Fibrous dysplasia (FD) is a disturbance of the mesenchymal tissue accounting for 2.5% of all bone tumors and more than 7% of nonmalignant bone tumors [
1]. In 1891, Von Recklinghausen defined a pathologic condition of the bone characterized by deformity and fibrotic changes as “osteitis fibrosa generalisata” [
2]. In 1938, Lichtenstein and Jaffe used for the first time the term “fibrous dysplasia” [
3]. FD is a rare disease that occurs predominantly in the first and third decades, and in most cases the progression stops after adolescence; it is more common in female patients. The etiology of these abnormal fibro-osseous processes depends on the increased formation of cyclic adenosine monophosphate (cAMP) due to mutations in a Gs protein. The overproduction of cAMP promotes osteoclastogenesis [
4]. FD presents in three forms: monostotic, polyostotic, and polyostotic with endocrinopathies (also known as
McCune-Albright syndrome). The monostotic form constitutes 80 to 85% of all FD cases, and craniofacial lesions occur in 10% of monostotic FD patients. In the craniomaxillofacial region, FD affects the calvaria, skull base, zygoma, and jaws; the prevalent site is the maxilla (50% of cases) [
5]. Maxillary lesions often involve adjacent bones. Thus, the term “monofocal” is appropriate when several skull segments in a single area are affected [
6].
Craniofacial FD primarily involves erosion from inside of the medullary or cancellous bone; this behavior gives a typical radiologic pattern to the lesions, which have a woven-like or ground-glass appearance, always with a thin shell of the normal cortical bone and poor margins blending gradually into regular bone. Because lesions involving the mandible can be misdiagnosed as simple bone cysts, a computed tomography (CT) scan is considered the best imaging technique for diagnosis, staging, and treatment planning. Once the diagnosis of craniofacial FD is made, other skeletal lesions can be searched by bone scintigraphy [
1].
Histologically, the lesions can present three types of patterns: the “Chinese letters” model, the most common, with thin bone trabeculae and active osseous reabsorption, the pagetoid model, and the hypercellular model [
7].
Clinically, the presenting complaint of craniofacial FD is progressively growing painless swelling in 90% of cases; midfacial and periorbital FD can cause nasal obstruction, sinusitis, and visual impairment. FD of the jaws can cause malocclusion and dental problems; in some patients it can involve most of the craniomaxillofacial region, causing mega-cranium and a condition known as “lion face”.
FD usually is a benign condition, but nearly 1% of patients have malignant transformation, particularly patients affected by McCune-Albright syndrome and patients treated with radiotherapy [
1].
The radiographic characteristics of FD have three basic patterns: no ossification, mottled ossification, and lamellar ossification. The first CT pattern shows a total absence of bone formation within the tumor and CT reveals hyperdense areas with irregular edges. The second CT pattern shows irregular borders and invades the cortex, in some cases with a groundglass appearance; this radiologic feature may be confused with FD. The third CT pattern shows new bone formation within the tumor, in the form of characteristic bony lamellae irradiating from a focus like a “sunburst”. Thus there are no pathognomonic radiological aspects for FD [
8,
9].
Therapy for craniofacial FD is surgical with the goals being to prevent functional disorders and restore facial symmetry, volume, and contour. According to Chen and Noordhoff [
10], the craniomaxillofacial bones are in four major zones with each zone having a precise indication for conservative or radical treatment.
The craniofacial skeleton can be classified into four major zones in the surgical treatment of FD [
11]. Zone 1 includes the fronto-orbital, zygomatic, and upper maxillary regions; zone 2 represents the hair-bearing cranium; zone 3 is the central cranial base; and zone 4 includes the teeth-bearing regions of the maxillary alveolus and mandible. Radical resection of the dysplastic bone is recommended for lesions in zone 1 and conservative excision or shaving is proposed for lesions in other zones [
12].
This article reports the case of a young female patient affected by right orbital-zygomatic-maxillary FD who had developed facial asymmetry and malocclusion that was corrected with an osteotomy using the Schuchardt-Kufner technique.
Case Report
The patient was a 25-year-old woman suffering from FD involving the right hemiface with clinical onset at the age of 5 years. At the age of 14 years, she underwent histopathologic investigations that confirmed the diagnosis. At the age of 17 years, she had two surgical remodeling procedures of the right maxillary bone and mandibular zygomatic region, with extraction of teeth 1.8, 2.7, 2.8, 4.7 and 4.8, and gingivoplasty. At the age of 25 years, she was referred to us.
The clinical picture showed severe deformity of the right half of the face with protrusion and swelling of the orbital-zygomatic maxillary region and involvement of the right hemimandible. In the submentovertex projection, severe asymmetry with macrosomia of the right hemiface was evident. There was also asymmetry of the oral rim with deviation from left to right and from top to bottom.
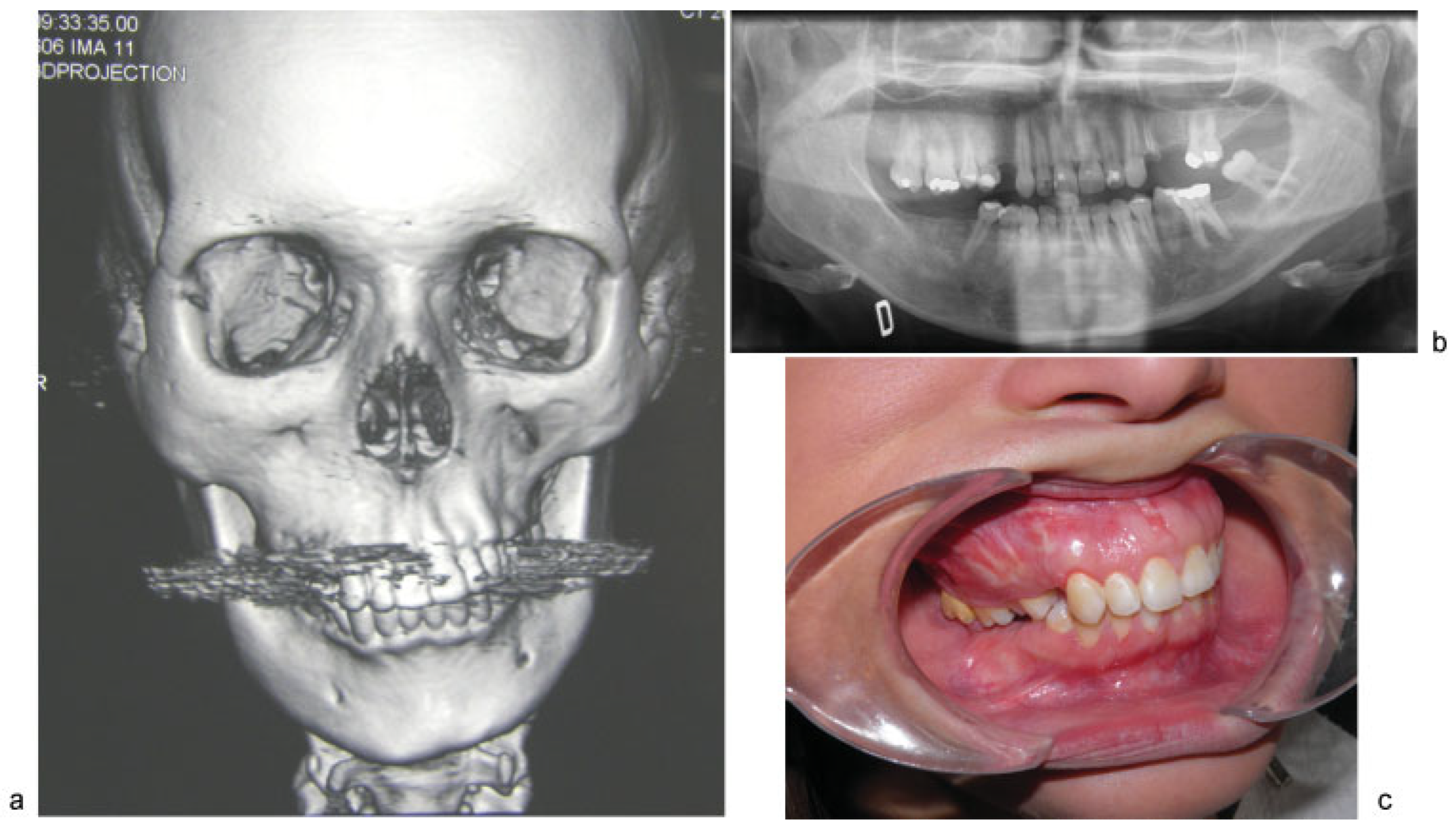
Intraoral inspection showed swelling of all the right maxillary bone from the right vestibular fornix with diastema between the canine and premolars. There was a significant downward prolapse of all the alveolar bone comprising the dental elements 1.4, 1.5, 1.6, and 1.7, with these teeth in contact with the mucosa of the corresponding mandible that appeared edentulous (
Figure 1a–c). This caused serious difficulty with chewing and also a lack of space for mandibular prosthetic rehabilitation. The patient was then submitted to segmental osteotomy of the superior maxilla.
Surgical Steps
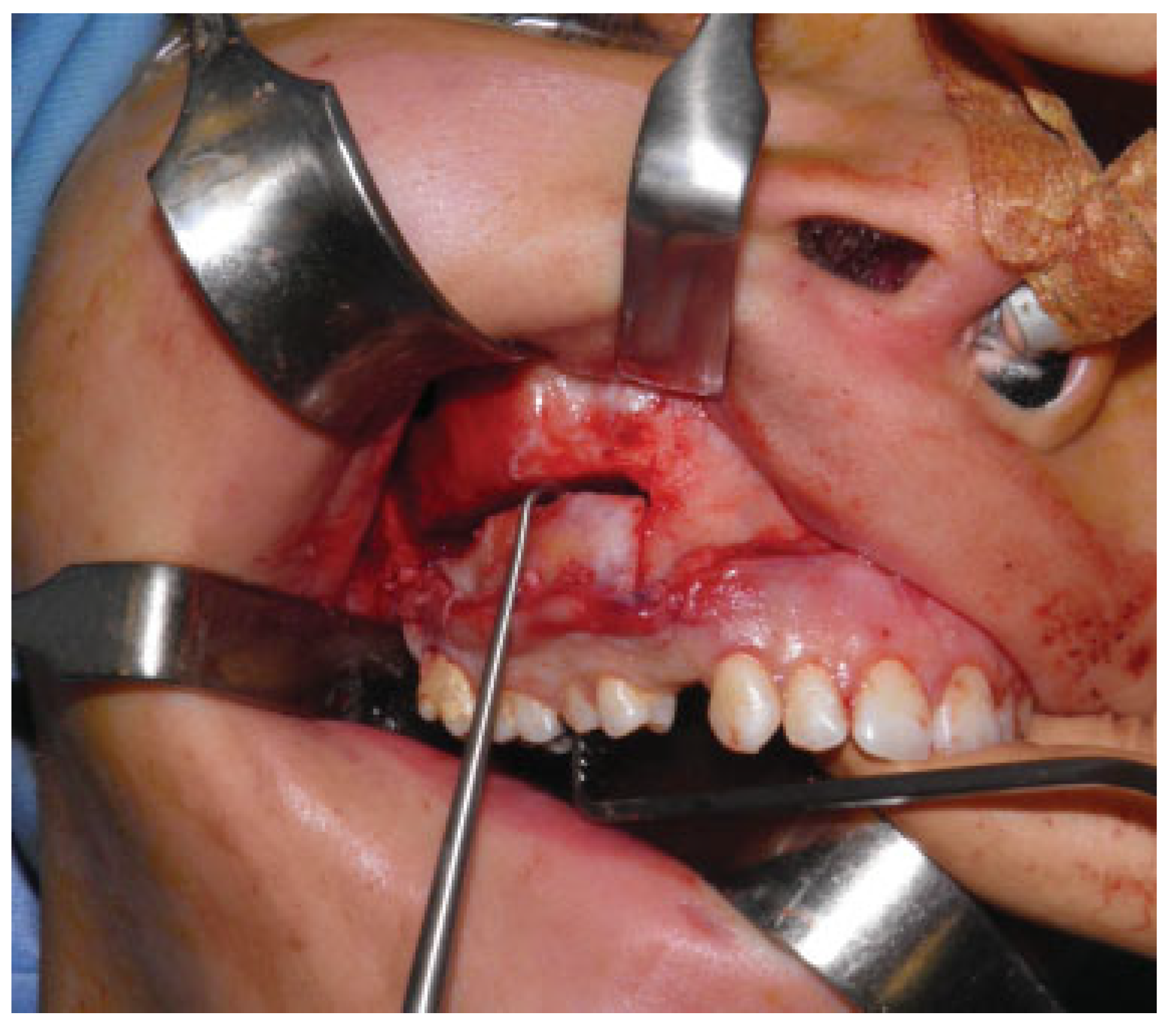
The main surgical steps were infiltration, incision of the top right maxillary mucosa, bone exposure, and preparation of a vestibular mucoperiosteal flap. Thereafter right zygomatic bone and upper maxilla shaving and simmetrization with the contralateral side were completed (
Figure 2).
Segmental osteotomy, according to Schuchardt-Kufner, comprises the elements 1.5, 1.6, and 1.7; impaction of the maxilla 3 mm in the front and 10 mm in the rear with a feed rate of 4 mm; pterygomaxillary dysjunction; and mobilization of the bone fragment (
Figure 3).
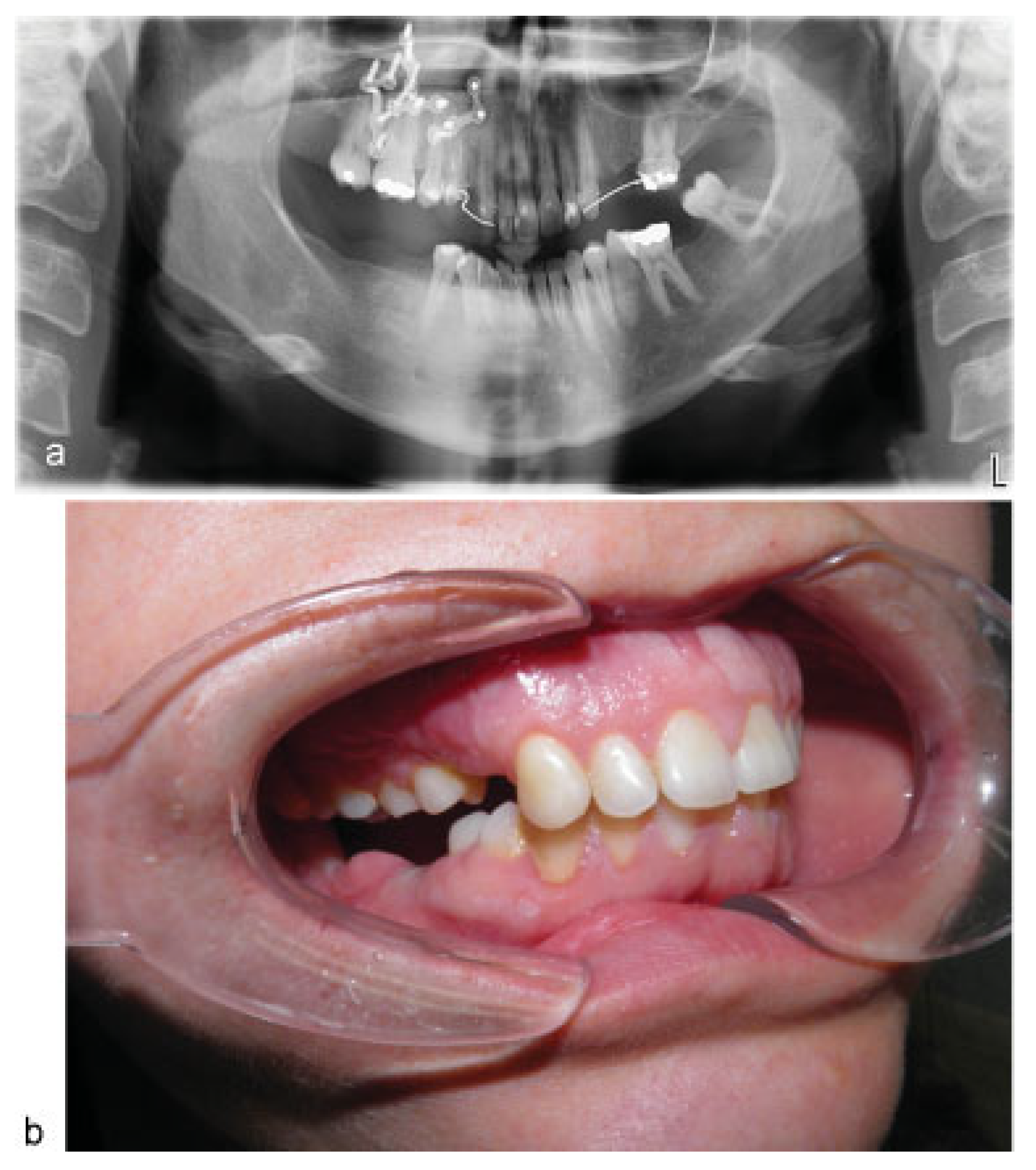
Given the consistency of the dysplastic bone, it was preferred to perform the osteotomy with the aid of piezo-surgery. Then placement of preshaped palatine plaque fixed with wires and a lower movable bite was performed. Synthesis of the bony fragment to the new location with three plates and screws was followed by suture of the surgical incision and pressure dressing to reduce postoperative bleeding. Intraoperatively, it was possible to place a removable prosthesis in the lower molar region (
Figure 4a,b). Bone fragments from the zygomatic region were also taken for histologic examination. The histologic diagnosis was osseous tissue with irregular and twisted trabecular bone structure and some osteoblastic flanges, mainly coexisting with compact lamellar bony tissue referable to cortical bone. The report was compatible with “fibrous dysplasia”. The postoperative course of the patient was regular with complete healing of the mucosa after 24 months (
Figure 5a,b).
Discussion
FD is a developmental tumor-like disease having characteristics of replacement of the normal bone by excessively proliferated cellular fibrous connective tissue intermixed with irregular bony trabeculae [
13]. FD may affect single (monostotic = MFD) or multiple (polyostotic = PFD) bones. MFD is called craniofacial fibrous dysplasia when it occurs adjacent to the craniofacial bones. However, CFD is a rare form of FD. Craniofacial involvement in CFD most commonly results in neurologic symptoms such as hearing loss, visual loss, headache, proptosis, and so forth [
14].
FD can be seen in children and young adults. MFD is equally distributed in both sexes and is six times more common than PFD. In the monostotic form, the maxilla is involved more than the mandible (max/mand = 2/1), and it occurs unilaterally at the posterior of the jaws [
13,
14,
15,
16,
17]. Three different radiographic patterns have been defined for FD: cystic (radiolucent or lytic), sclerotic, and mixed (radiolucent/radiopaque) [
13,
14]. Jaw lesions cause displacement of the teeth, loss of the lamina dura, narrowing of the periodontal ligament space, and, rarely, root resorption [
13,
14,
15]. Superior displacement of the mandibular canal is suggestive of FD [
14]. Nasal obstruction may occur if the paranasal sinuses are affected. Lesions extending to the orbit may cause visual impairment and temporal bone lesions may cause hearing loss. Facial pain, headaches, or facial numbness can develop.
Since it was first described in the 1930s, the only therapeutic possibility had been surgical management until the 1990s [
15]. Important insights into the pathophysiology of the disease have been gained over the last two decades, with a description of the mutated gene and the main abnormal biological pathways. Also, medical therapy with bisphosphonates has been developed.
The prognosis generally is good, although poor outcomes are more frequent in younger patients and in those with polyostotic forms of the disease [
16]. The risk of malignant transformation is a rare but established complication. It should be considered when recurrent or stable FB produces pain or soft tissue extension or neurologic deficits. The most common malignant transformation reveals osteosarcoma followed by fibrosarcoma, chondrosarcoma, and giant cell sarcoma [
17].
Surgery is indicated for confirmatory biopsy, correction of deformity, prevention of pathologic fracture, and/or eradication of symptomatic lesions [
18]. Because of the benign nature of the condition, the surgery itself should be relatively conservative with the primary goal being preservation of existing function [
19]. The choice of surgical option depends on several factors: site of involvement, rate of growth, aesthetic disturbance, functional disruption, patient’s preference, and the general health of the patient.
Some authors have adopted conservative treatment for the alveolar part of the jaws, which are always treated with shaving [
16,
17]. Valentini et al. proposed radical removal of the alveolar bone involved by CFD with immediate reconstruction using revascularized or free bone graft [
7].
There have been controversies in bone grafting and the use of common internal fixation devices (plates and screws). Some researchers argued that these procedures were almost always doomed to early failure [
18], others thought reconstruction after excision was important in the management of craniofacial FD and recommended grafts of calvarial bones and ribs, while still others suggested the use of cortical grafts rather than cancellous grafts or bone-graft substitutes because of the superior physical qualities of remodeled cortical bone [
19].
Conclusions
Although FB is a benign hamartomatous growth, it can lead to severe deformity and functional alterations of the involved sectors. The treatment of choice varies depending on the affected region. For the orbital region and the regions with dental elements, the surgical treatment must be conservative (remodeling and/or limited resections) in agreement with Ray Chen. In the reported case the dysplasia involved the right hemiface and hemi-maxillary bone. Because the patient was also edentulous in the right mandible, all the alveolar processes with the dental elements were completely collapsed until the lower gum, completely eliminating the space for prosthetic rehabilitation. After the examinations, treatment consisted of orbital-zygomatic bone remodeling and a vertical resection of the maxillary bone using the Schuchardt-Kufner technique. This permitted a good reduction in the dysplastic orbital and intermaxillary tissue, the conservation of dental elements, as well as the lifting of all the right alveolar process (~2 cm) to make the necessary room for prosthetic rehabilitation. Two years after the surgery, the patient’s condition is stable with a suitable prosthesis of the lower posterior teeth.