Frontal sinus fractures account for only 5 to 15% of all facial fractures in adult craniomaxillofacial trauma due to the increased thickness of the frontal bone.[
1] The frontal bone can withstand 800 to 1,600 pounds of force,[
2] thus confers resistance against most forms of traumatic injury. Motor vehicle accidents are the most common cause, followed by assaults and sports-related injuries. The appropriate man- agement of frontal sinus fractures is a controversial and highly debated topic in craniomaxillofacial trauma and a lack of consensus exists in the current literature regarding the preferred treatment of frontal sinus fractures secondary to the fact that most clinical recommendations are derived from single-center retrospective case series with relatively small numbers of patients. Controversies exist in regards to the roles of frontal sinus obliteration, cranialization, and nasofrontal duct stenting in the acute trauma setting.
Anatomy and Physiology
The frontal sinuses are derived from the frontal recess portion of the middle meatus, the eventual location of the ostium of the nasofrontal duct or on occasion from air cells of the ethmoid infundibulum. They are absent at birth, development begins at age 2, becomes radiologically evident by age 8, and reach adult size at around age 12 years. About 4% of the population does not have a frontal sinus, and 10% with only a unilateral frontal sinus. An additional 4 to 5% have only rudimentary supraorbital air cells.[
3] The sinuses are not simple chambers, but rather are often subdivided into subcompart- ments or recesses by incomplete bony partitions. The average height of the frontal sinus is 24 mm (range: 5–66 mm), and length is 29 mm (range: 17–49 mm). The boundaries of the sinus floor include the orbital roof inferiorlyand the cribriform plate medially. The intersinus septum, an extension of the crista galli, separates the two sides of the frontal sinus.[
4] The anterior wall is much thicker than the posterior wall, espe- cially along the supraorbital buttress. The posterior wall is thinner (0.1–4 mm) and is not part of the transverse buttress system. The posterior wall is of mesodermal origin and due to the similar embryologic origin it is intimately adhered to the dural lining of the anterior cranial fossa. The dura becomes thinner and more adherent along the inferior edge and over the roof of the ethmoid air cells (fovea ethmoidalis). Significant fractures of the frontal bone can propagate easily and exten- sively along the orbital and nasoethmoid complex areas of lower tolerances to impact force.
The frontonasal ducts provide the drainage into the nasal cavity via the middle meatus. The hourglass-shaped fronto- nasal duct has an average diameter of 3 to 4 mm and consists of three parts: (1) a wide frontal infundibulum that drains into (2) a short, narrow ostium before expansion into (3) the ethmoid infundibulum. Located in the posteromedial seg- ment of the sinus floor, the course is highly variable in length from a few millimeters up to 2 cm.
The mucosa of the frontal sinus consists of a pseudostra- tified ciliated columnar epithelium interspersed with goblet cells. Mucus is produced by these goblet cells which are primarily located within the caudal portion of each sinus cavity. A clinically significant anatomical structure of the mucosa of the frontal sinus is the foramina of Breschet. These foramina are sites of venous drainage of the mucosa and can serve as the route of spread of infection intracranially. Since the mucosa deeply invaginates, if not completely cleared from the foramina in sinus obliteration or cranialization, a potential risk of mucocele formation is created.[
5]
Diagnosis
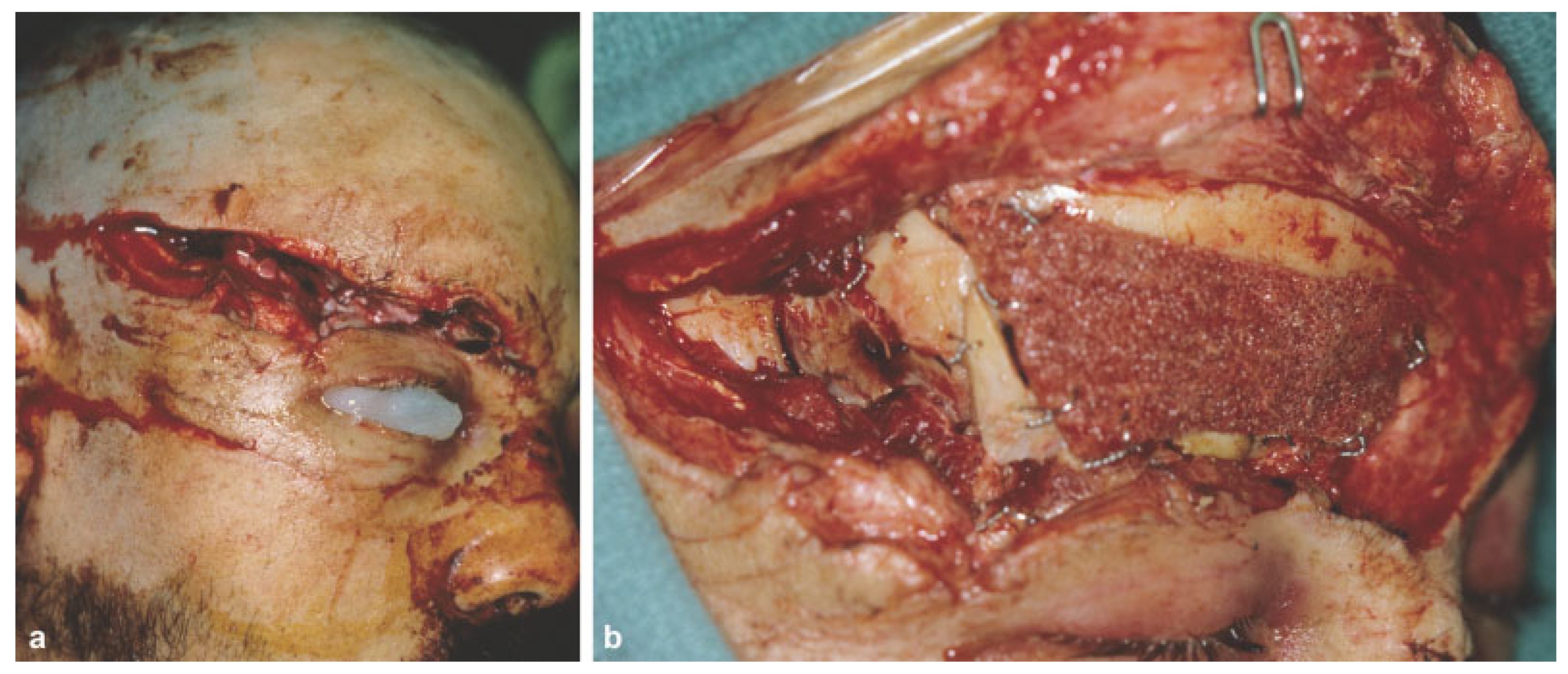
The presence of a supraorbital ridge, glabella, or forehead laceration should raise suspicion for the presence of a frontal sinus fracture (
Figure 1). Patients with frontal sinus fractures will often have visible depression in the supraorbital region that accompanies the soft-tissue compromise. Palpation over the suspected injury area may reveal crepitus, instability, and step-off. In patients with significant swelling, however, these physical findings are often masked. Sensory deficits are also common secondary to injury of the supratrochlear and or supraorbital nerves.
Forces capable of disrupting the anterior table will fre- quently injure the posterior table and other elements of the craniofacial skeleton. A complete examination of the entire craniofacial skeleton is warranted. Because of the proximity of the globe, an ocular exam including evaluation of globe integrity, extraocular movements, visual fields, visual acuity, and pupillary response should be done. Fractures of the orbital roof that propagate to the orbital apex can cause superior orbital fissure and orbital apex syndromes. Occasionally, frac- tures of the frontal sinus will extend to the skull base beyond the anterior cranial into the middle cranial fossa.[
6]
Persistent clear nasal drainage should raise the suspicion of cerebrospinal fluid (CSF) rhinorrhea. This finding indicates a violation of the posterior table and dura tear that permits direct communication between brain and upper aerodiges- tive tract. The presence of β-2 transferrin is the gold standard for the diagnosis of CSF leak.
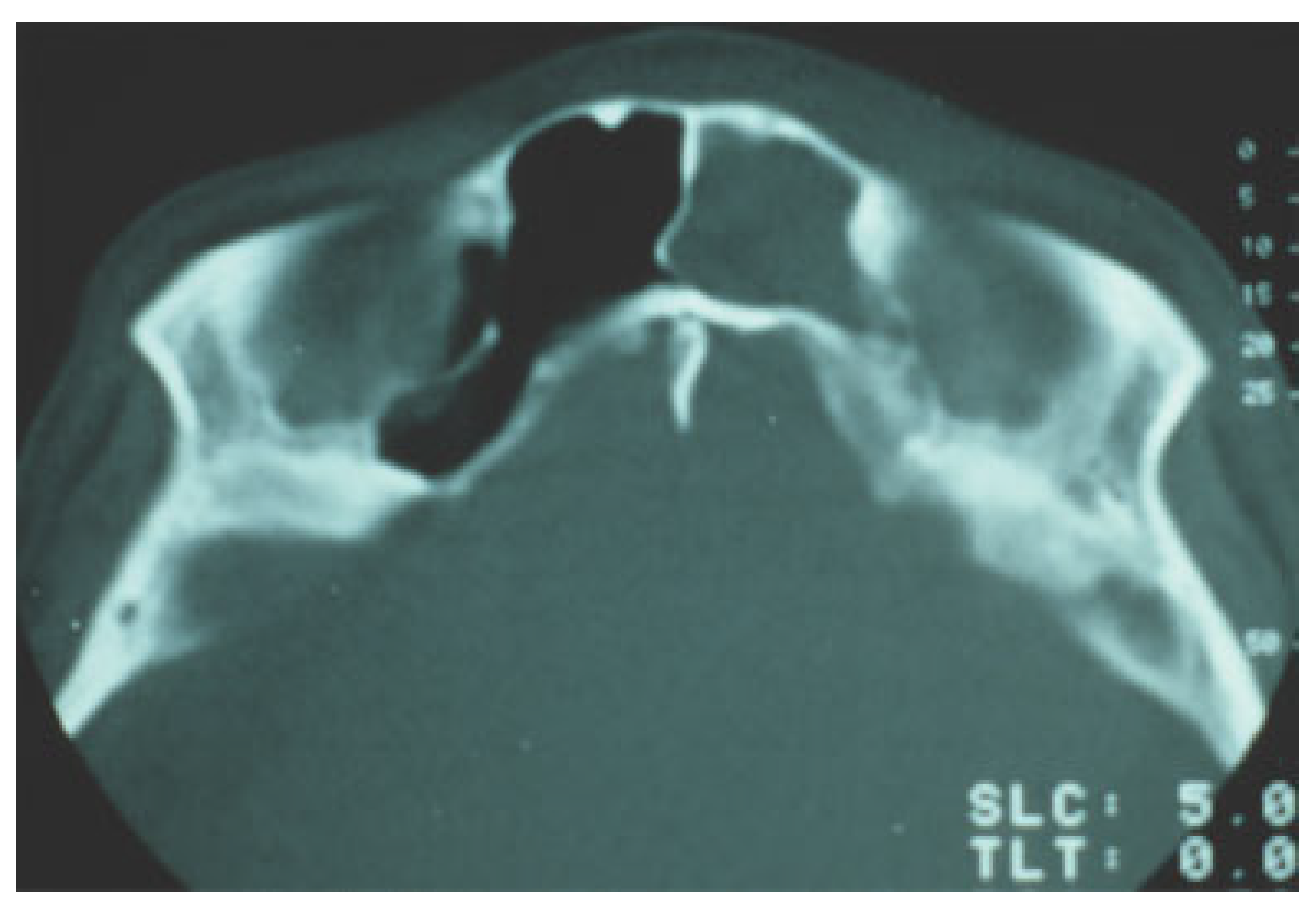
The advances in computed tomography (CT) technology have greatly enhanced diagnosis and treatment planning of frontal sinus fractures. CT scans have improved assessment of posterior wall and nasofrontal outflow tract injury. Nasofrontal outflow tract injury is found in 13 to 55% of the frontal sinus fracture cases[
7]; thus, preoperative determination of patency, if possible, is crucial to management. The two imaging findings of outflow tractobstruction are a sinus air–fluid level and fracture involvement of the tract in the sagittal view.[
8,
9] The index of suspicion should be high of an injury to the drainage tract in the presence of associated nasoethmoid fractures (
Figure 2).
Treatment
The ultimate goals in the management of frontal sinus frac- tures are restoration of form and function such as forehead contour and structural integrity, and prevention of early and late complications. Short-term complications include CSF leak, meningitis, and epidural abscess. Long-term complications include frontal bone osteomyelitis, mucocele, mucopyocele, and brain abscess. In 1954, Lewin demonstrated the risk of subsequent meningitis to be at least 25% in patients with CSF rhinorrhea and posterior table fracture in the absence of dural repair.[
10] Surgical repair of dura reduced the overall risk of meningitis from 30% preoperatively to 4% after surgery with a reduction in the cumulative risk at 10 years from 85% before dural repair to 7% after dural repair.[
11] In their 1998 publica- tion, Sakas et al identified several factors on neuroimaging that were linked to high long-term risk of developing posttraumatic meningitis[
12]:
Proximity of the fracture to the midline cribriform plate.
Large fracture displacement (>1 cm).
Prolonged rhinorrhea (>8 days).
Treatment decisions depend on fracture type, comminu- tion, degree of posterior tablefracture, nasofrontal duct injury, neurological status, and CSF leak.[
13] Rodriguez et al developed a treatment algorithm based on the fracture patterns with consideration for nasofrontal outflow tract injury.[
14] In non- displaced fractures of frontal sinus with a patent nasofrontal duct, only clinical observation with head elevation and sinus precaution is needed. For frontal sinus fractures with naso-frontal duct outflow obstruction, either sinus obliteration or cranialization is indicated depending on posterior wall invol- vement. In displaced frontal sinus fractures with no obstruc- tion of the nasofrontal duct, reconstruction of the anterior wall is indicated.
Adequate exposure of the affected region is crucial for intraoperative assessment of the fracture. Existing lacera- tions are useful only in cases of minor isolated anterior table fractures. Most commonly, the fractures should be exposed with a bicoronal incision. The coronal flap is elevated in the subgaleal plane, and dissection extends inferiorly to supraor- bital rims and nasoglabellar junction medially and fronto- zygomatic suture line laterally. Some consideration should be given to the necessity of a pericranial flap. If so, the dissection at a point 6 to 8 cm from the supraorbital rims shifts from subgaleal to the subperiosteal plane. If not, the subperiosteal plane is entered 2 cm superior to enable protection of the supraorbital nerve and artery.
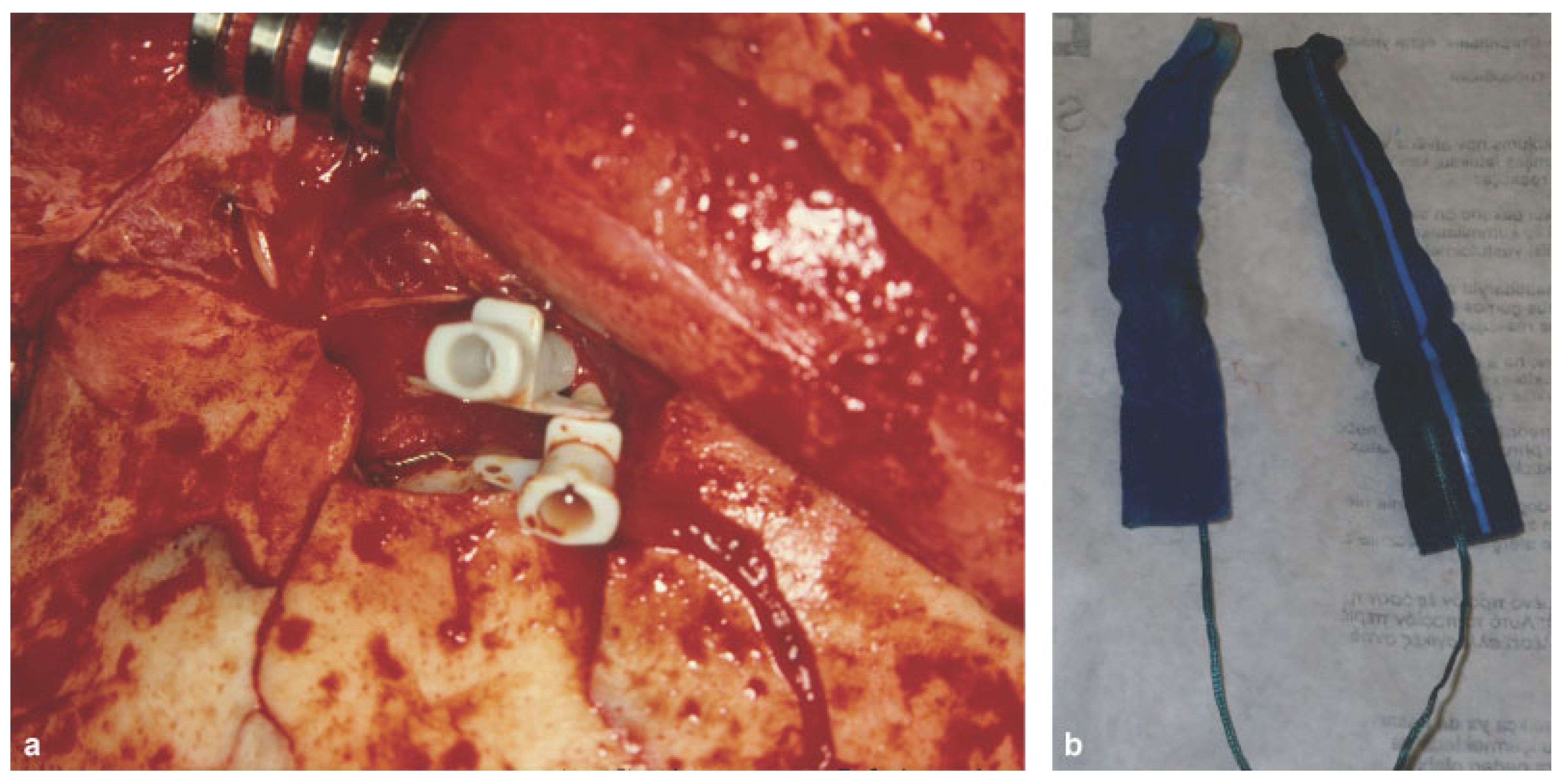
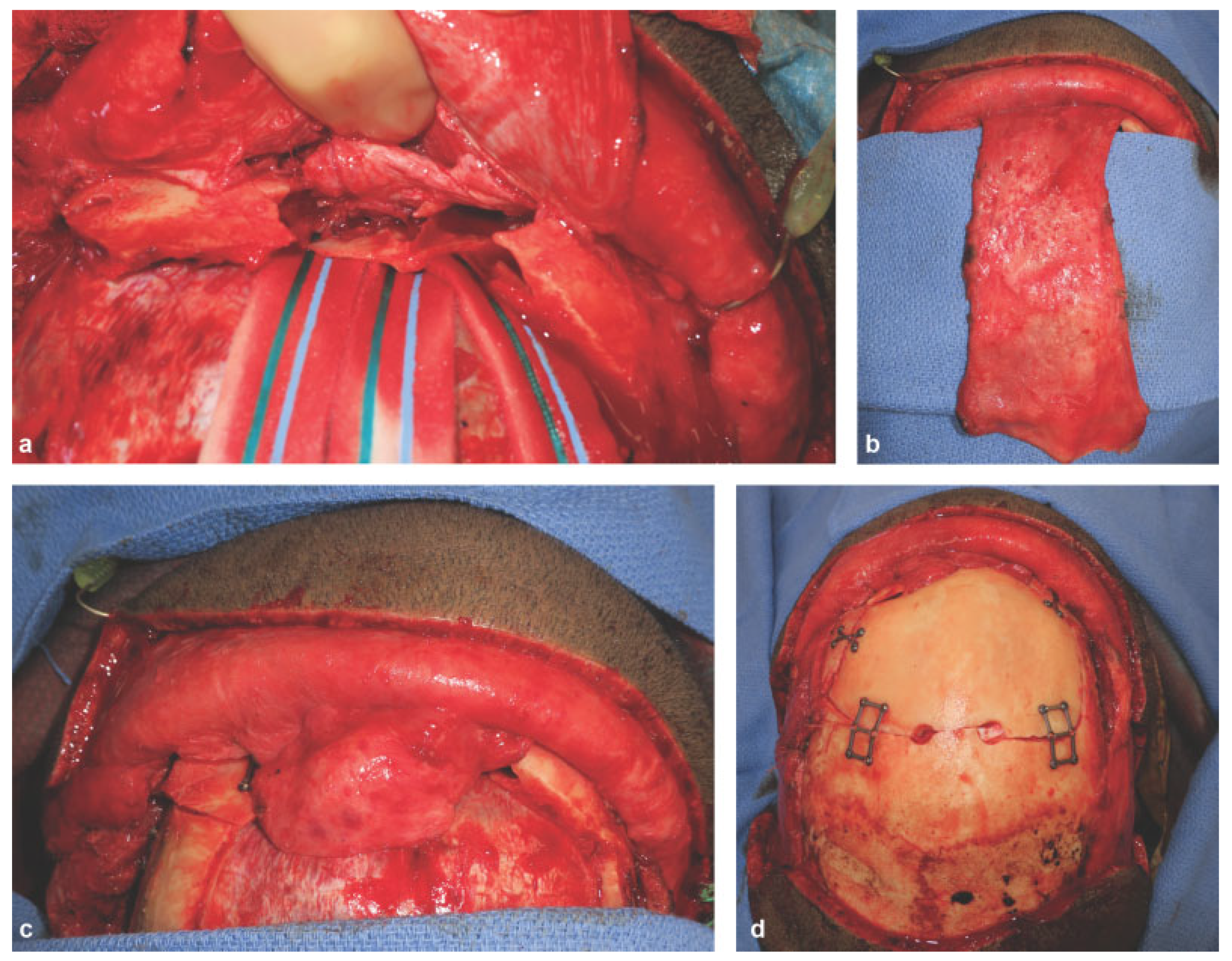
For isolated displaced anterior table fractures, standard reduction and rigid fixation is sufficient. Low profile 1.0-mm microplates are used in palpable areas. If frontonasal duct injury is suspected, the duct is first examined for patency prior to fixation. Fragments are disimpacted and removed to visua- lize the base of the sinus frontonasal ducts. Methylene blue is injected into the duct with a polyethylene catheter and a cotton tip applicator or cottonoids are placed into the nose near the middle meatus (
Figure 3a). If dye is detected, the frontonasal ducts are patent (
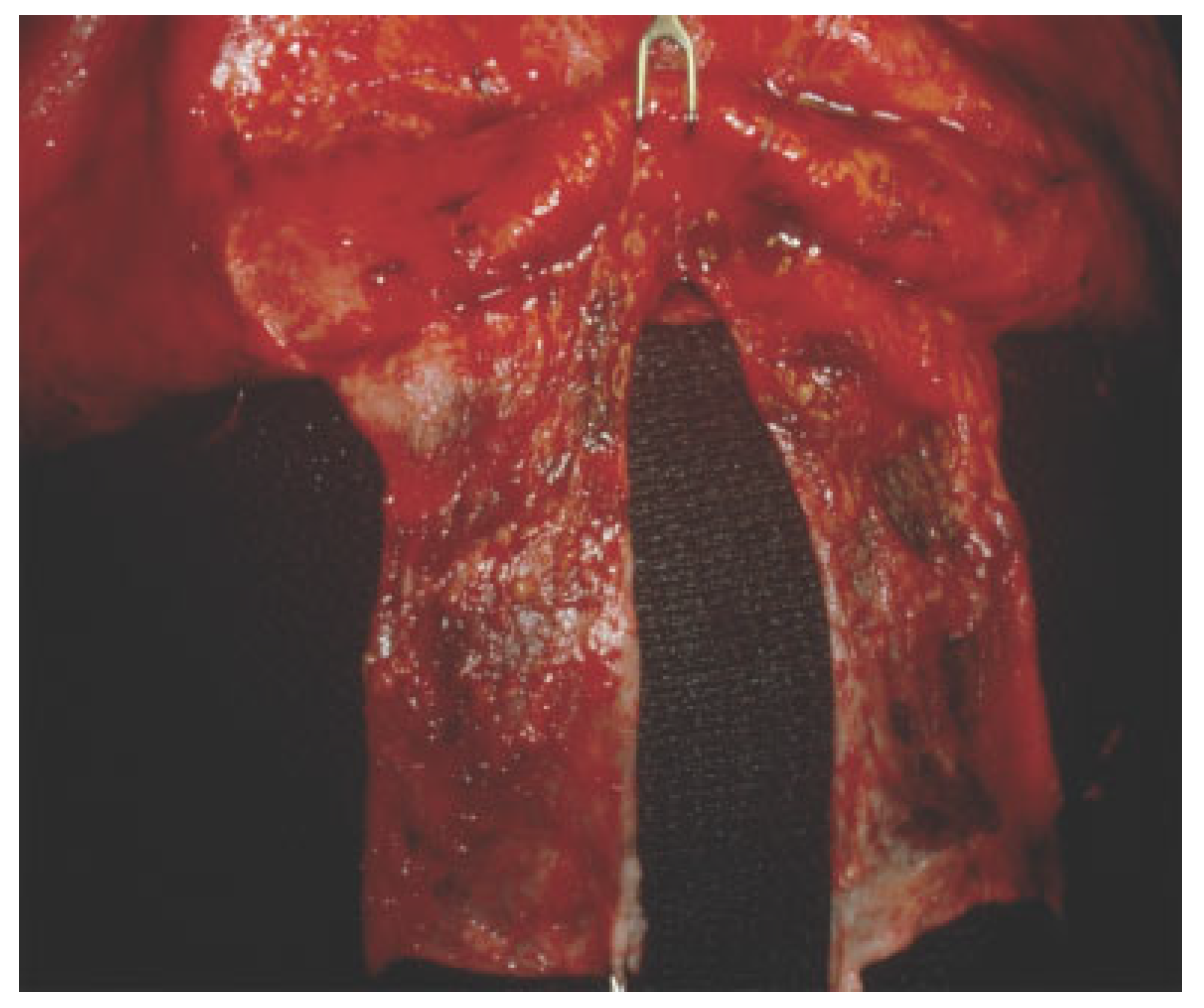
Figure 3b). If no dye is visualized or if significant doubt exists about frontonasal patency, the sinus should be obliterated. Frontal sinus obliteration is defined as obliteration of the aerated frontal sinus cavity during the maintenance of intact bony walls. Sinus mucosa is removed and mucosal curettage is performed with high speed burr. Attention is directed particularly along the posterior sinus wall toward the foramina of Breschet. The frontonasal duct can be pluggedwitha pericranial flap[
15] (
Figure 4). The optimalmethod for frontal sinus obliteration has been the subject of great debate. Many graft options exist including fat, dermis, fascia, muscle, bone, and alloplastic material such as silicone, Surgicel, and hydroxyapatite.[
16,
17,
18] However, alloplastic material is not recommended because the surgical site is considered a con- taminated area and the increased risk of postoperative infec- tion. Spontaneous osteoneogenesis has been described for frontal sinus obliteration in which nothing is placed in the sinus to allow fibrous tissue ingrowth and formation of new bone.[
19] In the experimental setting, the obliteration is often incomplete and complicated by infection. Rohrich and Mickel compared frontal sinus obliteration using fat, muscle, bone, and spontaneous osteoneogenesis in a cat model and literature review found no differences in the material used.[
20] They concluded that successful obliteration of frontal sinus by either spontaneous osteoneogenesis or the implantation of autoge- nous fat, muscle, or bone depends on meticulous extirpation of the frontal sinus mucosa with the aid of an operating micro- scope, removal of the inner cortex of bone, and permanent occlusion of the nasofrontal duct.[
20,
21] Cranialization should be considered when the anatomic barrier between the sinus and intracranial cavity has been disrupted secondary to fractures of the posterior wall and dural tears.[
22] Cranialization involves removal of the entire posterior sinus wall and debridement of all sinus mucosa, followed by frontonasal duct blockade with pericranial flap and/or autogenous bone (
Figure 5a–d).
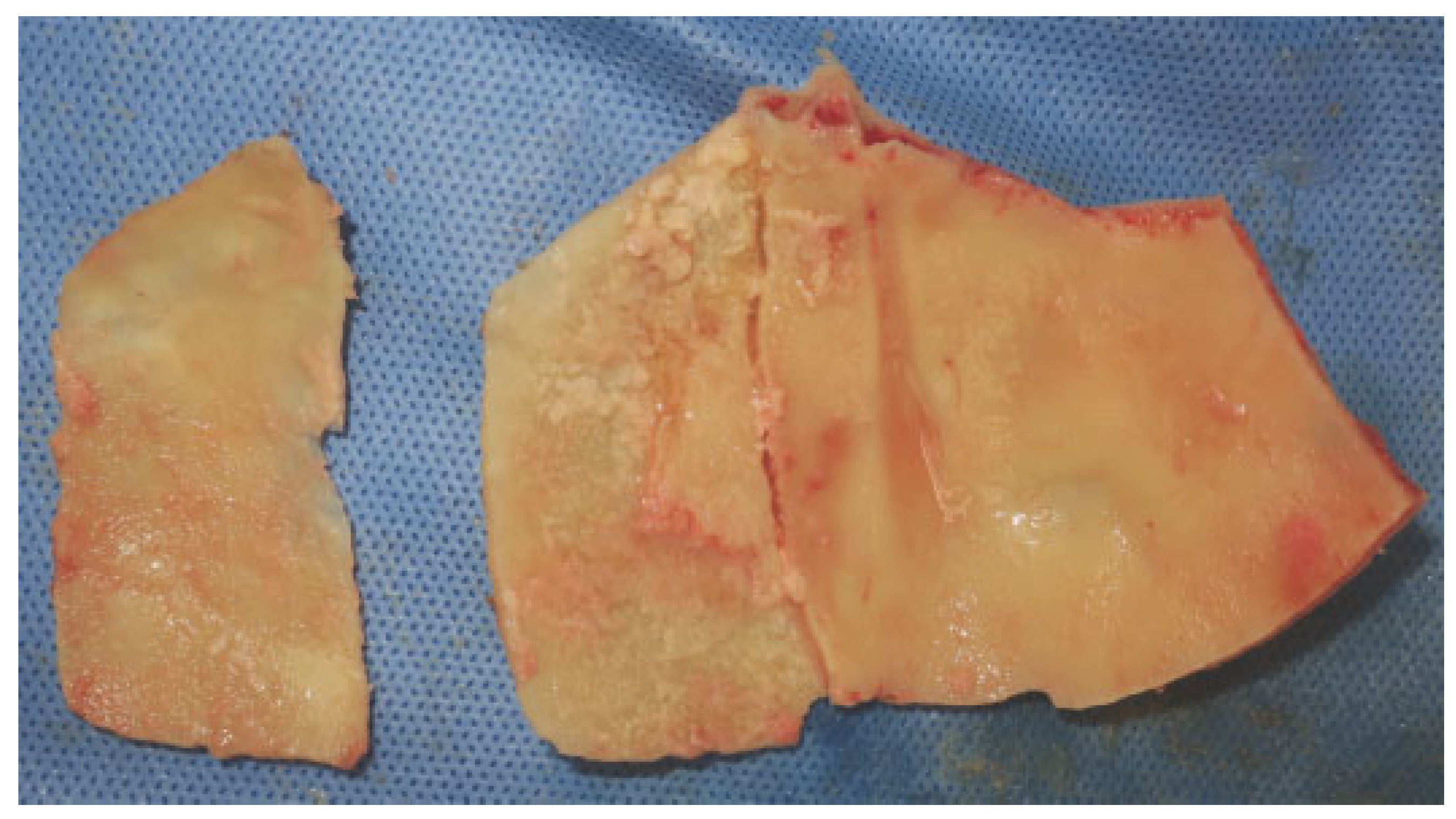
In cases of severe comminution, bony loss, and instability, reconstruction of the anterior table can be done with auto- genous bone graft. There are several sources for nonvascu- larized autologous bone graft including calvarium, ribs, ilium, temporal fossa, and patella.[
23,
24] Free rib grafts have been shown to partially resorb, thus leading to secondary deformities. Although iliac bone has been used extensively in the past, at present most surgeons prefer split calvarial bone graft[
25] (
Figure 6).
Complications
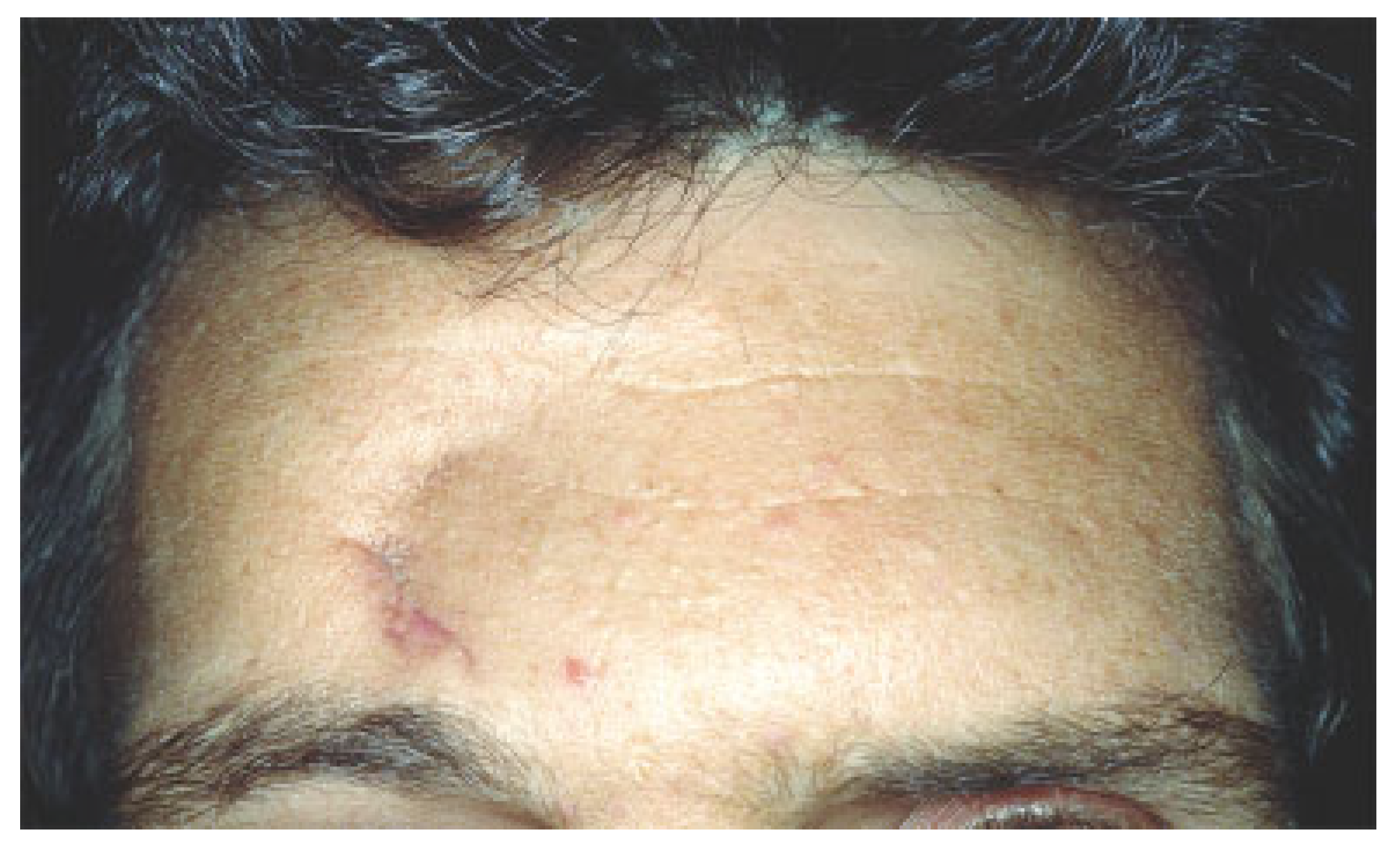
Earlycomplications occur within the first few weeks of surgery. Intracranial hemorrhage pneumocephalus, cerebral contusion, and increased intracranial pressure are associated with frontal sinus fractures but are relatively uncommon. Contour defor- mities can occur, particularly when observation alone has been the mode of treatment (
Figure 7). Paresthesias in the supratro-chlear and supraorbital distributions are usually transient but have a long-term incidence ofpermanentdysesthesia of 5%. The most significant early complication is a CSF leak. CSF leaks are troublesome in the presence of intracranial injury. Postopera- tive CSF rhinorrhea is usually secondary to a fracture of the cribriform plate or other basilar skull fracture. Conservative management is indicated in most instances. The indications for procedures to address this scenario are beyond the scope of this discussion.
Meningitis can occur in frontal sinus fracture patients and may not be associated with an active CSF leak.[
26] As these patients may be neurologically compromised from a head injury, they are uniquely susceptible to the consequences of meningitis. Attention should be directed toward postoperative patients for signs of fever, hypotension, mental status changes, or neck rigidity. Use of broad-spectrum antibiotics with good CSF penetration is an essential first step. Antibiotics should be adjusted following the results of CSF cultures.
Mucoceles or mucopyocele are long-term complications from untreated fractures or failure to recognize frontonasal duct obstruction. Sinus malfunction proceeds through an indolent course and presents many years after initial frontal sinus injury management.[
27] The natural course for a mucocele is slow, insidious expansion following the initial injury.[
28] Mucoceles cause progressive bone erosion and are capable of involvement of the sinus, the orbit, and the cranium.[
29] Since mucoceles are slow growing and produce few symptoms, they present late in their development only after orbital or cranial invasion has already occurred. The most frequent complaints are frontal headache, nasal purulent drainage, frontal sinus tenderness, and fluctuant swelling of the forehead. Secondary involvement of the orbit creates visual disturbances, orbital dystopia, and ocular dysfunction. Central nervous system sequelae may present with more serious clinical signs and symptoms, such as seizures, headaches, photophobia, and nuchal rigidity. Complete removal of the mucocele and recon-struction of the cranial vault or orbit and nasal cavity is the treatment method of choice.[
30]
Frontal bone osteomyelitis is a rare complication and occurs mostly in frontal sinus fractures when alloplastic material has been implanted that subsequently becomes secondarily infected. Osteomyelitis requires complete excision of the involved frontal bone, treatment with long-term antibiotics, and subsequent reconstruction of the frontal bone after infec- tion has resolved.
Various options are available to correct contour deformi- ties of the forehead: autogenous bone such as split calvarial bone graft or allogenic products such as demineralized bone matrix (DBM). DBM is produced after acid extraction of donor stock long diaphyses, retaining the collagen scaffold for osteoconduction and growth factors, such as bone mor- phogenic protein. The quantity of bone morphogenic protein in different preparations of DBM varies considerably by commercial vendors. Commercial DBM has been mixed with carriers such as hyaluronan (DBX; Synthes USA, West Chester, PA), calcium sulfate (Allomatrix; Wright Medical Technology, Inc., Arlington, TN), glycerol (Grafton; Osteo- tech, Eatontown, NJ), or gelatin (Regenafil; Regeneration Technologies Inc, Alachua, FL) for improved clinical handling and localization of DBM particles within the surgical reci- pient site. Acarturk and Hollinger[
31] have demonstrated in their animal model that DBX and Grafton produce more bone formation than Allomatrix, Dynagraft, and Regenafil due to the quantity of particulate DBM within the critical size defect and perhaps because DBX and Grafton are more localized to the implant site.
Minimally Invasive and Nonoperative Management
The operative management of frontal sinus fractures implies access via a bicoronal incision, an approach not devoid of negative implications including, on occasion, an unsatisfac- tory scar. In some patients with receding frontal hairline, those implications become more of a concern. As a result, some interest exists in either a less invasive or a nonopera- tive approach, particularly perhaps in patients with isolated anterior wall fractures, patients in whom the treatment indications are primarily aesthetic.
Investigators have described an endoscopic approach, either through a brow incision, hairline, or transnasal access.[
32,
33] These approaches have either utilized the endo-scope to enable a small skin incision for reduction without internal fixation or endoscopic confirmation by a transnasal passage to ascertain the patency of the nasofrontal duct. The liability of an endoscopic technique is the inability to per- form, with any degree of facility, internal fixation of the reduced anterior wall fragments. A transnasal endoscopic procedure does enable assessment of the frontal sinus drai- nage system but often requires a variation of an internal ethmoidectomy as well as increased operative time and a steep learning curve. Nevertheless, with development of the technology, a minimally invasive approach to frontal sinus fractures may play a more prominent role in the future.
In the same vein, some recent interest in a selected con- servative management of a band of the spectrum of frontal sinus fractures has been discussed.[
34] If an acuity exists of frontal sinus fractures from least, namely, nondisplaced ante- rior wall to that of the most severe, open, comminuted injuries with bone loss, attended by disruption of the posterior wall, dural tears, and CSF leak, an opportunity exists perhaps for the nonoperative treatment of the lesser degree of severity. Poster- ior wall injury and/or outflow tract obstruction merits opera-tive intervention primarily because of the nature of the potential complications, epidural/subdural abscess, or muco- pyocele. Conceivably, as described, an anterior wall fracture even with some degree of displacement could be managed with observation alone, further treatment dictated by follow- up examination including CT scan.