Condyle-bearing reconstruction plates or condylar head add-on systems are intended for temporary reconstruction in patients undergoing ablative tumor surgery requiring the removal of the mandibular condyle. This device is not for permanent implantation, for patients with TMJ or traumatic injuries, or for treatment of temporomandibular joint disease (TMD). The use of this system is limited to a maximum of 2 years, and the device is not intended to be loaded to reestablish complete function (Information stated on Depuy Synthes Web site). However, in many units around the world, these are used as a permanent solution for the benefit of less cost and/or morbidity compared with microvascular or alloplastic total joint reconstruction.
This case report describes the long-term faith of a condyle bearing reconstruction plate replacing resected part of the mandible due to a keratocystic odontogenic tumor (KOT) where total joint reconstruction was the ultimate choice of treatment.
Case Report
A 51-year-old woman was referred to the Department of Oral and Maxillofacial Surgery at Karolinska University hospital in Stockholm in January 2000 with a chief complaint of intermittent pain and swelling in the right posterior mandible with duration of several weeks. The patient was initially seen and treated by another surgeon at the department and her notes were reviewed retrospectively. She was well nourished and her medical history was noncontributory. Upon clinical examination, there was no asymmetry in the face, no sensory disturbance, and no intraoral swelling, and she demonstrated normal occlusion and normal range of motion in the TMJ. An orthopantomogram revealed a multilobular process involving the right hemimandible with an extension from the first molar to the condylar neck and head. A computed tomographic (CT) scan with contrast was ordered, which clearly demonstrated the extent of the lesion (
Figure 1a,b). Differential diagnosis included follicular cyst, KOT, ameloblastoma, and odontogenic myxoma. An incisional biopsy under local anesthesia confirmed the diagnosis of a para-KOT. Taking the size and type of the lesion into account different treatment modalities was suggested to the patient. Full resection including disarticulation and reconstruction with a condyle-bearing reconstruction plate, a decompression procedure to shrink the lesion and perhaps save the involved condyle and finally enucleation of the lesion, were discussed with the patient. Pros and cons with each and every alternative were explained to the patient. For unknown reasons, no bony reconstruction was discussed with the patient. The patient opted for a decompression procedure, which was completed 2 weeks after the initial visit. The lesion was unroofed through a vestibular approach and the cavity was drained on its content and irrigated with saline. A 3-cm suction catheter serving as a stent was sutured to the edges of the mucosa to keep a persistent opening into the lesion. The patient was instructed to irrigate the cavity with a 20-mL syringe of saline twice a day and was kept under regular follow-up appointments. During the ensuing 8 months, there were numerous, unscheduled visits to manage, adjust, reinsert, or retrieve the decompression stent. Hence, the desired shrinkage of the lesion was not obtained and the patient agreed upon full resection and reconstruction with a condyle bearing reconstruction plate. Again, no bony reconstruction was discussed or suggested to the patient according to the notes.
In December 2000, the patient was subjected to surgery for the second time. Through an extended submandibular incision on the right side, the lesion was accessed and a full resection posterior to the second bicuspid including disarticulation was performed. Care was taken not to violate the thin tumor boundaries of the tumor on the medial side. A condyle-bearing reconstruction plate (no information on type or origin available) was inserted to restore function and symmetry to a certain degree. Incision was closed in layers and a drain was kept in place for 48 h. Recovery was uneventful and the patient was discharged 2 days later. The final diagnosis was para-KOT. One year postoperatively, the symmetry of the face was acceptable and the function of the right TMJ was within normal range. The patient was put on a regular recall system up to 10 years postoperatively to detect any recurrence.
No recurrence was seen during this period and regular follow-ups were discontinued.
In March 2015, the patient returned to the clinic almost 15 years after surgery, complaining of “weird bite” and pain upon chewing. At this time, she was seen by the author. She described a cracking sound from the jaw couple of days earlier while chewing. Her medical history was once again noncontributory. Clinical examination revealed a deviated chin to the right and slight asymmetry in the right cheek (
Figure 2). Furthermore, there was obvious malocclusion and the range of motion was restricted (
Figure 3). The intraoral lining was intact. An orthopantomogram disclosed a fracture of the reconstruction plate in the body area. The condylar head was intact (
Figure 4).
A CT scan with maximum of 1-mm cuts was obtained, which did not reveal any abnormalities in the joint. Free vascularized flap or a custom-made prosthesis was suggested to the patient, and pros and cons with each procedure were explained. Because of the large defect, the desire of the patient to limit scarring on the face, and also the fact that the patient did not express any wish to replace the missing teeth, it was decided to perform reconstruction with an alloplastic total joint prostheses rather than with a vascularized flap. The CT scan was sent to TMJ Concepts technician where a three-dimensional (3D) stereolithographic skull model was created. The left hemimandible was mirrored and an extended custom-made prosthesis was waxed up and fabricated eventually (
Figure 5 and
Figure 6). A hole was made in the condyle for a vertical suspension suture.
In June 2015, the patient was operated on where the condyle-bearing reconstruction plate was removed through an endaural and a submental incision (
Figure 7). Remnants of the native disc and synovial tissue were removed and the fossa contoured according to the planning. The fossa component was secured to the zygomatic arch in a routine fashion. A tunnel was created between the submental and endaural incision, and the ramus part was placed through the submental approach and seated in the fossa. A 2–0 PDS Vicryl suture secured the condyle to one of the fixation screws on the fossa part (
Figure 8). The incision was closed in layers and no drain was used postoperatively. Recovery was uneventful and the patient was discharged 24 h after surgery. A CT scan was done postoperatively and confirmed adequate placement of the prosthesis (
Figure 9). Sutures were removed 1 week later. Upon 6-month follow-up, there was excellent occlusion and adequate symmetry, the scars were almost inconspicuous, and maximum incisor opening measured 40 mm. The patient has been followed up for 15 months postoperatively with good symmetry and range of motion (
Figure 10).
Figure 4.
Orthopantomogram reveals fracture of the reconstruction plate.
Figure 4.
Orthopantomogram reveals fracture of the reconstruction plate.
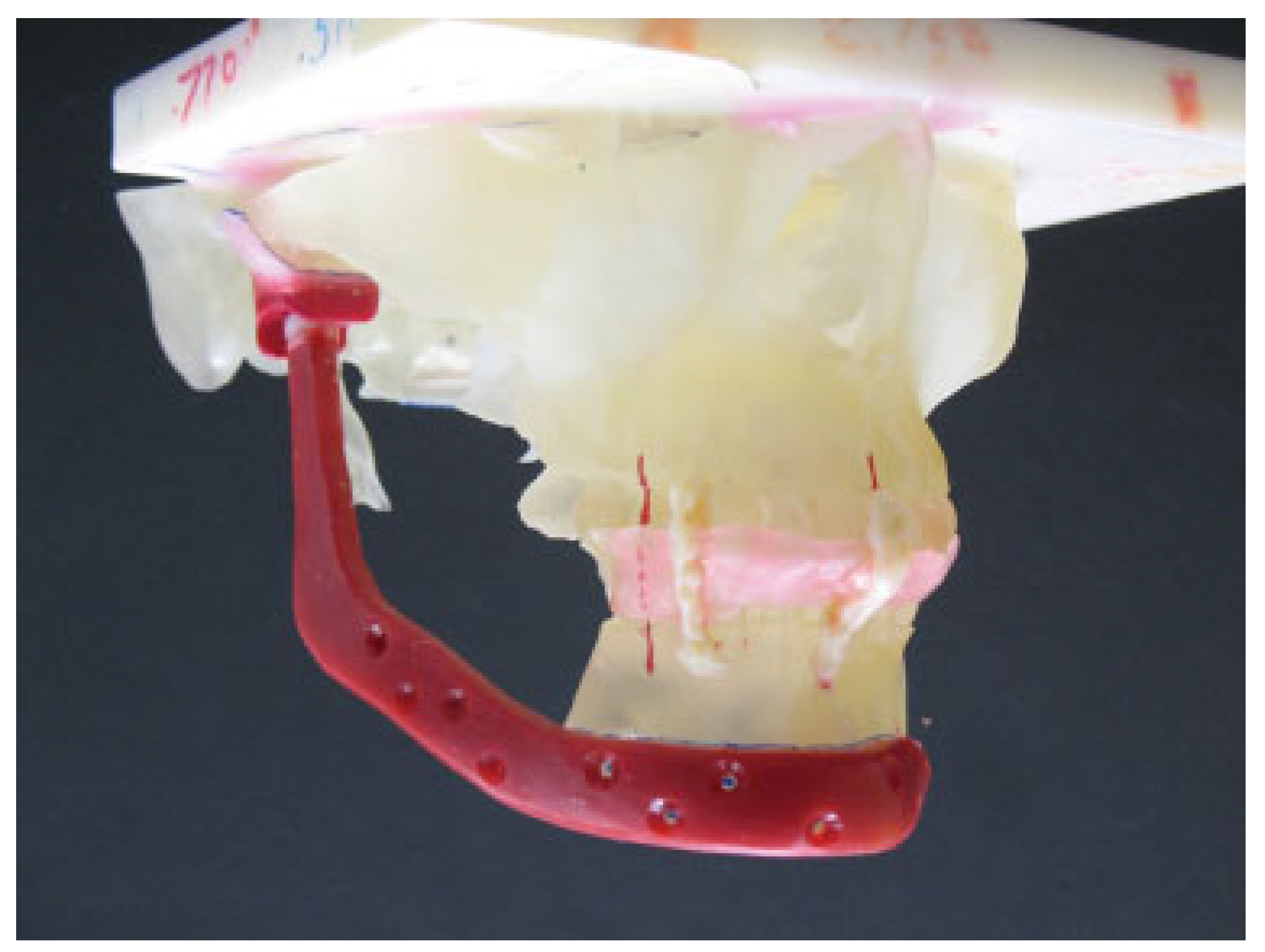
Figure 5.
Vax-up of the extended custom-made prosthesis made on a 3D stereolithographic model.
Figure 5.
Vax-up of the extended custom-made prosthesis made on a 3D stereolithographic model.
Discussion
KOTs are known for unique and varied behavior, high recurrence rates, and distinctive histopathology findings [
4]. They account for approximately 12 to 14% of all odontogenic cysts of the jaws and have a predilection for the posterior part of the mandible with a peak incidence in patients between 10 and 30 years of age [
5]. Radiographically, the lesion is most often unior multilocular radiolucency, surrounded by smooth or scalloped margins with sclerotic borders. KOT has presumably arisen from cell rests of the dental lamina or from offshoots of the basal cell layer of the oral epithelium [
5]. Although various therapies for KOT have been documented in the literature, the universally accepted approach remains undecided. Multiple treatment protocols for KOT have been reported in the literature, with recurrence rates ranging from 0 to 62% [
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35]. Resection is reported to have 0% recurrence rate but at an increased morbidity for the patient [
5,
15,
20,
21,
22,
34]. Decompression with or without residual cystectomy and enucleation with or without adjuvant therapy (Carnoy solution, cryotherapy, or peripheral ostectomy) are often tolerated for the benefit of less morbidity for the patient [
6,
8,
10,
12,
13,
23,
24,
25,
26,
35]. Microscopically, KOTs are divided into two categories: orthokeratocysts and parakeratocysts of which the latter have a more aggressive behavior, exhibiting potential for local destruction and extension into adjacent tissues, rapid growth, a higher rate of recurrence, and a tendency for multiplicity [
5].
Figure 6.
Actual prosthesis with a hole made in the condylar head for a vertical suspension suture.
Figure 6.
Actual prosthesis with a hole made in the condylar head for a vertical suspension suture.
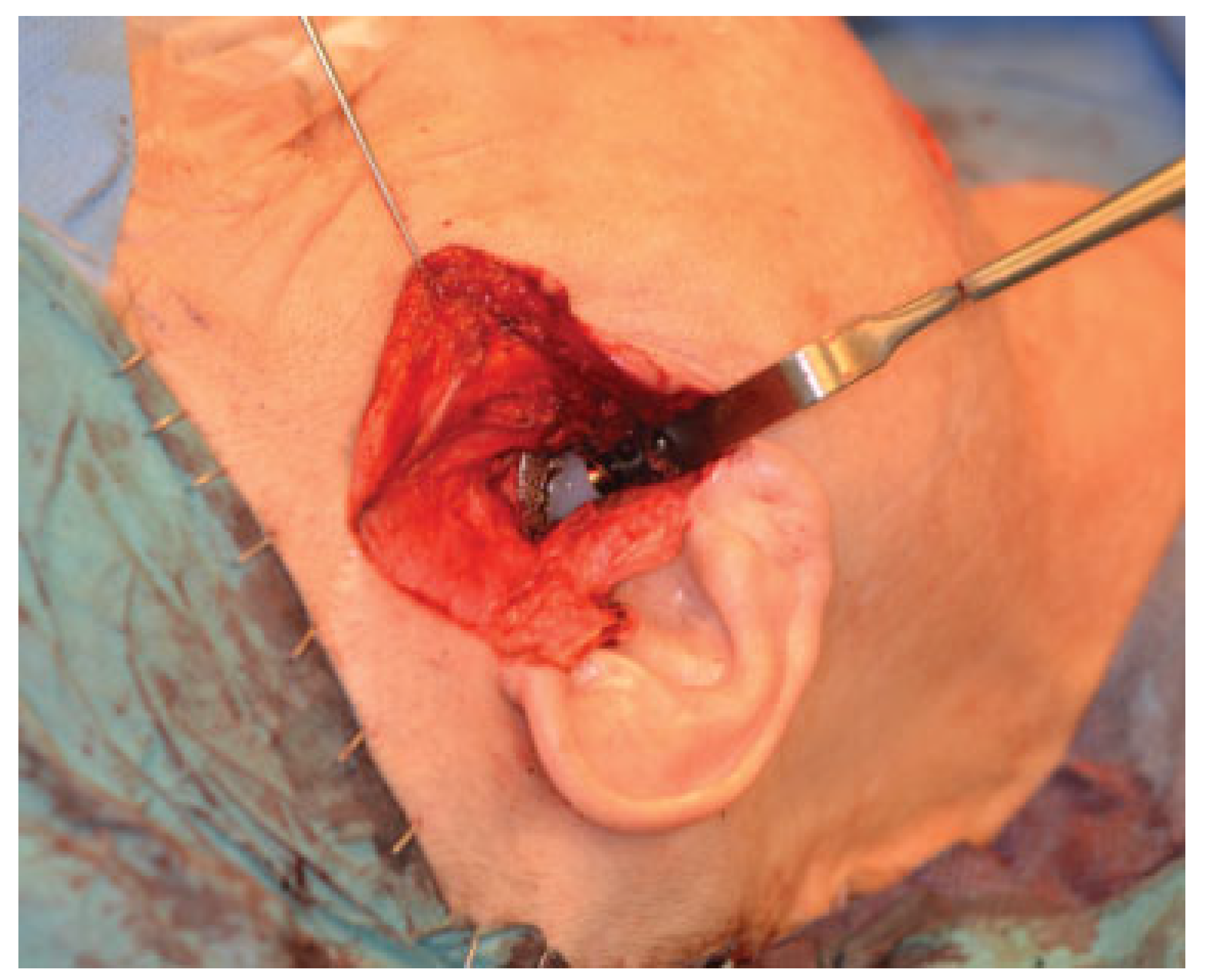
Figure 7.
Fractured reconstruction plate removed through a combination of endaural and submental incision.
Figure 7.
Fractured reconstruction plate removed through a combination of endaural and submental incision.
Figure 8.
Fossa part fixated to the zygomatic arch. Ramus part is seated in the fossa. Note the suspension suture secured to one fixation screw on the fossa part.
Figure 8.
Fossa part fixated to the zygomatic arch. Ramus part is seated in the fossa. Note the suspension suture secured to one fixation screw on the fossa part.
Figure 9.
Postoperative 3D scan showing adequate placement of the prosthesis.
Figure 9.
Postoperative 3D scan showing adequate placement of the prosthesis.
In the present case, a more conservative approach was chosen by the treating surgeon initially to save the native TMJ. It is debatable whether this treatment modality was the best option for this patient taking the size and the radiographic appearance of the lesion into account. Furthermore, this treatment modality might seem obsolete today. However, there are still several authors advocating this treatment to save vital structures and reduce morbidity for the patient, and we believe that this treatment was more common almost two decades ago when the patient was treated initially [
11,
12,
35]. Unfortunately, in this case the expected outcome with decompression was not satisfactory due to noncompliance and/or difficulties irrigating the cavity with normal saline. Because the KOT in this case was multilobular, involved the condylar neck, and histologically belonged to the more aggressive type, the next in-line treatment modality was full resection including disarticulation.
Disarticulation resection of the mandible results in a complex deformity that has significant potential to affect facial appearance and oral function. It is expected that a successful reconstruction of such deformity will restore the facial form, maintain the premorbid dental relationship, and preserve mouth opening. Ideally, this would be accomplished at the time of ablative surgery.
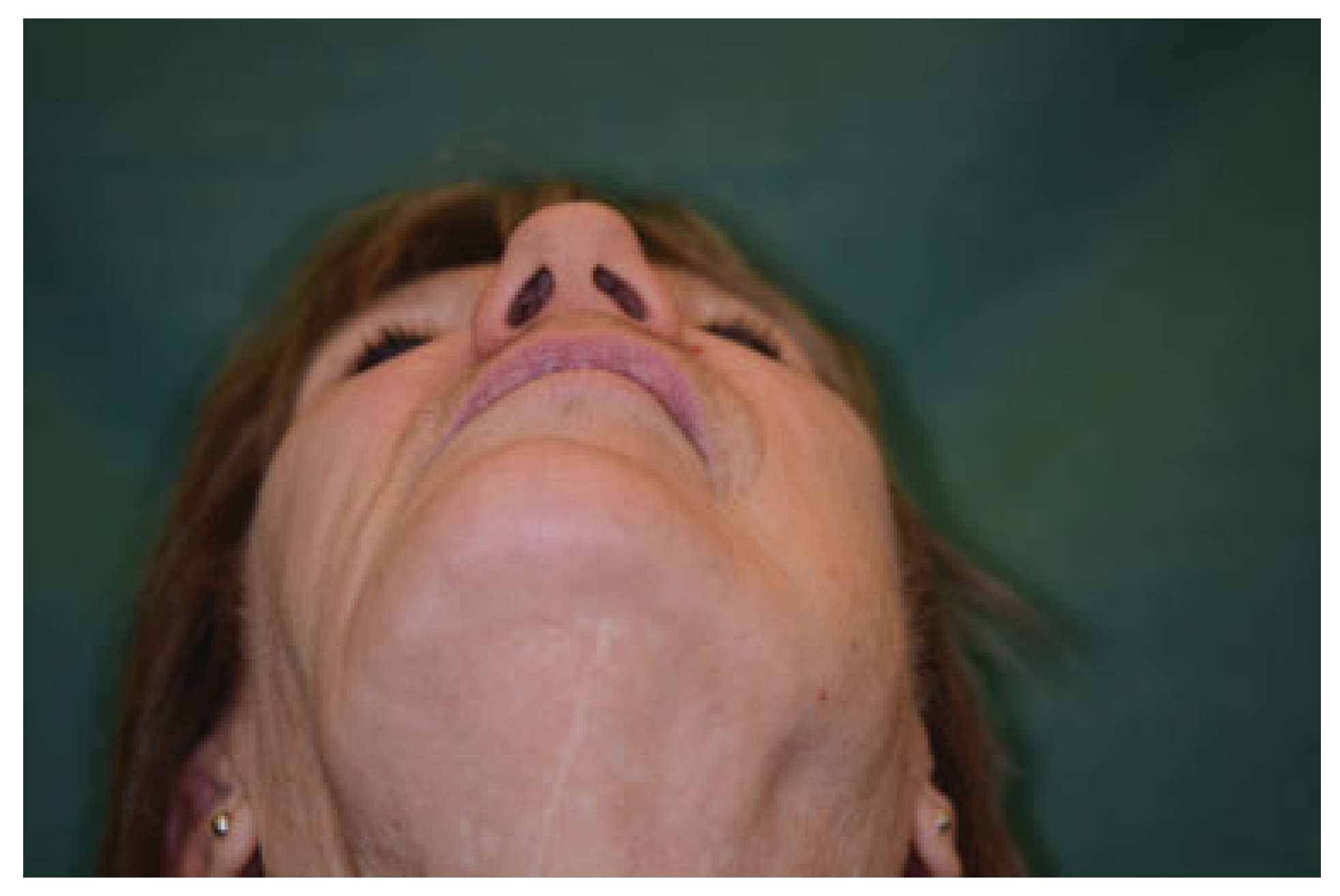
Figure 10.
Final outcome photograph. Slight asymmetry is seen in the soft tissues on the right side.
Figure 10.
Final outcome photograph. Slight asymmetry is seen in the soft tissues on the right side.
Ideal reconstruction of the mandible including the TMJ in a tumor case as such would probably be a vascularized bone graft. Vascularized tissue transfer has several recognized benefits. First, because blood flow is maintained, there is a relative resistance to infection, which makes its use in primary reconstruction reliable. Donor sites can be selected to best match the resected tissue. Composite flaps can be designed to restore bone and soft tissue in one procedure.
The workhorse in the mandible is the free fibula, which was introduced back in 1989. The fibula free flap approach allows the possibility of using bone with/without skin for restoring the defect. It has the advantages of consistent shape, ample length, and distant location to allow a two-team approach. It can also be raised with a skin island for composite-tissue reconstruction. The fibula also seems particularly well suited for condyle replacement as the bone is tubular in shape and densely cortical. It is easily adapted to passively fit in the glenoid fossa, and its narrow shape allows it to fit easily through the soft tissue tunnel avoiding dissection in the region of the facial nerve [
36]. Guyot et al. reported on 11 patients followed up over 6 years and found a rounding off of the fibula in the glenoid fossa, which they felt was related to function against the temporomandibular disc. In their cases, oral function was preserved and there was no case of ankylosis [
36]. However, in another series of six patients in whom the condyle was reconstructed with a vascularized fibular flap and followed up for a mean period of 36 months, one case of temporofibular ankylosis was reported [
37].
One major drawback to the fibula is its restriction in terms of 3D shaping and also transfer of a fibula graft vastly increases surgery time and morbidity for the patient. Comorbidities of a patient may also preclude free tissue transfer. Costochondral and sternoclavicular grafts are other autogenous options when reconstructing the TMJ [
38,
39].
In this patient, the TMJ, entire ramus, and portion of the mandibular body had to be reconstructed, which is not feasible with the latter two alternatives. The costochondral and sternoclavicular graft do not enable adequate reconstruction of the ramus and body of the mandible indicating need for another donor site, which adds to the overall morbidity. The option of free vascularized fibula was suggested and discussed with the patient. However, the patient expressed a strong desire to minimize scarring on the face and at the same time did not request any dental rehabilitation postoperatively to replace the missing teeth. She also thought that a free tissue transfer would be “too much of surgery” at her age. Taking these facts in to consideration, we opted for an alloplastic reconstruction, although long-time prognosis of such an extended device would theoretically be inferior to a vascularized flap. Prosthetic TMJ reconstruction in cases with major mandibular defects or other abnormal anatomy usually requires custom-made devices.
Alloplastic custom-made joints allow for a more precise anatomic and aesthetic reconstruction, avoid donor site morbidity, and reduce operative time. The major disadvantage would probably be the unknown life expectancy of the devices, the possibility of a giant cell foreign-body reaction due to wear, dystrophic bone formation, loosening of the implant, and the high expence [
40].
The TMJC (TMJ Concepts INC, Ventura, CA) device is a computer-assisted designed and manufactured (CAD CAM) prosthesis constructed on a stereolithic 3D model fabricated from the patient’s CT scan data. The fossa component consists of an ultra-high-molecular-weight polyethylene (UHMWPE) articulating surface and the ramus component is made of a machined alloyed titanium with a condylar head of chrome-cobalt-molybdenum (Cr-Co-Mb) [
40]. Most TMJC devices installed over the years have been straightforward local TMJ reconstructions, but more recently they have been used to bridge increasingly large mandibular defects [
41,
42,
43,
44]. Westermark et al. reported a series of four cases where the prosthetic components were designed to restore major defects in the zygomatic arch, mandibular ramus, and body, including one case in which the mandibular component was used to restore total mandibular continuity. Follow-up was up to 6 years, and they concluded that a customized prostheses combined with TMJ reconstruction is a reliable treatment alternative for bridging complex, major maxillomandibular defects [
41].
Zanakis et al. reported a case of hemifacial microsomia that was initially reconstructed with autogenous bone, but because of major resorption of the graft, a new reconstruction was made with a custom-made TMJ prosthesis. The patient was followedup for 2 years with good range of motion and excellent symmetry [
42]. Other case reports show similar promising results with the extended type of TMJ prostheses in function up to 3 years [
43,
44]. When using such a big piece of alloplastic device, there is theoretically a risk of condylar sag, especially in congenital deformity cases where the pterygomasseteric sling is totally or partially absent. A modification which is standard nowadays in all extended TMJC devices is a smooth edged hole that has been introduced just inferior to the condylar head. The hole can be placed either medial to lateral or anterior to posterior depending on the surgeon’s preference. This allows for a vertical suspension suture to maintain the vertical position until the scar tissue is mature enough to support the mandible. We used 2–0 PDS suture, which was secured around one of the fixation screws of the fossa component.
In this patient, the outcome of the previous intervention was acceptable in terms of symmetry, TMJ function, and no recurrence. The patient reported no symptoms during the next 15 years, but the reconstruction plate fractured eventually due to fatigue of the device.
Reconstruction of disarticulation continuity defects using metallic condylar replacements and its outcomes have been reported by several authors with mixed results and profound conclusions. However, all these studies report only a few cases with short-term follow-up, making their conclusion unreliable. Lindquist et al. reported a series of 23 TMJ arthroplasties, using metallic prostheses back in 1992. Indications for arthroplasties included severe ankylosis, segmental mandibular resection in tumor surgery, and extensive trauma. Seven (30%) prostheses were removed and/or exchanged during the average 27.6-month follow-up [
2]. They concluded that in case of primary joint pathology, such as rheumatoid arthritis or ankylosis, metallic condylar replacements that do not include a fossa component are contraindicated. Patel and Maisel reported their results in four patients receiving condylar replacements for malignant tumor extirpations with a mean follow-up of 23.3 months. They reported significant complications: malocclusion, infection, three plate exposures, and one plate migration that resulted in neurosensory hearing loss [
45]. Daniel and Browne reported much more positive results in six similar condylar replacements due to malignant tumor extirpation with a mean follow-up of 6.4 years. They observed no plate exposures, plate migration, or malocclusions, and attributed their high rate of success to preservation of the disc and TMJ capsule, purse-string sutures around the condylar head to prevent migration, and adequate soft tissue coverage [
46]. Carlson reported his results in 16 patients in whom metallic condylar head was used for disarticulation resections for both benign and malignant tumors. Only 3 of 16 patients developed complications. He also attributed his success rate to preservation of the disc and strict adherence to the principles of rigid fixation [
47].
To date, the largest series of disarticulation resections, reconstructed with metallic condylar head alone, was reported by Marx and coworkers [
48]. They reported of 131 cases followed up for a mean time of nearly 8 years. Complication rate was less than 10% and these occurred mainly in the irradiated patients. They concluded that alloplastic replacement of the mandibular condyle with a metallic condyle on a rigid reconstruction plate functioning against a natural disc or a soft tissue graft in the temporal fossa provides long-term stability with minimal complications. Although there is some evidence in the literature against the use of condyle-bearing reconstruction plate as a permanent solution, one needs to bear in mind that in patients undergoing ablative surgery including disarticulation, the maximal biting force and consequent compressive forces on the glenoid fossa are strongly reduced [
49]. This is in contrast to patients suffering from TMJ disorders often combined with immense pressure on the glenoid fossa. This is probably an explanation to why reconstruction plates with a condylar head work, sometimes even as a long-term condylar replacement in ablative surgery.
Having said that, in the author’s opinion, the use of condylar bearing reconstruction plates should be restricted to a short period during which a permanent reconstruction is being planned.
We did not see any signs of erosion upon surgery nor did the patient report any symptoms from the TMJ and this was probably due to preservation of the native disc at previous surgery. This is in accordance with the conclusion made by Marx and coworkers. They underline the importance of a soft tissue interface between the metal condyle and the native fossa, which ideally is preservation of the native disc or use of temporalis fascia, allogenic dura, or cartilage [
46].
In conclusion, reconstruction of large mandibular defects is possible with good clinical outcome. Although successful in this patient, with increasing length and volume of the mandibular components, it is likely that the risk of fatigue fracture will increase and further studies are needed to reveal this.