Abstract
Ectopic molars within the mandibular ramus/condyle unit, although rare, present a unique challenge to the surgeon. Multiple approaches have been described in the literature for their removal. A review of the English literature on the subject of and surgical techniques was completed. In addition, a case report is presented of an ectopic mandibular molar in the mid-ramus region which was removed via a minimally invasive, intraoral, technique combining the use of endoscopy and piezoelectric surgery. The authors advocate this technique as it offers the following advantages: avoidance of injury to branches of the facial nerve, unaesthetic scars, and sialocele formation; maximization of surgical field visualization with limited dissection; ability for safe sectioning of the tooth with minimal risks to adjacent structures; and precise bone removal, reducing the risk of iatrogenic or postoperative mandible fracture.
Impacted mandibular third molars are a common condition usually located between the second molar and anterior border of the ramus. Ectopic mandibular third molars, although a rare occurrence, have been described as being located in the ascending ramus, in the coronoid process, near the sigmoid notch, and within the mandibular condyle.1 This study provides a review of the literature from 1950 to present day to evaluate reported cases of the ectopic mandibular third molars within the ramus/condyle unit, indications for removal, surgical approaches, and techniques. Additionally, a report of a case by the current authors is presented to emphasize a minimally invasive technique combining endoscopy and piezoelectric surgery.
Methods and Materials
A PubMed search was completed including articles from January 1950 to present day using the key words “ectopic molar.” A total of 625 articles were generated. Inclusion criteria for the study are as follows: articles describing a case of a patient presenting with an ectopic mandibular molar located in the condylar ramus unit, which was defined as posterior to the anterior border of the mandibular ramus, and at or above the level of the mandibular plane of occlusion. The 28 articles which met inclusion criteria were then evaluated to assess the following criteria: patient demographics, tooth location, symptoms/association with pathology, surgical indications/techniques, and complications. Tooth location within the condylar ramus unit was subdivided into five categories: intracondylar, subcondylar, coronoid, sigmoid notch, and mid-ramus as depicted in Figure 1.
Results
The 28 articles which met the inclusion criteria are summarized in Table 1 [1–28]. In these 28 articles, 31 patients with 32 separate ectopic molars are described.
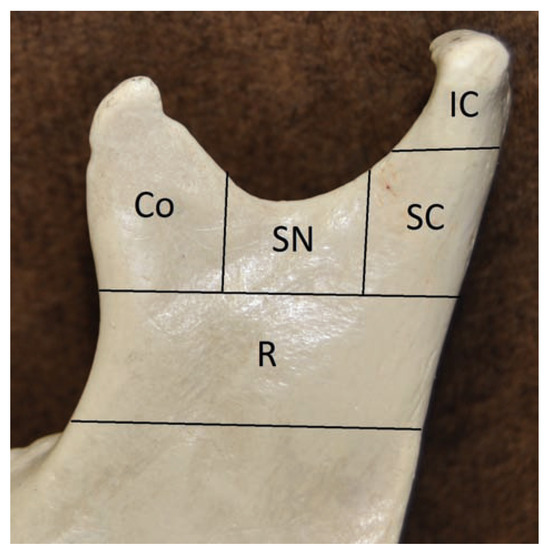
Figure 1.
The mandibular ramus/condyle unit and its divisions are depicted. Co, coronoid; IC, intracondylar; R, mid-ramus; SC, subcondylar; SN, sigmoid notch.
Patient Demographics/Presenting Symptoms
The mean age of patients was 46 years with the youngest being a 9-year-old and the oldest being 68-years-old. The majority were female (61%) and presented with symptoms (90%) including pain, facial swelling, trismus, and purulent drainage.
Ectopic Molar Location/Association with Pathology
Forty-four percent of the molars were located in the subcondylar region, 18.7% were located in the sigmoid notch region, and 12.5% were located in each of the intracondylar, ramus, and coronoid regions. Fifty-nine percent of the ectopic molars were associated with radiolucent lesions and most were confirmed histologically as dentigerous cysts.
Surgical Treatment/Approaches
Treatment approaches were nearly equal between intraoral approaches and extraoral approaches. Fifty-two percent of teeth that were removed were done so via intraoral approaches and 48% were removed extraorally. Three teeth were not removed. Of the three teeth not removed, two were asymptomatic with no associated pathology. The other was not removed as it was determined not to be the source of the patient’s symptoms. Instead, parotid sialadenitis was deemed the source of this patient’s symptoms and a partial parotidectomy was completed [26].
Seventy-one percent of teeth located in the subcondylar region were removed via extraoral approaches. 100% of the sigmoid notch located teeth were removed via an intraoral approach, and two-thirds of the intracondylar located teeth were removed via extraoral approaches. Lastly, for both the coronoid and mid-ramus regions, three-fourths of the teeth removed were done via intraoral approaches.
Two of the reported intraoral cases were completed with endoscopic assistance. One of these teeth was located in the intracondylar and the other was located in the coronoid region.
Complications
The one reported complication was extraoral scarring. In addition, two cases which used extraoral approaches reported temporary CNVII weakness, and one of the intraoral approaches reported temporary lingual/inferior alveolo nerve (IAN) paresthesia.
Report of a Case
A 51-year-old man with a symptomatic, ectopically located mandibular fourth molar was referred by the ENT (Ear Nose Throat) service to the division of Oral and Maxillofacial Surgery (OMFS). The patient had developed left facial swelling, trismus, and dysphagia in December 2015, and was initially evaluated by his general dentist who made an initial diagnosis of a left parotid stone, giving rise to acute sialadenitis. He was started on antibiotics and referred to the ENT service. Examination revealed a diffusely swollen and tender parotid region. No purulence was able to be expressed from Stenson duct. A working diagnosis was made; the patient was continued on antibiotics, and given recommendations for hydration, parotid massage, warm compresses, and sialagogues. There was no improvement at 1 week follow-up. Computed tomography (CT) of the head and neck was obtained which noted a cystic lesion in the left mandibular ramus with an associated impacted tooth. The patient was then referred for evaluation and treatment.
At the time of presentation to the OMFS clinic, the majority of swelling and symptoms had resolved, but he reported persisting numbness in his left lower lip and chin. CT scan (Figure 2) revealed a unilocular, radiolucent lesion associated with an impacted fourth molar closely approximated to the lingula. This was felt to be the source of the symptoms and removal of the tooth and associated cyst was indicated. To provide the most minimally invasive and atraumatic technique, an endoscopic-assisted intraoral approach with a piezoelectric hand piece was planned. Of note, the decision was made not to treat the symptomless teeth on the right side.
Procedure: An approach to the left ramus was completed with a left retromolar incision, as used for a sagittal split osteotomy. Subperiosteal dissection was performed to create an optical cavity. A 30-degree endoscope was used to visualize the position of the impacted tooth on the lateral aspect of the ramus, and a piezo surgery unit was used to create a cortical window around the tooth (Figure 3). The tooth was exposed (Figure 4). The crown and roots were divided with the piezo surgery unit and delivered (Figure 5). The cystic lining was identified and removed while avoiding the IAN. The IAN was visualized and found to be intact (Figure 6).
Postoperative imaging showed the mandible to be intact and the tooth completely removed (Figure 7). Histopathological diagnosis confirmed a dentigerous cyst.

Table 1.
Summary of articles included from literature search.
Table 1.
Summary of articles included from literature search.
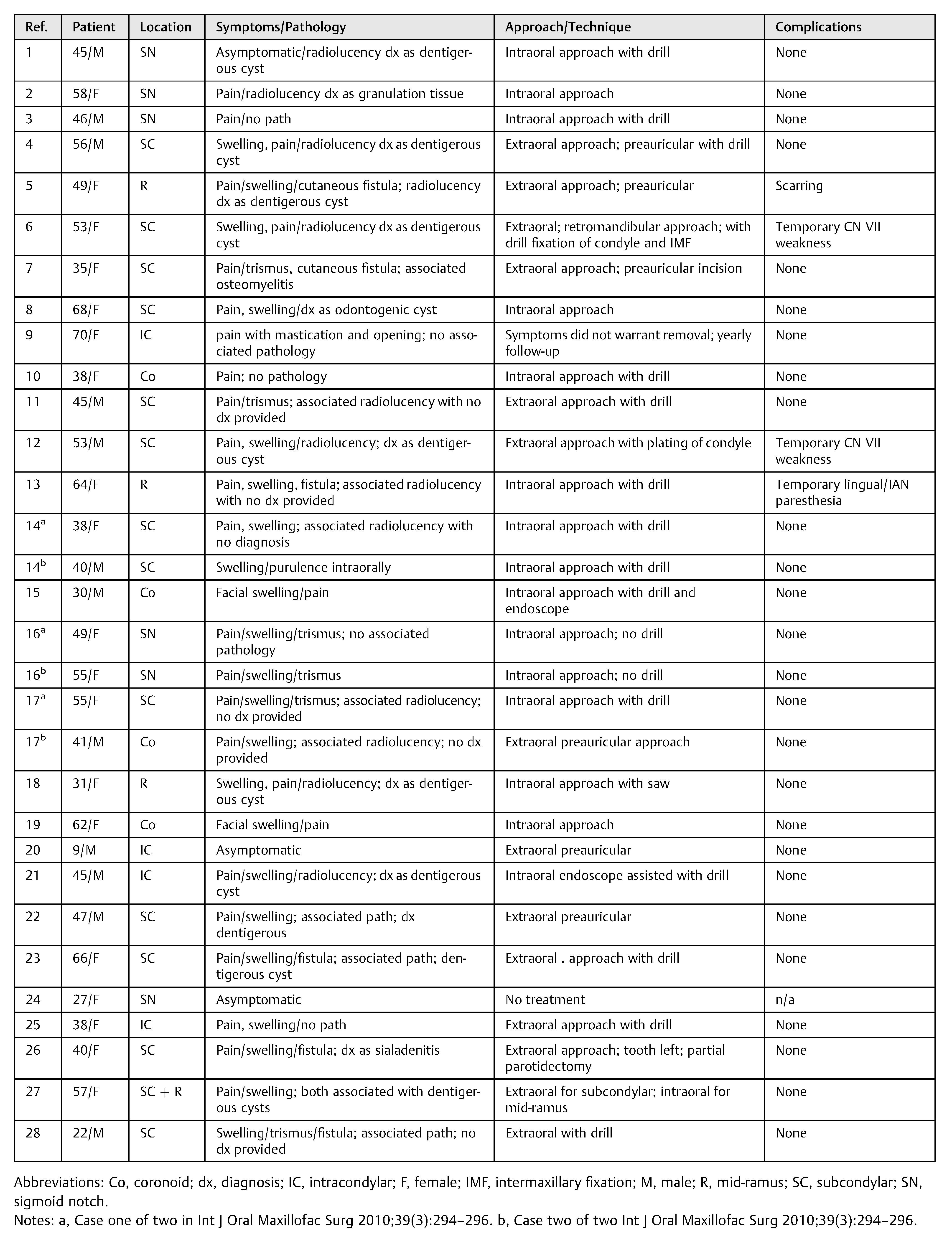 |
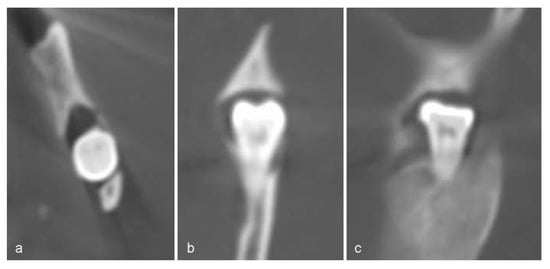
Figure 2.
Preoperative CT views. (a) Axial view illustrating lingual cortical perforation, (b) coronal view, (c) sagittal view illustrating close proximity lingula.
At initial follow-up, the patient reported improved mouth opening, decreased hypoesthesia, and pain. At 5-month follow-up, the patient fully regained function of the left IAN, pain had resolved, mouth opening was normalized, and an orthopantogram revealed complete bony fill in.
Discussion
A total of 32 total ectopic molars located in the mandibular ramus/condyle unit were reported in the English literature from 1950 to present day. There is the potential that these cases are under reported and therefore the prevalence remains unknown. Though rare, an ectopically located molar in the posterior mandible should be included in the differential diagnosis when a patient presents with facial swelling. In our case and the case reported by Scott et al [8], sialadenitis was misdiagnosed initially. Early imaging with an orthopantogram could aid in prompt diagnosis.
Possible causes of these ectopic molars have been debated in the literature and include trauma, infection, pathological conditions, crowding, and developmental anomalies [1]. All of these are plausible, but association with pathology, in particularly with dentigerous cysts, appears to be the most common. The majority of dentigerous cysts found in our search, as well as with our case, were small. One would think it would require a much larger cyst, almost occupying the entire ramus, to force a molar far into the posterior mandible. Thus, it has been proposed that the cysts found to be associated with these ectopic third molars may once have occupied the entire ramus and their walls may have been perforated which resulted in drainage and decompression [1,23]. This may have occurred in our case as the medial plate was noted to be perforated.
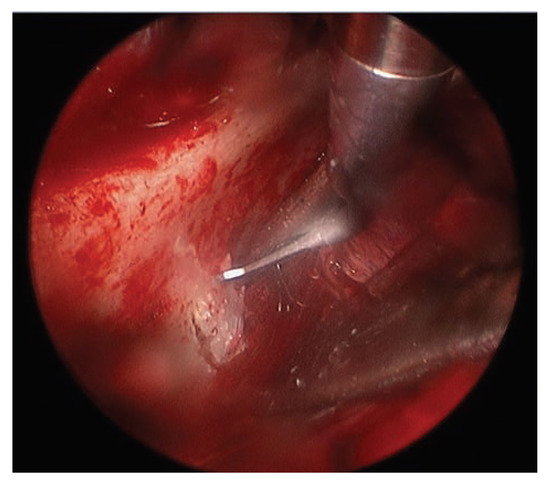
Figure 3.
Endoscopic view of the buccal corticotomy being initiated after localizing the ectopic molar position.
Once a tooth is diagnosed to be ectopic and is asymptomatic, regular follow-up and observation is mandatory to monitor any change in position, development of any pathology, and bone resorption [7]. Proposed indications for removal of ectopic molars include associated pathology, gross caries, infection, pain/trismus, and recurrent episodes of pain/swelling in the auricular region [7]. As with any surgery, the risks versus the benefits should ultimately be weighed. The risk of damaging neuronal structures and temporomandibular joint (TMJ) components, aesthetic concerns, bony defects after surgery, and the age of the patient should be evaluated before treatment [18].
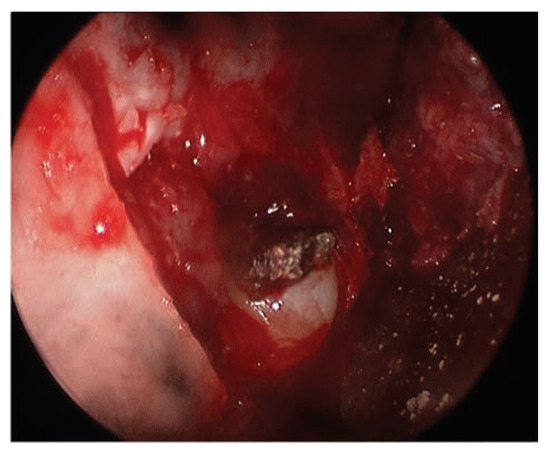
Figure 4.
Buccal corticotomy complete with tooth and cyst lining now exposed.
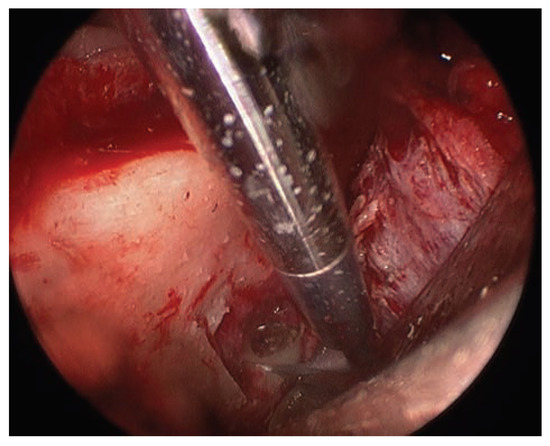
Figure 5.
Tooth being sectioned with piezo prior to removal.
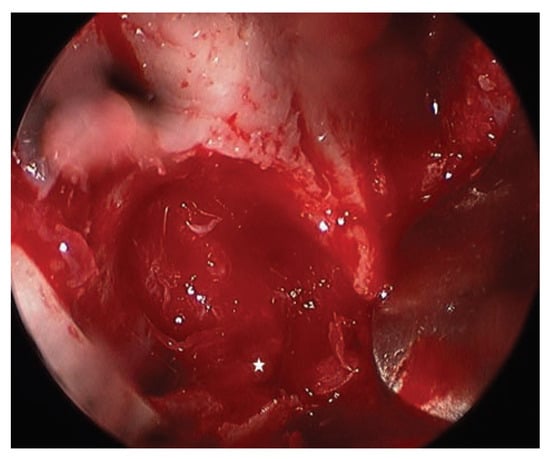
Figure 6.
Endoscopic view after the tooth and cyst lining were removed. Both the medial cortical perforation and IAN (*noted to be intact) are visualized.
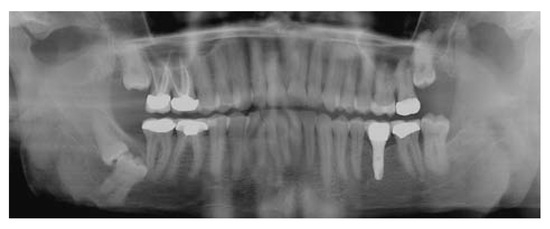
Figure 7.
Five-month postoperative Panorex shows complete bony fill of extraction site from left ramus.
Surgical approaches to removing ectopically erupted molars in the condylar ramus unit are nearly equally divided between intraoral and extraoral approaches. Although this literature review only provides a sample size of 32 teeth, trends can still be seen in regard to approaches based on specific locations. Extraoral approaches were preferred in the SC and IC regions, and the intraoral approach was favored for the Co, R, and SN regions. This trend would make sense, as the SC and IC areas are most difficult to visualize from an intraoral approach.
Not only will the position of the tooth influence the decision on a surgical approach, but surgeon preference and the need to minimize comorbidities are also taken into account. Extraoral approaches have been advocated, as they may provide better exposure of the surgical field, but they may result in complications such as scar formation, damage to TMJ components, and facial nerve injury [18]. In addition, extraoral approaches resulting in the parotid capsule being incised can lead to sialocele formation. Another reported advantage of the extraoral approaches is the ease to apply rigid fixation to prevent or treat iatrogenic fracture. Two reported cases of prophylactic fixation were noted with both molars located in the subcondylar region [[6.[12]. These authors thought the loss of some of the bony support in the condylar neck region would lead to an increased risk of fracture; therefore, when a tooth is in the subcondylar region, it may be prudent to prophylactically fixate the condyle to lower the risk of fracture.
The perceived disadvantage with intraoral approaches is the inability to achieve adequate access, exposure, and lighting to safely remove the tooth and verify complete removal of the associated pathology. This problem can be alleviated with the use of endoscopy. Endoscopy has been proven effective in providing good visualization and illumination, allowing complete eradication of cystic lining through smaller incisions [15]. The use of endoscopy to access the mandibular ramus/condyle unit has been previously described.15 To our knowledge, the case presented is the third case reported in the literature using endoscopy to aid with removal of an ectopic molar in the posterior mandible. In common with previous authors, we found that with minimal dissection we were able to achieve adequate visualization and illumination to achieve our surgical goals. We were able to delineate cystic lining and the IAN. This ensured the cyst was completely removed and then provided the ability to identify and protect the neurovascular bundle and confirm it was intact after completion of surgery.
In our case, with the tooth/cyst located directly against the lingula and being intimately associated with the inferior alveolar neurovascular bundle, we also chose to use the piezoelectric hand piece for bone removal and tooth division. Piezoelectric surgery has been indicated for all osteotomies in which respect to surrounding soft tissues is necessary to decrease the risk of damage to the most critical structures (nerves, vessels, and mucosa). The piezoelectric hand piece has the ability to recognize tissue hardness and cuts only on mineralized structures [29]. To our knowledge, this is the first reported case which combines the use of endoscopy and piezoelectric surgery to remove an ectopic molar located in the mandibular ramus/condyle unit. Its use allowed us to perform a precise ostectomy and safely section the tooth while avoiding injury to the neurovascular bundle and tissues medial to the lateral cortical perforation.
Conclusions
Ectopic mandibular third molars in the mandibular ramus/ condyle unit, although rare, should be included in the differential diagnosis of parotid/preauricular pain and or swelling. They can be readily identified with simple imaging, such as an orthopantogram. We report the first combined use of endoscopy and piezoelectric surgery to remove an ectopic molar in the mandibular ramus/condyle unit. This approach allows for intraoral access, with the advantage of avoiding injury to CNVII, unaesthetic scars, and sialocele formation. Endoscopy maximizes surgical field visualization with limited dissection, and the use of piezo surgery allows for safe sectioning of the tooth with minimal risks to adjacent structures, and precise bone removal reducing the risk of iatrogenic or postoperative mandible fracture.
References
- Fındık, Y.; Baykul, T. Ectopic third molar in the mandibular sigmoid notch: Report of a case and literature review. J Clin Exp Dent 2015, 7, e133–e137. [Google Scholar] [CrossRef] [PubMed]
- Adachi, M.; Motohashi, M.; Nakashima, M.; Ehara, Y.; Azuma, M.; Muramatsu, Y. Ectopic third molar tooth at the mandibular notch. J Craniofac Surg 2015, 26, e455–e456. [Google Scholar] [CrossRef]
- Lee, Y.K.; Park, S.S.; Myoung, H. Surgical extraction of mandibular third molar in pterygomandibular space: A case report. J Korean Assoc Oral Maxillofac Surg 2013, 39, 242–245. [Google Scholar] [CrossRef][Green Version]
- Bowman, J.; O’Regan, B.; Bhopal, S. Transmasseteric antero-parotid approach: A technique adaptation for ectopic subcondylar third molar removal and associated dentigerous cyst enucleation. Br J Oral Maxillofac Surg 2014, 52, e7–e8. [Google Scholar] [CrossRef] [PubMed]
- Sanghera, R.K.; Jones, J. Parotid fistula–an extra-orally draining infected dentigerous cyst associated with a supernumerary fourth molar in ascending ramus. Dent Update 2013, 40, 343–345. [Google Scholar] [CrossRef]
- Iglesias-Martin, F.; Infante-Cossio, P.; Torres-Carranza, E.; PratsGolczer, V.E.; Garcia-Perla-Garcia, A. Ectopic third molar in the mandibular condyle: A review of the literature. Med Oral Patol Oral Cir Bucal 2012, 17, e1013–e1017. [Google Scholar] [CrossRef] [PubMed]
- Lambade, P.; Lambade, D.; Dolas, R.S.; Virani, N. Ectopic mandibular third molar leading to osteomyelitis of condyle: A case report with literature review. Oral Maxillofac Surg 2013, 17, 127–130. [Google Scholar] [CrossRef]
- Scott, N.; Bater, A.; Wilson, A. An unusual cause of a facial swelling. J Surg Case Rep 2012, 2012, 10. [Google Scholar] [CrossRef]
- Kim, J.S. Cone beam computed tomography findings of ectopic mandibular third molar in the mandibular condyle: Report of a case. Imaging Sci Dent 2011, 41, 135–137. [Google Scholar] [CrossRef]
- Procacci, P.; Albanese, M.; Sancassani, G.; Turra, M.; Morandini, B.; Bertossi, D. Ectopic mandibular third molar: Report of two cases by intraoral and extraoral access. Minerva Stomatol 2011, 60, 383–390. [Google Scholar]
- Shivashankara, C.; Manjunatha, B.S.; Tanveer, A. Ectopic mandibular third molar in subcondylar region: Report of a rare case. Oral Maxillofac Surg 2012, 16, 153–155. [Google Scholar] [CrossRef]
- Pace, C.; Holt, D.; Payne, M. An unusual presentation of an ectopic third molar in the condylar region. Aust Dent J 2010, 55, 325–327. [Google Scholar] [CrossRef] [PubMed]
- Bortoluzzi, M.C.; Manfro, R. Treatment for ectopic third molar in the subcondylar region planned with cone beam computed tomography: A case report. J Oral Maxillofac Surg 2010, 68, 870–872. [Google Scholar] [CrossRef] [PubMed]
- Gadre, K.S.; Waknis, P. Intra-oral removal of ectopic third molar in the mandibular condyle. Int J Oral Maxillofac Surg 2010, 39, 294–296. [Google Scholar] [PubMed]
- Sembronio, S.; Albiero, A.M.; Zerman, N.; Costa, F.; Politi, M. Endoscopically assisted enucleation and curettage of large mandibular odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009, 107, 193–196. [Google Scholar] [CrossRef]
- Kupferman, S.B.; Schwartz, H.C. Malposed teeth in the pterygomandibular space: Report of 2 cases. J Oral Maxillofac Surg 2008, 66, 167–169. [Google Scholar]
- Salmerón, J.I.; del Amo, A.; Plasencia, J.; Pujol, R.; Vila, C.N. Ectopic third molar in condylar region. Int J Oral Maxillofac Surg 2008, 37, 398–400. [Google Scholar] [CrossRef]
- Wang, C.C.; Kok, S.H.; Hou, L.T.; et al. Ectopic mandibular third molar in the ramus region: Report of a case and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008, 105, 155–161. [Google Scholar] [CrossRef]
- Wong, Y.K.; Liew, J.C.; Tsui, S.H.; Cheng, J.C. Ectopic molar near the coronoid process: Case report. Quintessence Int 2007, 38, 597–600. [Google Scholar]
- Silva, G.C.; Silva, E.C.; Gomez, R.S. Migration of an unerupted second molar to the condyle: Report of a case with sequential radiographs. J Oral Maxillofac Surg 2007, 65, 570–572. [Google Scholar] [CrossRef]
- Suarez-Cunqueiro, M.M.; Schoen, R.; Schramm, A.; Gellrich, N.C.; Schmelzeisen, R. Endoscopic approach to removal of an ectopic mandibular third molar. Br J Oral Maxillofac Surg 2003, 41, 340–342. [Google Scholar] [PubMed]
- Tümer, C.; Eset, A.E.; Atabek, A. Ectopic impacted mandibular third molar in the subcondylar region associated with a dentigerous cyst: A case report. Quintessence Int 2002, 33, 231–233. [Google Scholar]
- Bux, P.; Lisco, V. Ectopic third molar associated with a dentigerous cyst in the subcondylar region: Report of case. J Oral Maxillofac Surg 1994, 52, 630–632. [Google Scholar]
- Chongruk, C. Asymptomatic ectopic impacted mandibular third molar. Oral Surg Oral Med Oral Pathol 1991, 71, 520. [Google Scholar] [PubMed]
- Yusuf, H.; Quayle, A.A. Intracondylar tooth. Int J Oral Maxillofac Surg 1989, 18, 323. [Google Scholar] [PubMed]
- Srivastava, R.P.; Singh, G. An unusual impacted inverted molar in mandibular condyle with preauricular sinus (a case report). J Indian Dent Assoc 1982, 54, 67–69. [Google Scholar]
- Burton, D.J.; Scheffer, R.B. Serratia infection in a patient with bilateral subcondylar impacted third molars and associated dentigerous cysts: Report of case. J Oral Surg 1980, 38, 135–138. [Google Scholar]
- Schwimmer, A.; Keaveny, J.T.; Caponigro, C.; Ragaini, V.E. Subcondylar impaction of a third molar resulting in chronic preauricular sinus: Report of case. J Oral Surg 1972, 30, 41–44. [Google Scholar]
- Robiony, M.; Polini, F.; Costa, F.; Sembronio, S.; Zerman, N.; Politi, M. Endoscopically assisted intraoral vertical ramus osteotomy and piezoelectric surgery in mandibular prognathism. J Oral Maxillofac Surg 2007, 65, 2119–2124. [Google Scholar]
© 2017 by the author. The Author(s) 2017.