Abstract
Facial cleft is a rare and challenging craniofacial malformation. Treatment of rare facial cleft is complex, and the evaluation of its long-term results is challenging because of the low incidence. In this article, we would like to present middle-term follow-up of 6 patients with facial cleft Tessier number 4, number 5, and number 7 who were treated in our center during charity surgical mission. We will discuss surgical option, difficulties, and complication that may arise in this surgery.
Introduction
Facial cleft is a rare congenital anomaly with incidence between 1.43 and 4.85 per 100,000 live birth.[1,2,3] Treatment of rare facial cleft is complex, and the evaluation of its long-term results is challenging because of the low incidence. In comparison to cleft lip and palate abnormalities, the operation technique for the repair facial cleft is currently not well established because high variants and low incidence may occur in facial cleft cases.
Tessier number 4 and 5 facial clefts are a rare, complex, and challenging craniofacial malformation. The treatment requires interdisciplinary cooperation to reach better outcome. Among the oblique facial clefts, Tessier number 5 cleft is extremely rare, representing 0.25% of all facial clefts.[4] The cleft begins medial to the upper lip commissure and extends across the cheek as a groove that ends at the junction of the middle and lateral thirds of the lower eyelid. The inferior eyelid has a coloboma in the middle third and the orbital floor is cleft, with shortening of the distance between the oral commissure and the lower eyelid. Also found an alveolar cleft in the premolar region that extends across the maxilla, lateral to the orbital nerve, up to the infraorbital rim and orbital floor.
Tessier number 4 facial cleft starts distally from canine teeth, it extends across the cheek, passing medially to the infraorbital foramen up to the orbital floor.[1] Tessier number 5 facial cleft starts medial to the oral commissure, extending to the cheek and ends at the junction of the middle and lateral thirds of the lower eyelid. The difference between Tessier number 4 and 5 is that the infraorbital nerve is generally located medial to the skeletal defect.
Tessier number 7 facial cleft also called transverse facial cleft. Tessier number 7 is the most lateral craniofacial cleft.[5,6,7] Prevalence of the abnormality is 1 in 80,000 live births. The anomaly occurs as isolated anomaly or may also features another syndrome such as hemifacial microsomia. The anomaly occurs generally unilateral, though bilateral anomaly cases are reported.

Figure 1.
Patient with Tessier number 5 facial cleft.

Figure 2.
Facial appearance 5 years after operation.
Case 1
A 10-month-old Caucasian baby girl with body weight 9.5 kg presented to the Department of Oral and Maxillofacial Surgery at our hospital with bilateral almost symmetrical Tessier number 5 facial cleft. The cleft begins 2.5 cm medial to the oral commissure giving macrostomia appearance; it runs across the cheek and ends at lateral lower eyelid. The inferior lower eyelid has a coloboma. Palate was intact and alveolar cleft was absent. No other abnormalities were found.
Under general anesthesia, multiple Z-plasty was done bilaterally. A repair of macrostomia were also done bilaterally. The muscle was approximated and sutured. The skin was closed without any tension. The 5-year follow-up reveals good healing with minimum contracture. Lips movement is good without limitation, the chewing movement is also good.
Case 2
A 4-year-old Caucasian boy with body weight 18 kg presented to our Department of Oral and Maxillofacial Surgery with asymmetrical Tessier number 4 facial cleft bilateral, cleft on hard and soft palate. Severe hypernasality is noted on the patient speech because of cleft palate. Alveolar bone was intact. The patient is ectrodactyly on the left hand and anophthalmia on the left eye.
Modified Kawamoto technique was used to treat this case. A paranasal pedicle flap with medial canthus pedicle was used to reconstruct the lower eyelid. Wide dissection of the soft tissue bilaterally was performed including bilateral sulcus incision and mobilization. Multiple small Z-plasty was performed to avoid linear closure of the soft tissue. Cleft lip was closed using central prolabium mucosa and lateral lip element. Surgical approximation of the muscularis orbicularis oris was done in the typical manner as the cleft lip surgery. Monofilament 6.0 resorbable suture was used to close the skin. Cleft palate was closed using modified push back technique with radical muscle dissection and approximation 1 year after initial surgery.
The 4-year follow-up shows acceptable scar. Patient is still assigned to continue speech therapy and under monitoring from our speech language pathologist.
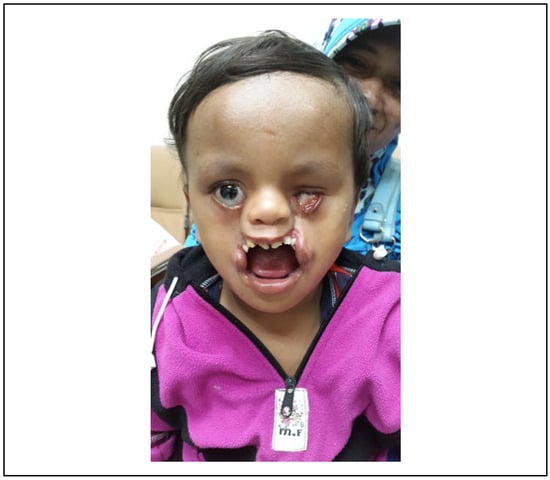
Figure 3.
Patient with Tessier number 4 facial cleft.
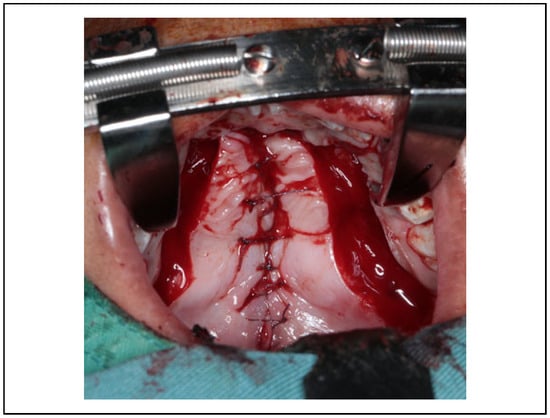
Figure 4.
Palatoplasty was done 1 year after initial operation.

Figure 5.
Patient with Tessier no.4 Facial cleft, 5 years after operation.
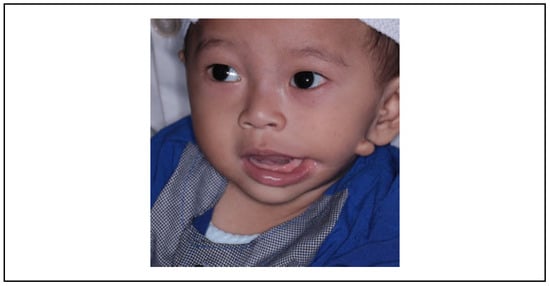
Figure 6.
One-year-old patient with Tessier number 7 facial cleft. Frontal view before operation.

Figure 7.
Four years postoperative.
Case 3
Four patients were presented to our Department with Tessier number 7 cleft.
First patient was 1-year-old boy presented with typical Tessier number 7 cleft on the left side. Second patient was 3-month-old baby presented with Tessier number 7 cleft on the right side. Third patient was 25-year old female, weight 45 kg with Tessier number 7 cleft on the left side. Maxillary hypoplasia with severe crowding was observed. The patient oral hygiene is considered bad with periodontitis at the upper and lower jaw. The patient experienced mastication difficulty and severe aesthetic disorder. Fourth patient was 1-year-old boy with unilateral Tessier number 7 cleft on the left side.
The operation of all these patients was performed with Z-plasty and mucocutaneous-based inferior flap. The postoperative control of 4-year period has shown scar in good range, open–closed mouth function and mastication is noted in good range of movement.
Discussion
We present a rare case of Tessier facial cleft number 4, 5, and 7 with middle-term follow-up. An estimated incidence of rare facial cleft is 1.43 to 4.85 per 100,000 live birth.[1,8] In our country, there is no specific incidence data of facial cleft. A cleft number 3 is the most common, while cleft number 4 and 5 are the least common. Tessier number 5 facial cleft is an extremely rare facial cleft representing 0.25% of all facial cleft.[2,4]
“Medial oro-ocular” cleft, Morian 2 cleft or known as Tessier number 4 can present ranging from unilateral notch to bilateral large tissue defect with bone fissure. It begins with cleft lip, lateral to the Cupid’s bow, skirting the nose and pass through cheek and lateral to the lacrimal duct.[1,2] The skeletal defect begins between the lateral incisor and canine teeth, continues superiorly, passing medially to the infraorbital foramen, up to the orbital floor. Patient may present with microphthalmos, and the eye globe is prone to injury (exposure keratopathy) due to eyelid deficiency. The surgical restoration aims to restore the oro-ocular distance and close hard and soft-tissue palate. More than that, there are some principles that have to be kept in mind, the initial priority is to protect the corneas, the soft tissue component may be treated in the first months of life to restore a relatively normal appearance; each component (lip, nasal, alveolar, ocular, and orbital deformities) should be evaluated and treated; as many of these patients do not have normal facial growth potential, so it is unnecessary to wait for full facial development before starting the surgical repair.[1,6]
Surgical treatment to repair Tessier number 4 included Tessier’s technique and some modification proposed by Kawamoto, Van der Meulen, Resnick, and Esser. Tessier technique uses upper eyelid flap to reconstruct lower eyelid and Z-plasty to repair midface defect, while Kawamoto technique uses vertical paranasal flap to reconstruct lower eyelid.[1,2,6]
Tessier number 5 is extremely uncommon, account for only 0.25% among all facial clefts [2,4]. The cleft begins in the lip just medial to the oral commissure, extending superiorly across the cheek. Skeletal involvement includes the alveolus where the cleft extends behind the canine into the premolar region. The cleft stops in the lateral portion of the orbital floor. Like Tessier number 4, Tessier number 5 is frequently associated with microphthalmia. The objective of the surgical treatment for Tessier number 5 is to close both the eyelid and the labiomaxillary cleft, elevate the lateral canthus, and reconstruct the orbital floor, the malar bone, and the body of the maxilla with bone grafting.
Treatment of patient with facial cleft is very individualized, challenging and based on the surgeon’s experience and judgment. The treatment objective of these cases are to protect cornea, restore soft tissue defect, correct macrostomia, restore bone defect, treat other abnormalities if found, and to observe facial and jaw development. The early concern is to protect the eye from the damage as the consequences of corneal exposure. Soft tissue defect can be reconstructed in most of the cases with local flap, ideally using tissues with similar texture and color. Multiple Z-plasty on the soft tissue can provide better scar than a straight linear scar. Reconstruction of the lower eyelid can be achieved using local flap. Tessier technique using upper eyelid flap can be used to reconstruct lower eyelid. However, the scar resulted from this technique did not respect the natural folds and anatomical unit of the face. Kawamoto procedure is an alternative technique by using vertical nasal flap with superior basis and linear scar in the paranasal area. Linear scar could also be achieved using Tessier technique if the incision was made more medially than in its original design.1 The advantage using Tessier technique is that it can expose the area where the transnasal canthopexy needs to be done. To define medial canthus position in unilateral case, we could use contralateral side as reference, and in bilateral case, the external canthus can be served as a reference point. In the cases we presented, we use Kawamoto procedure to reconstruct lower eyelid bilaterally. Furthermore, regarding the lip defect, we use mucosa from central prolabium and mucosa from lateral lip element to close the lip defect. Bone graft can be done at the later stage of age on secondary operation to close the bony defect. We prefer to avoid doing bone grafting before 5 years old to reduce risk of bone exposure and bone loss. Iliac crest graft is the gold standard material for this procedure. As an alternative, rib graft can be used.
Transverse facial cleft or macrostomia is also called Tessier number 7 cleft with incidence 1 in 80,000 birth.[5,7] Transverse facial cleft has a variable severity from the minor form until the severe form which show complete transverse cleft that extends from the oral cavity to the external auditory meatus or rarely to the temporal fossa. The objectives in repairing transverse facial cleft are symmetrical oral opening, natural appearing commissure, functional orbicularis oris muscle, minimal external scaring, and avoidance of lateral commissure migration.[5,7] In the past, simple linear closure was used. This technique tends to cause contracture of the commissure and cause lateral commissure migration. The repaired commissure tends to drop downwards after surgical correction. The most important step in repair transverse facial cleft is to reconstruct the orbicularis oris muscle. For more extensive transverse facial cleft, some author also recommends to reconstruct the buccinators muscle to avoid a depression on the cheek. In this case, we use Z-plasty technique with mucocutaneous flap based inferiorly to repair transverse facial cleft. The technique can prevent contracture and provide acceptable external scarring. Early closure is preferable to establish oral continence, support better feeding, and improve speech.
Conclusions
Through this report, we present facial cleft cases with middle-term follow-up that we found during charity mission in our center. We explained our techniques in detail. Until now there is no one technique is better than others for a facial cleft case, and it is because of the low incidence of this cases.
Generally, soft tissue reconstruction in facial cleft case can be done with a local flap and multiple Z-plasty to avoid contracture from the scar. Early management has its advantages of getting better aesthetics, support feeding, and better speech outcome.
Facial cleft cases like in this report can be managed well as our surgical charity operation.
Authors’ Note
All surgeries in this publication were supported by Smile Train and Siloam Hospital Lippo Village, Tangerang-Indonesia.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Alons, N.; da Silva Freitas, R.; e Cruz, G.A.; Goldenber, D.; Tolazzi, A.R. Tessier no. 4 facial cleft: Evolution of surgical treatment in a large series of patients. J Plast Reconstr Surg. 2008, 122, 1505–1513. [Google Scholar] [CrossRef] [PubMed]
- Bohra, T.; Ladani, P. Bilateral Tessier number 4 and 5 facial cleft: Case report & review of literature. Acad J Ped Neonatol. 2018, 6, 1–3. [Google Scholar]
- Fijalkowska, M.; Antoszewski, B. Rare facial clefts. Polski Przegląd Chirurgiczny. 2015, 87, 389–394. [Google Scholar] [CrossRef] [PubMed]
- da Silva Freitas, R.; Alonso, N.; Shin, J.H.; Busato, L.; Tolazzi, A.; Cruz, G.A. The Tessier number 5 facial cleft: Surgical strategies and outcomes in six patients. Cleft Palate Craniofac J. 2009, 46, 179–186. [Google Scholar] [PubMed]
- Rogers, G.F.; Muliken, J.B. Repair of transverse facial cleft in hemifacial microsomia: Long-term anthropometric evaluation of commissural symmetry. J Plast Reconstr Surg. 2007, 120, 728–737. [Google Scholar] [CrossRef] [PubMed]
- Sieg, P.; Hakim, S.G.; Jacobsen, H.G.; Saka, B.; Hermes, D. Rare facial clefts: Treatment during charity missions in developing countries. J Plast Reconstr Surg. 2004, 114, 640–647. [Google Scholar]
- Aketa, J.; Nodai, T.; Kuga, Y.; Yamada, N.; Hirakawa, M. A method for repair of transverse facial clefts. J Cleft Palate. 1980, 7, 245–248. [Google Scholar]
- Afifi, A.M.; Djohan, R.; Sweeney, W.; et al. Long term follow up of Tessier no. 5 facial cleft. J Craniomaxillofac Trauma Reconstr. 2011, 4, 35–42. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2020 by the author. The Author(s) 2020.