The exposure of the facial skeleton to injuries has alarmingly increased in India due to over population, poor road conditions, and increasing number of speedy automobiles. Among all bones of the facial skeleton, the zygoma and the mandible are highly accessible to the traumatic elements. In response to heavy forces, zygomatic bone gets separated from its neighboring bones at or near the respective sutures. “Zygoma” is a prominent bone in the face, when viewed frontally, semilaterally and laterally through bird’s eye and worm’s eye view. Term “zygoma” means a yoke which unites structures and is a major contributor to the orbit. The four articulations of zygoma with facial bones are of aesthetic significance in restoration of facial width and lateral projection and in treating maxillofacial trauma. These disarticulations may lead to fractures of zygomaticomaxillary complex (ZMC), zygomatic complex, or fractures of orbitozygomatic region. Sphenozygomatic junction was the important landmark with respect to zygomatic fractures reduction (especially in laterally displaced fractures). The alignment of the zygoma with the greater wing of the sphenoid in the lateral orbit is critical for determining adequate reduction of zygomatic fractures. ZMC fractures are associated with orbital volume change. Surgical reduction of the three points that makes up the buttresses also helps ensure proper alignment of the zygoma and proper reduction of other facial fractures present.
Point fixation is done at frontozygomatic (FZ) suture and zygomaticomaxillary buttress: three-point fixation is done at FZ, zygomaticomaxillary buttress, and infraorbital rim; four-point fixation of zygoma has been advocated at FZ, zygomaticomaxillary buttress, infraorbital rim, and zygomatic arch; and five-point fixation will include phenozygomatic suture according to the latest fixation techniques. Though fixation is adequate and even if fixed in two points, other areas need to be explored for reduction. Sphenozygomatic suture, zygomatic arch, and infraorbital rim need expertise to explore the fracture. Fractures of zygomatic complex present challenges in diagnosis and reconstruction for maxillofacial surgeons.
Edema that rapidly sets in makes clinical examination difficult, since the physical findings are masked. Successful reductions are often difficult to evaluate clinically because of great amount of swelling. Numerous techniques have been described to reduce zygoma fractures. The position of the fragment is usually confirmed by palpation; however, digital exploration and crepitus are unreliable guide in some cases. The assessment of the treatment of zygomatic complex fractures has also been done by visualization methods such as computed tomography (CT), photographs, and radiographs. The photographic comparison of the face by frontal, profile, three-quarter, bird’s, and worms eye views are to be done. These are useful for determining the malar symmetry, position of the globe (enophthalmos, pupillary height), eyelid position and form, facial width, and obvious scars [
1].
Outcome for zygomatic fracture has been quantified using orbital volume as criteria since any deviation in volume can have detrimental effects on aesthetics. In a country like India where resources are limited, effective use of available technology is very important. Imaging modalities [
2] such as ultrasound [
3], cone beam CT (CBCT), and CT [
4] are used for intraoperative [
5] real-time visualization of closed reduction and helps decrease surgical complications. Notably, the C-arm fluoroscopy imaging technique is widely applied to the maxillofacial surgery for the true-to-original reconstruction. Conventional imaging techniques during surgery often present difficulties in positioning the patient and delay in printing the film which increases the operative time. Recently, the use of C-arm as an intraoperative imaging tool has facilitated optimal fracture site reduction, with a minimum amount of radiation exposure as compared with CT and has eliminated the need for postoperative radiographs. On the contrary, the paranasal sinus (PNS) view of the X-ray offers to assess these sutures by assessing the reduction of the zygomatic line, orbital line, maxillary line, and innominate line.
The aim of this article was to assess whether accurate reduction of ZMC fracture was possible using C-arm as an intraoperative imaging with limited surgical exposure.
Materials and Methods
Patients with isolated unilateral displaced ZMC fracture with orbital volume change are included in the study. Study was done for a time period of 1 year from September 2013 to September 2014 in Sri Ramachandra University, Chennai. All the patients had mid-facial trauma, acquired in road traffic accident. Among 248 trauma cases, 63 patients had zygomatic fractures.
As per exclusion and inclusion criteria, 20 patients were included in the study and 2 of them lost for follow-up. Hence, 18 patients (17 males and 1 female) underwent postoperative CT scan and orbital volume assessment. The patients’ age group range from 18 to 50 years (
Table 1).
Inclusion criteria are adult patients (patients with completed growth periods, older than 18 years) with unilateral displaced ZMC fractures (tetrapod fracture) with or without associated mandibular fractures.
Exclusion criteria are (1) patients with craniofacial anomalies, (2) bilateral displaced ZMC fractures, (3) patients with complete Le Fort II or Le Fort III fractures with bilateral change in orbital volume, (4) patients with ZMC fracture on one side and with contralateral optic nerve injury, (5) patients with ZMC fracture associated with naso-orbito-ethmoidal fractures, (6) patients with undisplaced ZMC fractures (not tetrapod fracture and no separation of bone fragments at sutural areas), (7) patients with monocular or binocular diplopia, and (8) patient requiring orbital floor grafting. Of the 18 patients, 9 were included in the C-arm group and 9 in the control group randomly, with the help of Random allocation software by simple randomization (
Table 5).
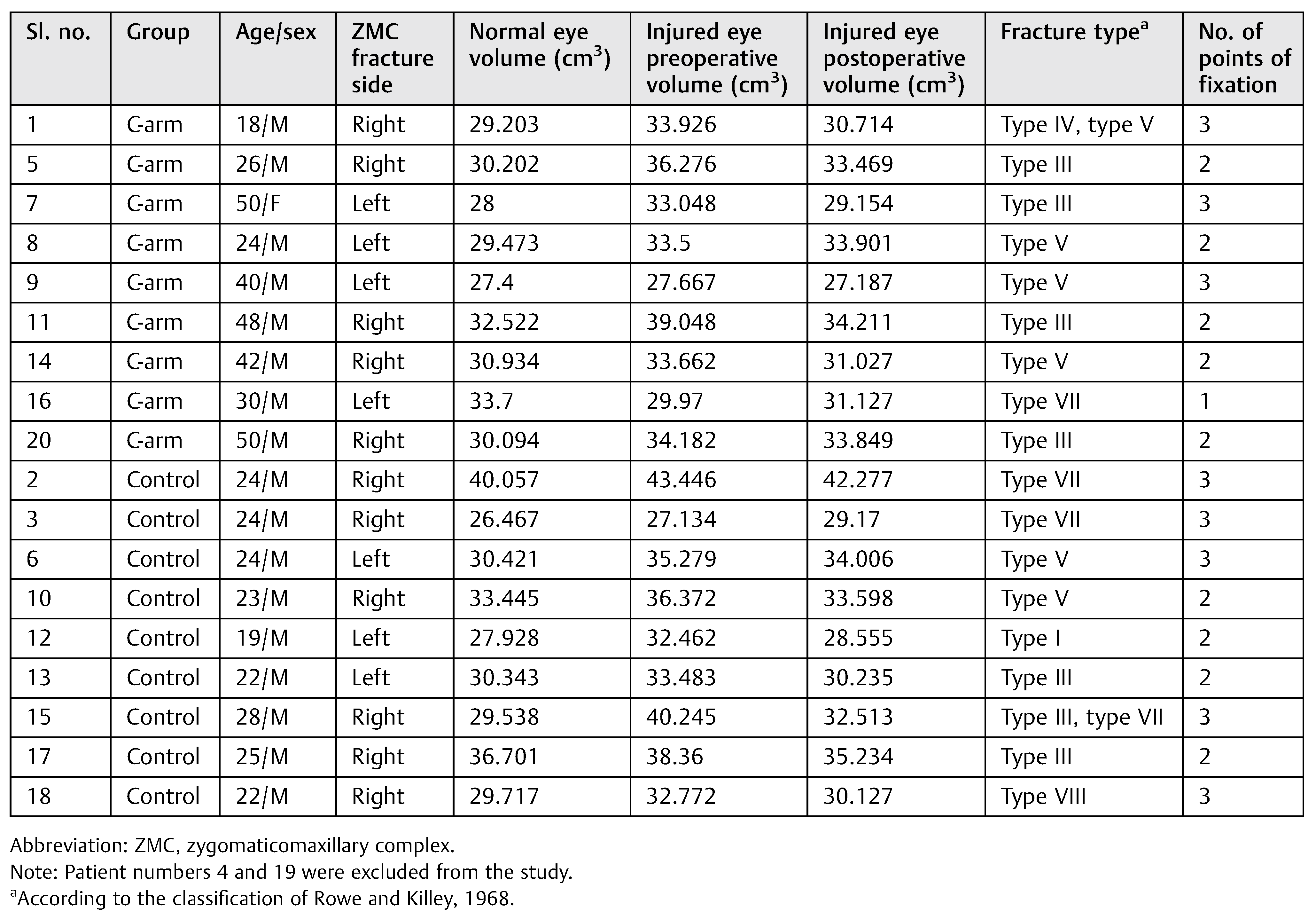
Figure 1.
Mapping the orbital content with marker in continuous axial, sagittal, coronal sections.
Figure 1.
Mapping the orbital content with marker in continuous axial, sagittal, coronal sections.
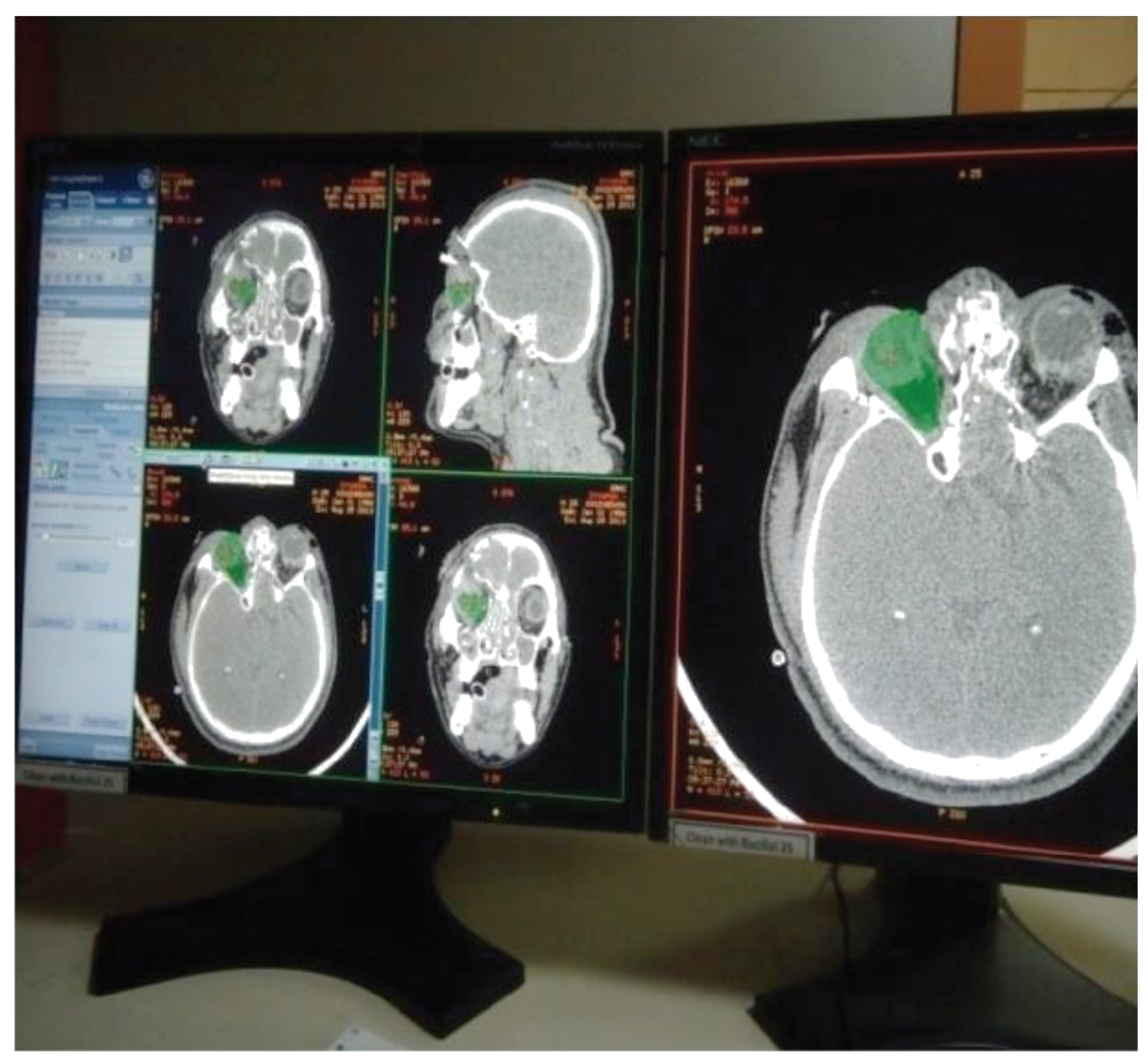
Figure 2.
Mapping the orbital content with marker in continuous axial, sagittal, coronal sections.
Figure 2.
Mapping the orbital content with marker in continuous axial, sagittal, coronal sections.
Based on preoperative orbital volume of both eyes assessed through three-dimensional CT, greater than 18 to 20% of orbital volume difference of injured orbit [
6] compared with normal eye and patients evident with orbital floor fracture with a defect were planned for exploration of orbital floor. A study was planned in which unilateral displaced zygomatic complex fractures were treated with intraoperative assessment of the reduction with C-arm. All patients were operated by same surgeon and the intraoperative procedure is as follows: Preoperative images (
Figure 6) were done with standardized settings (73 kV, 0.32 mA) of the C-arm to obtain images at 0 and 30 degrees (
Figure 7 and
Figure 8). The sutural contacts of zygoma were assessed and fracture segments were identified at 0-degree view and malar projection and zygomatic arch alignment at 30-degree view. An incision at frontozygomatic area and intraoral vestibular incision were given and fracture was reduced and the reduction was confirmed with C-arm (
Figure 9 and
Figure 10) at five mentioned areas and ZMC fracture [
7] was fixed at two or three points (
Figure 13). The continuity of the Dolan lines [
8] was used to confirm the reduction in the water view image displayed on the monitor (
Figure 11 and
Figure 12). The continuity of the innominate line helped in aligning the sphenozygomatic suture. If the surgeon feels that infraorbital rim continuity is not achieved on C-arm image, then infraorbital rim is exposed and fixation is done. By this way, unnecessary exploration of the infraorbital rim can be avoided and in cases where orbital floor exploration based on preoperative CT evaluation, exploration is done only after primary fixation and assessment by C-arm. Minimal exposure principle is followed. In the group of patients operated without intraoperative imaging, zygoma was assessed at three points and was reduced in the frontozygomatic suture region, zygomaticomaxillary buttress, and the infraorbital rim.
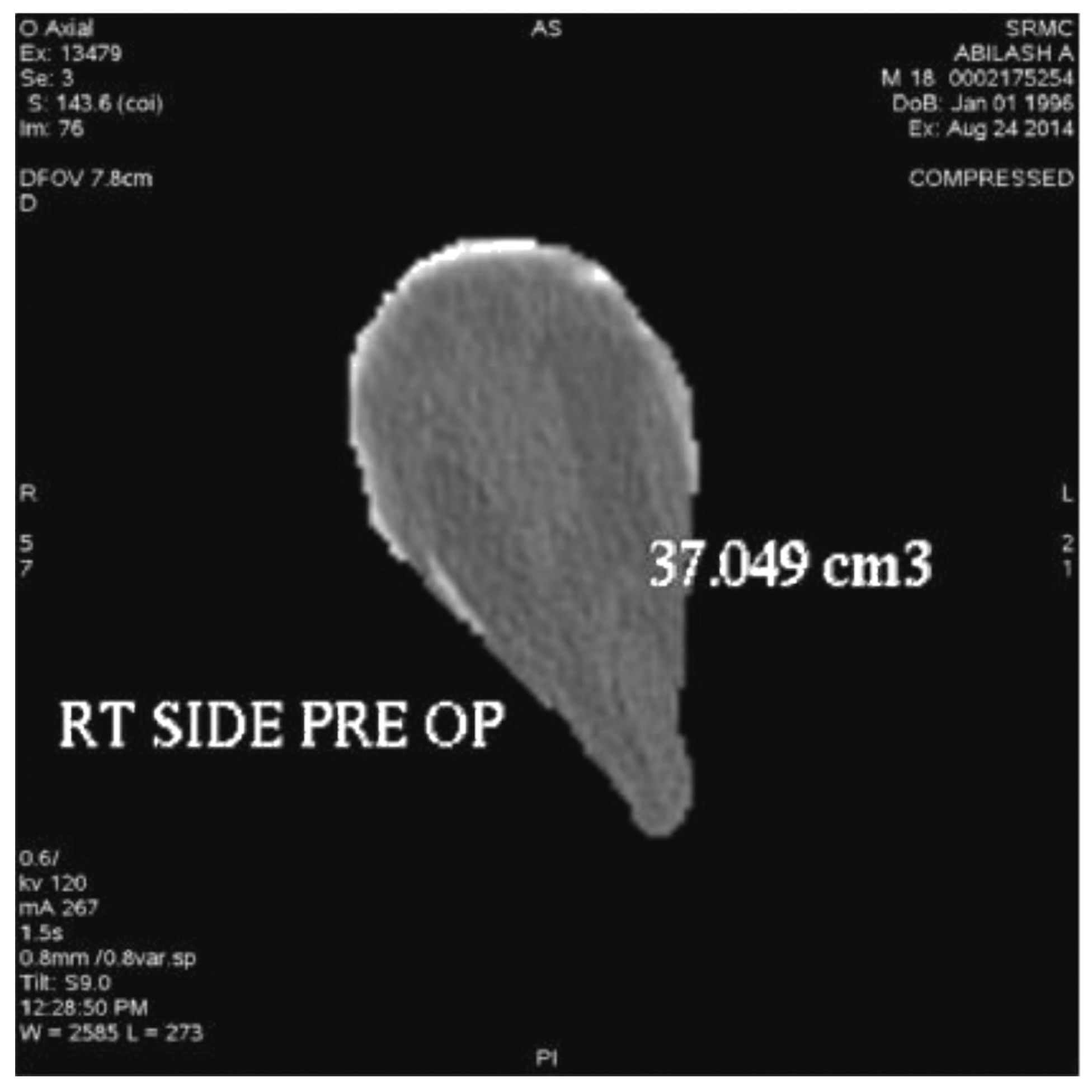
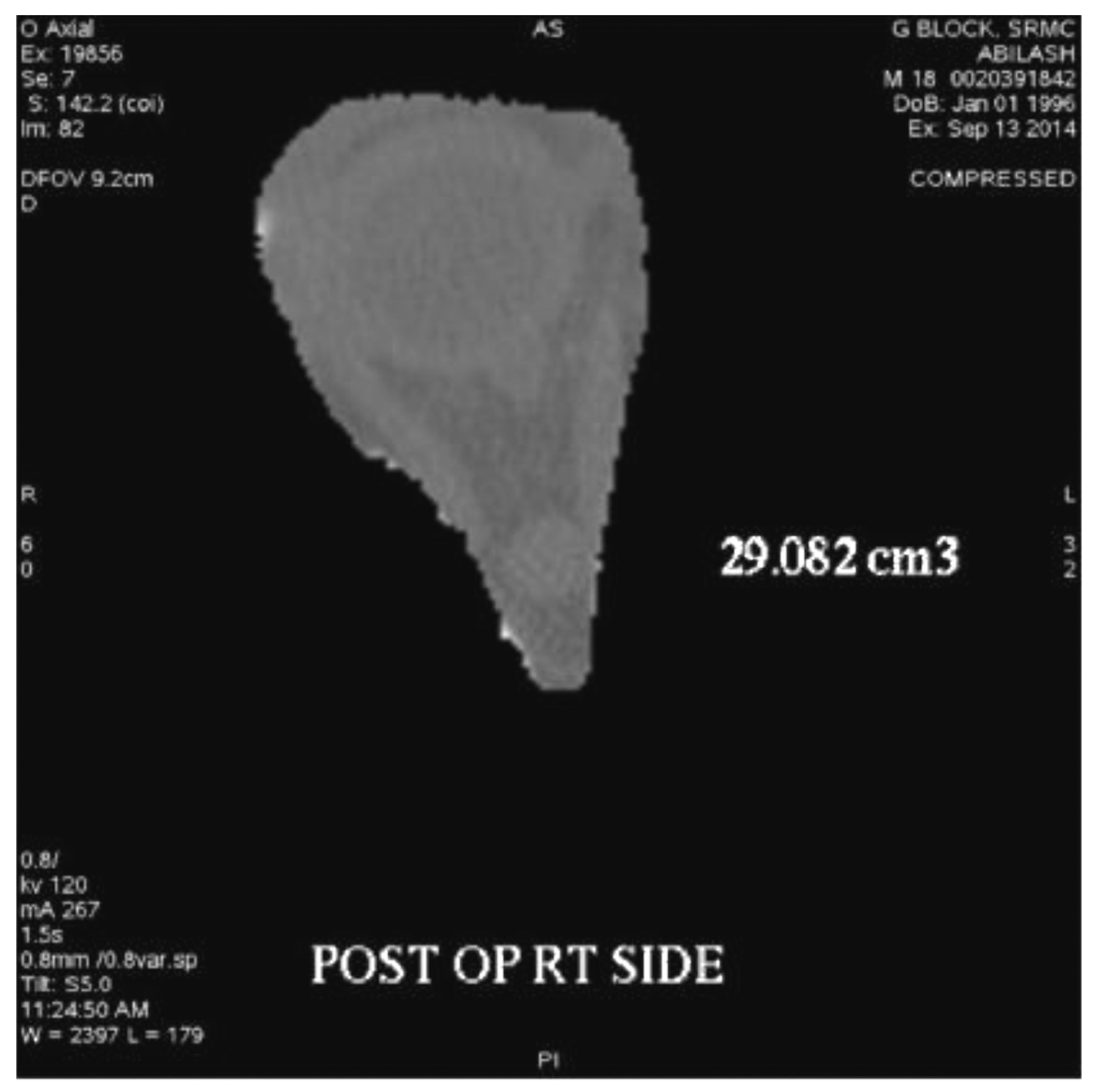
Figure 3.
Images showing output of orbital volume.
Figure 3.
Images showing output of orbital volume.
All patients were kept on standard postoperative regimen [
9,
10] of antibiotics and a repeat CTwas done after 2 weeks. The orbital volume was calculated virtually using advanced imaging software (volumetric computed tomography (CT-VCT) [
11] 64 slice XT console, 120 kV, 250 mA, and slice thickness with appreciation of 2 mm). The volume of the injured and the uninjured orbits were calculated and tabulated. Orbital volumes were assessed in postoperative CT scans and the change in volume was calculated and the restoration of orbital volume in both groups were calculated and tabulated.
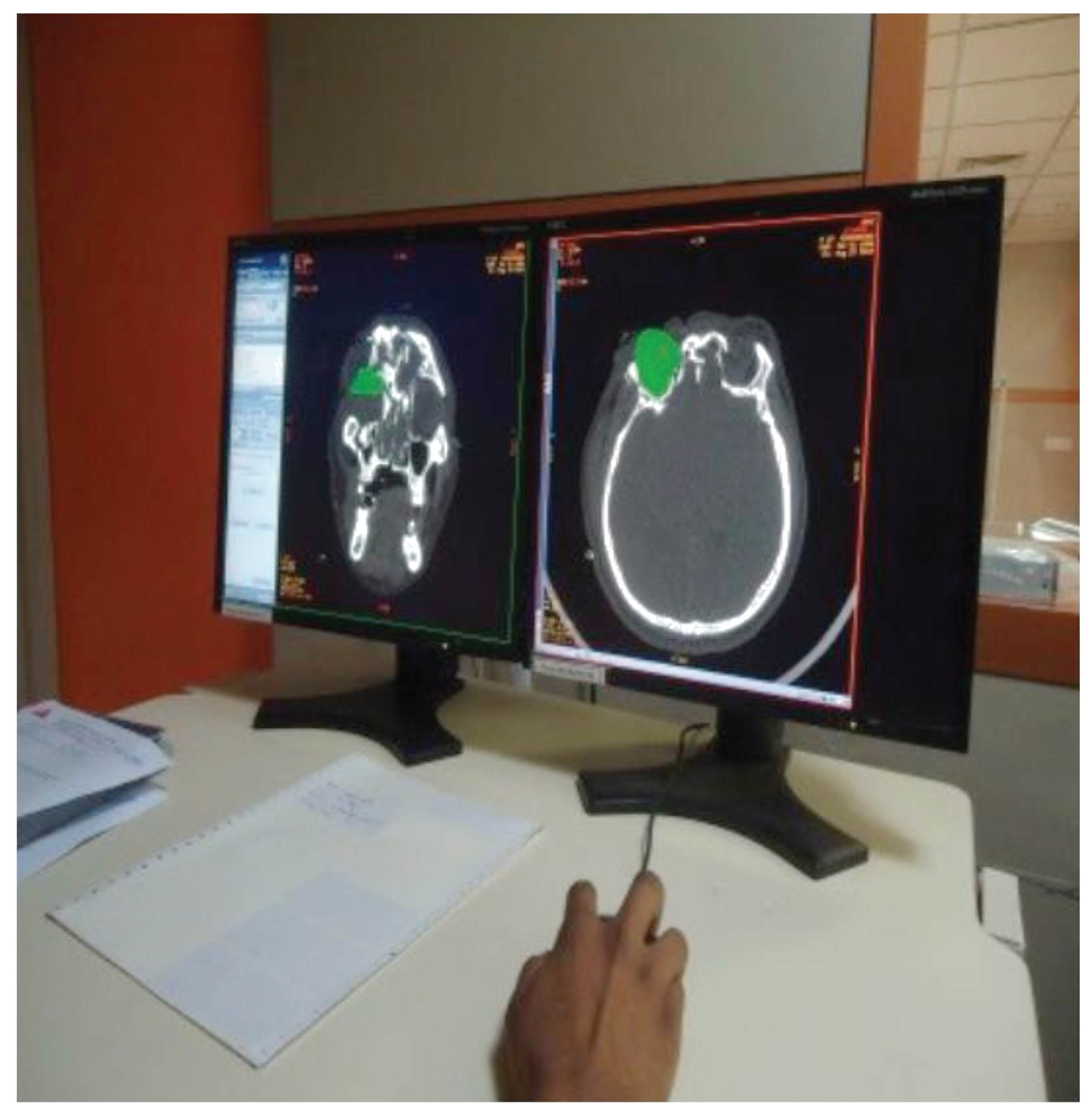
Figure 4.
Images showing output of orbital volume.
Figure 4.
Images showing output of orbital volume.
Figure 5.
Images showing output of orbital volume.
Figure 5.
Images showing output of orbital volume.
The preand postoperative change in the orbital volume of the affected side with nonaffected side was compared in both groups and measured to assess the better reduction of the fracture. The results were statistically analyzed using SPSS 15.0 for Windows Evaluation Version and for statistical significance, Student “t” test was applied.
Using CT-VCT 64 slice XT console, preand postoperative CT [
12] scans were done for the patients with 120 kV, 250 mA, and slice thickness with appreciation of 2 mm. Retro reconstruction was done at 0.625 mm in a bone window of window width 2,000 and window length 350: soft-tissue window of window width 300 to 350 and window length 100 in an advance workstation ADW 4.4. The anterior border of the orbital floor was determined using first CT slice and the posterior border is the apex of orbital cavity. Orbital volume [
13] is measured in axial, sagittal, and coronal sections (
Figure 1 and
Figure 2) by selecting mapping tool provided with the software of computer program, and orbital volume within the bony borders is mapped in every slice to calculate the orbital volume automatically displayed on the monitor (
Figure 3,
Figure 4 and
Figure 5) after the end of mapping.
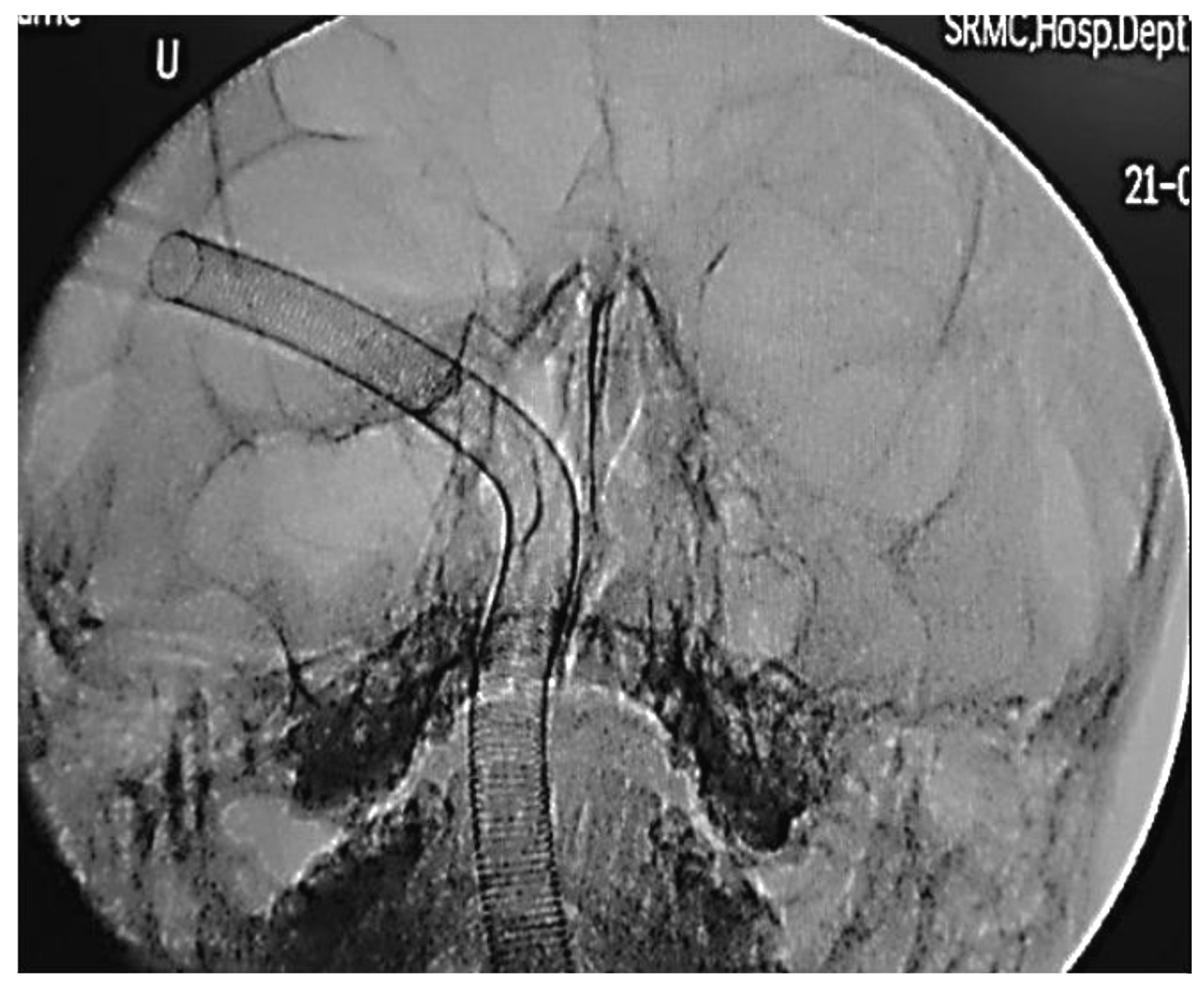
Figure 6.
Pre-operative CT-PNS image of a patient.
Figure 6.
Pre-operative CT-PNS image of a patient.
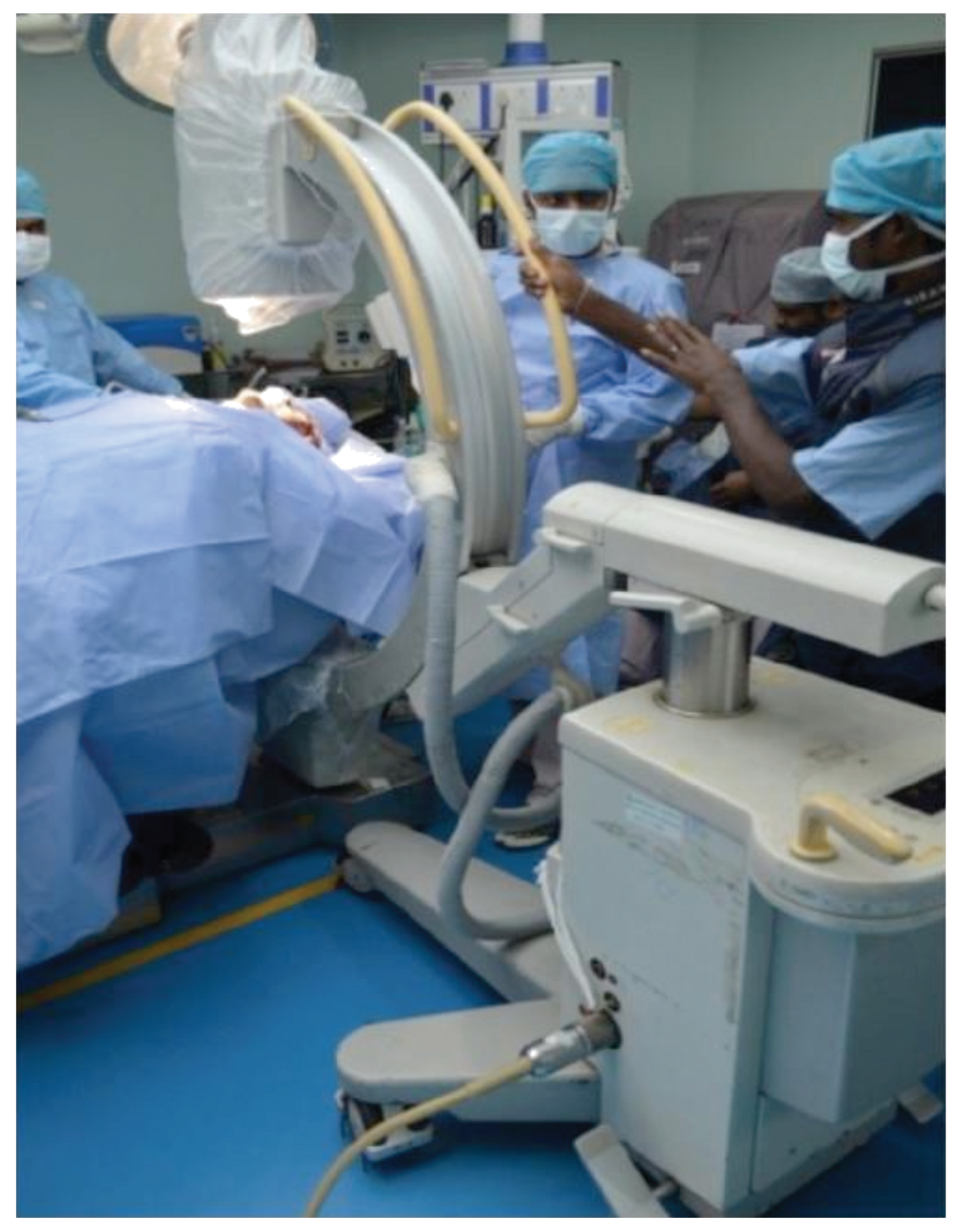
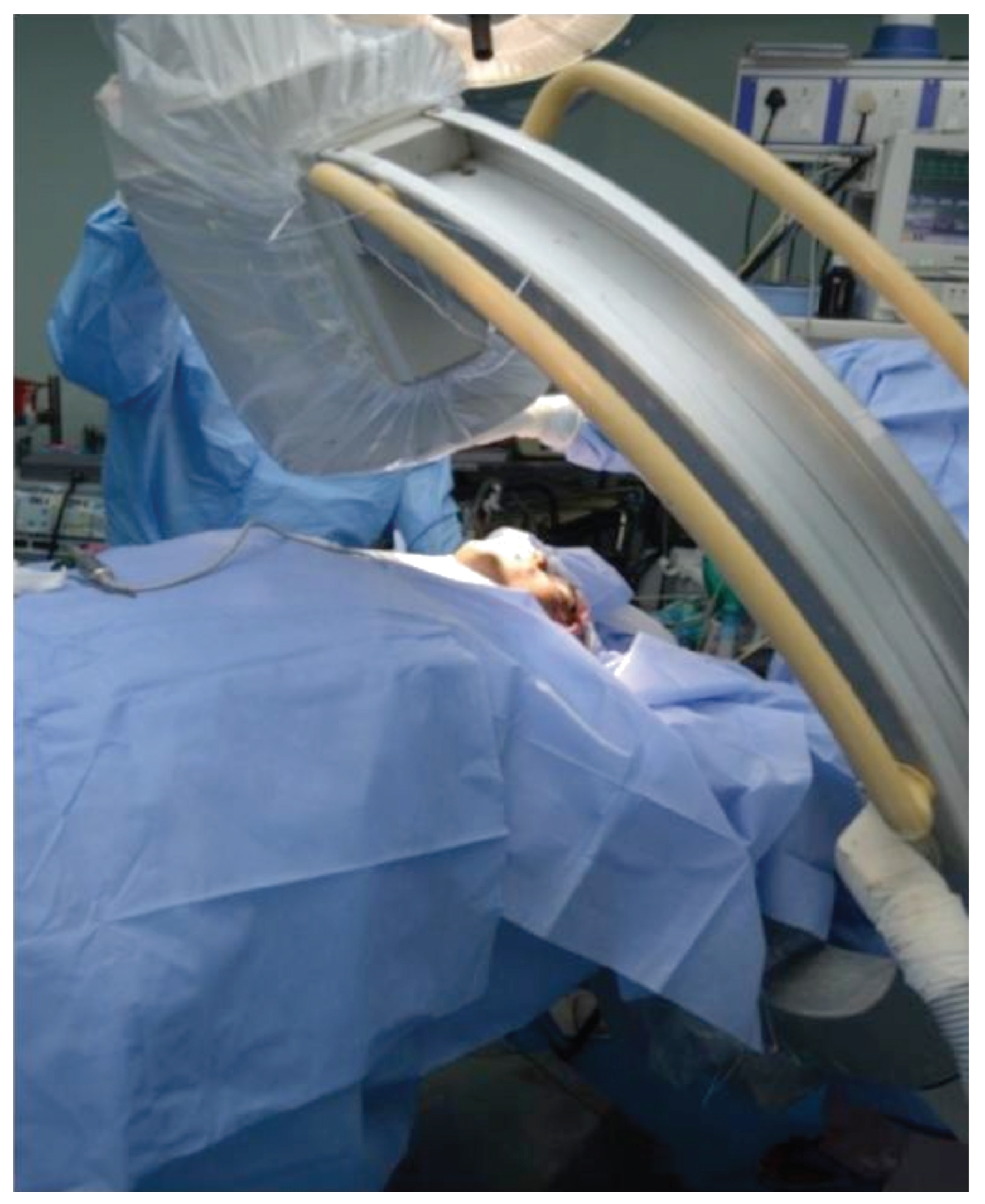
Figure 7.
Pre reduction C-arm alignment at 0°.
Figure 7.
Pre reduction C-arm alignment at 0°.
Figure 8.
Pre reduction C-arm alignment at 30°.
Figure 8.
Pre reduction C-arm alignment at 30°.
Figure 9.
Pre reduction C-arm image at 0°.
Figure 9.
Pre reduction C-arm image at 0°.
Patient was placed in anti-Trendelenburg position with neck in extended position. To minimize the magnification, the X-ray source was kept far away and intensifier kept close to patient’s vertex. The directions of X-rays are from chin to vertex appropriately at an angle of 5 degrees from menton to bregma in automatic pulsed fluoroscopy mode. Personal protective equipment such as lead aprons, thyroid collars, and Goggles were used.
Results
Here, the difference in orbital volume of injured eye and normal eye was calculated both preoperatively and postoperatively. We are interested to know that whether C-arm help in achieving the orbital volume of injured eye value as close as possible to value of uninjured eye.
Orbital volume of normal eye ranges from 26.47 to 40.05 cm
3. Orbital volume of injured eye preoperatively ranges from 27.134 to 43.446 cm
3. Change in orbital volume of injured eye with respect to normal eye preoperatively ranges from −3.73 to 10.707 cm
3. Orbital volume of injured eye postoperatively ranges from 27.187 to 42.277 cm
3. Change in orbital volume of injured eye with respect to normal eye after surgery ranges from −2.573 to 4.42 cm
3. Percentage of change in orbital volume of injured eye with respect to normal eye ranges from −7.63 to 15.06%. Percentage of orbital volume restored after surgery ranges from −7.7 to 10.7% in C-arm group and −3.43 to 26.15% in control group (
Table 2).
The difference in orbital volume (orbital volume of injured eye and uninjured eye) between two eyes can be negative in two situations, preoperative or postoperative. Preoperative negative values indicate inward displacement of fractured zygoma, whereas postoperative negative values indicate overreduction.
Figure 10.
Fracture ends before reduction.
Figure 10.
Fracture ends before reduction.
Patients included under C-arm group have a mean + standard error (SE) value of 11.614 + 2.26% of change in orbital volume of injured eye compared with normal eye preoperatively and a mean + SE value of 7.26 + 1.75% postoperatively. Percentage of restoration of orbital volume in C-arm group is noted to have a mean + SE of 4.34 + 2.08% with a standard deviation (SD) of 6.237%, and percentage of restoration of orbital volume in control group is noted to have a mean + SE of 9.9 + 2.80% with a SD of 8.42%. Our results shows that out of 18 patients, 3 patients (2 in C-arm group and 1 in control group) have negative values in percentage of orbital volume restored which shows that increase in orbital volume is seen in injured eye postoperatively rather than decreasing, in which overreduction of fractures is seen in postoperative CT scans.
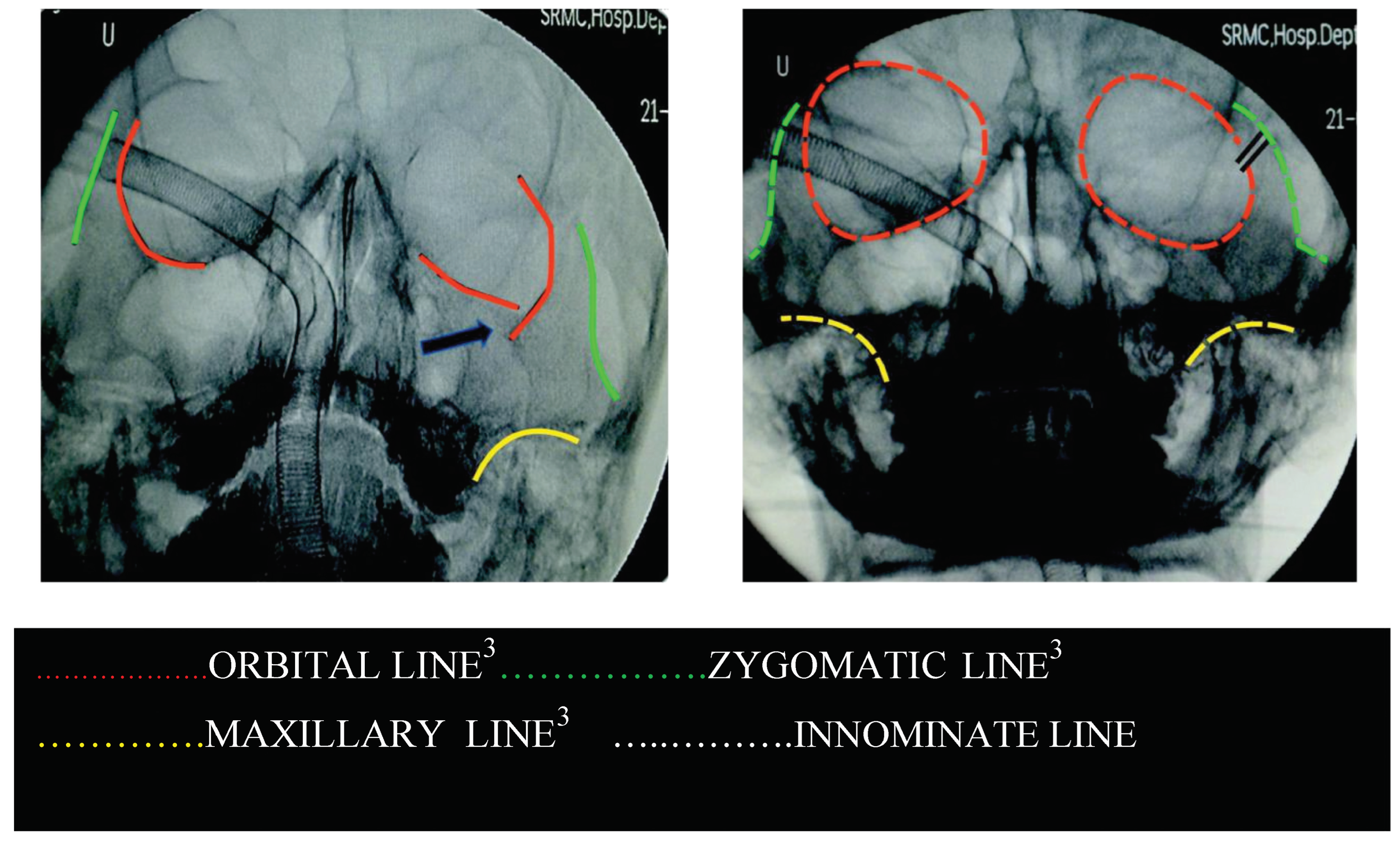
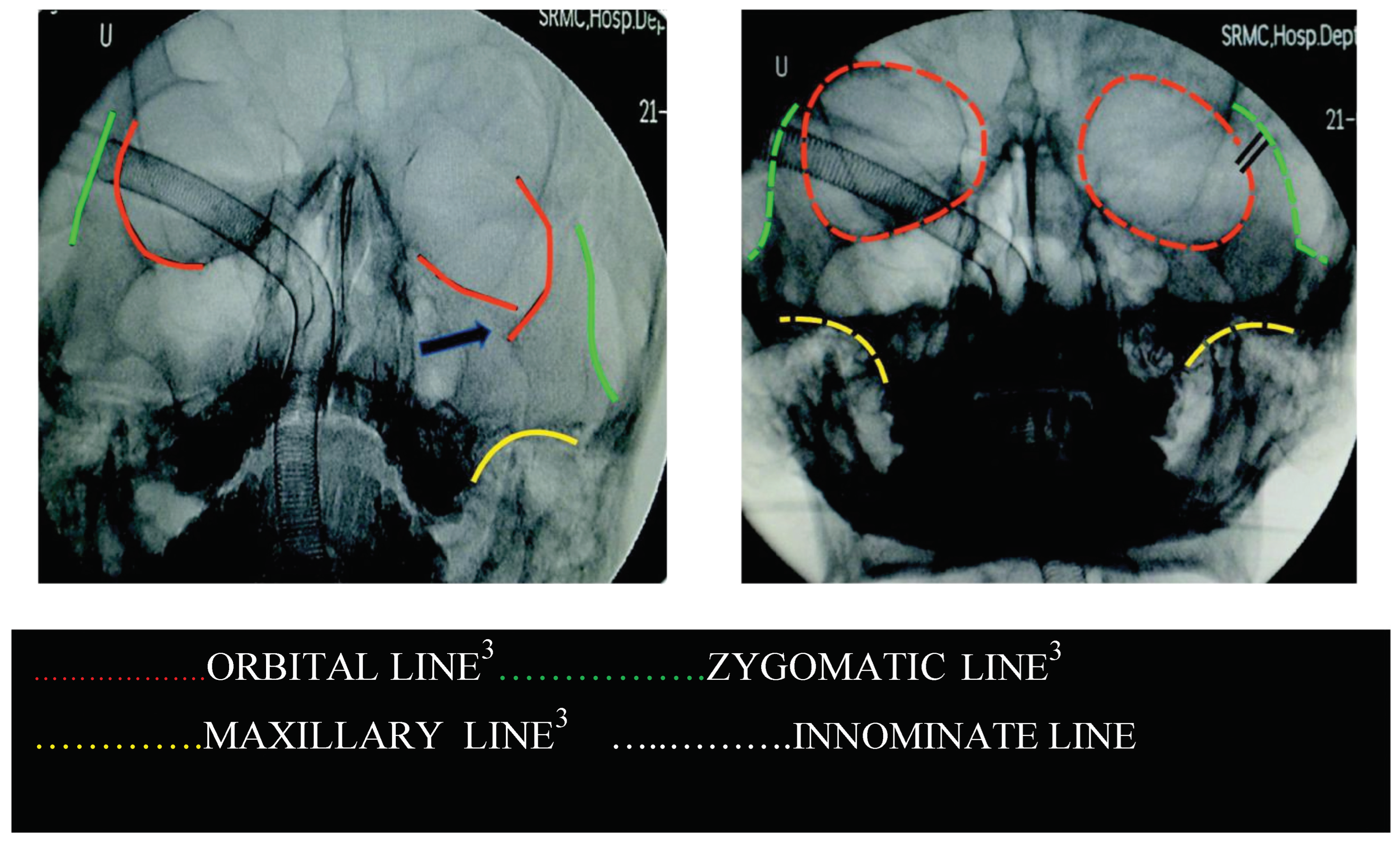
Figure 11.
C-arm image after reduction and before fixation.
Figure 11.
C-arm image after reduction and before fixation.
Figure 12.
C-arm image after fixation with markings.
Figure 12.
C-arm image after fixation with markings.
Figure 13.
Flowchart: Protocol of the study.
Figure 13.
Flowchart: Protocol of the study.
Discussion
C-arm [
14] (image intensifier) is used to check for reduction and alignment of fracture segments, aided with submentovertex projection provides excellent intraoperative control for reduction of ZMC fracture to achieve acceptable facial width. Image intensifiers exposes the patient and surgical team to radiation, but it is 60 to 80% less as compared with CT. Unfamiliarity can lead to difficulty in proper projection while patient is in supine position. Proper usage of intraoperative imaging reduces the need for secondary surgery for residual deformity and helps in eliminating operator-related error.
The study was done with an idea to expand the role of C-arm in oral and maxillofacial surgery by assessing few other uses in addition to assessment of zygomatic arches alone in midface that is by evaluating intraoperative use of C-arm in reduction of ZMC fracture. The concept of Dolan lines in association with C-arm has never been used. This is the first article to propose the role of Dolan lines and innominate line in C-arm PNS view image and submentovertex view. Fluoroscopy is evaluated by surgeons themselves. Comparison between C-arm group and control group was done by keeping in mind the stabilization principle of treating maxillofacial fractures as important criteria. C-arm is helpful to fulfill the criteria to treat tetrapod fractures of zygoma with minimal exposure by two-point fixation.
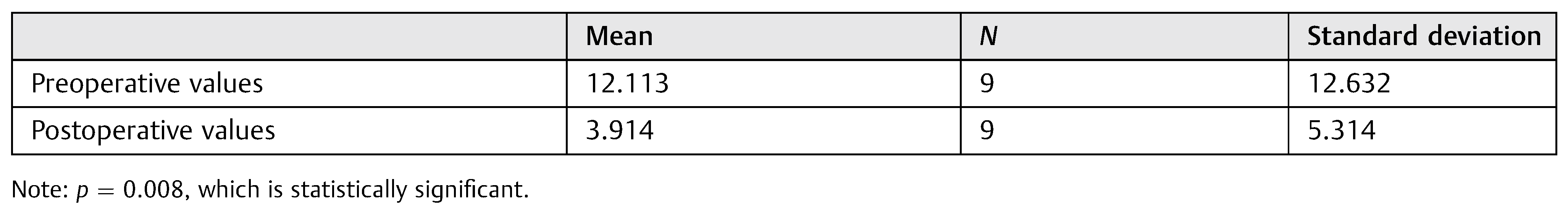
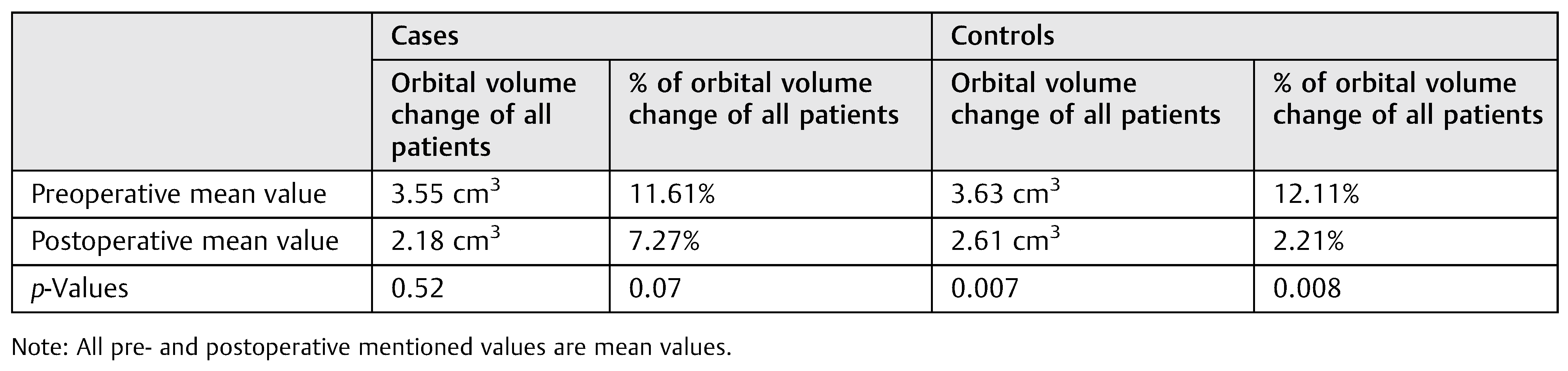
Table 2.
Comparison of preoperative and postoperative orbital volume change in percentages in control group using t-test.
Table 2.
Comparison of preoperative and postoperative orbital volume change in percentages in control group using t-test.
Table 3.
Mean orbital volumes of cases and controls.
Table 3.
Mean orbital volumes of cases and controls.
In our study, we used pulsed low-dose mode as described by Cho et al. [
15] to reduce the radiation absorbed doses.
We assessed the reduction in C-arm images with the help of Dolan lines which was first popularized by Dolan et al. [
16] We found that intraoperative C-arm is very useful to view innominate line and assess the proper reduction of ZMC fractures at the sphenozygomatic suture. As Gruss et al. [
17] proposed that zygomatic arch is the key in mid-facial fracture repair, in our study, zygomatic arch with malar prominence is assessed in every case at preoperative, intraoperative, and postreduction periods.
The problem associated with calculating the orbital volume is twofold (1) defining the anterior extent of the orbit and (2) boundaries defined at each CT slice due to the thin bones such as lamina papyracea and buckling effect of the periosteum can prove to the challenge in accurately calculating or reproducing the volume of each orbit. Volume of left and right orbits may differ by approximately 7 to 8%. Markiewicz et al. [
18] summarized their 23 cases over 2 years to evaluate the reliability of measuring orbital volume and found a significant reduction in orbital volume from pre- to postoperative period (30.6 vs. 25.5 cm
3) compared with present result (34 vs. 30 cm
3). Study is similar to protocol of Markiewicz et al. involving intraoperative navigation [
19], which provides a useful guide and presumably more accurate. Difficulty in intraoperative monitoring of reduction of fractures due to swelling highlights the necessity of an effective tool for intraoperative monitoring of the reduction of zygomatic fractures, so that the need for a secondary surgery is eliminated and more predictable and functionally acceptable results are obtained.
Table 4.
Percentage of restored orbital volume.
Table 4.
Percentage of restored orbital volume.
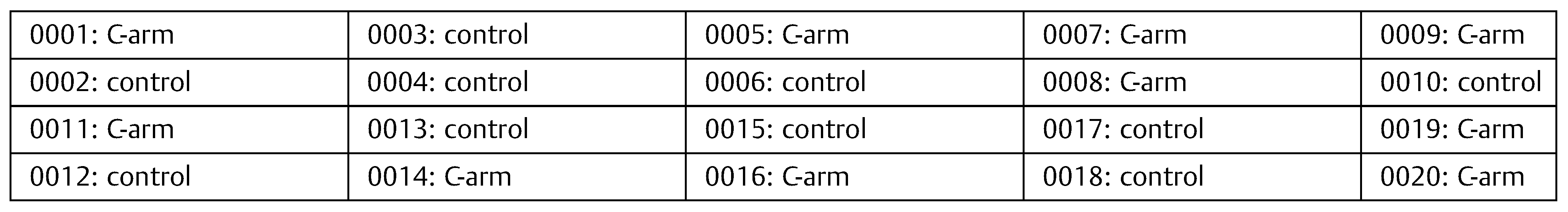
Table 5.
Distribution of patients among cases and controls by random allocation software.
Table 5.
Distribution of patients among cases and controls by random allocation software.
In our study, we found that percentage of orbital volume change is 11.61% preoperatively and 7.27% postoperatively in C-arm group, whereas percentage of orbital volume change is 12.11% preoperatively and 2.21% postoperatively in control group with a
p-value of 0.008, which shows that wide range of difference in postoperative orbital volume is noted in control group with a
p-value of 0.07 in the C-arm group (
Table 3).
Interestingly, we found that on comparing the percentage of orbital volume restored in each group gives a
p-value of 0.228 (
Table 4), which is statistically not significant. Hence, null hypothesis is accepted, which indicates that there is no difference in restoration of orbital volume in ZMC fractures among the two methods, that is, by treating without C-arm or with the aid of C-arm.
This study helps in understanding and interpreting the uses of C-arm in (1) closed reduction of ZMC fractures in future with good alignment, (2) avoiding the return to operating room because of improper management, and (3) avoiding postoperative radiographs.
Conclusion
With the results obtained in this study, we state that C-arm is helpful for accurate reduction with minimal exposure in patients with tetrapod fractures. Most of the zygomatic fractures are stable after elevation and do not necessitate fixation in more than one or two planes. These cases can gain the maximum benefit in the intraoperative C-arm fluoroscopy as all the fracture lines can be visualized and the buttresses can be adequately restored. In comminuted fractures, there are practical difficulties in restoration of orbital volume near to normal of uninjured orbit, which needs exploration of orbital floor and difficult to assess with C-arm. Hence, furthermore studies are required with more sample size using C-arm in comminuted fractures with different applications such as Dolan lines in our study. C-arm would be used as a substitute to preoperative scan in children with claustrophobia, handicapped, or demented patients. Intraoperative and postoperative CT scans can be avoided. It differs from CT and CBCT by having less radiation exposure. Therefore, the C-arm is definitively an effective tool in the oral and maxillofacial surgery armamentarium and in the assessment of zygomatic fracture reduction, and it definitely gives better results with minimal surgical exposure and we suggest it as a best aid, feasible, producing low radiation compared with CT and displaying clear, easily reproducible images without a time lag.