The condylar process is one of the most commonly injured regions of the mandible, accounting for 20 to 35% of all mandible fractures.[
1,
2,
3] The management of adult condylar injuries remains one of the most controversial topics in facial trauma. While satisfactory outcomes can be achieved in the majority of patients with closed treatment, which fractures may benefit from open treatment remains up for debate.[
4,
5] Multiple factors should be considered in making the decision to select open treatment; these include the level of fracture, fracture displacement, condylar dislocation, associated inju- ries to the mandible and midface, state of the patient’s dentition, confidence of the surgeon to perform open treat- ment, and adaptability of the masticatory system. Another frequently described consideration is the presence of bilat- eral condylar fractures, which was traditionally considered a relative indication for open treatment.[
6,
7]
Bilateral condylar fractures account for 24 to 33% of all mandibular condylar fractures and is usually the result of a high-energy impact to the anterior mandible.[
8,
9] Shortening of bilateral rami frequently leads to an anterior open bite, and comparedwithunilateralinjuries, a higher rate of malocclusion is associated with bilateral condylar process fractures.[
10] Furthermore, bilateral condylar injuries lead to a disruption of the normal morphology of both temporomandibular joints (TMJ), and significant neuromuscular adaptation would be required to restore satisfactory masticatory function and dental occlusion.[
11,
12] Because of thesefactors, several authors have advocated that open treatment of bilateral condylar fractures may lead to more predictable outcomes.[
13,
14,
15,
16,
17] In contrast, other studies have shown that closed treatment can lead to successful reestablishment of occlusion and comparable maximal mouth opening (MMO) to open treatment.[
8,
18,
19]
Contributing to these conflicting results is the fact that bilateral condylar fractures encompass a group of heteroge- neous injury patterns. Therefore, attempts to answer the question of which bilateral condylar injuries should be man- aged open or closed must account for the contribution of the patient’s specific injury pattern to the functional outcome. The level of injury is an important consideration in selecting the treatment option for condylar fractures,[
20,
21] and few studies have compared the outcomes of different types of bilateral condylar fractures.[
15] The purpose of this study was to compare the functional outcomes of patients with different types of bilateral condylar process fractures after surgical treatment. Our hypothesis was that the injury pattern would be an independent predictor of functional outcomes.
Materials and Methods
Study design: This was a retrospective cohort study of con- secutive patients who presented with bilateral mandibular condylar process fractures to a level-1 trauma center over a 15-year period. Patients with bilateral mandibular condylar fractures were identified from the institutional trauma registry. Maxillofacial CT imaging of all identified patients were then reviewed to confirm the presence of mandibular condylar fracture and record associated facial injuries. All patients with confirmed bilateral fractures of the mandibu- lar condylar processes and who have at least 1 month of follow-up were eligible for inclusion. Patients who were younger than 18 years, passed away during their admission, had incomplete medical records, or were not managed by one of the facial trauma surgical services were excluded. This study was approved by the institutional review board.
Predictor variables: Predictor variables were factors potentially associated with complication rates and were classified as demographic, injury-related, and treatment variables. Demographic factors included age (years), sex (male or female), and race (Caucasian, black, or other). Injury-related variables included mechanism, admission Glasgow coma scale (GCS), length of hospital stay, and injury severity score.[
22] Anatomic level of condylar fracture was defined according to Lindahl’s classification.[
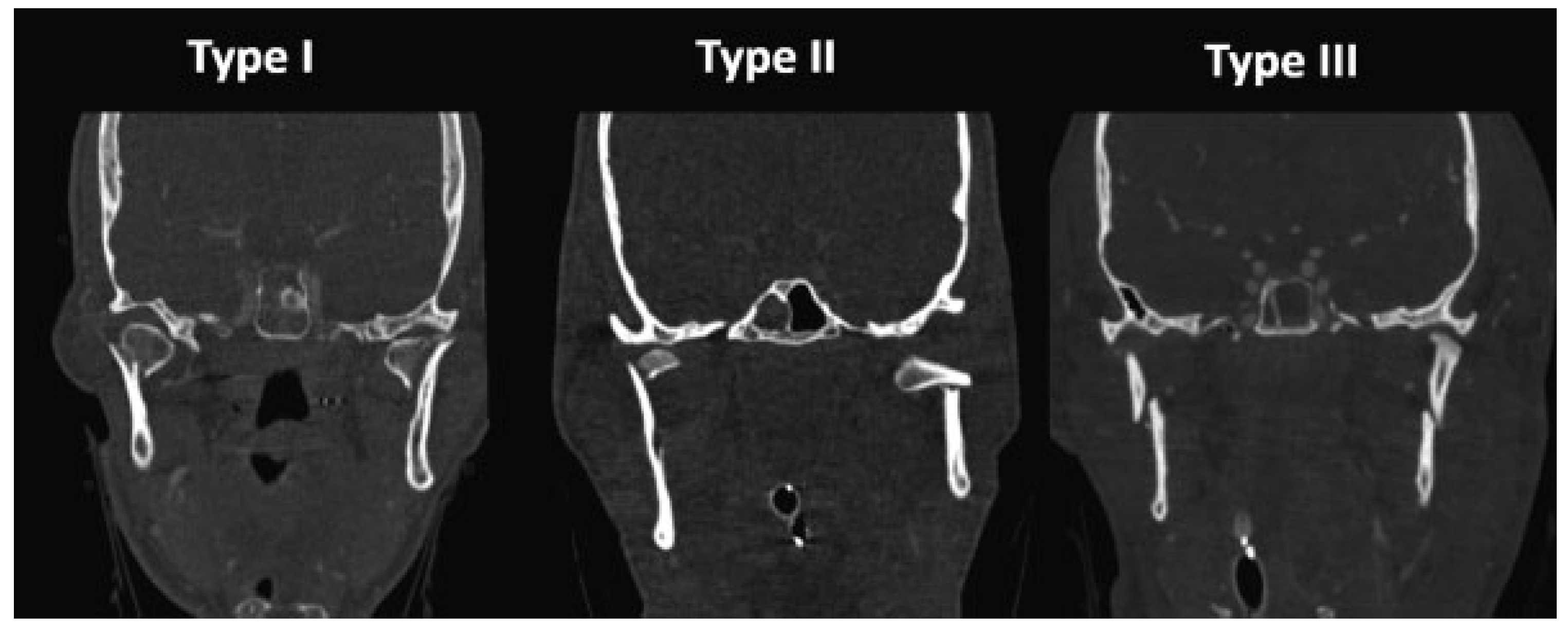
23] Bilateral con- dylar fractures were classified into three types according to Chen’s classification system, with type I defined as bilateral condylar head (intracapsular) fractures, type II as one condylar and one subcondylar fracture, and type III as bilateral subcondylar fractures (
Figure 1).[
15] In addition to condylar fracture characteristics, facial fracture patterns including the presence of noncondylar mandible fractures, concomitant midface fractures, and midface and mandibular fractures that required operative intervention were considered as well. The facial injury severity score (FISS) was calculated to account for the overall severity of facial trauma.[
24]
The choice of treatment was surgeon driven. Closed management of the condylar injuries consisted of intermaxillary fixation (IMF) usually with arch bars, with an average time in IMF of 14.7 ± 7.4 days (range: 0–32 days) and a median time of 14 days. Patients were placed into guiding elastics directly at the time of surgery or transitioned to guiding elastics after release of wire IMF. The mean duration of guiding elastic use was 23.8 ± 9.1 days (range: 0–47 days); the median duration was 21 days. Patients are then followed up closely in the clinic to assess their dental occlusion. Open treatment was performed through either a preauricular or retromandibular approach, and rigid fixation was achieved with miniplates. Some patients were treated with a combi- nation of open treatment for one fracture and closed treat- ment for the condylar injury on the contralateral side.
Outcome variables: The primary outcome variables were functional complications including trismus (defined as mouth opening <35 mm), malocclusion, TMJ ankylosis, and the need for a subsequent operation. Operative reports and clinic notes were reviewed for all patients in the sample to ascertain the method of management and to calculate the rate of complications.
Statistical methods: De-identified data were entered into a statistical database (SPSS, v.24.0, IBM Inc., Armonk, NY) over the course of the study. Descriptive statistics were computed for the study sample. Bivariate statistics were used to identify associations between the predictor variables and complications. Bivariate associations with p ≤ 0.15 and biologically relevant measures (age and sex) were included in a multiple logistic regression model, which was used to compute asso- ciations between the type of condylar injury and complica- tions, adjusting for the simultaneous effects of other measures. For all analyses, a p-value ≤ 0.05 was considered statistically significant.
Results
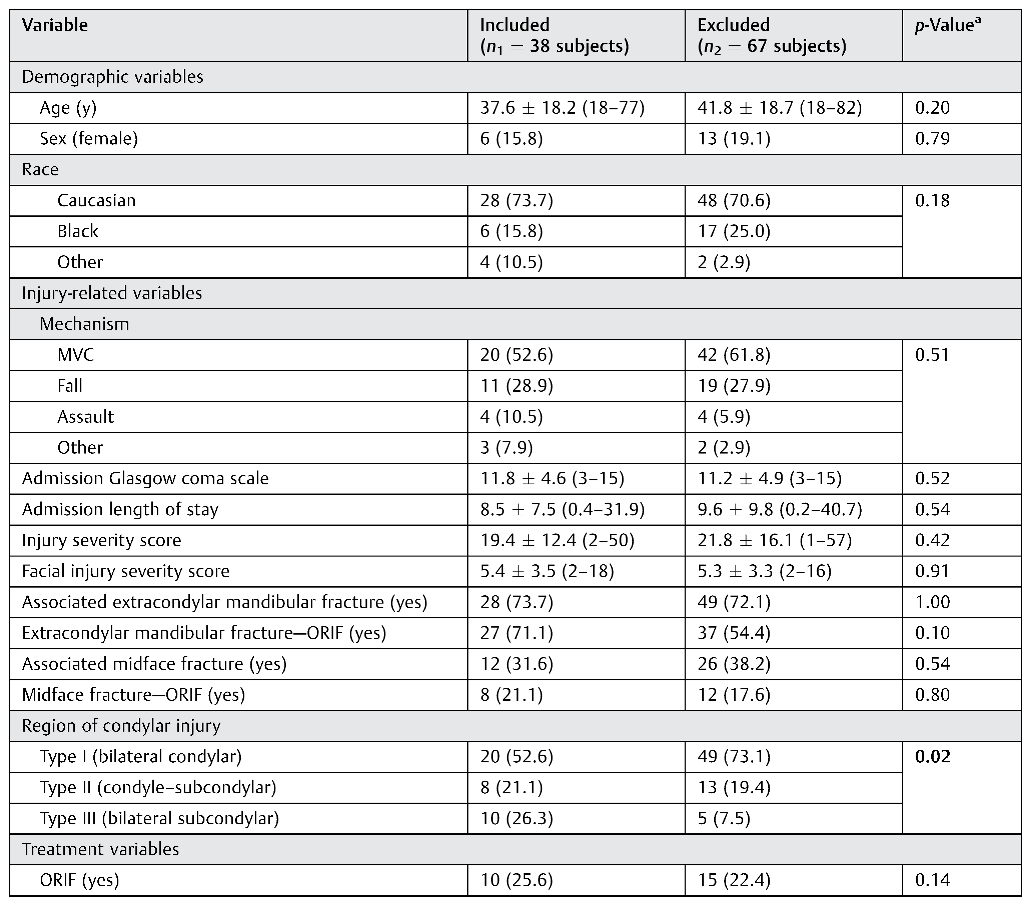
Over thestudy period, we identified 105 subjects with bilateral condylar injuries. The sample’s mean age was 40.5 ± 18.5 years (range: 18–82 years), 18.1% were female, and 72.4% were Caucasian. Most injuries were the result of motor vehicle collisions (59.0%) and mechanical falls (28.6%). The mean GCS on admission was 11.4 ± 4.8 (range: 3–15). The mean hospital length of stay was 9.2 ± 9.0 days (range: 0.2–40.0). The mean ISS was 20.9 ± 14.8 (range: 1–75), and the mean FISS was 3.9 ± 2.9 (range: 2–18). 72.6% of injuries involved another noncondylar fracture of the mandible; nearly all (81.8%) of these additional mandibular fractures were managed with open reduction and internal fixation (ORIF). Approximately 35.9% of cases involved an associated midface fracture; of these, 52.6% were managed operatively. Sixty-nine subjects (52.6%) had type I (bilateral condylar) injuries; twenty-one (21.1%) had type II (condylar–subcondylar) injuries; and fifteen (26.3%) had type III (bilateral subcondylar) injuries. Twenty-five subjects (23.8%) received ORIF for their condylar injuries. Descriptive statistics are summarized in
Table 1.
Patients with incomplete data or did not have at least 1 month of follow-up were excluded. Thirty-eight patients (36.2%) met inclusion criteria and were included for further analysis. Comparisons of the included sample versus the excluded sample are summarized in
Table 2. The two groups were similar in most demographic, injury-related, and treatment variables except for the type of fractures. The excluded group had a significantly higher percentage of type I injuries (bilateral condylar) and a smaller percentage of type III injuries (bilateral subcondylar) compared with the included sample.
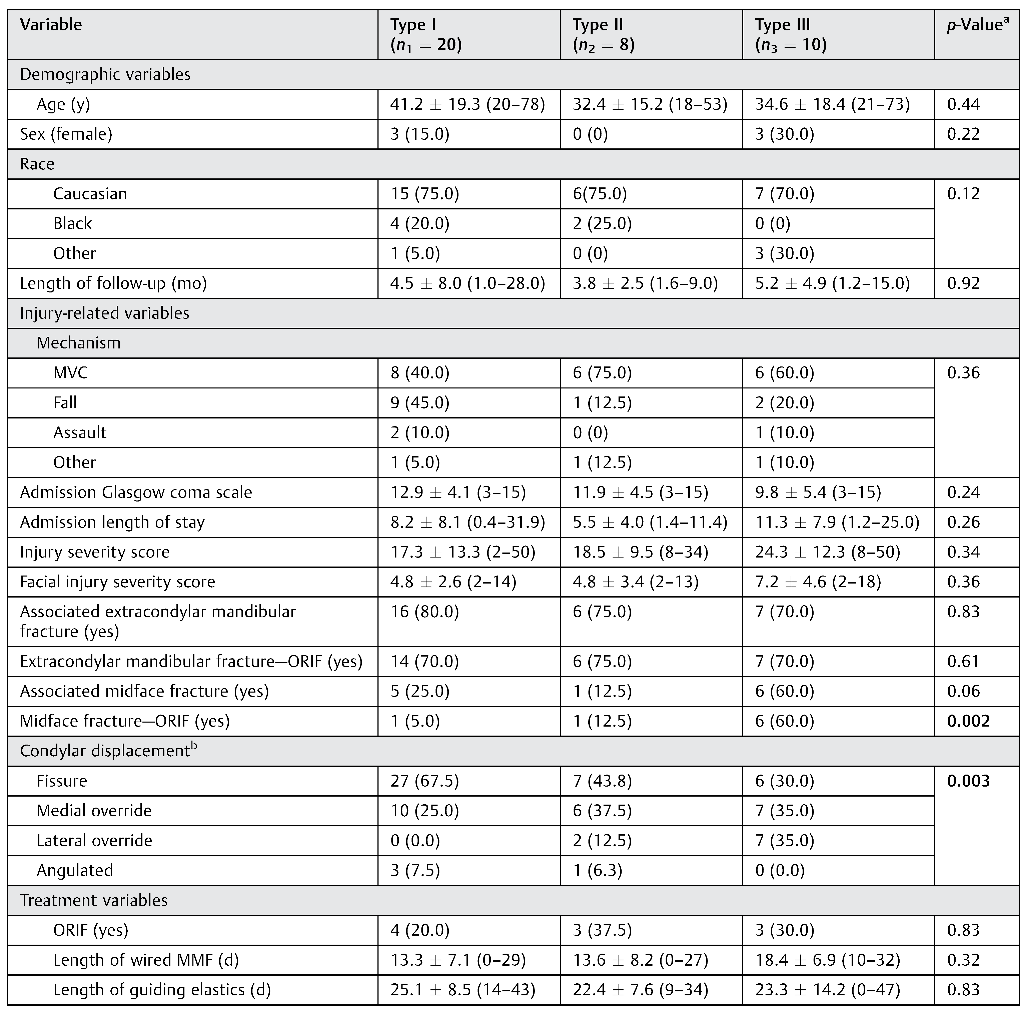
The average length of follow-up for the included subjects was 4.5 ± 6.3 (range: 1.0–28.0) months. The included sub- jects were divided based on the three types of injury patterns, and
Table 3 summarizes the comparisons of the demographic, injury-related, and treatment variables among them. The demographic, injury-related, and treatment char- acteristics were similar among subjects with the three types of injury patterns with few exceptions. The distribution of injury patterns by condylar displacement was significantly different across the three subgroups, with medial and lateral override more common in type II and type III injuries (
p = 0.003). Additionally, type III injuries were more likely to be associated with a midface fracture that required operative treatment (60%) compared with type I (5.0%) and type II (12.5%) injuries (
p = 0.002).
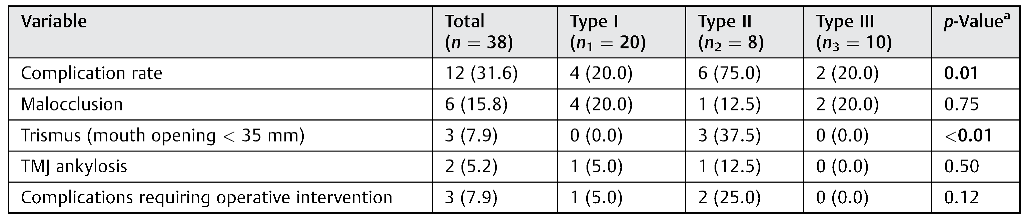
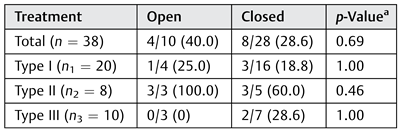
Comparison of the functional outcomes among the three injury types is summarized in
Table 4. The most common complications were malocclusion and trismus, which occurred in six (15.8%) and three (7.9%) subjects, respectively. Two subjects developed TMJ ankyloses, and three required an additional operative intervention (e.g., TMJ arthroplasty or orthognathic surgery). Twelve (31.6%) subjects had at least one of the abovementioned functional complications. When the three injury types were compared regardless of the treatment method, type II injury wasassociated with a significantly higher rate of adverse outcomes (75%) compared with type I (20.0%) and type III (20.0%) injuries (
p = 0.01). The incidence of trismus was significantly higher with type II injuries (37.5%) compared with type I (0%) and type III (0%) injuries (
p < 0.01). Bivariate associations between demographic, injury-related, and treatment variables with complication rates were calculated. The length of follow-up was the only variable found to be associated with overall complication rate (
p = 0.01). The presence of extracondylar mandibular fractures was not significantly associated with higher complication rates (
p = 0.90). Condylar dis- placement was not independently associated with overall or individual complications (
p > 0.09). Similarly, the length of wire IMF (
p > 0.19) and thelength of guiding elastics (
p > 0.67) were also not associated with overall or individual complications.
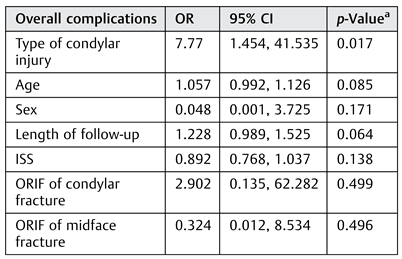
A multiple logistic regression model for complications is summarized in
Table 5. After adjusting for the effects of age, sex, length of follow-up, injury severity score, ORIF of concomitant midface injury, and open treatment for con- dylar injury, the pattern of bilateral condylar injury was an independent predictor of complications (odds ratio: 7.77, 95% confidence interval: 1.45–41.53,
p = 0.02). Patients with type II injuries had the greatest odds for a complication, followed by type III injuries. This model explained 66% of the variability in complication rates (
R2 = 0.66).
Table 6 out- lines the overall complication rates of open versus closed treatment for the entire cohort and each type of bilateral condylar injuries. There was no significant difference in the complication rates between those treated open or closed.
Case 1: Closed Treatment of Type I Injury
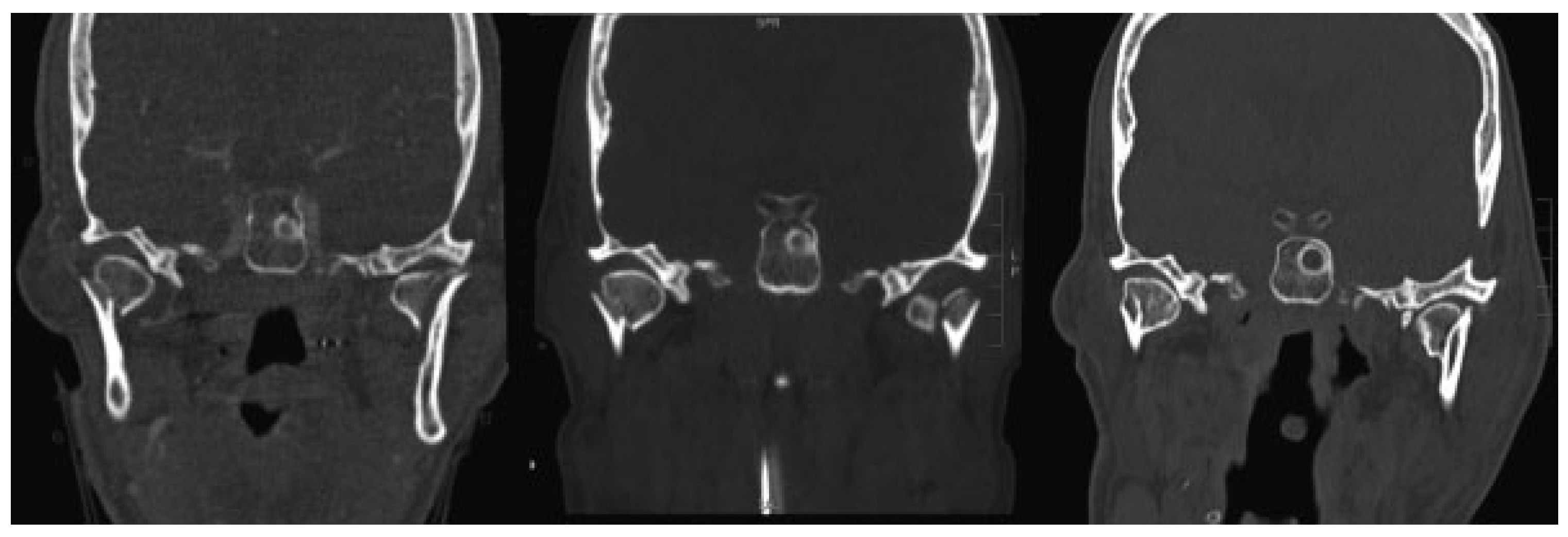
A 52-year-old man fell from a ladder and sustained bilateral condylar head fractures (type I) and a left parasymphyseal fracture (
Figure 2). His anterior mandibular fracture was treated with rigid fixation with an inferior border plate and a tension band. Closed treatment of the condylar injuries was performed with arch bars and guiding elastic to allow for early range of motion. By 6 weeks after the injury, the patient had achieved a normal occlusion and a MMO of 40 mm. Long- term follow-up imaging at 2 years after injury demonstrated malunion of the condylar fractures without any appreciable functional consequences.
Case 2: Unilateral ORIF of Type II Injury
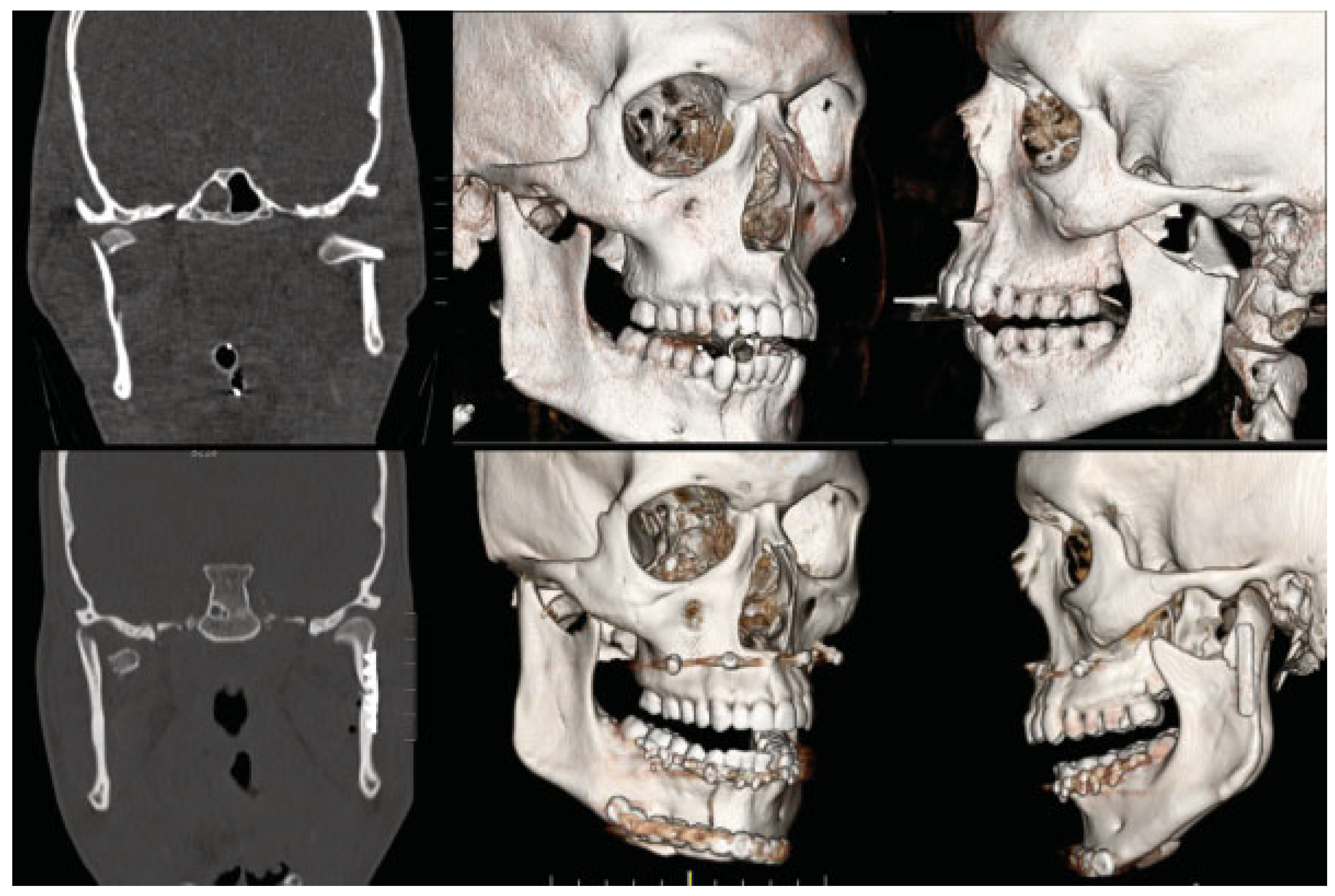
A 19-year-old man was involved in an ATV crash and pre- sented with left subcondylar, right condylar head (type II), and right parasymphyseal fractures (
Figure 3). He underwent rigid fixation of the parasymphyseal fracture. The left subcondylar fracture was displaced medially and dislocated from the glenoid fossa; open reduction of this fracture was performed through a retromandibular approach and fixation was achieved with a 2.0-mm plate. The right condylar head injury was intracapsular and was managed with closed treatment. The patient was placed into IMF with guiding elastics immediately postsurgery. On subsequent follow-up, active and passive mouth opening exercises were initiated. At the 8-week follow-up, his MMO remained limited at 23 mm. Continued physical therapy was recommended, but the patient was then lost to follow-up.
Case 3: Bilateral ORIF of Type III Injury
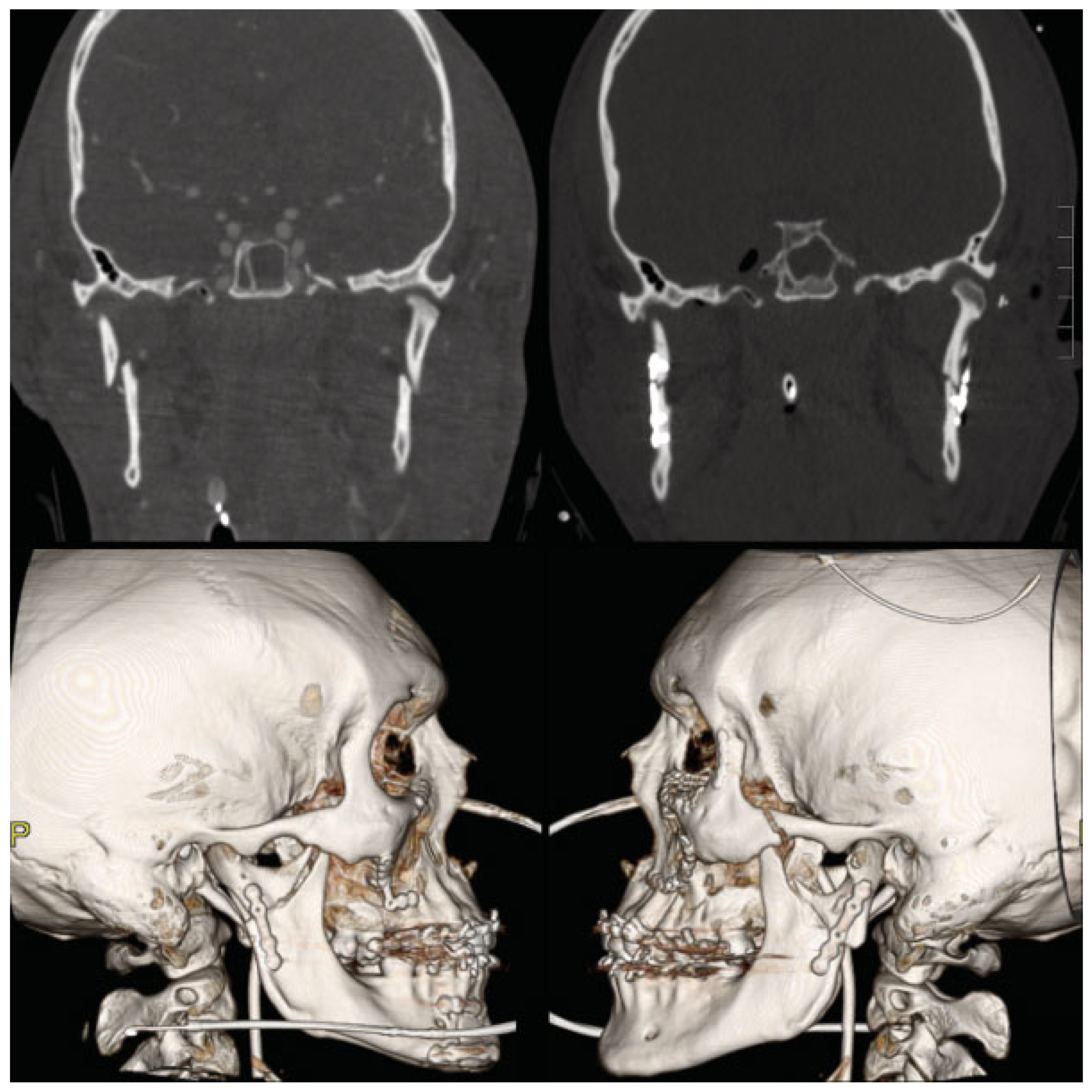
A 25-year-old man was in a motor vehicle crash and was admitted for multiple facial fractures including left zygoma- ticomaxillarycomplex, left orbital floor, bilateral Le Fort I, right parasymphyseal, and bilateral subcondylar (type III) fractures (
Figure 4). He underwent ORIF of his extensive midface and mandible fractures. Open treatment of both subcondylar fractures was performed through retromandibular approaches to reestablish occlusion and posterior facial height. The patient was kept in wired IMF for 10 days and then transitioned to guiding elastics. He had pain in bilateral TMJ areas which eventually resolved at approximately 6 weeks after the injury. At that time, the arch bars were removed and patient had achieved MMO of 42 mm with normal occlusion.
Discussion
The management of mandibular condylar process fractures remains highly controversial. Most studies on this topic have included a heterogeneous group of subjects with both uni- lateral and bilateral condylar injuries, with few reports focusing exclusively on bilateral injuries.[
25] While well- defined absolute indications for open reduction of unilateral condylar fractures have been proposed,[
7] there are no abso- lute indications for open treatment of bilateral fractures. As such, there is a paucity of evidence to guide treatment decisions. Among patients with bilateral injuries, the frac- ture pattern can potentially impact the ultimate functional outcome. As such, the purpose of this study was to identify which type of bilateral condylar injuries is associated with worse functional outcomes among a cohort of patients who were managed with either closed or open treatment based on surgeon- and patient-specific characteristics.
The results of this study confirmed our hypothesis that the fracture pattern is an independent predictor of functional outcomes irrespective of the treatment method performed. Type II bilateral condylar injury was found to be associated with the worse functional outcomes compared with the other two injury types. Type II injuries represent asymmetric bilateral injuries with one subcondylar fracture and a con- tralateral intracapsular injury.
Asymmetric injuries present a dilemma in treatment selection for the provider as a high condylar fracture may benefit from early range of motion to prevent ankylosis, whereas a low displaced subcondylar fractures may have better functional outcomes after ORIF.[
25,
26] In our patient cohort, three subjects with asymmetric condylar fractures received ORIF of the subcondylar fracture and closed treat- ment of the contralateral high condylar injury. Two out of these three patients developed trismus and one developed persistent malocclusion. This is admittedly a small sample size, but the high complication rate suggests that surgical fixation of one of two condylar injuries may result in poor functional outcomes in patients with asymmetric injuries.
Multiple studies have indicated that neuromuscular adapta- tions of the masticatory system play an important role in achieving satisfactory outcomes after condylar fractures.[
18,
27] As such, the higher rate of functional complications may be related to an inability of the masticatory system to compensate adequately for asymmetric injuries. It is possible that asym- metric intracapsular involvement and asymmetric involvement at the level of the lateral pterygoid muscle insertion pose a more difficult problem in terms of neuromuscular adaptations during the rehabilitation period. While this is a plausible pathophysiologic explanation for the findings herein, we cannot make definitive statements regarding this process with the available data. The decision to perform closed treatment, unilateral ORIF, or bilateral ORIF for type II bilateral condylar injuries is a topic that warrants additional inquiry.
Our finding that type II injuries were associated with poor functional outcome is in contrast to a previous study per- formed by Chen et al, where the authors identified that type I injuries were associated with the worst functional outcome after ORIF.[
15] All subjects included in this previous study were treated with ORIF, whereas only 25.6% of subjects in our cohort were treated open. This difference in management likely contributed to the discrepancy in the findings of the two studies. Bone resorption and TMJ ankylosis are worrisome concerns after open treatment of intracapsular condylar fractures,[
28,
29] and in the study by Chen et al, 24.2% of subjects with type I injuries treated with ORIF developed trismus as defined by MMO less than 35 mm.[
15] Newman previously reported a high rate of trismus with closed treatment of bilateral condylar injuries as well; however, in that study, subjects who received closed treatment were kept in wire IMF for an average of 37 days.[
16] In our cohort of subjects with type I bilateral condylar fractures, the mean duration of wire IMF was 13.3 ± 7.1 days with a mean duration of guiding elastics of 25.1 ± 8.5 days. All 20 subjects achieved MMO greater than 35 mm at the last follow-up. Our preferred approach for type I injuries is to perform closed management with early range of motion exercises and aggressive physiotherapy to minimize risk of trismus in lieu of anatomic reduction. The data herein suggest that a short period of wire IMF (2 weeks) followed by 2 to 3 weeks of guiding elastics may be appropriate for post- operative management for type I injuries, allowing adequate union without consequential trismus.
Type III injury was found to be most likely to be associated with severe midface injuries and may represent overall higher energy injuries. All patients achieved adequate MMO, but two patients did develop malocclusion, both of who had been managed with closed treatment. The low rate of trismus may be explained by the fact that these fractures are not intra-articular. However, significant fracture displacement can be associated with a loss of posterior height and subsequent malocclusion. In general, the larger condylar fragment in subcondylar injuries facilitates surgical access and internal fixation.[
21] Thus, patients with significant bilateral condylar dislocation from the glenoid fossa or fracture displacement may benefit from open treatment of these condylar injuries to restore posterior facial height and adequate occlusion. However, surgical complications associated with open treatment, including temporary and permanent facial nerve palsy, must be taken into consideration.[
30,
31]
An important limitation of our study is the small sample size, which does not allow us to draw conclusions on the comparative outcomes of open versus closed treatment in each subtype of bilateral condylar fractures. However, the primary predictor variable, fracture type, was statistically significant (
p = 0.02) in the regression model, despite the relatively small sample size (i.e., low likelihood of a type I statistical error). This suggests that the effect for that fracture type was large enough to be detected in a small sample. In this regard, the results of the regression analysis may be most reliable when stating that the complication incidence is highest for type II injuries compared to type I injuries. A second limitation of our study is related to the use of retrospective data in a population with inconsistent follow- up patterns that predisposed the study to selection bias. Studies on the trauma patient population are often limited by poor follow-up;[
32] our study was no different with only 36.2% of our cohort having at least 1 month of follow-up. Interestingly, there were more type I injuries in the group that was lost to follow-up, and this may reflect the relatively lower injury severity and overall better outcomes associated with type I injuries. While the mean follow-up was less than 6 months within this cohort, many, if not all, of the complications assessed would be present within the first few months following removal of IMF and would have been captured within our dataset. However, the short length of follow-up does limit the ability to appreciate the long-term functional sequela of bilateral condylar injuries.
Conclusion
The results of this study suggest that type II bilateral condylar fractures (condylar–subcondylar) may be associated with an increased risk of adverse functional outcomes compared with bilateral condylar and bilateral subcondylar fractures. Future studies comparing the outcomes of closed treatment, unilateral ORIF, and bilateral ORIF of type II bilateral condylar fractures are necessary to guide the treatment for these challenging injuries.
Financial Disclosures
Dr. Dorafshar receives indirect research support and is entitled to royalties from KLS Martin. Dr. Dorafshar also receives indirect research support from DePuy Synthes. Dr. Susarla owns stock in Polarity TE, Inc. The remaining authors have no financial interests to disclose.