Fractures of the mandibular condyle are common and account for 25 to 35% of all mandibular fractures. There are various guidelines regarding the management of condylar fractures of the mandible by open or closed treatment, but there is still a continuing debate over how to best manage this type of fractures.[
1,
2] Condylar fractures are different from other fractures of mandible, as infection and nonunion are rare.[
3] However, functional derangements such as malocclusion, facial asymmetry, chronic pain, and limited mouth opening are of main concern. Various treatment options for their management are available, such as[
4] functional therapy without a period of maxillomandibular fixation (MMF), a period of MMF followed by functional therapy, and open reduction and internal fixation with or without MMF. In an attempt to provide a universally acceptable guideline, Bhagol et al[
5] provided a classification system for subcondylar fracture. They advocated open reduction and internal fixation for severely displaced fracture. There are other authors who also favor open reduction and internal fixation for such fractures.[
6,
7,
8,
9,
10] However, Ellis[
3] had different opinion regarding this. According to him, all the unilateral condylar fractures, even displaced fractures, can be managed by closed treatment. However, anatomical reduction is considered as a prerequisite for fracture management. Open reduction and internal fixation of condylar fracture contains surgical risks, such as facial nerve paresis, parotid fistula, and facial scar and a lot of surgical expertise is required for the open reduction. So, if displaced condylar fractures can be managed successfully by closed treatment, it will be beneficial for both the patients and surgeons.
Thus, in the light of the aforementioned situation and considering all treatment modalities related to condylar fracture, a prospective study was performed to compare evaluation of closed and open treatments in the management of unilateral displaced mandibular subcondylar fractures. The findings of this study, to some extent, would be beneficial in guiding surgeons to choose between surgical and nonsurgical treatment for displaced subcondylar fractures with more than 10 mm ramal height shortening and more than 20 degrees of displacement of condyle. So, the aim of the study is to evaluate the closed and open treatment in the management of unilateral displaced mandibular subcondylar fractures.
Materials and Methods
A randomized study was performed to compare closed and open treatment options in the management of unilateral displaced mandibular subcondylar fractures. A total of 20 patients who reported to the Department of Oral and Maxillofacial Surgery, Pt. B.D. Sharma University of Health Sciences, Rohtak, India, with unilateral displaced subcondylar fractures were included in the study. They were informed of the need for 6-month follow-up. Patients were thoroughly informed, explaining the possible advantages and disadvantages of the open and closed treatment options. This was a double-blinded, parallel group randomized controlled trial with balanced/equal randomization. Outcome assessors and data analysts were kept blinded to the allocation.
Inclusion Criteria
Patients older than 18 years.
Unilateral subcondylar fracture as classified by Lindahl and Hollender[
11] and illustrated by Ellis et al.[
12]
The patient must have a good complement of teeth, especially posterior teeth.
Patient should consent to participate in the study.
Degree of displacement of the condylar fragments in the coronal plane greater than 20 degrees.
Shortening of the height of the ascending ramus of the mandible more than 10 mm.
Additional fractures of themandible were treated with open or closed reduction independent of randomization.
Exclusion Criteria
Previous history of temporomandibular joint dysfunction.
Severe pretraumatic dysgnathia.
Mandibular condylar head or neck fractures. (Condylar neck is the region where the caudal portion of the joint capsule attaches. It is the thin constricted area immediately below the condylar head.)
Methodology
After approval from the institutional review board, patients with unilateral displaced subcondylar fractures were included in the study. Patients were selected based on the inclusion and exclusion criteria. Patients were explained about the surgical procedure. Informed consent was taken from all patients. All examinations and calculations were done by a single calibrated surgeon.
Preoperatively
Detailed case history was recorded and primary examination pertaining to trauma was done and preoperative assessment included evaluation of the following parameters: age and gender of the patient, etiology of fracture, site of fracture, degree of fracture displacement, occlusion, mouth opening, and shortening of ramus height.
Treatment
Closed treatment consisted of MMF with elastics for a period of 7 to 42 days (mean: 21 days). Postoperative instructions regarding mouth opening exercises and physiotherapy were given to all the patients.
In open treatment, standardized surgical treatment options were used by one surgeon of consultant grade using retromandibular approach for surgical access. The fractures were fixed with 2-mm miniplates. MMFs with light elastics were kept for 3 to 5 days postoperatively. Postoperative instructions regarding mouth opening exercises and physiotherapy were given to all the patients.
Postoperatively
Follow-up examinations were performed at 1, 3, and 6 months. Results of the clinical and radiological examinations were recorded on a specific form. Assessment of the following clinical parameters was done:
Range of motion of the injured joint together with the contralateral joint as given by the mouth opening (maximum interincisal distance) and by the extent of lateral excursion and of protrusion.
Deviation or deflection during mouth opening.
Assessment of pain with a visual analog scale with values from 0 (no pain) to 100 (strongest pain or discomfort).
Occlusion:
Motor nerve function (House–Brackmann grading system[
13]):
No deficit.
Mild weakness.
Moderate weakness.
Severe weakness.
Absence of function.
Sensory perception:
Patient satisfaction: Yes or No.
Radiological Assessment
Quantification of Degree of Displacement
The following methods were used to measure the degree of displacement of the fracture in the Towne radiograph: a line drawn between the medial and lateral poles of the condyle. Another line should be drawn tangent to the ramus. The inner angle formed by the intersection of the two lines was calculated. The difference between the angle on the nonfractured and the fractured sides was used as a measure of coronal displacement.[
5]
Quantification of Ramus Height Shortening
Furthermore, the loss of ramus height was measured on the panoramic radiograph: a reference line was drawn through both gonial angles. The perpendicular distance between the most superior point on the condyle and the reference line was calculated. The difference between the nonfractured and the fractured sides was used as a measure of difference in ramus length (loss of ramus height).[
5]
Statistical analysis: Shapiro–Wilk test was used to check which variables were following normal distribution. The scores of visual analog scale (assessment of pain), mouth opening, lateral excursion, protrusive movement, ramal height shortening, and fracture displacement were normally distributed. Independent Student’s t-test was used for comparing two groups with respect to continuous and normally distributed variables (p-value was >0.05). Chi-square test (degrees of freedom) was used for comparison between categorical variables (age, gender, etiology, site, occlusion, motor perception, sensory perception, and patient satisfaction). Level of statistical significance was set at p-value less than 0.05.
Results
Demographic Details
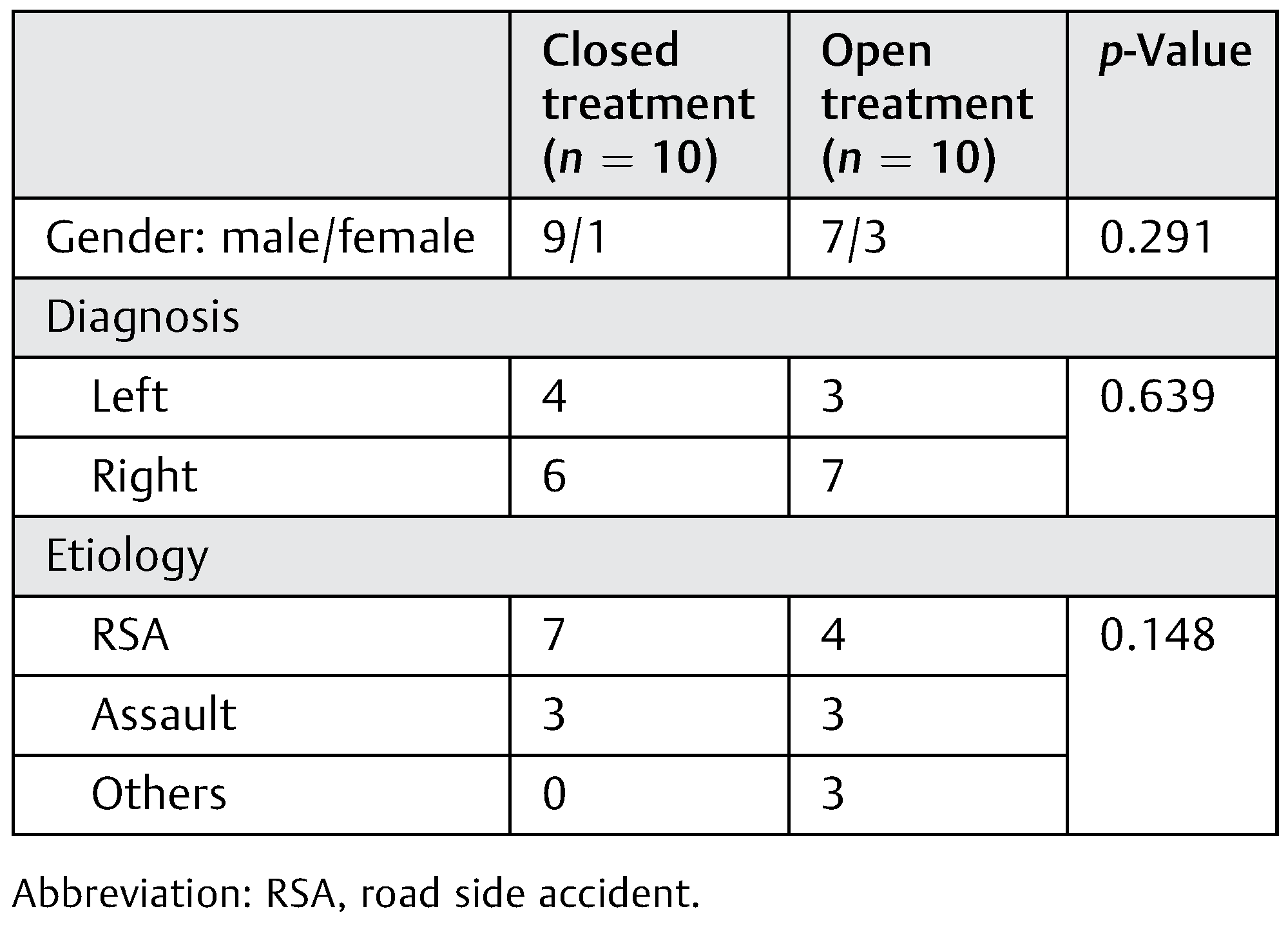
A total of 20 patients selected were included in the study. Out of which, 10 (50%) belonged to group A (closed treatment) and 10 (50%) belonged to group B (open treatment). The mean age at the time of injury was 29.8 years (range: 19–60), with 16 (80%) males and 4 (20%) females. In Group A, seven (70%) patients reported road traffic accident (RTA), three (30%) patients reported assault, and no (0%) patients reported other causes as etiology of fracture. In Group B, four (40%) patients reported RTA, three (30%) patients reported assault, and three (30%) patients reported other causes as etiology of fracture (
Table 1).
Clinical Results
Site of Fracture
In Group A, four (40%) patients had fracture at left side and six (60%) at right side. In Group B, three (30%) patients had fracture at left side and seven (70%) at right side. It was not found to be statistically significant (p = 0.639).
Assessment of Occlusion
In group A, two (20%) patient reported with functional malocclusion (range: 1–3) and in Group B, no patient reported with functional malocclusion (range: 1–2). It was not found to be statistically significant (p = 0.218).
Presence of Pain
In this study, the mean for the presence of pain was found to be statistically significant (p < 0.01) and less in Group B— open 5 (5.2) as compared with Group A—closed 23 (14.5).
Mouth Opening (1 and 6 Months)
The mean for mouth opening after 1 month was found to be 27.6 (1.5) in Group A and 36.2 (1.7) in Group B. It was compared using independent Student’s t-test and this difference was found to be statistically significant (p < 0.01).
The mean for mouth opening after 6 months was found to be 37.8 (2.57) in Group A and 40.9 (1.91) in Group B. It was compared using independent Student’s t-test and this difference was found to be statistically significant (p < 0.01).
Lateral Excursion and Protrusive Movements
The mean for lateral excursion was found to be 4.8 (0.78) in Group A and 6.7 (0.82) in Group B. It was compared using independent Student’s t-test and this difference was found to be statistically significant (p < 0.01).
The mean for protrusive movements was found to be 1.60 (1.07) in Group A and 1.1 (0.87) in Group B. It was compared using Independent Student’s t-test and this difference was not found to be statistically significant (p = 0.27).
Neurological Assessment
The distribution of patients according to the assessment of motor nerve function and sensory perception among the two groups was compared using chi-square test. It was not found to be statistically significant (p = 0.5).
Radiological Assessment
Ramal Height Shortening and Fracture Displacement
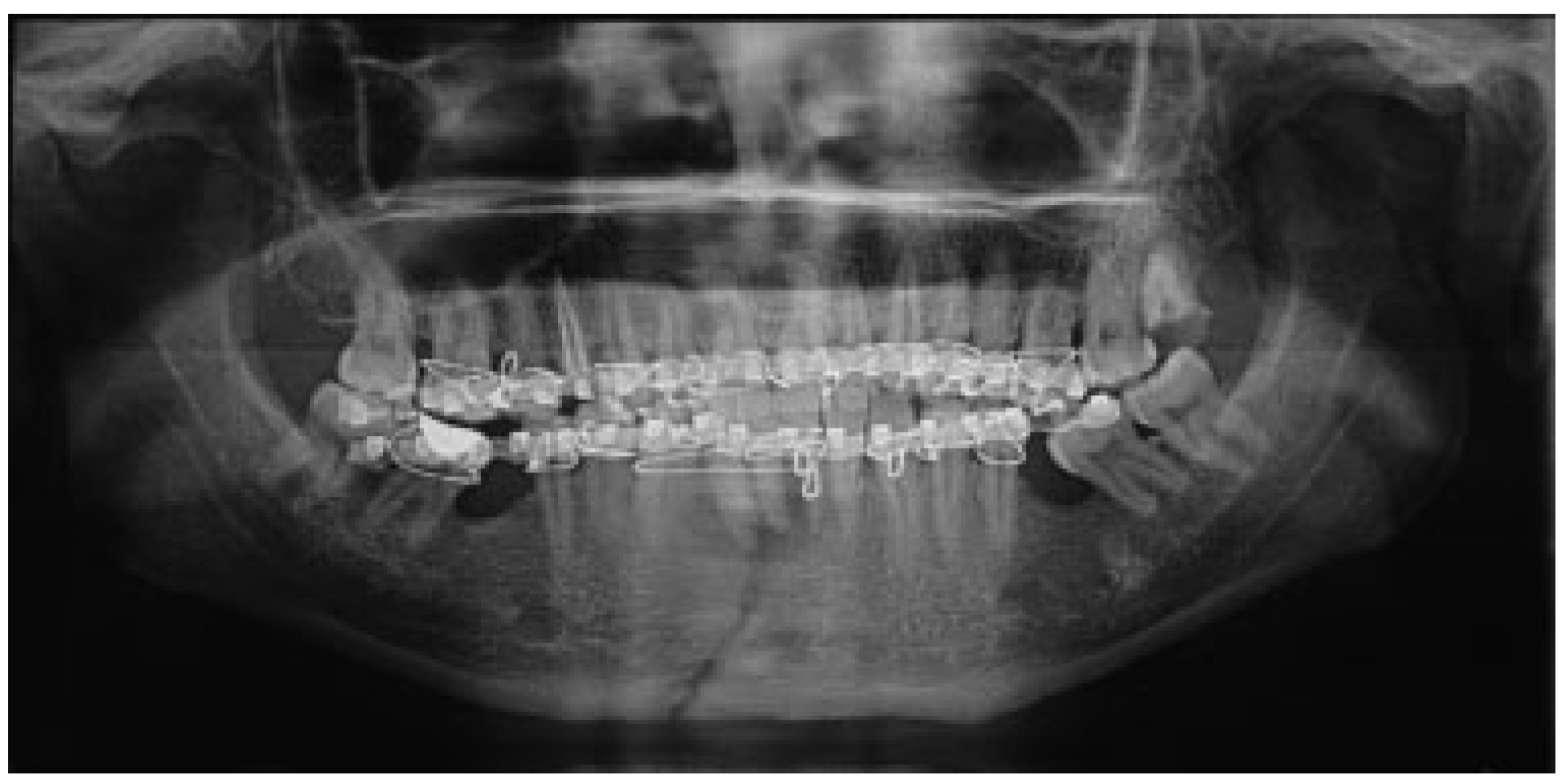
The mean for ramal height shortening was found to be 11.9 (0.99) preoperatively and 11.6 (1.57) postoperatively in Group A. It was compared using paired
t-test and this difference was found not to be statistically significant (
p = 0.34;
Figure 1 and
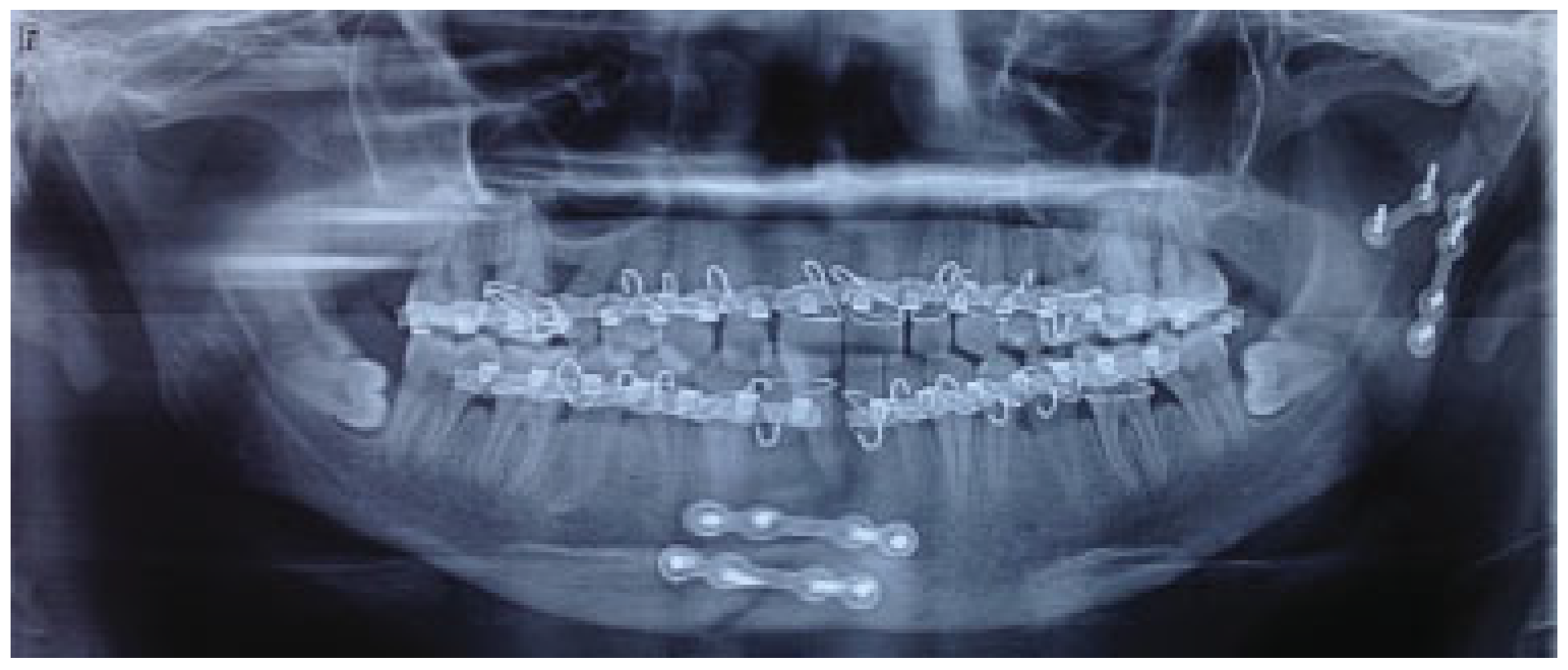
Figure 2). The mean for ramal height shortening was found to be 12.5 (0.84) preoperatively and (0.87) postoperatively in Group B. It was compared using paired
t-test and this difference was found to be
statistically significant (
p < 0.05;
Figure 3 and
Figure 4).
The mean for fracture displacement was found to be 29.9 (4.67) preoperatively and 28.2 (5.67) postoperatively in Group A. It was compared using paired
t-test and this difference was found not to be statistically significant (
p < 0.34). The mean for fracture displacement was found to be 30.9 (3.14) preoperatively and 1.8 (1.47) postoperatively in Group B. It was compared using paired
t-test and this difference was found to be
statistically significant (
p < 0.05;
Table 2).
Discussion
Facial area is one of the most frequently injured areas of the body, accounting for 23 to 97% of all facial fractures. There are changes in patterns of facial injuries, extent, clinical features, and so forth resulting in mild-to-massive disfigurement of maxillofacial skeleton along with functional loss.[
14] Mandibular fractures occur twice as often as midfacial fractures. Condylar fractures are a unique subset of traumatic injuries in the maxillofacial skeleton. Condylar and subcondylar fractures constitute 26 to 40% of all mandible fractures.[
15] Fractures of the subcondylar region constitute 20 to 62% of all mandible fractures.[
16,
17]
Many classification systems have been proposed by various authors for condylar fractures that offer insight into which fractures might be best treated with open or closed treatment.[
18]
Even after so much of research, a general consensus is that undisplaced subcondylar fractures should be managed with closed treatment, while displaced fractures should be managed by open treatment. The opinion regarding displaced fractures is based on the clinical experience of the surgeons. Most of the studies have compared the treatment options— closed or open for the management of subcondylar fractures without mentioning the details about their displacement. Their results cannot be relied upon as undisplaced fractures are managed by closed treatment and displaced fractures with open treatment and they compare the results. To the best of our knowledge, no study till date attempted to compare the two treatment options for similar kind of fractures, that is, the displaced subcondylar fractures. We also agree with the thought that undisplaced fractures should be managed with closed treatment, so that we can avoid the complications associated with surgery. However, the question arises is that whether we can avoid surgery in displaced fractures. This study was planned to answer this question. There are limited authors nowadays who advocate closed treatment in the displaced fractures. One of them is Edward Ellis; according to him, even displaced or dislocated unilateral condylar fractures can be managed with closed treatment if the patient has good dentition support and patient’s compliance.
There are studies that support open treatment for displaced subcondylar fractures. Liu et al[
19] in their meta-analysis of randomized controlled trials reported that closed treatment and open treatment, both options for unilateral displaced condylar fractures of the mandible, yielded acceptable results. Cranford et al[
20] also reported that decades of research has yielded a greater understanding of temporomandibular joint biomechanics and the benefits of open reduction and internal fixation, in cases of displaced and foreshortened subcondylar fractures. Therefore, in the present scenario, the actual challenge exists in the selection of appropriate treatment for a “displaced subcondylar fracture of mandible.”
The level of condylar fracture has a major effect on the selection of a method of treatment and is one of the most important factors; the degree of the displacement is the second most important variable for selecting method of therapy. Several reports regarding condylar fractures suggest that, compared with nonoperative treatment, treatment of condylar fractures by open reduction and rigid fixation creates more favorable results. The advocates of surgical treatment are convinced that this makes it possible to achieve the correct restoration of the condylar process, and to reestablish the optimal function of the jaw. The proponents of conservative treatment believe that the selective exercises lead to functional adaptation of the bony structures and the surrounding soft tissues. Henceforth, this study was undertaken to upgrade the concepts related to the management of unilateral displaced subcondylar fractures.[
3,
4]
For this prospective randomized study, unilateral subcondylar fracture as classified by Lindahl and Hollender[
11] and illustrated by Ellis and Throckmorton was included.[
9] In this study, ramal height shortening and degree of fracture angulation were also included as proposed by Bhagol et al.[
5]
A meta-analysis states that for unilateral “moderately” displaced mandibular condylar fractures, operative treatment was superior in most objective and subjective functional parameters.[
19] Bhagol et al also found similar results for the moderately displaced subcondylar fractures.
These further strengthen the results of the present study for “unilateral “severely” displaced mandibular subcondylar fractures, that is, better treatment outcomes and less pain were observed in the open treatment group. The surgical treatment used was retromandibular approach. Chrcanovic, in a recent meta-analysis, reported this to be the preferred choice of treatment, followed by submandibular approach.[
10]
In this study, we found statistically significant difference in pain, mouth opening, and lateral excursion movement between the two groups. Open treatment provides better clinical and radiological outcomes for the displaced subcondylar fractures. No significant complications existed in the open group (10% facial nerves paresis). No significant scarring was evident in any of the operated patient.
However, contrary to this, disfigurement was seen in some of the patients of closed treatment group in this study. These findings suggest that if tissues and supporting structure are heavily damaged as in case of displaced condylar fractures, repair occurs by laying down of connective tissue, a process that may result in facial disfigurement. Therefore, the advantage of anatomical reduction is not just of radiological significance but it also aids in restoring the facial form of the patient.
This research is also accompanied with several shortcomings which need to be further explored for better understanding of the treatment protocol. One of the limitations of the study could be the time period for postoperative assessment. Evaluation of clinical outcome after 1, 2, and 5 years would have resulted in better understanding of the treatment modalities. It is well known that in the long term, incomplete anatomical restoration in nonsurgical methods can cause facial asymmetry and inclination of the occlusal plane, as well as functional occlusal problems, such as premature contact in protrusion and lateral protrusion. Moreover, nonsurgical treatment, even if correctly performed, is lengthy, requires continuous adjustment, and is more uncomfortable for the patient than open reduction and rigid fixation. Second, it should be noted that the classification method used in this study is not landmark based and might have restricted enrollment of patients in the study.
Conclusions
The results of the study favor the open treatment for the management of displaced subcondylar fractures. However, we recommend a prospective, multicenter study with larger sample size to assess the results.