Abstract
Nasal fractures account for up to 58% of facial fractures. However, the literature characterizing associated injuries and risk factors for nasal fractures is sparse and is mostly composed of single-center experiences. This study sought to provide a large descriptive analysis and identify associated injuries and risk factors for nasal fractures in trauma using a national database. A retrospective analysis of the National Trauma Data Bank (NTDB) from 2007 to 2015 was performed. Patients ≥18 years of age with nasal fractures were included. A multivariable logistic regression model was used to identify predictors for nasal fracture in trauma. Of 5,494,609 trauma patients in the NTDB, 255,533 (4.6%) had a nasal fracture. Most were male (74.8%) with a mean age of 45.6 years. Blunt trauma accounted for 90.5% of fractures, with motor vehicle accident being the most common mechanism (27.5%). Closed fractures occurred in 93.0% of patients. Concomitant injuries included traumatic brain injury (TBI; 56.9%), malar/maxillary fracture (27.9%), and open wound of the face (38.6%) and nose (9.5%). Of all patients, 10.1% underwent closed or open reductions at index hospitalization. The strongest associated injuries with nasal fracture included open wound of the nose (odds ratio [OR]: 8.71, 95% confidence interval [CI]: 8.49–8.94, p < 0.001), epistaxis (OR: 5.26, 95% CI: 4.59–6.02, p < 0.001), malar/maxillary fracture (OR: 4.38, 95% CI: 4.30–4.45, p < 0.001), and orbital fracture (OR: 3.99, 95% CI: 3.91–4.06, p < 0.001). Nasal fractures are common traumatic injuries with more than 90% occurring by blunt mechanism and over half suffering from a concomitant TBI. The strongest associated injury with nasal fracture is an open wound of the nose.
Nasal fractures are the most common type of facial fracture, accounting for 40 to 58% of facial fractures.[1,2,3] The nasal bone is also the third most commonly broken bone in the body.[4] For patients with multiple system injuries, attention to life- threatening injuries takes precedence over injuries, such as nasal fractures. However, a nasal fracture may be an indi- cator of underlying serious facial and head trauma, or other concomitant lethal injury. Additionally, there are also serious sequelae of these injuries including unrelenting epistaxis, nasal airway compromise, or secondary deformity. Func- tional and cosmetic defects have been associated with delayed time to treatment.[5] Thus, early diagnosis and man- agement is crucial.
Physical examination and the mechanism of injury influ- ence a physician’s decision to pursue imaging. Hence, iden- tifying associated injuries and risk factors for nasal fractures is helpful in guiding this evaluation, especially when physical examination may be unrevealing.[2]
In prior studies and populations, the descriptive epide- miology and demographics of patients who sustain facial fractures, including nasal fractures, have varied signifi- cantly.[6,7,8,9,10,11] The most common mechanisms of injury identi- fied to cause nasal fractures include motor vehicle accidents (MVAs), assaults, and falls depending on the age, gender, and other demographics of the population studied.[2,6,8,10] These studies, however, were often from a single center and utilize a relatively small population size.[8,12,13,14,15,16,17]
Therefore, we sought to perform a large descriptive ana- lysis of demographics, concomitant injuries, surgical inter- ventions, and outcomes associated with nasal fractures in patients who present as trauma activations. Second, we aimed to identify associated injuries and risk factors for nasal fractures in trauma.
Materials and Methods
National Trauma Data Bank
A retrospective analysis of the National Trauma Data Bank (NTDB) between 2007 and 2015 was performed. The NTDB, managed by the American College of Surgeons, is the largest aggregated database of trauma patients in the United States and is considered one of the leading performance improve- ment tools for trauma care.[18] The NTDB encourages volun- tary participation from trauma centers across the nation, and includes data regarding patients who presented to the hospital as trauma activations. As of 2018, the NTDB includes data from over 850 trauma centers across 50 states. This study utilizes de-identified data and was exempt by the Institutional Review Board at the University of California, Irvine School of Medicine.
The NTDB was queried for all patients ≥18 years of age with nasal fractures. International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes were used to identify adult patients with both closed (802) and open (802.1) nasal bone fractures. Baseline patient charac-teristics were collected, including age, sex, social history, and whether hypotension (systolic blood pressure <90 mm Hg) on admission was present. Severity of overall trauma was assessed using the injury severity score (ISS) and the abbre- viated injury scale (AIS) score for each body region.[19,20] Various comorbidities, mechanisms of injury, and associated injuries were also queried in our analysis. Facial fractures were categorized by location—for example, the mandible, malar/maxilla, and orbital bone. Panfacial fracture was defined in patients with the combination of mandible, max- illa, and orbital fracture. Open wound of the nose included the nose, nasal septum, nasal cavity, and nasal sinus. Open wound of the face included those of the cheek, forehead, lip, jaw, and other sites of the face. Outcome measures of mean length of stay (LOS), intensive care unit (ICU) LOS, ventilator days, open or closed nasal reduction, complications, and mortality were also evaluated. Furthermore, we analyzed demographics and outcomes in patients with an isolated nasal fracture. This was defined by patients presenting with a nasal fracture, without an orbital, maxilla, mandible, or other facial fracture.
Statistical Analysis
A univariable logistic regression was performed to identify associated injuries and predictors for adult trauma patients with nasal fracture. After adjusting for covariates, a multi- variable logistic regression was performed to more accu- rately identify associated injuries and predictors for nasal fracture. Comparisons were considered statistically signifi- cant at a two-sided p-value of less than 0.5. All statistical analyses were performed with IBM SPSS Statistics for Win- dows, Version 24 (IBM Corp, Armonk, NY).
Results
Demographics
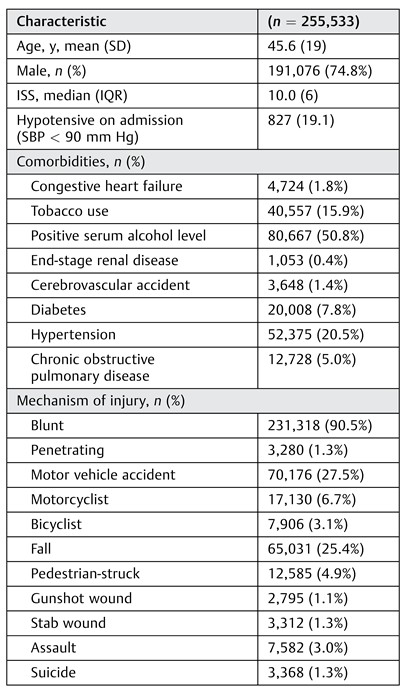
Of 5,494,609 patients in the NTDB during the years of this study, 255,533 (4.6%) had a nasal fracture (Table 1). The majority of these patients were male (74.8%) with a mean age of 45.6 years. The most commonly associated comorbidities were positive serum alcohol level (50.8%), hypertension (20.5%), tobacco use (15.9%), and diabetes (7.8%).

Table 1.
Demographics of adult trauma patients with nasal fracture.
Mechanism of Injury
Blunt trauma accounted for 90.5% of nasal fractures with the most common mechanism being MVA (27.5%, n = 70,176), followed by motorcycle collisions (6.7%, n = 17,130) and bicycle accidents (3.1%, n = 7,906; Table 1). Penetrating trauma accounted for only 1.3% of patients with a nasal fracture (n = 3,280).
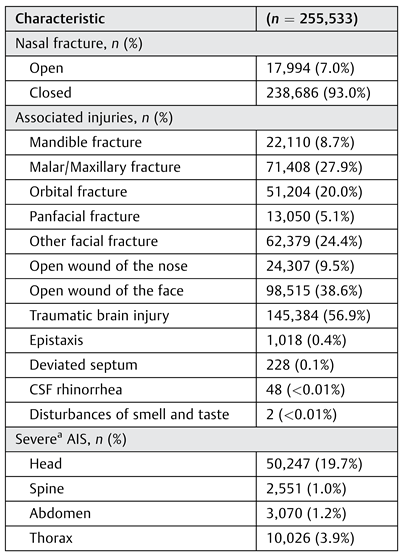
Injuries Sustained
Closed nasal fractures occurred in 93.0% (n = 238,686) of patients, while open nasal fractures occurred in the remain- der (Table 1). Patients with a nasal fracture presenting as a trauma activation had a median ISS of 10.0 (interquartile range: 6). Traumatic brain injury (TBI) (56.9%, n = 145,384) was an associated injury in more than half of nasal fracture cases. Additional facial fractures included malar/maxillary fractures (27.9%, n = 71,408), orbital fracture (20.0%, n = 51,204), other facial fracture (24.4%, n = 62,379), pan-facial fracture (8.7%, n = 13,050), and mandibular fracture (5.1%, n = 22,110). Although open wound of the face was associated with 38.6% of patients with nasal fractures, open wound of the nose was associated with only 9.5%. Deviated septum was diagnosed in 0.1% of patients. Other complica- tions such as loss of smell/taste (n = 2, <0.01%) and cere-brospinal fluid rhinorrhea (n = 48, <0.01%) were rare.
Outcomes
Of all patients, 10.1% underwent some form of surgical inter- vention during index hospitalization: 7.5% underwent closed reduction and 2.6% underwent open reduction (Table 2). The mean overall LOS was 6.9 days (standard deviation [SD]: 11) and mean ICU LOS was 6.5 days (SD: 9). Similarly, the mean days of ventilator usewas 6.7 days (SD: 9). The mortality rate in patients with nasal fractures was low at 4.4%. Although complications were generally low, the most common compli- cation was pneumonia (4.3%), followed by acute respiratory distress syndrome (ARDS; 2.0%; Table 2). Osteomyelitis occurred only in 41 (<0.1%) of the 255,533 included patients with nasal fractures.

Table 2.
Analysis of clinical outcomes in adult trauma patients with nasal fracture.
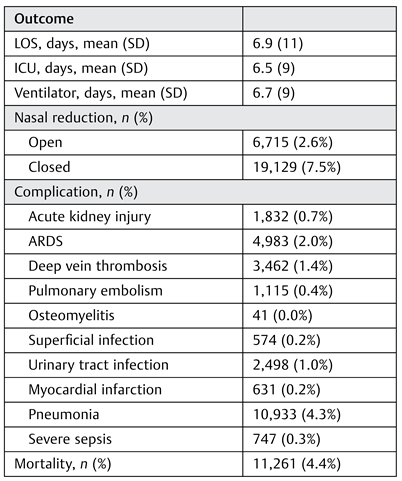
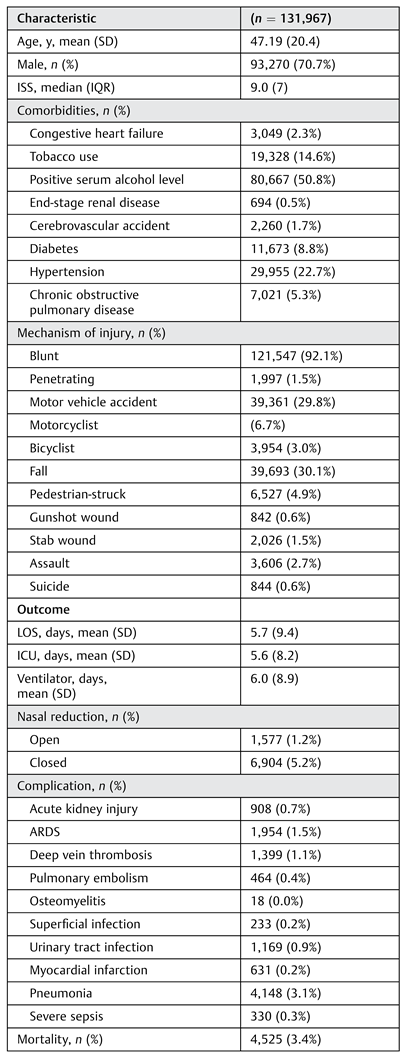
Demographics and Outcomes of Isolated Nasal Fractures
Of those with nasal fractures, 131,967 (51.6%) were isolated nasal fractures, with 93.7% as closed fractures (Table 3). Most were male (70.7%) with mean age of 47.2 years. The most commonly associated comorbidities were positive serum alcohol level (31.8%), hypertension (22.7%), tobacco use (14.6%), and diabetes (8.8%). Blunt trauma accounted for 92.1% of isolated nasal fractures with the most common mechanism being fall (30.1%, n = 39,693), followed by MVA (29.8%, n = 39,361). Of patients with isolated nasal fractures, 5.2% underwent closed reduction and 1.2% underwent open reduction. The mean overall LOS was 5.7 days (SD: 9.4) and mean ICU LOS was 5.6 days (SD: 8.2). The mortality rate was low at 3.4%, with the most common complication being pneumonia (3.1%), followed by ARDS (1.5%).

Table 3.
Demographics and outcomes for isolated nasal fracture in adult trauma patients.
Associated Injuries and Predictors
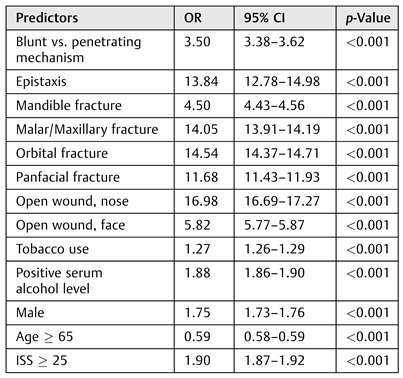
Univariable analysis identified the presence of an open wound to the nose as thestrongest associated injury for nasal fractures (odds ratio [OR]: 16.98, 95% confidence interval [CI]: 16.69–17.27, p < 0.001; Table 4), followed by orbital fractures (OR: 14.54, 95% CI: 14.37–14.71, p < 0.001), malar/maxillary frac-tures (OR: 14.05, 95% CI: 13.91–14.19, p < 0.001), and epis-taxis (OR: 13.84, 95% CI: 12.78–14.98). Blunt trauma mechanisms (OR: 3.50, 95% CI: 3.38–3.62, p < 0.001) and ISS ≥ 25 (OR: 1.90, 95% CI: 1.87–1.92, p < 0.001) were also associated with higher odds of nasal fracture.

Table 4.
Univariable analysis of associated injuries and predictors for nasal fractures in adult trauma patients.
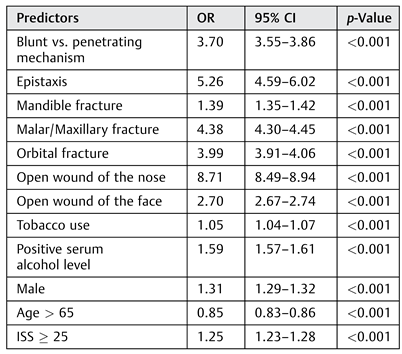
After adjusting for covariates in a multivariable logistic regression model (Table 5), the strongest independent associated injury for nasal fractures continued to be an open wound of the nose (OR: 8.71, 95% CI: 8.49–8.94, p < 0.001). Epistaxis was the second strongest independent association (OR: 5.26, 95% CI: 4.59–6.02, p < 0.001). Simi-larly, malar/maxillary fractures (OR: 4.38, 95% CI: 4.30–4.45, p < 0.001) and orbital fractures (OR: 3.99, 95% CI: 3.91–4.06, p < 0.001) had the next highest odds.

Table 5.
Adjusted odds ratio for associated injuries and predictors for nasal fracture in adult trauma patients.
Discussion
This retrospective review of 255,533 nasal fractures identi-fied the epidemiology, outcomes, associated injuries, and risk factors for nasal fractures using data from trauma centers across the United States. To our knowledge, this study is the largest national study evaluating nasal fractures with these fractures affecting 4.6% of the subjects in the database. Over 90% of these nasal fractures occurred by blunt trauma, with 27.5% by MVAs. The most commonly associated injury was a TBI, which occurred in over half of the patients. Independently associated injuries for nasal fractures included open wound to the nose, epistaxis, and associated facial fractures, most significantly malar/maxillary and orbi- tal fractures. About 10% of patients underwent some form of surgical intervention during the index hospitalization.
In our study, physical exam findings of open wounds to the nose and epistaxis were the strongest clinical indicators of a nasal fracture. Although an open wound of the nose was seen only in 9.5% of cases, its presence had greater than eight times increased odds for nasal fracture. Although the litera- ture describing the prevalence of comorbid findings in nasal fractures is scarce, this similar association was demonstrated in a retrospective review by Pérez-Guisado and Maclen- nan.[21] This study of cases in a hospital specializing in occupational injuries found that the presence of a nasal wound was clinically useful in the diagnosis of nasal fracture, with an increased odds of 2.35 times. These findings suggest that the force and trauma needed to create an open wound is strong enough to additionally cause a fracture.[22] Hence, patients who sustain open wounds of the nose should undergo careful examination and consideration of imaging.
Additionally, epistaxis has been documented in previous studies to be associated with nasal fractures.[21,23,24] Inter- estingly, the same single-hospital study by Pérez-Guisado and Maclennan found that patients with epistaxis had a 25 times increased risk of nasal fracture, with a sensitivity of 69% and specificity of 94%.[21] Though the study populations were different, our study demonstrated that epistaxis was associated with a greater than five times increased risk of nasal fracture. Future prospective studies using associated injuries such as open nasal wound and epistaxis should be conducted to determine if these clinical indicators can be utilized to determine which patients do and do not need imaging to evaluate for nasal fractures.
In our population, TBI was found in over half of all patients with nasal fractures. Previously, it has been thought that facial bones protect the brain from injury, playing a role in shock absorption and deceleration.[25] However, many studies have similarly found an association between facial fractures and TBI, and that facial fractures actually do not carry a protective role.[23,26,27,28] Davidoff et al reported the incidence of concomi- tant closed head injury (defined as a loss of consciousness and/or posttraumatic amnesia) among patients with nasal frac- tures was greater than 50%.[27] In a case–control study, Smith et al found that TBI was more prevalent in those with midface fractures than those without midface fractures (p = 0.041). Furthermore, more severe facial damage, as indicated by higher facial ISS, has been associated with worse initial neu- rological condition and higher rates of parenchymal damage, edema of brain, and cerebral hematoma.[6,29] The presence of a nasal fracture and other midface fractures may indicate that a higher force of impact was present. Therefore, although the presence of a nasal fracture alone may not warrant computed tomography imaging of the head, it certainly should be incor-porated in the decision making of the provider given the significant risk (>50%) of concomitant TBI that our study and others have demonstrated.
Blunt trauma was found to be significantly associated with nasal fractures and MVAs were the most common mechan- ism of injury in the NTDB. The most common cause of nasal fractures reported in previous studies varies depending on the center and study population and includes assaults, MVAs, sports injuries, or falls.[1,2,7,8,30] One possible reason for the discrepancy between our study and other studies is that the NTDB evaluates subjects categorized as trauma patients, which differs from other studies that may evaluate all patients who present to an institution, including simple falls and sports injuries which commonly are managed by emer-gency room physicians, or plastic surgeons and otolaryngol- ogists in the ambulatory setting.[8,11] We do note that in our study, of those with isolated nasal fractures, falls were the most common mechanism. However, in evaluating trauma patients with nasal fractures (both isolated and nonisolated), our results are similar to a retrospective multicenter study by Greathouse et al, which found that 61.7% of facial fracture patients evaluated by the trauma service sustained a nasal fracture from a MVA.[1] Their study saw a twofold higher prevalence of nasal fractures from MVAs compared with our NTDB study, likely due to their location at the crossroads of several major roadways. Comparatively, a meta-analysis by Hwang et al found that the most frequent cause of nasal fractures was assaults, followed by MVAs, sports injuries, and falls.[8] Although previous literature shows that the rate of facial fractures from MVA is decreasing due to new safety methods in cars, such as airbags and seatbelts, the protective effect is far less for nasal fractures.[1,28,31,32] Mouzakes et al suggested that airbags alone may even pose an increased risk of nasal fractures.[33] However, the majority of literature suggests that airbags and seat belts are paramount to injury prevention, especially the reduction of significant morbidity and mortality overall.[32,34,35]
Our surgical intervention rate in trauma patients with nasal fractures was 10.1%, with closed reduction accounting for approximately three-fourths of interventions. In isolated nasal fractures, the intervention rate was even lower at 6.4%, with 93.7% accounting for closed reductions. Our intervention rate in the NTDB was about half of previous studies in North America evaluating patients with nasal fractures.[1,36] When compared with a single-institution study evaluating only severely injured nasal fracture patients with ISS greater than 12, our intervention rates were substantially smaller than theirs (10.1 vs. 78.3%).[6] Greathouse et al evaluated all opera- tions performed across three Level I trauma centers and one independent surgical center for trauma patients with facial fractures and found that 25.2% of patients with nasal fractures received surgical intervention at a mean of 8.9 days following injury.[1] They also included operations after discharge, while the NTDB only includes operations on the index hospitaliza- tion. Since our average hospital LOS was 6.9 days (i.e., longer thanwould be expected for nasal fracture alone) and dueto the lack of follow-up data, our study did not capture all patients who eventually received treatment for their fracture at a later date.[1] However, previous studies of trauma patients have demonstrated poor rates of outpatient follow-up.[37,38] Stewart and Chen found that 66% of patients with isolated facial trauma attended their first follow-up appointment, but only 46% kept their recommended follow-up care.[39] Thus, given the low rate of follow-up, future multicenter studies on facial fractures that include follow-up data are needed to further evaluate whether our findings are representative of actual national rates of interventions in trauma subjects.
As the NTDB is a substantial aggregated database, it has several limitations that need to be considered. Emergency department visits, outpatient evaluations, and other non- trauma activations are not included in the database; there- fore, the NTDB does not capture all patients with nasal fractures. Furthermore, outcomes of the study such as ARDS, osteomyelitis, LOS, and mortality should be inter- preted specific to trauma patients, who often have conco- mitant injuries in addition to nasal fractures that are certainly more likely the reason for these significant com- plications than the nasal fracture itself. In addition, as the NTDB only describes the index hospitalization, information regarding follow-up, outpatient operative management, long-term complications, and long-term functional or cos- metic data are unavailable. Furthermore, important data fields are lacking such as the timing of any consultant services, specialty of consultant (i.e., plastic surgery, otolar- yngology, and/or oral maxillofacial surgery), whether the patient was deemed appropriate for surgery based on other concomitant injuries, and other physiologic information that may affect interventions and outcomes. However, our study has the advantage of a large multi-institutional, nationwide population that allows us to more accurately describe the epidemiology and risk factors associated with nasal fractures in patients who present as trauma activations at trauma centers across the country. This diversity allows the findings to be more generalizable, compared with single-institution studies, and provides valuable information applicable to multiple specialties involved in the care of facial trauma (i. e., emergency medicine, trauma surgery, plastic surgery, otolaryngology, and oral and maxillofacial surgery).
Conclusion
In this study, nasal fractures were found to have an incidence of 4.6% of traumas, with more than 90% occurring by blunt mechanism and over half suffering a concomitant TBI. Only ~10% of patients received any form of surgical intervention during their index stay, with the majority undergoing closed reduction. The strongest associated injury with increased odds for a nasal fracture was an open wound of the nose followed by epistaxis. Understanding the epidemiology, out- comes, and risk factors associated with nasal fractures may help clinicians better diagnose and treat this injury. Future prospective multi-institutional studies are needed to inves- tigate the follow-up rate of this population and long-term functional and cosmetic outcomes.
Acknowledgments
No funding sources were utilized for this research.
Conflicts of Interest
None.
References
- Greathouse, S.T.; Adkinson, J.M.; Garza, R., III; et al. Impact of injury mechanisms on patterns and management of facial fractures. J Craniofac Surg 2015, 26, 1529–1533. [Google Scholar] [CrossRef] [PubMed]
- Kelley, B.P.; Downey, C.R.; Stal, S. Evaluation and reduction of nasal trauma. Semin Plast Surg 2010, 24, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Bartkiw, T.P.; Pynn, B.R.; Brown, D.H. Diagnosis and management of nasal fractures. Int J Trauma Nurs 1995, 1, 11–18. [Google Scholar] [CrossRef]
- Reilly, M.J.; Davison, S.P. Open vs closed approach to the nasal pyramid for fracture reduction. Arch Facial Plast Surg 2007, 9, 82–86. [Google Scholar] [CrossRef][Green Version]
- Rohrich, R.J.; Adams, W.P., Jr. Nasal fracture management: minimizing secondary nasal deformities. Plast Reconstr Surg 2000, 106, 266–273. [Google Scholar] [CrossRef]
- Alvi, A.; Doherty, T.; Lewen, G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope 2003, 113, 102–106. [Google Scholar] [CrossRef]
- Erdmann, D.; Follmar, K.E.; Debruijn, M.; et al. A retrospective analysis of facial fracture etiologies. Ann Plast Surg 2008, 60, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.; Ki, S.J.; Ko, S.H. Etiology of nasal bone fractures. J Craniofac Surg 2017, 28, 785–788. [Google Scholar] [CrossRef]
- Hwang, K.; Yeom, S.H.; Hwang, S.H. Complications of nasal bone fractures. J Craniofac Surg 2017, 28, 803–805. [Google Scholar] [CrossRef]
- Kraft, A.; Abermann, E.; Stigler, R.; et al. Craniomaxillofacial trauma: synopsis of 14,654 cases with 35,129 injuries in 15 years. Cranio- maxillofac Trauma Reconstr 2012, 5, 41–50. [Google Scholar]
- Ridder, G.J.; Boedeker, C.C.; Fradis, M.; Schipper, J. Technique and timing for closed reduction of isolated nasal fractures: a retro- spective study. Ear Nose Throat J 2002, 81, 49–54. [Google Scholar]
- Chan, K.H.; Gao, D.; Bronsert, M.; Chevallier, K.M.; Perkins, J.N. Pediatric facial fractures: demographic determinants influencing clinical outcomes. Laryngoscope 2016, 126, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Shere, J.L.; Boole, J.R.; Holtel, M.R.; Amoroso, P.J. An analysis of 3599 midfacial and 1141 orbital blowout fractures among 4426 United States Army Soldiers, 1980-2000. Otolaryngol Head Neck Surg 2004, 130, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Imahara, S.D.; Hopper, R.A.; Wang, J.; Rivara, F.P.; Klein, M.B. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg 2008, 207, 710–716. [Google Scholar] [PubMed]
- Allred, L.J.; Crantford, J.C.; Reynolds, M.F.; David, L.R. Analysis of pedia- tric maxillofacial fractures requiring operative treatment: char- acteristics, management, and outcomes. J Craniofac Surg 2015, 26, 2368–2374. [Google Scholar]
- Chou, C.; Chen, C.W.; Wu, Y.C.; Chen, K.K.; Lee, S.S. Refinement treatment of nasal bone fracture: a 6-year study of 329 patients. Asian J Surg 2015, 38, 191–198. [Google Scholar]
- Zelken, J.A.; Khalifian, S.; Mundinger, G.S.; et al. Defining predictable patterns of craniomaxillofacial injury in the elderly: analysis of 1,047 patients. J Oral Maxillofac Surg 2014, 72, 352–361. [Google Scholar] [CrossRef]
- Chang, M.C. National Trauma Data Bank 2016 Annual Report; American College of Surgeons, 2016. [Google Scholar]
- Baker, S.P.; O’Neill, B.; Haddon, W., Jr.; Long, W.B. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974, 14, 187–196. [Google Scholar] [CrossRef]
- Gennarelli, T.A.; Wodzin, E. AIS 2005: a contemporary injury scale. Injury 2006, 37, 1083–1091. [Google Scholar]
- Pérez-Guisado, J.; Maclennan, P. Clinical evaluation of the nose: a cheap and effective tool for the nasal fracture diagnosis. Eplasty 2012, 12, e3. [Google Scholar]
- Cormier, J.; Manoogian, S.; Bisplinghoff, J.; et al. The tolerance of the nasal bone to blunt impact. Ann Adv Automot Med 2010, 54, 3–14. [Google Scholar] [PubMed]
- Smith, H.L.; Chrischilles, E.; Janus, T.J.; et al. Clinical indicators of midface fracture in patients with trauma. Dent Traumatol 2013, 29, 313–318. [Google Scholar] [PubMed]
- Daniel, M.; Raghavan, U. Relation between epistaxis, external nasal deformity, and septal deviation following nasal trauma. Emerg Med J 2005, 22, 778–779. [Google Scholar]
- Lee, K.F.; Wagner, L.K.; Lee, Y.E.; Suh, J.H.; Lee, S.R. The impact-absorbing effects of facial fractures in closed-head injuries. An analysis of 210 patients. J Neurosurg 1987, 66, 542–547. [Google Scholar] [PubMed]
- Keenan, H.T.; Brundage, S.I.; Thompson, D.C.; Maier, R.V.; Rivara, F.P. Does the face protect the brain? A case-control study of traumatic brain injury and facial fractures. Arch Surg 1999, 134, 14–17. [Google Scholar]
- Davidoff, G.; Jakubowski, M.; Thomas, D.; Alpert, M. The spectrum of closed-head injuries in facial trauma victims: incidence and impact. Ann Emerg Med 1988, 17, 6–9. [Google Scholar]
- Hitosugi, M.; Mizuno, K.; Nagai, T.; Tokudome, S. Analysis of max- illofacial injuries of vehicle passengers involved in frontal colli- sions. J Oral Maxillofac Surg 2011, 69, 1146–1151. [Google Scholar] [PubMed]
- You, N.; Choi, M.S.; Roh, T.H.; Jeong, D.; Kim, S.H. Severe facial fracture is related to severe traumatic brain injury. World Neurosurg 2018, 111, e47–e52. [Google Scholar]
- Atisha, D.M.; Burr Tv Allori, A.C.; Puscas, L.; Erdmann, D.; Marcus, J.R. Facial fractures in the aging population. Plast Reconstr Surg 2016, 137, 587–593. [Google Scholar]
- Hyman, D.A.; Saha, S.; Nayar, H.S.; Doyle, J.F.; Agarwal, S.K.; Chaiet, S.R. Patterns of facial fractures and protective device use in motor vehicle collisions from 2007 to 2012. JAMA Facial Plast Surg 2016, 18, 455–461. [Google Scholar]
- McMullin, B.T.; Rhee, J.S.; Pintar, F.A.; Szabo, A.; Yoganandan, N. Facial fractures in motor vehicle collisions: epidemiological trends and risk factors. Arch Facial Plast Surg 2009, 11, 165–170. [Google Scholar]
- Mouzakes, J.; Koltai, P.J.; Kuhar, S.; Bernstein, D.S.; Wing, P.; Salsberg, E. The impact of airbags and seat belts on the incidence and severity of maxillofacial injuries in automobile accidents in New York State. Arch Otolaryngol Head Neck Surg 2001, 127, 1189–1193. [Google Scholar]
- Hwang, K.; Kim, J.H. Effect of restraining devices on facial fractures in motor vehicle collisions. J Craniofac Surg 2015, 26, e525–e527. [Google Scholar]
- Murphy, R.X., Jr.; Birmingham, K.L.; Okunski, W.J.; Wasser, T. The influence of airbag and restraining devices on the patterns of facial trauma in motor vehicle collisions. Plast Reconstr Surg 2000, 105, 516–520. [Google Scholar] [PubMed]
- Lanigan, A.; Lospinoso, J.; Bowe, S.N.; Laury, A.M. The nasal fracture algorithm: a case for protocol-driven management to optimize care and resident work hours. Otolaryngol Head Neck Surg 2017, 156, 1041–1043. [Google Scholar] [PubMed]
- Hansen, L.; Shaheen, A.; Crandall, M. Outpatient follow-up after traumatic injury: challenges and opportunities. J Emerg Trauma Shock 2014, 7, 256–260. [Google Scholar] [PubMed]
- Stone, M.E., Jr.; Marsh, J.; Cucuzzo, J.; Reddy, S.H.; Teperman, S.; Kaban, J.M. Factors associated with trauma clinic follow-up compliance after discharge: experience at an urban Level I trauma center. J Trauma Acute Care Surg 2014, 76, 185–190. [Google Scholar]
- Stewart, M.G.; Chen, A.Y. Factors predictive of poor compliance with follow-up care after facial trauma: a prospective study. Otolaryngol Head Neck Surg 1997, 117, 72–75. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2019 by the author. The Author(s) 2019.