Posttraumatic Lateral Dislocation of Mandibular Condyle: A Proposed New Classification with Report of 14 Dislocated Condyles
Abstract
Materials and Methods
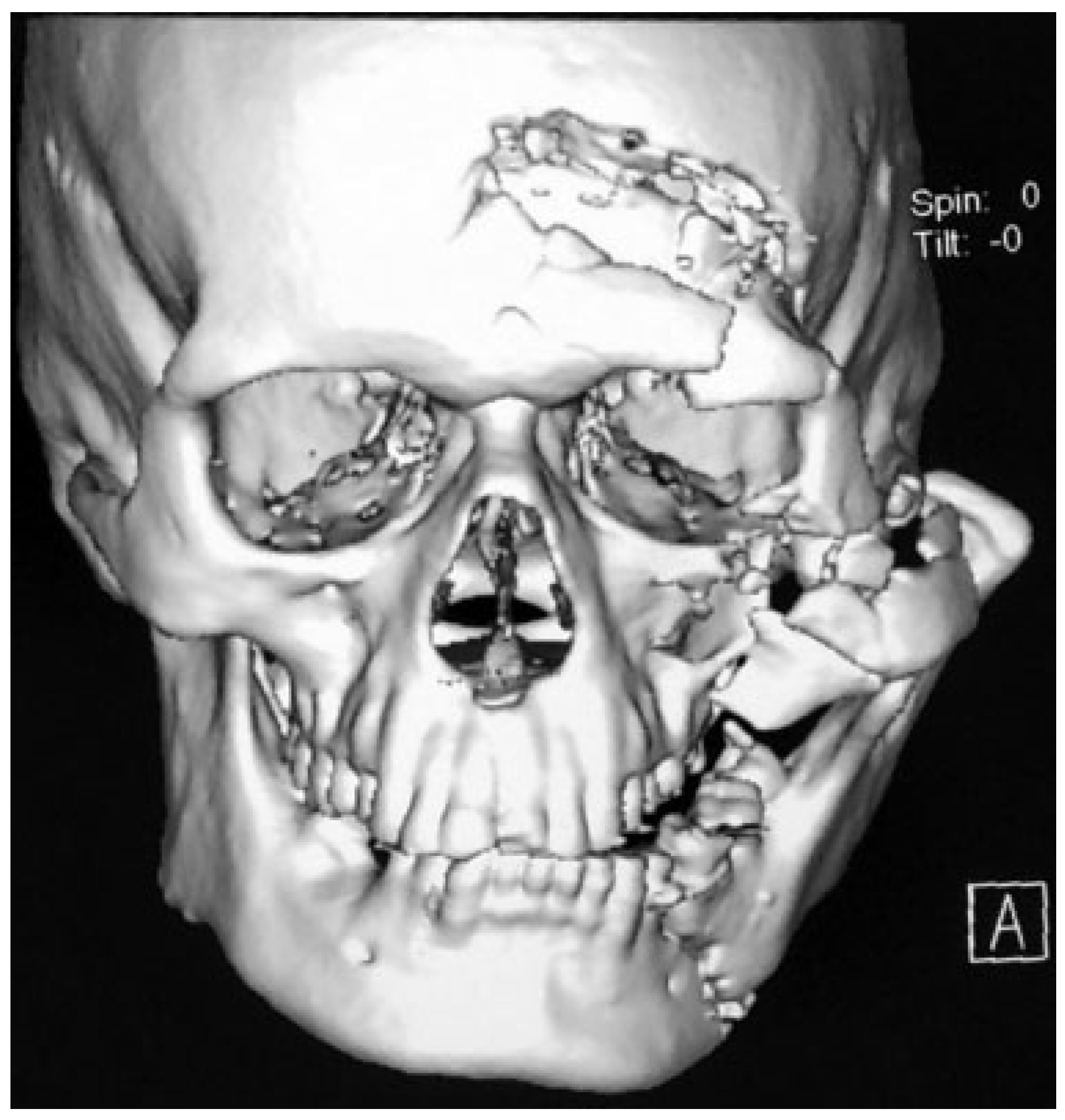
Results
Discussion
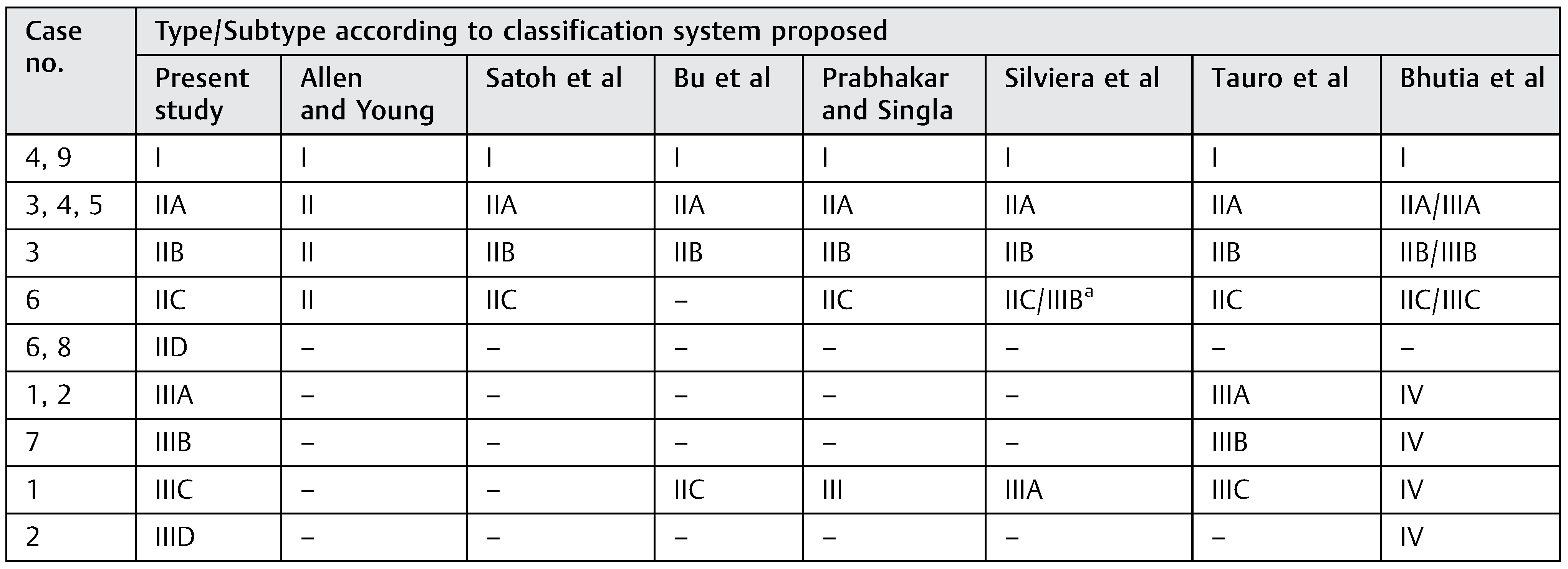
- There is an overlapping between the various types proposed in different classification systems. For example, type IV of Bhutia et al. [9] could be type IIIA of Silviera et al.’s [7] classification, type III of Prabhakar’s and Singla’s [6] classification, and type IIIA/B/C of Tauro et al.’s [8] classification (Table 2).
- One given type in some classification systems accounts for many variable clinical presentations. For example, in the classification system proposed by Bhutia et al., [9] type IV accounts for complete dislocations with an intact mandible. This may include type IIIA, B, and C of Tauro et al.’s [8] classification; each of which corresponds to a different type of presentation (Table 2).
- Type I: Lateral subluxation.
- Type II: Complete dislocation with fracture of anterior/posterior mandible.
- IIA: Condyle not hooked above zygomatic arch.
- IIB: Condyle hooked above zygomatic arch.
- IIC: Condyle medial to fractured zygomatic arch.
- IID: Condyle medial to intact zygomatic arch.
- Type III: Complete dislocation without fracture of anterior/posterior mandible.
- IIIA: Condyle not hooked above zygomatic arch.
- IIIB: Condyle hooked above zygomatic arch.
- IIIC: Condyle medial to fractured zygomatic arch.
- IIID: Condyle medial to intact zygomatic arch.
Funding
Acknowledgments
Conflicts of Interest
References
- Li, Z.; Li, Z.B.; Shang, Z.J.; Wu, Z.X. An unusual type of superolateral dislocation of mandibular condyle: Discussion of the causative mechanisms and clinical characteristics. J Oral Maxillofac Surg 2009, 67, 431–435. [Google Scholar] [CrossRef]
- Rahman, T. Unusual superolateral dislocation of mandibular condyle. Craniomaxillofac Trauma Reconstr 2018, 11, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Allen, F.J.; Young, A.H. Lateral displacement of the intact mandibular condyle. A report of five cases. Br J Oral Surg 1969, 7, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Satoh, K.; Suzuki, H.; Matsuzaki, S. A type II lateral dislocation of bilateral intact mandibular condyles with a proposed new classification. Plast Reconstr Surg 1994, 93, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Bu, S.S.; Jin, S.L.; Yin, L. Superolateral dislocation of the intact mandibular condyle into the temporal fossa: Review of the literature and report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007, 103, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Prabhakar, V.; Singla, S. Bilateral anterosuperior dislocation of intact mandibular condyles in the temporal fossa. Int J Oral Maxillofac Surg 2011, 40, 640–643. [Google Scholar] [CrossRef] [PubMed]
- Silviera, R.L.; Ranuzia, I.; Melo, M.F.S.; de Oliveira, R.A.; de Brito, A.A.; Vidigal, V.L. Traumatic anterosuperior dislocation of the intact mandibular condyle into the temporal fossa. Craniomaxillofac Trauma Reconstr 2018, 11, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Tauro, D.; Lakshmi, S.; Mishra, M. Superolateral dislocation of the mandibular condyle: Report of a case with review of literature and a proposed modification in the classification. Craniomaxillofac Trauma Reconstr 2010, 3, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Bhutia, D.P.; Mehrotra, D.; Mahajan, N.; Howlader, D.; Gamit, J. Posttraumatic superolateral dislocation of condyle: A case series of 18 condyles with review of literature and a proposed classification. J Oral Biol Craniofac Res 2017, 7, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Worthington, P. Dislocation of the mandibular condyle into the temporal fossa. J Maxillofac Surg 1982, 10, 24–27. [Google Scholar] [CrossRef] [PubMed]

 |
 |
© 2019 by the author. The Author(s) 2019.
Share and Cite
Rahman, T.; Hashmi, G.S.; Ahmed, S.S.; Rahman, S.A. Posttraumatic Lateral Dislocation of Mandibular Condyle: A Proposed New Classification with Report of 14 Dislocated Condyles. Craniomaxillofac. Trauma Reconstr. 2019, 12, 249-253. https://doi.org/10.1055/s-0039-1677725
Rahman T, Hashmi GS, Ahmed SS, Rahman SA. Posttraumatic Lateral Dislocation of Mandibular Condyle: A Proposed New Classification with Report of 14 Dislocated Condyles. Craniomaxillofacial Trauma & Reconstruction. 2019; 12(4):249-253. https://doi.org/10.1055/s-0039-1677725
Chicago/Turabian StyleRahman, Tabishur, Ghulam Sarwar Hashmi, Syed Saeed Ahmed, and Sajjad Abdur Rahman. 2019. "Posttraumatic Lateral Dislocation of Mandibular Condyle: A Proposed New Classification with Report of 14 Dislocated Condyles" Craniomaxillofacial Trauma & Reconstruction 12, no. 4: 249-253. https://doi.org/10.1055/s-0039-1677725
APA StyleRahman, T., Hashmi, G. S., Ahmed, S. S., & Rahman, S. A. (2019). Posttraumatic Lateral Dislocation of Mandibular Condyle: A Proposed New Classification with Report of 14 Dislocated Condyles. Craniomaxillofacial Trauma & Reconstruction, 12(4), 249-253. https://doi.org/10.1055/s-0039-1677725



