated in the fields of mandibular trauma, resection and reconstruction of mandibular tumors as well as in accessing the C2-C4 disc space. The anatomy of the marginal mandibular as well as cervical branches of the facial nerve represent the pertinent anatomy relevant to this incision. In this study we attempt to execute the incision at a greater distance from the mandibular inferior border. The modification attempts to place the incision in a more aesthetically pleasing position while also protecting the terminal branches of the facial nerve.
- Materials and methods: A group of five patients were treated applying the modified submandibular approach. 3 cases were managed for resection of an Ameloblastoma and 2 patients were managed for a comminuted fracture of the mandible. All patients were followed up clinically at regular intervals. Two panels assessed the aesthetic result of the incision. One panel was formed of specialized OMFS and the other panel was formed of nonspecialized laypersons. The panels were shown a PowerPoint presentation showing the postoperative result for the patients who had the submandibular incision performed at a standard 2 cm distance from the inferior border of the mandible technique. The presentation also showed cases operated utilizing the incision placed at distance greater than 3 cm from the inferior border.
- Results: No neurosensory disturbances were recorded in the operated five cases. The assessing panels reported enhanced aesthetic results.
- Conclusion: Placing the submandibular incision within the natural skin crease in the neck places it farther from the mandibular inferior border. This enhances the aesthetic aspect while minimizing the chance of facial nerve damage.
TOPIC: TRAUMA
OR05
CT Scan Consideration for Occult Skull Fracture in Paediatric Head Trauma
- Janhvi Shah, Stephanie Agar, Sukhpreet Dubb, Paayal Shah, Tahir Mirza
- Luton and Dunstable Hospital, Luton, United Kingdom
Abstract
- Objectives: Pediatric head injuries commonly present to the emergency department, with forehead lacerations in particular being frequently referred to the oral and maxillofacial team. Assessing the GCS and neurological status of pediatric patients is particularly challenging. There remains marked ambiguity regarding computed tomography (CT) imaging in children without obvious signs of traumatic brain injury. We present a case series of three patients (aged less than three years) presenting to our unit with forehead lacerations following a fall. All cases had normal GCS, no obvious neurology, and were listed for wound closure under general anesthesia. Intraoperatively, these patients were found to have underlying skull fractures necessitating emergency CT scanning while under general anesthesia. All cases were discussed with neurosurgery, with one patient requiring transfer and emergent operative management.
- Methods: Retrospective analysis was performed. Current guidelines were reviewed, and a literature review was performed to identify factors that may aid in identification of occult skull fractures in the context of pediatric head trauma. These guidelines included those published by the National Institute for Health and Care Excellence (NICE), the Royal College of Radiologists, the British Society of Pediatric Radiology, and international guidelines published in Scandinavia and Canada.
- Results: Despite the subsequent discovery of skull fractures under general anesthesia, none of our patients satisfied present absolute indications for CT scanning when all present guidelines were consulted. There exist a number of helpful factors that are not common across United Kingdom guidelines but present in others, including hematoma of the skull and lacerations greater than 5 cm among others.
- Conclusion: The assessment of pediatric head trauma patients remains difficult when assessing features such as headaches, focal neurology and amnesia. A high index of suspicion, formal examination under anesthesia, and communication with the radiology department are imperative to avoid missing occult injury potentially resulting in brain injury.
OR06
Monocortical vs. Bicortical Plating for Mandible Fractures of the Angle, Body, and Parasymphysis
- Richard Guidry1, Jourdain Artz2, Ian Wisecarver3, Silpa Sharma2, Hugo St. Hilaire2,Gerhard Mundinger2,4
- 1Louisiana State University School of Medicine, New Orleans, United States. 2Division of Plastic and Reconstructive Surgery, Louisiana State University Health Sciences Center, New Orleans, United States. 3Department of Plastic Surgery, University of Texas Southwestern, Dallas, United States. 4Division of Plastic and Reconstructive Surgery, Children’s Hospital of New Orleans, New Orleans, United States
Abstract
- Objectives: Currently, two dominant philosophies for open reduction internal fixation (ORIF) guide management of mandibular fractures. Arbeitsgemeinschaft für Osteosynthesefragen (AO) considers use of large plates with bicortical screws for rigid fixation. However, Champy system advocates use of smaller plates stabilized with monocortical screws around “ideal lines of osteosynthesis.” Our study was performed to compare characteristics related to differing screw insertion.
- Methods: Data was collected retrospectively via review of electronic medical records from two academic institutions in New Orleans. Patients who underwent ORIF of mandible from July 2010 to December 2016 were included. Procedure times, postoperative maxillomandibular fixation (MMF) duration, complications, and antibiotic prophylaxis related to bicortical, bicortical with monocortical tension bands, and monocortical ORIF were compared. Stata/IC was used to determine significant association.
- Results: 77 of 172 mandibular fractures, in 58 patients (mean age 36.9 ± 13.5 years), had complete medical records for patient demographics and fixation method. Smoking (62.0%) and alcohol use (50.0%) were prevalent. Assault (55.7%) was the most common mechanism of injury. Fracture treatment were: 31 bicortically, 30 bicortically with tension bands, and 16 monocortically. For isolated angle and parasymphysis fractures, monocortical fixation had shorter procedure times (83.0 ± 32.8 min; 71 ± 0 min) than both bicortical (220.2 ± 103.4 min; 170.0 ± 88.8 min) and bicortical with tension bands (150 ± 0; 155.2 ± 36.0) (p < 0.05). Postoperative MMF duration, complication rates, and infections related to antibiotic prophylaxis were comparable between techniques.
- Conclusion: Monocortical and bicortical fixation resulted in similar complication rates; however, intraoperative procedure times for monocortical plating was shorter, aligning with the recent clinical shift toward using less obtrusive hardware for technically easier procedures and similar complications. However, both techniques are safe, reliable, and should be tailored to the patient situation and daily practice. Considering our limited sample, further investigation is recommended for designation of one technique over another.
OR26
Facial Self-Inflicted Gunshot Wounds: Analysis of Demographics, Injury Patterns, and Costs of Treatment in 70 Patients
- Jourdain Artz1, Matthew Bartow1, Silpa Sharma1, Radbeh Torabi1, Mark Stalder1, Hugo St. Hilaire1, Gerhard Mundinger1,2
- 1Division of Plastic and Reconstructive Surgery, Louisiana State University Health Sciences Center, New Orleans, USA. 2Division of Plastic and Reconstructive Surgery, Children’s Hospital of New Orleans, New Orleans, USA
Abstract
- Objectives: In U.S., suicide by firearms is increasingly recognized as a major public health concern. We sought to quantify demographics, facial injury patterns, insurance status, and healthcare costs of self-inflicted facial gunshot wounds.
- Methods: Self-inflicted facial gunshot wounds between July 2012 and July 2017 at a level 1 trauma center was reviewed retrospectively. Cost data was evaluated according to standard cost-reporting metrics. Main determinant outcome between predictor variables was death. Descriptive and outcome statistics were compared with student’s t-tests (significance level p ≤ 0.05, two-tailed). Facial fracture location was classified by facial thirds as upperface, midface, or mandible.
- Results: 70 patients met inclusion criteria: 26 survived (37.1%) and 44 expired (62.9%). Mean Glasgow coma scale score was significantly higher and injury severity score scale was significantly lower in surviving patients. Uninsured patients were significantly more prevalent in the group that died (3.8% vs 23.9%, p = 0.001), and lack of insurance carried 10.9-fold higher odds of death. Mean treatment cost for surviving patients was significantly higher ($333,296.7 vs $21,466.7, p = 0.009). Hospital room costs accounted for 28.3% of total cost (average: $38,462.10), followed by surgical costs at 20.5% (average: $27,912.60). Surviving patients typically had combined central midface injuries involving two or more facial thirds (66.7% vs 47.1%, p = 0.279). Midface and mandible fractures were statistically more common in surviving patients than expired patients (29.5% vs. 21%, p = 0.038; 9% vs 2.8%, p = 0.002, respectively).
- Conclusion: Results from larger series of self-inflicted facial gunshot wounds confirm demographic, social determinants, and injury patterns associated with successful suicide attempts suggested by smaller studies. Failed suicide attempts with isolated firearm injuries to the craniofacial skeleton carry significant monetary costs to the United States health care system. Besides investment in prevention and psychiatric treatment for suicidal patients, value of care following suicide attempts with firearms can best be increased by minimizing hospitalization costs and improving surgical outcomes.
TOPIC: BASIC RESEARCH
OR09
A Digital Surface Scan to Identify Skin Perfusion Disorders
- Julie Deferm1, Frank Baan2,3, Ruud Schreurs4,5, Robin Willaert6,7, Thomas Maal5, Gert Meijer8,9
- 1Oral and Maxillofacial Surgery Department, Radboudumc, Nijmegen, Netherlands. 23D lab, Radboudumc, Nijmegen, Netherlands. 3Depatment of Orthodontics and Craniofacial Biology, Radboudumc, Nijmegen, Netherlands. 4Department of Oral and Maxillofacial Surgery (OMFS), University of Amsterdam, Amsterdam, Netherlands. 53D lab, Radboudumc, Nijmegen, Netherlands. 6Department of Oral and Maxillofacial Surgery, University Hospital Leuven, Leuven, Belgium. 7Department of Head and Neck Surgery, Ghent University, Gent, Belgium. 8 Oral and Maxillofacial Surgery Department, Radboudumc, Nijmegen, Netherlands. 9Department of Implantology and Periodontology, Radboudumc, Nijmegen, Netherlands
Abstract
- Objectives: Monitoring of vascular perfusion of transferred tissue is essential in reconstructive surgery to recognize early flap failure. The aim of this study is to evaluate the capability of a digital surface scanner to detect vascular perfusion disorders through monitoring of skin color changes.
- Methods: In a feasibility study with ten participants, a total of 160 surface scans of the forearm skin were performed with TRIOS® 3D Intraoral Scanner. Vascular compromise was simulated by alternated occlusion of the arterial and venous blood supply on different time points. Skin color changes were shown according to the Hue, Saturation and Value color scale. Color differences were analyzed with a paired t-test.
- Results: Significant differences are observed between colors of the normal skin compared to the vascular compromised skin (p < 0.01). The surface scanner can distinguish between an arterial occlusion and a venous congestion (p < 0.01).
- Conclusion: A digital surface scan of the skin is a useful, noninvasive tool to detect early vascular perfusion disorders. This measurement can be used in future studies to objectify the vascularization of transferred tissue and to improve rates of surgical salvage.
TOPIC: ORTHOGNATHIC SURGERY
OR12
Beautiful Face Pattern
- Mikhail Solovyov1,2, Irina An2
- 1St. Petersburg State Medical University, St. Petersburg, Russian Federation. 2City Hospital No. 2, St. Petersburg, Russian Federation
Abstract
- Aesthetic result of orthognathic operations remains unstable, despite many planning methods. Literature analysis showed there is no description of face proportions in anteroposterior direction.
- Methods: To determine proportions, the plane Rondist (Ro) was introduced: a horizontal plane corresponding to the natural facet dividing the head into lower and upper parts, three planes perpendicular to it, passing through points Sn (subnasal), Gb (glabella) and Tf (frontal tubercle) and LF plane (lower third of face). Also, concepts of profile depth (PD) as ratio of distances Sn-Gb to Gb-Tf and lower face inclination (LFI) as the angle between LF/Ro are introduced.
- Analysis of photographs of 122 women of the most beautiful faces from various ratings was carried out. The following groups were distinguished: modern women of Caucasian race (52), Caucasian race of the 20th century (33), Mongoloid race (19), Negroid race (18). For each face, a profile photo was found and PD and LFI were identified. A statistical analysis was carried out in the StatFi program. The general statistics were calculated, and the normality of distribution was checked by nonparametric statistical criteria.
- Results: In the main group, PD value was 0.97 + /− 0.016. LFI value was 93.3 + /− 0.6. Both values corresponded to Gaussian distribution. In other groups, the values were distributed respectively: 2 group PD 0.97 + /− 0.02, LFI 93 + /− 0.8; 3 group PD 0.96 + /− 0.02, LFI 93.6 + /− 1.1; 4 group PD 0.97 + /− 0.03, LFI 92.6 + /− 1.1. Statistical analysis showed all distributions belong to general population.
- Conclusions: description of new plane ‘Rondist’ of face and cephalometric analysis based on it made it possible to identify criteria for facial beauty, which are intuitively determined by most people and not dependent on race or historical era. The results are used in planning orthognathic operations and make it possible to obtain a stable aesthetic outcome.
OR14
Concomitant Temporomandibular Total Joint Reconstruction and Orthognathic Surgery
- Emanuele Zavattero, Giovanni Gerbino, Claudia Borbon, Guglielmo Ramieri
- Città della Salute e della Scienza Hospital, Division of Maxillofacial Surgery, Torino, Italy
Abstract
- Objectives: Alloplastic joint prostheses have been used in the treatment of severe diseases of the temporomandibular joint (TMJ) for many years. TMJ disorders or pathology and dentofacial deformities commonly coexist. The TMJ pathology could be the causative factor of the deformity or develop as a result of the jaw abnormality or both may develop independently of each other. We report a single stage technique for replacement of an affected joint using custom-made prosthesis and orthognathic surgery to change or correct the occlusion. Technical aspects and the indications will be discussed.
- Methods: 24 prostheses were placed in 14 patients who underwent unilateral or bilateral alloplastic total TMJ replacement with mandibular repositioning and orthognathic surgery (18 Lorenz/Biomet, 4 TMJ Concepts, 2 CAD skills). Data collected from the patient records included age, gender, etiology, number of previous TMJ operations, treated TMJ, hospital stay, complications. Preoperative and follow-up assessment for TMJ pain, diet consistency, and maximal interincisal opening was performed. Accuracy of the maxillamandibular movements and of the fit of the implants were recorded. The minimum follow-up was one year.
- Results: The prosthetic components used in these cases provided excellent anatomical reconstruction. All patients presented a noticeable improvement in maximal interincisal opening, TMJ pain, and diet consistency at follow-up compared to preoperative situation. Accuracy measurement shows an excellent fit of the implants and the movements had a high accuracy compared to the planning in 13 patients out of 14. Occlusion and aesthetical changing remain stable at one-year follow-up.
- Conclusions: Patients with TMJ disorders and concomitant dentofacial deformities may benefit from one-stage corrective surgical intervention. Computer-assisted surgical simulation decreases the preoperative workup time and increases the accuracy and safety of surgery.
TOPIC: ORAL SURGERY/IMPLANTS
OR16
Surgical Outcome Following Third Molar Surgery: The Role of Case Selection Among Undergraduate Dental Students
- Izzati Nabilah Ismail, Mohammad Faiz Razali, Iqbal Ahliun, Nor Adilah Harun
- Faculty of Dentistry, International Islamic University Malaysia, Kuantan, Malaysia
Abstract
- Objectives: Lower third molar surgery in undergraduate dental education is limited to selection of appropriate cases suited for their level of clinical experience to reduce the risk of complications. This study is aimed at identifying the operative details and post-operative outcomes in different types of third molar impaction among dental students.
- Methods: 50 cases of lower third molar surgery performed by undergraduate dental students were recruited and divided into Pell and Gregory, and Winter’s classification. Preoperative and postoperative facial measurements, neurosensory assessment, mouth opening, Oral Health Impact Profile-14 (OHIP 14), and postoperative complications were obtained.
- Results: There was no significant difference in the operative time for different types of impaction in Pell and Gregory and Winter’s classifications with mean operative time of 83 minutes. Generally, the postoperative outcomes revealed significant increase in facial swelling, reduction in mouth opening, and increase in OHIP-14 score (p < 0.05). In comparing pre- and postoperative outcomes within Pell and Gregory classification, Class 1A showed significant increase in swelling postoperatively (364.3 mm vs. 376.0 mm) (p < 0.008) and significant reduction in mouth opening (47.7 mm vs. 41.3 mm). Significant reduction in mouth opening was also reported in Class 2A (44.9 mm vs. 35.7 mm) and Class 2B (44.5 mm vs. 33.3 mm) (p < 0.05). In comparing within Winter’s classification, significant reduction of mouth opening was observed in all types of Winter’s impaction (p < 0.05). No significant postoperative complications were reported.
- Conclusions: Different classes of Pell and Gregory and Winter’s classification of impaction did not strongly dictate the outcomes of third molar surgery. In general, no severe complications were observed in all surgical procedures done by undergraduate dental students under supervision when cases selected were limited to Pell and Gregory class 1A, 1B, 2A, 2B, and Winter’s classification of mesioangular, vertical and horizontal.
TOPIC: FACIAL DEFORMITY SURGERY
OR20
Ipsilateral Transnasal Medial Canthopexy to Correct Secondary Telecanthus after Naso-Orbito-Ethmoid Fracture
- Yu-Ying Chu
- Chang Gung Memorial Hospital, Tauyuan, Taiwan
Abstract
- Background: Telecanthus results from medial canthal tendon (MCT) disruption, which can result from traumatic nasoorbitoethmoid (NOE) fractures. Several methods, using different anchoring materials, incision approaches, or fixation positions, have been proposed for MCT reconstruction. Herein, we report our experience in treating MCT disruption using ipsilateral transnasal medial canthopexy with a Y-V approach.
- Methods: Between 2008 and 2017, seven patients with traumatic naso-orbito-ethmoid (NOE) fractures underwent ipsilateral transnasal MCT fixation with Y-V epicanthoplasty. The length ratio, defined as the length of the affected side divided by that of the normal side, was calculated preoperatively and postoperatively. A modified Y-V epicanthoplasty incision was made, after first marking the site in the apex of the caruncular fornix. The nasal wall was exposed and the MCT was accessed carefully. Bulky MCT tissue was trimmed. The lacrimal bone was ground using a bur, creating a concave shape to reposition the MCT, and two holes were drilled into the ipsilateral lacrimal fossa and frontomaxillary process. The MCT was fixed to the frontomaxillary process using number 2 transnasal wire, which was secured by a 6 mm screw. Finally, the Y-V epicanthoplasty was repaired using 5.0 nylon.
- Results: The preoperative length ratio (mean ± standard deviation: 83.3% ± 5.99%; range: 73.7%–92.0%) was significantly lower than the postoperative length ratio (mean ± standard deviation: 99.4% ± 0.63%; range: 98.5%– 100%) (p < 0.05). No major complications were observed, with an average of 13 months of follow-up.
- Conclusions: Ipsilateral transnasal wiring fixation with Y-V epicanthoplasty is a useful and adequate method for MCT reconstruction after NOE fractures, without remarkable complications.
TOPIC: RECONSTRUCTION
OR31
Role of Nonvascularized Iliac Crest Graft as an Autogenous Bone Grafts for Mandibular Reconstruction
- Saif Ullah Khattak1, Muhammad Jamal2, Kaleem Ullah3, Zafar Khan4
- 1Mardan Medical Complex, Mardan, Pakistan. 2Islamabad Medical and Dental College Islamabad, Islamabad, Pakistan. 3KRL Hospital, Islamabad, Pakistan. 4College of Dentistry, University of Jouf, Sakaka, Saudi Arabia
Abstract
- Various functional and esthetic defects in the oral and maxillofacial regions are treated according to their extent and requirements. Any good reconstruction in the maxillofacial region should be a simple suitable procedure which achieves best functional and cosmetic results while having least donor site morbidity. Oral and maxillofacial reconstruction with good functional and cosmetic results when autogenous bone grafts are used.
- Objectives: The purpose of this study was to determine the role and reliability of non-vascularized iliac crest graft as an autogenous bone graft for mandibular reconstruction.
- Methods: A descriptive case series study carried out on seventy patients having bony mandibular defects reconstructed with the autogenous non-vascularized iliac crest graft. Graft success were noted in terms of absence of infection and graft resorption in postop visits.
- Results: Success rate found in the study was 84.3%. Only 15.7% of the cases showed graft failure in terms of infection and graft resorption. There was no hypertrophic scar formed and all donor sites were primarily closed.
- Conclusion: The autogenous non-vascularized iliac crest grafts proved to be a reliable method for the reconstruction of the bony mandibular defects with good esthetic and functional results.
OR32
Three-Dimensional Characterization of the Position of the Globe in the Orbit
- Robin Willaert1,2, Eman Shaheen3,1, Julie Deferm4, Hubert Vermeersch5, Reinhilde Jacobs6,7,Ilse Mombaerts8
- 1Department of Oral and Maxillofacial Surgery, University Hospitals Leuven, Leuven, Belgium. 2Department of Head and Neck Surgery, Ghent University Hospital Ghent, Belgium. 3OMFS IMPATH Research Group, Department of Imaging and Pathology, KU Leuven, Leuven, Belgium. 4Department of Oral and Maxillofacial Surgery, Radboud University Hospital, Nijmegen, Netherlands. 5Department of Plastic and Reconstructive Surgery Ghent University Hospital, Ghent, Belgium. 6OMFS IMPATH Research Group, Department of Imaging and Pathology, Faculty of Medicine, KU Leuven, Leuven, Belgium. 7Department of Dental Medicine, Karolinska Institutet, Huddinge, Sweden. 8Department of Ophthalmology, University Hospitals Leuven, Leuven, Belgium
Abstract
- Background: In the diagnosis and management of orbital disorders, the standard methods to assess globe positioning in the orbit include Hertel exophthalmometry and computerized tomography (CT) imaging, allowing to measure proptosis and enophthalmos based on the distance between the orbital lateral rim and corneal vertex. We aimed to design a method to measure the position of the globe in the axial, coronal and sagittal plane and independent from orbital bony and corneal references, using CT data and three-dimensional (3-D) reconstruction technology.
- Methods: Orbital CT data were retrieved from 10 control subjects (20 orbits) without orbital disease. With 3-D reconstruction technology, the center of the globe was defined and the globe position within the orbit was depicted in the three dimensions of space. The 3-D CT method was subsequently applied on the CT data of 5 patients (7 orbits) with thyroid orbitopathy before and after orbital decompression surgery including removal of the lateral orbital margin, to evaluate the postoperative 3-D shift of the globe.
- Results: The 3-D CT measurements of the globe position showed a low interand intra-observer variability (ICC > 0.99, 95% CI [0.97; 1.00]) . In the decompressed orbits, there was a statistically significant difference of the globe position along the anterior-posterior axis (p < 0.001, 95% CI [0.63; 3.66]). The amount of the globe shift corresponds with the amount of preoperative proptosis.
- Conclusions: The 3-D CT method allows the measurement of the globe position and postdecompression shift without the use of landmarks from the orbital lateral rim and corneal vertex. By defining the intra-orbital position of the globe in three orthogonal planes, the method can be useful in the assessment of orbital trauma or for planning orbital reconstructive surgery.
OR36
Reconstruction of Craniofacial Structural Defects Through Patient-specific 3-D-Printed Custom Beta Tricalcium Phosphate Scaffolds: Development of a Translational Porcine Model
- Richard Guidry1, Silpa Sharma2, Daniel Yoo2,Luis Marrero3, Catherine Takawira4, Bruce Bunnell5, Mandi Lopez4, Gerhard Mundinger2,6
- 1Louisiana State University School of Medicine, New Orleans, USA. 2Division of Plastic and Reconstructive Surgery, Louisiana State University Health Sciences Center, New Orleans, USA. 3Department of Orthopedic Surgery, Louisiana State University Health Sciences Center, New Orleans, USA. 4Laboratory for Equine and Comparative Orthopedic Research, Louisiana State University, Baton Rouge, USA. 5Center for Stem Cell Research and Regenerative Medicine, Tulane University School of Medicine, New Orleans, USA. 6Division of Plastic and Reconstructive Surgery, Children’s Hospital of New Orleans, New Orleans, USA
Abstract
- Objectives: 3-D-printed bone scaffolds can reconstruct specific craniofacial bony defects and can be commercially printed based on CT scans within days. Additional seeding of scaffolds with autologous stem cell populations may enable improved regeneration of normal bony architecture. However, ability of such scaffolds to regenerate loadbearing bone is untested in large animal models.
- Methods: We created a 6 cm critical load-bearing defect in the left mandibular angle and a 1.5 cm noncritical, non-load bearing defect in the right zygomatic arch in Yucatan pigs. In the control arm (n = 4), no construct was placed. Based on promising in vitro cell adhesion and viability assays, beta-tricalciumphosphate (βTCP) defect-specific bone scaffolds (KLS Martin, Mulheim, Germany) were 3-D–printed from preoperative CT scans and placed into bony defects in the experimental arm (n = 8). Serial CT scans were captured at three and six months postoperatively. At the six-month endpoint, bone regeneration was evaluated through histologic and micro-CT analysis. Additional bone-strength testing was performed on implant cores.
- Results: All animals reached study endpoint. In the negative-control group, CT and gross examination of defects revealed incomplete heterotopic ossification. Micro-CT confirmed presence of dystrophic bone formation at ostomy sites with disruption of normal bone architecture. Trichrome staining showed disorganized, porous bone in experimental as compared to control samples. In the experimental arm, scaffolds maintained high fidelity to the preoperative surgical plan with CT evidence of bone regeneration at three months. Evaluation at study endpoint demonstrated bone regeneration throughout the implants with bony integration at implant/native bone interfaces. Histologic, microcomputed tomography (micro-CT) and biomechanical testing is ongoing.
- Conclusion: Our model has broad applicability in preclinical evaluation of bone regeneration scaffolds. 3-Dprinted, defect-specific βTCP scaffolds demonstrated biocompatibility with bone regeneration and osseointegration. Insights from this model may realize the possibility of reconstructing bony defects by harnessing the power of 3-D printing and autologous stem cell seeding for congenital, post-traumatic and oncologic reconstruction.
OR37
Optimizing Mandibular Reconstruction for Osteoradionecrosis: Virtual Surgical Planning Facilitates Accurate Reconstructions and Curative Outcomes
- Gerhard Mundinger1,2, Matthew Bartow1, Rizwan Aslam3, Silpa Sharma1, Hugo St. Hilaire1, Mark Stalder1
- 1Division of Plastic and Reconstructive Surgery, Louisiana State University Health Sciences Center, New Orleans, United States. 2Division of Plastic and Reconstructive Surgery, Children’s Hospital of New Orleans, New Orleans, United States. 3Department of Otolaryngology, Tulane University, New Orleans, United States
Abstract
- Objectives: Mandibular osteoradionecrosis (ORN) can be a devastating complication of radiation therapy for head and neck malignancies. ORN can require radical surgical excision and reconstruction with vascularized bone. Virtual surgical planning (VSP) has become standard allowing for decreased operative time, and improved reconstruction accuracy. However, there is no defined standard for adequate resection margins that prevent ORN recurrence. We believe preoperative VSP along with a defined margin allows for accurate and efficient reconstructions, and effective prevention of ORN recurrence.
- Methods: A retrospective review of patients at our institution who underwent mandibular ORN resection and reconstruction using free fibula flap (FFF) between May 2011 and January 2019 was conducted. VSP was performed, and bony resections were based on radiographic extent of disease plus a one-centimeter margin. Demographic data, comorbidities, and anatomic classification of disease were analyzed. Outcomes assessed included ORN recurrence, flap reconstruction success, and reconstruction accuracy based on CT imaging analysis.
- Results: Twenty-five patients met inclusion criteria. Average follow-up time was 15 months. Fourteen patients had a second flap performed simultaneously for coverage along with FFF for a total of 39 free flaps. There were 6 partial flap losses. Of ten possible dimensions analyzed for reconstructive accuracy, only the intergonial distance demonstrated a significant difference between pre and postoperative imaging (p = 0.025). Clinically identifiable preoperative skin pathology correlated positively with a greater number of mandibular segments requiring resection and reconstruction (p = 0.039). There were no ORN recurrence cases.
- Conclusion: VSP has well-defined advantages for mandibular reconstruction using FFF: reduced operative times and bony construct accuracy. Though little has been reported regarding VSP for complicated reconstructions of mandibular ORN, our results reinforce the accuracy this technique can facilitate. More importantly, results of this study provide solid data to support a onecentimeter margin of resection beyond radiographically identifiable disease with reliable and curative results for mandibular ORN.
OR38
Precision in Reconstruction with Fibula Free Flaps for Defects Including the Angle of the Mandible
- Maria Isabel Falguera, Alicia Dean, Susana Heredero
- Hospital Universitario Reina Sofía, Córdoba, Spain
Abstract
- Objective: Accuracy may be difficult to obtain in mandible reconstruction when the angle is included, because both the horizontal and vertical planes must be considered. The aim of this study is to evaluate precision in reconstruction with three different methods.
- Methods: This is a retrospective study of patients who underwent mandible reconstruction including the angle with fibula free flaps. Bone fixation was performed using computer aided designed and manufactured (CAD-CAM) titanium plates, manufactured preformed titanium plates for mandible reconstruction (Synthes), or free hand bent titanium plates. CT scans were analyzed with iPlan (BrainLab). In the postoperative CT, the reconstructed side was compared to either the mirror uninjured healthy hemimandible, or to the original one imported as a Standard Tesellation Language object from the preoperative CT, if its shape was not disturbed. Precision was evaluated by measuring the maximal difference in vertical height (VD) of the mandible ramus and the maximal difference in the position of the mandible body in the horizontal plane (HD).
- Results: A total of 22 patients (11 males, 11 females) with a mean age of 51 ± 7 years were included. 1 patient underwent reconstruction because of a gunshot injury, 2 because of radionecrosis, and the other because of oncological ablative surgery.
- Statistically significant differences were found between the three methods of reconstruction, being higher in the group of patients reconstructed with free hand bent titanium plates. VD differences were statistically higher in reconstructions including the condyle or the highest part of the ramus.
- Conclusions: CAD-CAM plates increase accuracy in the horizontal plane. However, our results suggest that preformed titanium plates provide better precision than the free hand bent ones, comparable to the CAD-CAM plates, but being a more affordable option. Also, accuracy in the vertical plane is related to the height of the ramus involved.
OR39
Microsurgical Repair of Trigeminal Nerve Injuries. Our Experience
- Daniel Jerez1,2, German Laissle1,3,Carlos Fuenzalida1,3,2, Loreto Castellon2,3, Jaime Mayorga2,4, Camila Avila5
- 1Clinica Bupa Santiago, Santiago, Chile. 2Hospital Dr. Luis Calvo Mackenna, Santiago, Chile. 3Hospital Exequiel Gonzalez Cortes, Santiago, Chile. 4Hospital Militar de Santiago, Santiago, Chile. 5Facultad de Salud y Odontologia, Universidad Diego Portales, Santiago, Chile
Abstract
- Nerve injuries may occur during different oral procedures, being the most common ones during third molar removal, orthognathic surgery, maxillofacial trauma, resection surgery of oral pathologies and on occasions from endodontic therapy or local anesthetic injection. Although, the majority of injuries recover spontaneously, there is a group of patients that without adequate micro-surgical repair cannot recover their sensitivity completely. The objective of this work is to show our experience over the last three years in treating nerve injuries with microsurgical repair. A prospective clinical study of patients who underwent microsurgical repair of trigeminal nerve branches was performed. A total of 23 patients were evaluated for the study, of those, 20 patients met the inclusion criteria, 12 women and 8 men with 16 lesions to the IAN and 4 injuries to the LN. 5 allographic nerves (AxoGen) were used at same time of mandibular reconstruction. Success rate after microsurgical repair was 95%. All the patients were treated by the author. Our experience is similar to large reports in the literature concerning the statistics in incidence, microsurgical repairs and success by treating them with surgically. Microsurgical repair is an accepted technique for treating nerve injuries. From our knowledge, we are the only surgeons in the country treating this type of injuries.
OR59
Nasal Esthetic Surgery in Children: Feasibility and Safety. Corrective Rhinoplasty
- Samia Saied
- Sohag University Hospital, Sohag, Egypt
Abstract
- Rhinoplastic techniques have changed over the years and became more conservative towards tissue reorientation and augmentation rather than resection and reduction. In children, the overlying soft tissue envelope has a thicker layer of subcutaneous fat; the nasal skeleton of an infant is mainly cartilaginous. The growing cartilaginous nasal septum has been demonstrated to be an organizer of midfacial growth.
- There are two significant nasal growth spurts, the first two postnatal years and during puberty when the nose grows faster compared to other periods in lifeIndications of performing nasal surgery in children mainly are: nasal trauma, tumors, dermoid; situations in which the nasal breathing is severely impaired; or the deformity of the nose causes psychological problems, like in the cleft. For every indication, the expected benefits of intervention should be weighed against the possible adverse outcomes on nasal and midfacial growth. In the ideal situation, surgery should be postponed till after the pubertal growth spurt.
- The aim to perform nasal surgery from an aesthetic point of view, (corrective rhinoplasty in children) is to restore the anatomy, function and to promote normal development and outgrowth of the nose.
- Fifty patients were presented to craniofacial unit, plastic surgery department, Sohag Faculty of Medicine, in the last seven years. Their ages ranged from one month to ten years. They presented with different craniofacial anomalies in the nose as nasal dermoid, vascular malformation, tumors and clefts. Reconstruction was done according to their clinical situation.
TOPIC: TEMPOROMANDIBULAR JOINT (TMJ) DISORDERS
OR45
Total Temporomandibular Joint Replacement with Use of Custom 3-D Printed TMJ Prosthetics
- Sergey Epifanov, Dmitry Ruidel’
- Federal state budgetary institution ‘National Medical and Surgical Center named after N.I. Pirogov’ of the Ministry of Healthcare of the Russian Federation, Moscow, Russian Federation
Abstract
- Objective: To estimate the outcomes of surgical treatment of patients suffering from TMJ ankylosis, with use of a custom, 3-D-printed total TMJ prosthetics.
- Materials and methods: The research included a retrospective analysis of 19 patients (16 female| 3 male) with TMJ ankylosis, that underwent total TMJ replacement (21 joints in total - 17 hemiside | 2 bilateral) at The National Medical and Surgical Center named after N.I. Pirogov (Russian Federation), in a 4 year period. The average postoperative patient observation period was 26 months. The fossa prosthesis was made of ultra-high molecular weight polyethylene and the condyle was made from titanium alloy. In 7 patients (primary group) we used 3-D-printed condyle prosthetics (5 female | 1 male, 7 joints in total). In the control group, patients underwent an installation of milled condyles. The joint fossae prosthetics in both groups of patients were manufactured by milling.
- Results: Before surgical treatment, average MIO of patients participating in the primary group, was 13.5 mm (IQR = 5, 20 mm). In the post-op period it increased up to 32 mm (IQR = 29, 42 mm). The average mandibular lateral excursion improved from 0.4 mm up to 2.1 mm on the right side and from 0.9 to 1.5 mm on the left. The control group showed results of MIO increase from 13.5 mm (IQR = 5, 20 mm) before surgery, to 32 mm (IQR = 29, 42 mm after surgery. The average lateral excursion increased from 0.7 mm to 22 mm on the right and from 0.7 mm to 1.3 mm on the left. Patients’ state was estimated with analog scaling: TMJ pain head and facial pain TMJ function, diet and general state. Positive dynamics were observed by any definition.
- Conclusion: The use of custom 3-D-printed total TMJ prosthetics in patients with TMJ ankylosis is a common method aimed at improvement of TMJ function, pain management, an overall increase of life quality.
TOPIC: 3-D PLANNING
OR54
Computer-Aided Design and Computer-Aided Manufacturing (CAD/CAM) for Proportional Condylectomy
- Daniel Jerez1,2, German Laissle1,3,Loreto Castellon2,3, Carlos Fuenzalida1,2,3, Jaime Mayorga2,4, Camila Avila5
- 1Clinica Bupa Santiago, Santiago, Chile. 2Hospital Dr. Luis Calvo Mackenna, Santiago, Chile. 3Hospital Exequiel Gonzalez Cortes, Santiago, Chile. 4Hospital Militar de Santiago, Santiago, Chile. 5Universidad Diego Portales. Facultad de Salud y Odontologia, Santiago, Chile
Abstract
- With the development of computer aided planning we have been able to be more accurate in orthognathic surgery procedures in patients with complex maxillomandibular asymmetries. Computer software allows the surgeon to plan the surgery and also design cutting guides to reproduce what has been planned. In cases of asymmetries due to condylar hyperplasia, virtual surgical planning allows the precise definition of the level of a proportional condylectomy.
- Purpose: To present a protocol for proportional condylectomy using virtual surgical planning and cutting guides designed by the surgeon.
- Patients and method: This is a prospective study. CT-scans were taken from all patients. Three-dimensional mirroring was performed to generate a replica to estimate the level of the condylectomy. A custom-made 3-D-printed surgical guide was designed for the condylar neck to reproduce the virtual plan. A control CT-scan was taken 1 month after surgery. Heat maps and 3 measurements were made to determine the precision of the surgery.
- Results: 23 patients were included in the study. Measurements and surface deviation color showed precision of less than 1 millimeter from what was planned.
- Discussion and conclusion: By using CAD/CAM technology we were able to reproduce and make proportional condylectomies in patients with condylar hyperplasia. Our results show that is feasible to reproduce. A presentation of the protocol, statistical analysis and clinical cases will be made.
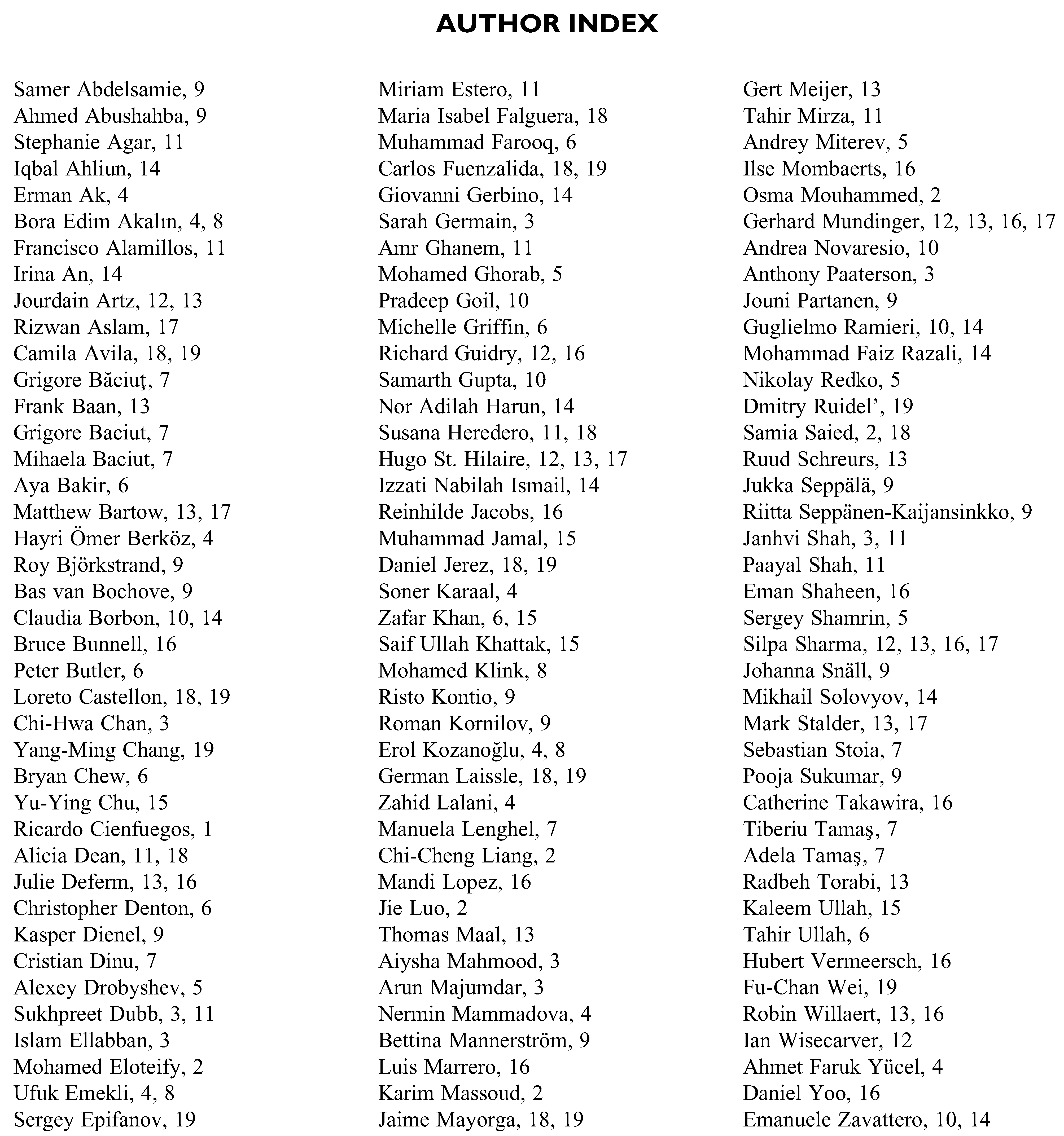
© 2020 by the author. The Author(s) 2020.