Introduction
Orbital blowout fractures (OBFs) are common in facial trauma. Many require surgical management to prevent long-term complications, such as globe displacement and motility restriction. The incidence of hospital admissions for OBF management is on the rise.[
1,
2] This can be attributed largely to a corresponding increase in motor vehicle accidents (including all-terrain vehicle and car accidents), falls, and assaults (including intimate partner violence and armed forces combat).[
3,
4,
5,
6] The need for acute surgical intervention is associated with prolonged hospital stays, higher health-care costs, and hospital-associated patient risks, such as radiation exposure and infection.[
1] As a result, there is an increasing need to optimize OBF management. While a significant amount of research focuses on preoperative selection of surgical candidates and surgical technique in OBF repair, there is limited commentary on approaches to optimizing postoperative care.
Routine computed tomography (CT) imaging following isolated OBF repair is used by various surgical subspecialties that manage OBF at our institution to evaluate for immediate postoperative complications, namely retrobulbar hemorrhage or implant malposition. Roth et al, in their 2010 evaluation of orbital trauma management, noted that, due to concern postoperatively for inadequate positioning of reconstruction materials, many orbital surgeons perform routine postoperative CT scans.[
7] They found, however, that as surgical experience increases, the frequecny of routine postoperative scanning decreases. Kontio and Lindqvist, in their 2009 evaluation of orbital fracture management, recommended postoperative CT evaluation in all cases of surgical repair.[
8] There are limited studies to date that evaluate the utility of postoperative imaging specifically in the surgical management of OBF. We hypothesize that the use of a routine CT scan following isolated OBF repair does not impact decisions regarding postoperative management in the vast majority of cases. If our hypothesis holds true, then the use of a postoperative CT scan after OBF repair may be eliminated in favor of targeted diagnostic imaging in the setting of a concerning postoperative clinical examination. Such a change would reduce health-care costs as well as patient radiation exposure without sacrificing the quality of patient care. The purpose of this study is to evaluate the clinical utility of the postoperative CT scan in isolated OBF repair as a possible area for improvement in OBF postoperative management as well as reduction in associated health-care expenditure.
Methods
Study Design and Patient Characteristics
A single-center, institutional review board–approved retrospective review of patients who underwent surgical OBF repair at the University of Maryland Medical Center, Baltimore, Maryland, USA between November 2008 and August 2016 was performed. Cases of surgical OBF repair were identified using Current Procedural Terminology codes 21385-7, 21390, 21401, and 21406-8 in accordance with the Health Insurance Portability and Accountability Act and the tenets of the Declaration of Helsinki. From these cases, adult patients with isolated OBF were identified. Patients who were under 18 years of age, who had suffered additional facial fractures requiring surgical intervention, or who had incurred associated intraocular trauma (eg, retinal detachment, globe rupture, hyphema) were excluded from the study. In addition, cases without a documented preoperative clinical examination, operative note, postoperative CT scan, and at least one documented follow-up appointment including an eye examination were also excluded.
Procedure
From the cases that met inclusion criteria, demographics (age at presentation, gender, mechanism of injury, eye involved), preoperative and postoperative clinical data (visual acuity, motility, globe displacement, subjective diplopia), and results of postoperative CT imaging were recorded. The postoperative examination data were collected from the final follow-up examination prior to a return to the operating room (OR) or completion of postoperative follow-up care. Postoperative CT data were collected from final reads by licensed radiologists. To confirm the scans were routine, the indication listed on the imaging order and preimaging clinical documentation was evaluated to ensure that it did not include a concerning clinical finding. The majority of CT indications were listed as “postoperative scan.” Any postoperative CT finding that was not described as within normal limits was collected and classified as major, indeterminate, or minor based on severity and predicted impact on clinical outcome. Major findings were defined as unequivocally necessitating a return to the OR, indeterminate findings as potentially prompting repeat surgical intervention, and minor findings as typical postoperative findings that would not require additional intervention. Each patient’s chart was reviewed for any repeat surgeries, and final radiologist reads of subsequent routine postoperative imaging were recorded from the electronic medical record. These reads were also reviewed for major, indeterminate, or minor findings.
Results
Cases
Eighty-nine cases of OBF treated at our study site during our study period were identified. Of these, 52 patients met the inclusion criteria. Thirty-seven cases were excluded: 33 patients (37.1%) did not undergo a postoperative CT scan, 3 patients were lost to follow-up and did not have documented postoperative clinical examinations, and 1 patient did not complete surgical repair.
Demographics
The 52 patients who met the inclusion criteria had an average age of 42.8 years at the time of operation (±12.8 years). Time from injury to operation averaged 6.2 days (±6.4 days). In the majority of cases, the mechanism of injury was assault (48.1%, n = 25), followed by motor vehicle accidents (28.8%, n = 15), falls (21.2%, n = 11), and sports injuries (1.9%, n = 1). The right eye (61.5%, n = 32) was more commonly affected than the left, and the majority of patients were male (69.2%, n = 36). Demographic characteristics of the study population are summarized in
Table 1.
Preoperative Examination
On preoperative examination, the most prevalent abnormal finding was subjective diplopia (71.2%, n = 37), followed by motility restriction (53.8%, n = 28), globe displacement (23.1%, n = 12), and reduced best-corrected visual acuity (BCVA; 11.5%, n = 6). One patient experienced dizziness, nausea, vomiting, and bradycardia with extraocular movements. All patients had preoperative axial CT scans with coronal and sagittal reformatted images confirming OBF. Each was scheduled for orbital reconstruction by open reduction with reposition of herniated tissue confirmed by visual inspection and internal fixation with titanium mesh implant evaluated by intraoperative forced duction testing and was documented in the medical record with an operative note.
Postoperative Imaging
Review of the postoperative CT interpretations revealed 10 categorical abnormal findings that were noted by the radiologist: mesh malposition, mesh impingement on a rectus muscle, mesh impingement on the optic nerve, rectus muscle herniation, rectus muscle contusion, fat herniation, sinus opacification, soft tissue edema, persistent orbital bony defects, and orbital edema. These findings were classified as major, indeterminate, or minor using the criteria outlined above. Mesh impingement on the optic nerve and mesh impingement on a rectus muscle were classified as major findings; persistent orbital bony defect, rectus muscle herniation, fat herniation, and mesh malposition were classified as indeterminate findings; and rectus muscle contusion, sinus opacification, soft tissue edema, and orbital edema were classified as minor findings.
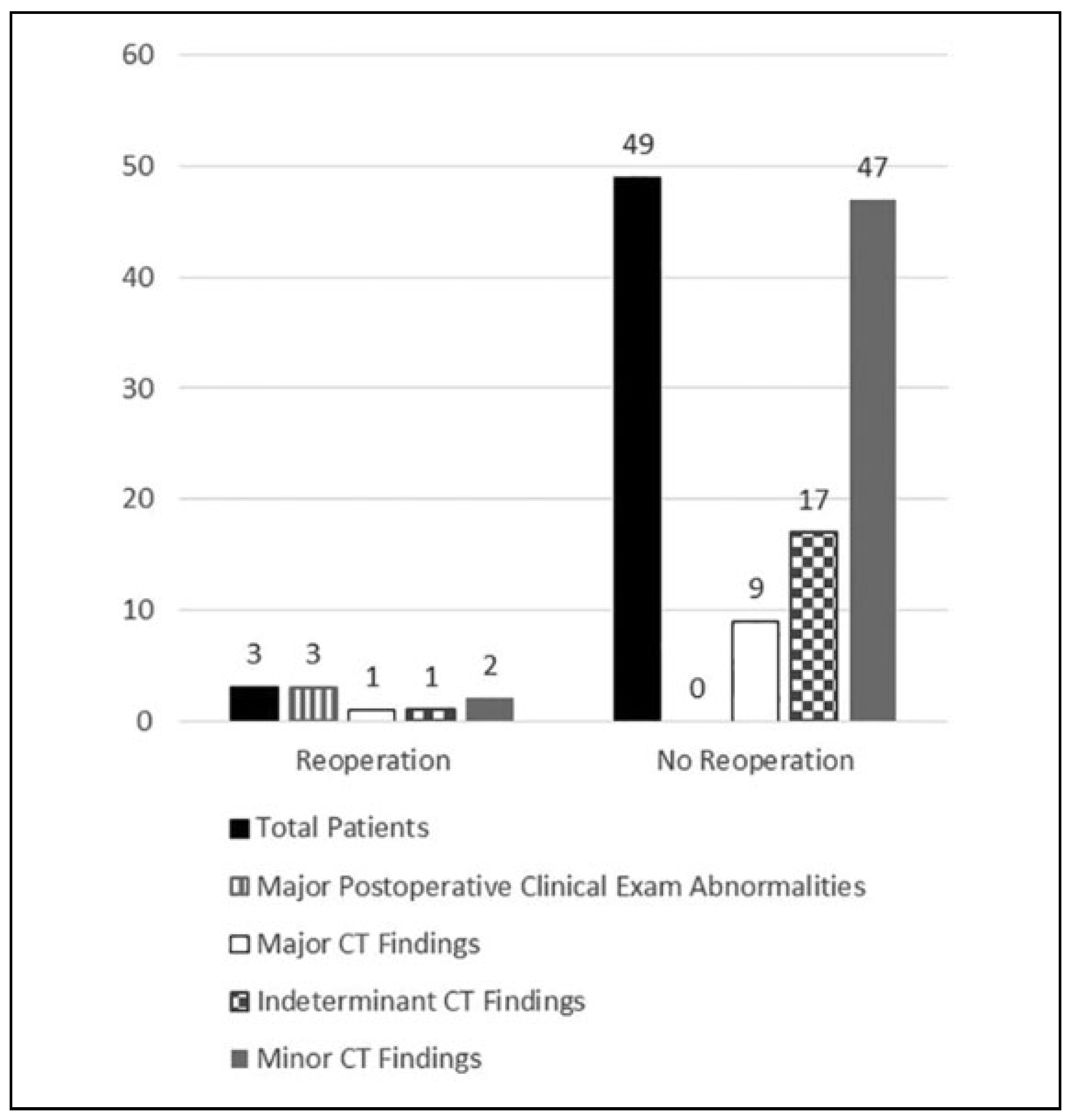
CT interpretations for a large majority of patients (94.2%, n = 49) revealed minor findings; approximately one-third (34.6%, n = 18) included indeterminate findings, and there were only 10 (19.2%) with major findings. Subgroup analysis revealed that the most common minor finding was sinus opacification (90.4%, n = 47), followed by orbital edema (36.5%, n = 19), soft tissue edema (34.6%, n = 18), and rectus muscle contusion (21.2%, n = 11). The most common indeterminate finding was persistent bony defect (19.2%, n = 10), followed by fat herniation (17.3%, n = 9), mesh malposition (11.5%, n = 6), and muscle herniation (9.6%, n = 5). The most common major finding was mesh impingement on a rectus muscle (19.2%, n = 10), followed by mesh impingement on the optic nerve (1.9%, n = 1;
Figure 1).
Postoperative Examination
On final postoperative examination before reintervention or discontinuation of follow-up, the majority of physical examinations were normal. The most common positive findings were motility restriction and diminished BCVA (n = 2, 3.8%). Other positive findings included 1 patient with globe displacement (1.9%). In total, only 3 cases had significant postoperative examination findings prior to a change in management (
Figure 1).
Postoperative Course
In our study population, 3 patients required return to the OR for surgical revision. In case 1, postoperative imaging demonstrated mesh impingement on the inferior rectus muscle and mesh impingement on the optic nerve, both major findings. While reoperation was pursued in the only patient with the CT finding of mesh impingement on the optic nerve, there were 9 other cases with mesh impingement on a rectus muscle in which revision was not performed. On immediate postoperative examination in the post-anesthesia care unit, the patient’s pupillary examination was noted to be normal without an afferent pupillary defect, or mydriasis that would be expected with mesh impingement on the optic nerve. However, the patient experienced severe subjective diplopia and was found to have a supraduction deficit and decreased BCVA to 20/50 (from 20/20 on preoperative examination) in the operative eye. The nonoperative eye demonstrated full extraocular movements and 20/20 vision. The patient returned to the OR for revision, and subsequent postoperative examinations were significant for full resolution of the supraduction deficit and return to baseline 20/20 vision at the 1-week follow-up appointment.
In case 2, postoperative imaging demonstrated rectus muscle herniation, mesh malposition, and fat herniation, all indeterminate findings. There were 4 other cases with CT reads noting rectus muscle herniation, 5 others noting mesh malposition, and 8 others noting fat herniation, none of which underwent reoperation. On postoperative evaluation, the patient was initially asymptomatic with a normal examination. After 6 months, the patient scheduled a follow-up appointment due to subjective diplopia and was found to have a supraduction deficit with obvious enophthalmos and hypoglobus. This development of late enophthalmos and hypoglobus prompted a return to the OR without diagnostic imaging. Late globe malposition was not predicted in this case by the original postoperative scan. In addition, there were 10 cases of postoperative scans identifying persistent bony defects concerning for possible late development of globe malposition; however, such a complication and none required reoperation. The postoperative CT scan following revision revealed the indeterminate findings of rectus muscle and fat herniation, mesh malposition, and persistent orbital bony defect, in addition to the major finding of mesh impingement on a rectus muscle. However, the postoperative clinical examinations were normal without recurrence of diplopia or globe malposition, and no further surgical intervention was pursued.
In case 3, postoperative imaging was read as normal. However, the patient experienced an acute loss of vision to hand motion in the operative eye approximately 18 hours postoperatively prompting immediate return to the OR for removal of the mesh implant and hematoma evacuation. This hematoma was not visible on postoperative CT imaging. The patient had a postoperative CT scan following revision, which revealed only soft tissue edema, a minor finding. On postoperative examinations, the patient’s visual acuity returned to baseline and subjective diplopia resolved. No further clinical management was pursued.
Discussion
During OBF repair, every effort is made to reposit all tissue and confirm appropriate mesh placement using intraoperative visualization and forced duction testing; however, a few patients still require reoperation. Despite the use of postoperative CT imaging in OBF repair to detect mesh implant malposition and retrobulbar hematomas in a way that directs the need for clinical intervention, there is limited literature evaluating its true utility as a standard practice following every OBF case. There is evidence pointing toward a lack of utility in the multiple studies recommending against routine postoperative imaging following traumatic facial fracture repair.[
9,
10,
11,
12,
13,
14,
15]
In a retrospective review of postoperative imaging following maxillofacial trauma repair by Van den Bergh et al, 16 of 579 patients returned to the OR for revision.[
9] Only 1 of the 16 patients returned due to imaging findings alone. The remainder returned due to concerning postoperative clinical findings. The authors concluded that intraoperative analysis and postoperative clinical symptoms are reliable indicators of complication requiring surgical revision and that imaging should be reserved for patients with significant changes on postoperative clinical examination.[
9]
Jain and Alexander similarly evaluated 431 patients with maxillofacial fracture repairs.[
10] Twenty patients from this cohort required further surgical intervention. However, no patient underwent reoperation in the absence of concerning clinical signs and symptoms, regardless of postoperative radiograph findings. The authors found that postoperative examination findings were statistically superior indicators of complication requiring revision compared to postoperative imaging findings and concluded that there was no role for routine postoperative radiographs.[
10]
In a study by Bali and Lopes, of 273 facial fracture repairs, 3 cases returned to the OR for surgical revision due to postoperative examination findings alone.[
11] The authors concluded that postoperative radiographs are overprescribed and that eliminating them would reduce both health-care costs and patient radiation exposure. In several additional retrospective reviews, the decision to return to the OR for revision after facial fracture repair was prompted by clinical examination findings alone. These authors repeatedly conclude that there is a lack of evidence supporting postoperative imaging when clinical examination alone is sufficient.[
12,
13,
14,
15]
There is only one study to date, to our knowledge, evaluating routine postoperative CT scans following isolated OBF repair. Sharma et al, in an evaluation of 58 patients who underwent orbital floor fracture repair with routine postoperative CT imaging, found that postoperative CT findings resulted in a return to the OR in the case of 6 patients, as compared to 28 patients who returned to the OR due to physical examination findings alone.[
16]
In keeping with previously published literature, we question the utility of routine imaging following isolated OBF surgical repair. After evaluating the postoperative CT findings for patients who did and did not undergo reoperation, we conclude that postoperative CT reads are not predictive of need for return to the OR. These findings are in line with the aforementioned studies of traumatic facial fracture repairs and reinforce the conclusions of the sole study regarding OBF repair specifically. Our study adds to the scientific literature by showcasing multiple isolated OBF cases with postoperative CT reads of mesh malposition without clinical findings who did not return to the OR and one case (case 3) of a retrobulbar bleed that resulted in emergent hematoma evacuation despite completely normal CT imaging.
Selective diagnostic imaging prompted by concerning clinical changes following isolated OBF repair is an attractive alternative to routine postoperative imaging. In this study, no patient returned to the OR without concerning clinical findings. This included 10 cases where the CT imaging and clinical examination findings were inconsistent (19.2%), including 9 cases where the postoperative CT scan showed concern for mesh impingement on a rectus muscle, however, extraocular movements on clinical examination did not support this imaging finding (
Figure 2). Alternatively, in case 3, where a CT scan showed completely normal postoperative results, the patient’s BCVA dropped to hand motion due to RBH requiring intervention. The argument can be made that, in cases 1 and 2, postoperative imaging influenced the decision to return to the OR (3.8%). However, changes in the postoperative clinical examination were more directly related to the reason for surgical intervention (100.0%). In case 1, the patient had a marked supraduction deficit correlating with the CT finding of impingement on a rectus muscle; however, mesh impingement on the optic nerve was not fully supported by clinical examination. If a postoperative CT scan had not been obtained, surgical revision would still have been pursued given clinical concern. In case 2, the patient was asymptomatic and did not return to the OR immediately, despite postoperative imaging with multiple indeterminate findings. However, the delayed development of globe displacement (which was not predicted by postoperative imaging) prompted a return to the OR without further imaging. Furthermore, after reoperation in case 2, routine imaging was now concerning for mesh impingement on the inferior rectus muscle (a new major finding), and the patient did not return to the OR in the setting of a benign clinical examination. This disconnect between postoperative imaging findings and clinical management questions the utility of obtaining imaging routinely following isolated OBF repair.
Other commonly cited reasons for the use of postoperative CT scans include medicolegal need and surgeon edification. However, given the significant disconnect between patient examination and CT scan findings, we argue that this practice is not helpful for these reasons either. In our study group, CT images showed concerning findings that were not supported clinically and were not actively managed by the operating physician. As such, the CT scans did not independently dictate the operating surgeon’s decision medicolegally to intervene or not. Furthermore, multiple CT scans showed mesh malposition in patients with excellent clinical results. Surgeon learning from postoperative examinations would be a better indicator than CT scans, as they correlate more directly with patient outcome.
Elimination of the routine postoperative CT scan would reduce patient radiation exposure as well as health-care costs, without sacrificing the quality of patient care. According to the American College of Radiology Blue Ribbon Panel on Radiation Dose in Medicine, prior to an imaging procedure becoming a part of patient care “...there should be general agreement that the benefits exceed the risks and that an attempt has been made to reduce the potential risks as low as practicable.”[
17](p. 273) Based on the results of our study, we did not identify a medical benefit for routine postoperative CT imaging and the necessary information for postoperative decision-making was most commonly obtained by physical examination alone. Furthermore, the cost of a noncontrast CT scan of the orbits with a radiologist read is approximately US
$1700.00. For this study population alone, that would amount to US
$88 400 for routine postoperative imaging, and specifically US
$85 000 worth of imaging resulted in no arguable contribution to patient management.
Limitations to this study include its modest sample size and single-center setting. Another limitation in our study design is its retrospective nature. OBF repairs in this study were performed by multiple surgeons from different subspecialties, thereby introducing variation in surgical technique, preoperative care, and postoperative care. This aspect of our study nevertheless lends itself to increased generalizability as OBF management is often a shared responsibility between different subspecialties (ophthalmology, otolaryngology, and plastic surgery) as is true at our institution. As with any retrospective review, this study risks information bias. We mitigated this risk using single-researcher patient selection for inclusion criteria and CT finding categorization for consistency. We also employed researcher blinding to reoperation outcome during data collection and categorization. Finally, the CT finding categories were organized into major, indeterminate, and minor by a surgeon who performs OBF repairs but who was not involved in the management of some cases included in our analysis.
In this study, we have provided strong evidence that routine postoperative imaging following isolated OBF repair is a superfluous component of OBF management and is a practice that should be discontinued in favor of targeted postoperative imaging guided by clinical examination. Cases that required revision presented with significant clinical signs and symptoms that were noted during the postoperative monitoring period or prompted the patient, who was educated on concerning signs and symptoms, to return for repeat evaluation. It is the authors’ opinion that a postoperative CT scan is not adding to the surgical management of isolated OBFs. In addition, this practice unnecessarily exposes patients to radiation and contributes to rising health-care costs. By prioritizing the postoperative clinical examination, we can further optimize OBF management in terms of what is best for both the health-care system and patient.