Introduction
Orbital floor fractures are common in patients with traumatic craniofacial injuries. Of the four walls of the orbit, the floor is most frequently fractured—particularly medial to the infraorbital canal, where the floor is especially thin.[
1,
2] The frequency of orbital floor fractures is as high as 84% of all orbital fractures.[
3]
A variety of methods have been utilized in reconstruction of the fractured orbital floor, including both biologic and alloplastic implant materials. There appears to be a trend toward greater use of alloplastic implants in treatment of adult patients. Titanium alone, porous polyethylene, and porous polyethylene/titanium composites are among the more commonly used materials in North America. This may be attributed to ease of use, safety, and efficacy of these types of implants.[
4] Additionally, there is the benefit of saving operating room time by using alloplastic material off-the-shelf. Being radiopaque, the titanium or the porous polyethylene/titanium composite implants can be visualized on computed tomography (CT) scans and on plain radiographs, providing the surgeon with information about accurate placement of these implants intraoperatively.
Intraoperative imaging has long been used in neurosurgery and orthopedic surgery, and is becoming more and more prevalent in the surgical management of facial fractures. Various forms of CT 3D imaging are cited as important intraoperatively tools for repair of facial fractures.[
5,
6,
7,
8,
9] Others have reported the utility of intraoperative navigation systems in management of such fractures, especially in more challenging cases.[
10,
11,
12] Repair using navigation systems is guided by mirroring the contours and dimensions of the unaffected side onto the fractured side. Our group previously reported that intraoperative 3D imaging (O-arm imaging system [Medtronic, Inc., Minneapolis, Minnesota]) resulted in real-time refinement of surgical management in 44% of patients with orbital fractures.[
13]
Multiple groups have outlined the benefits of intraoperative C-arm radiography in reduction of zygomatic fractures, touting the low radiation exposure, ease of use, efficiency, lower costs, and control of fracture reduction.[
14,
15,
16,
17] The use of plain radiographs in management of isolated orbital fractures has been limited or unreported mainly due to poor visualization of details of the orbit on plain radiographs.
The main purpose of this study is to establish a known parameter that would provide the surgeon with some valuable insights regarding placement of radiopaque orbital floor implants intraoperatively using plain radiography. This can be applicable to surgeons both at institutions where advanced 3D intraoperative imaging is available and at institutions where this technology is unavailable. We measured the anteroposterior (AP) angle of inclination of the orbital implant on lateral radiographs. More specifically, this is the angle that the trough of the implant makes with the craniometric Frankfort horizontal plane, as defined by the plane that connects the superior aspect of the external acoustic meatus (porion) with the most caudal point of the inferior orbital rim (orbitale).[
18,
19]
Methods
We obtained 14 well-preserved dry adult human skull specimens without any major craniofacial fractures from the collection of the Anatomy Bequest Program at the University of Minnesota. The specimens were chosen at random from a large collection of skulls. This study was exempt from Institutional Review Board (IRB) requirements due to involvement of deceased subjects only. The principles of medical ethics outlined in the Declaration of Helsinki were followed. The skull specimens had already undergone assessment by an independent biologic anthropologist; each deceased donor’s sex, age, and other craniometric features had been collected in a database. According to the database, 7 specimens were from male donors, and 7 from female donors. All donors had been at least 25 years old at the time of their death. The groups of skull specimens were ethnically diverse based on the independently analyzed craniometric features.
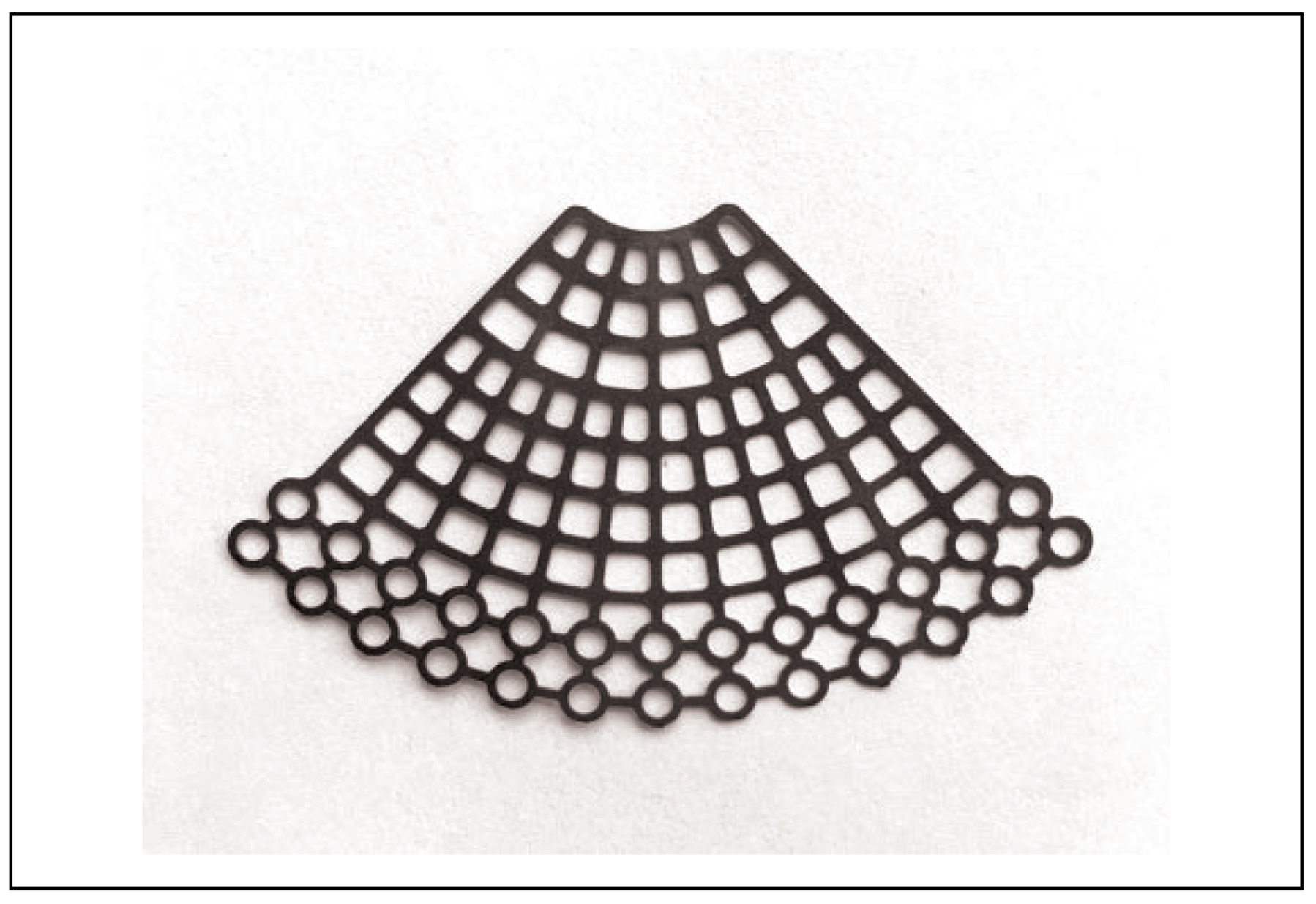
Titanium fan plate implants (
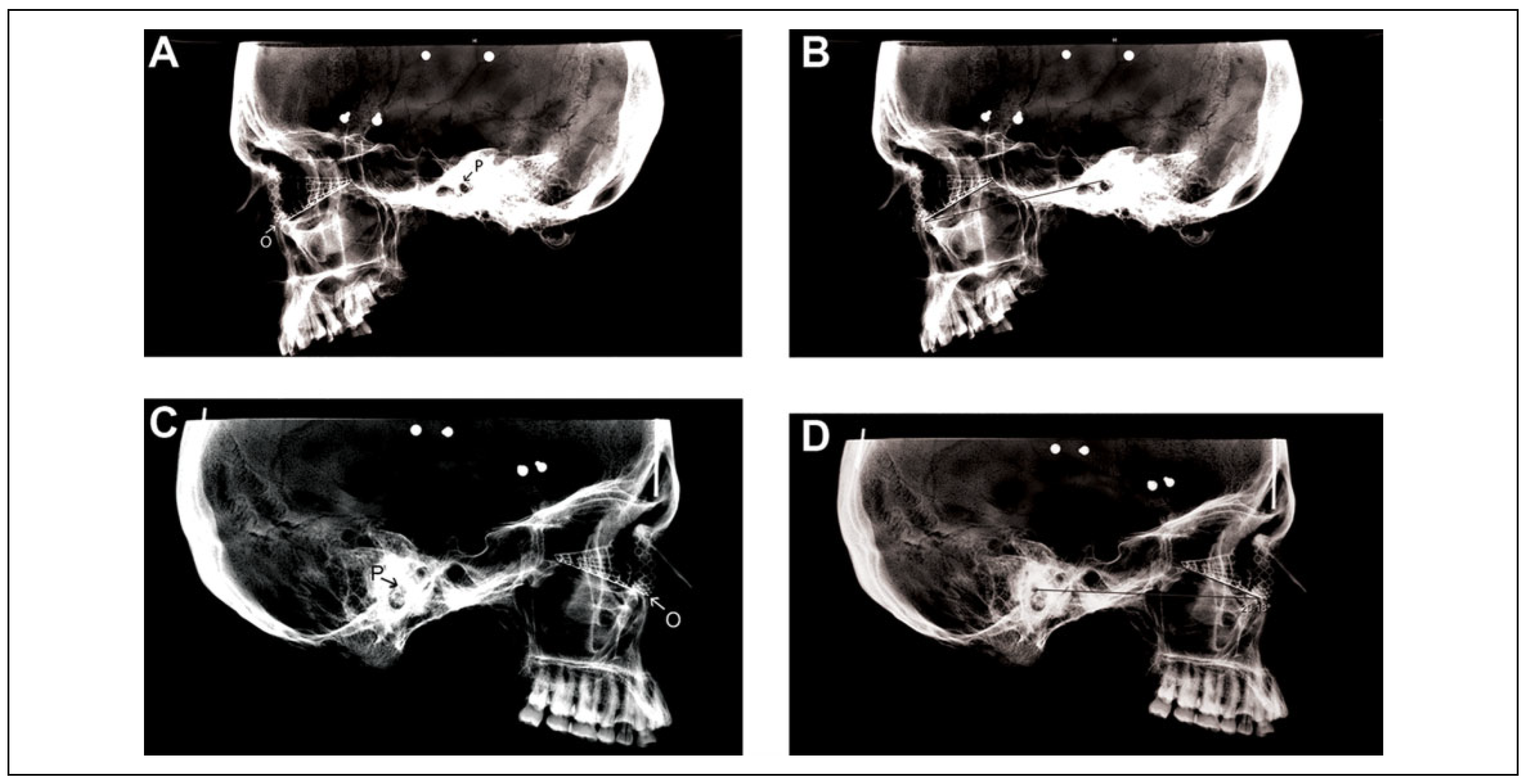
Figure 1) by DePuy Synthes Companies (West Chester, Pennsylvania) were molded and affixed with masking tape to individual orbits on each side separately. Next, flat plate lateral radiographs were obtained for each orbit containing an implant (
Figure 2). The radiography flat plate was placed on the side where the implant was placed in order to minimize the beam magnification effect. We were careful to obtain as true a lateral image as possible. The implants, though not trimmed, were seated well into each orbit, from the inferior orbital rim to the site where a posterior ledge would be encountered in a true fracture. None of these skulls had orbital floor fractures. Therefore, no distortion was expected in the way the implant was placed in each orbit. In order to make the specimens easier to handle during imaging, we had removed the mandibles.
All radiographs were uploaded on the Merge picture archiving and communication system platform (Watson Health Imaging, Chicago, Illinois), and this software was used to obtain the angle that the trough of the implant, on lateral view, made with the Frankfort horizontal plane (
Figure 2).
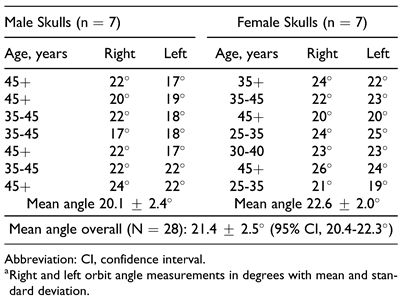
Measuring both the left and the right orbits on 14 skulls, we assessed a total of 28 angles. To analyze our data and determine statistical significance, we used Microsoft Excel software (Microsoft, Redmond, Washington).
Discussion
Measurement of the AP angle of inclination that a well-placed orbital implant makes relative to the Frankfort horizontal plane can be used to provide useful clinical information. Technically, this angle can be measured between the line that the trough of the implant makes with the Frankfort horizontal plane on a lateral plain radiograph. This study aims to define an average value for this angle of inclination that would be instrumental for the surgeon intraoperatively in gaining a better understanding of the position of the orbital implant. In our study of 14 skull specimens, we demonstrate this angle to be 21.4 ± 2.5°. Information regarding the AP inclination angles of the orbital floor has not been widely presented in the anatomic, surgical, or radiologic literature to date, which makes this study unique in presenting a clinically relevant value for this angle—a value based on how the implant sits in the orbit.
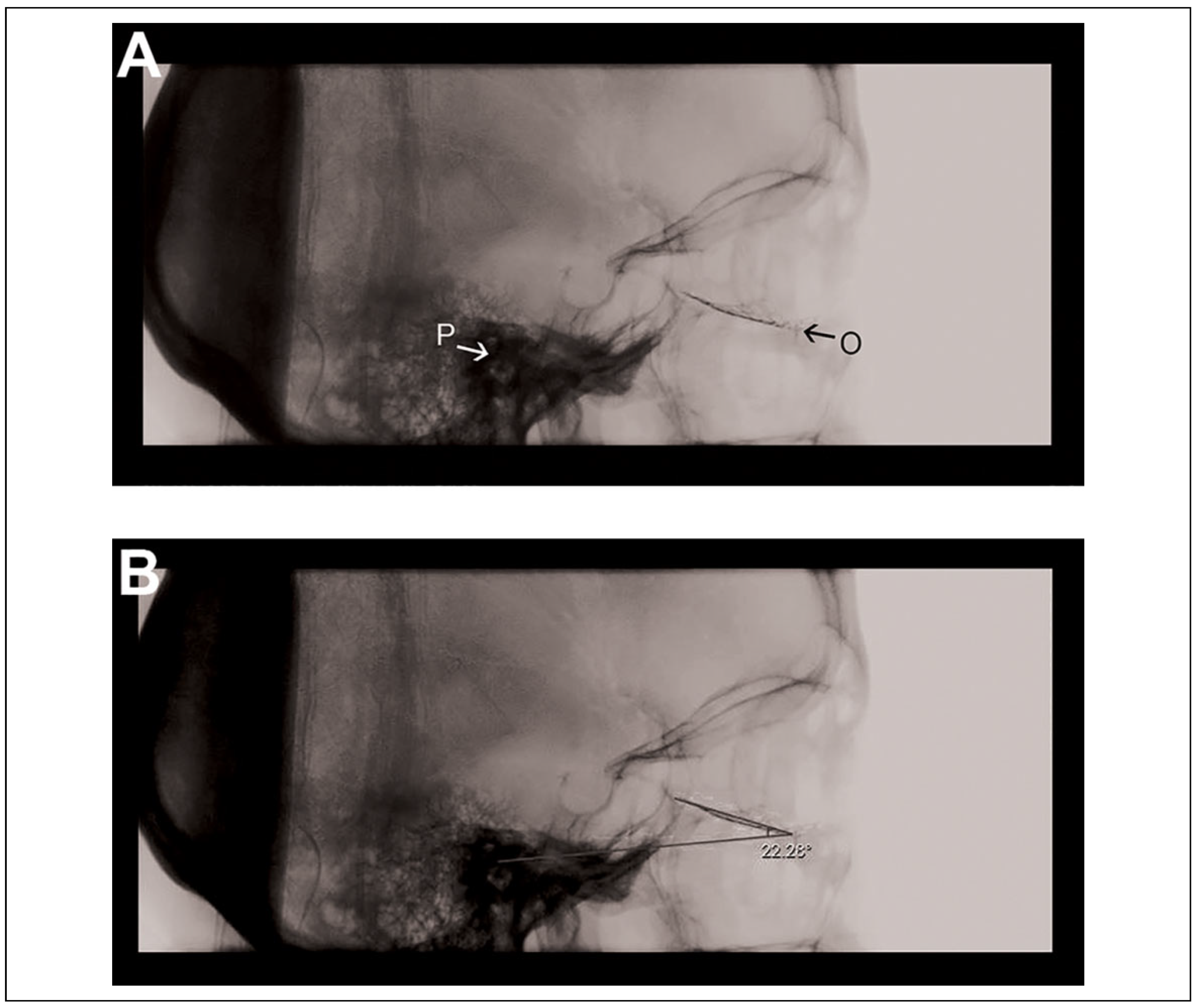
Based on clinical experience, most misplaced implants go through the fractured floor into the maxillary sinus. In that scenario, the angle (between the trough of the implant and the Frankfort horizontal plane) is decreased—and thus, if carefully assessed, would raise suspicions of inaccurate positioning of the implant. Based on our findings, this angle was fairly consistent among 14 different skull specimens, with a relatively tight standard deviation. It must be noted, however, that accurate measurement of this angle would require obtaining a true lateral radiograph, and adjusting the exposure to better differentiate the external acoustic meatus from the surrounding radio-dense petrous portion of the temporal bone. These tasks are not difficult to achieve as demonstrated on a sample intraoperative lateral radiograph of an actual patient in
Figure 3. In our practice, we try to overcome the challenge of obtaining as true a lateral image as possible by making sure that landmarks such as the mastoid processes and orbits align. The external acoustic meatus can be identified on an intraoperative lateral radiograph as a distinct circular structure located anterior and cephalad to the mastoid air cells. Porion is the point at the superior most aspect of the meatus. Most imaging devices are equipped with software that allows for measurement of angles on the screen intraoperatively.
In our 7 male and 7 female skull specimens, we found no statistically significant differences between the male and female angles. Even though some variations in the shape of the orbits between sexes have been reported in the literature,[
1] no specific measurement of the AP inclination angle of the orbital floor has been described. Singh et al report male orbits to be larger than female orbits in most linear measurement parameters, including depth, but orbital floor inclination angles are not measured.[
20] Fitzhugh et al also reported larger dimensions in the male orbital apertures,[
21] but again, the floor inclination angles were not measured.
Although the ex vivo conditions of this study limit extrapolation of these measurements to actual clinical circumstances, this study provides a groundwork for evaluation of the implant angle and how it relates to its appropriate placement. Presence of soft tissues and periorbita may render the in vivo angle slightly different from what is measured in this study on dry skulls; however, this may be a negligible difference. Additionally, measurement of the angle by this method applies to situations where radiopaque implants are used, not in cases where porous polyethylene or other radiolucent implants are placed. Moreover, we did not use any contoured implants in this study. Although the measured angle range in this study may possibly be extrapolated to the angle of the floor portion of a contoured implant, that is outside of the scope of this current study. In cases where there is an impure orbital floor fracture (ie, the inferior orbital rim is involved), this measured angle may not be accurate. Future studies will focus on reproducing these findings on radiographs of actual patients who have undergone repair with radiopaque implants. In addition, a larger sample size might elucidate any angle differences between sexes that may be clinically relevant.
At institutions where traditional 3D intraoperative imaging is utilized for repair of orbital floor fractures, lateral and AP scout radiographs are often obtained first in order to ensure proper positioning of the patient’s head within the device. At our institution, if we see the implant is making too acute an angle on the lateral scout radiograph, we readjust the position of the implant before the final 3D scan is performed. Therefore, these findings can be instrumental for surgeons at institutions where intraoperative CT imaging is routinely performed as well as at institutions where advanced 3D intraoperative imaging is not available. At operating rooms where advanced 3D imaging is not available, lateral plain radiographs can be performed to assess the angle of the implant relative to the Frankfort horizontal plane in order to give the surgeon a yardstick for evaluating appropriate placement of the implant. Although this may not be adequate to fully confirm appropriate placement of the implant as much as advanced 3D imaging is capable of doing, it is a tool that provides some guidance to the surgeon.
As an example from our institution,
Figure 3 demonstrates a lateral scout taken before the final scan on the O-arm. This is a 53-year-old female with an orbital floor fracture who underwent repair with a titanium fan implant. The measured angle happens to be 22.3°, which is within 1 standard deviation from the measured mean on the dry skull specimens in this study.
In conclusion, plain radiographs can play an important role in providing information about the placement of the orbital floor implant both at institutions where advanced 3D imaging modalities are not readily available and at institutions where 3D intraoperative imaging is routinely performed after obtaining scout radiographs. This may lead to improved patient outcomes in decreasing the need for revision procedures, decreasing operating room and anesthesia time, as well as eliminating exposure to radiation from repeat runs of intraoperative CT imaging.