Abstract
The etiology of fractures of the maxillofacial skeleton varies among studies, with motor vehicle accidents and assaults oftentimes the most common. The number of males outnumbers females throughout most studies. Fractures of the zygoma, orbit, and mandible are usually cited as most common fracture types. This study examines a single center’s experience with regards to etiology and distribution of fractures. A retrospective review of all radiologically confirmed facial fractures in a level 1 trauma center in an urban environment was performed for the years 2000 to 2012. Patient demographics, etiology of injury, and location of fractures were collected. During this time period, 2998 patients were identified as having sustained a fracture of the facial skeleton. The average age was 36.9 years, with a strong male predominance (81.5%). The most common etiologies of injury were assault (44.9%) and motor vehicle accidents (14.9%). Throughout the study period, the number of fractures as a result of assault remained relatively constant, whereas the number as a result of motor vehicle accidents decreased slightly. The most common fracture observed was of the orbit, followed by mandible, nasal bones, zygoma, and frontal sinus. Patients sustaining a fracture as a result of assault were more likely to have a mandible fracture. Patients in motor vehicle accidents were more likely to suffer fractures of the maxilla, orbit, and frontal sinus. Mandible fractures are more common in cases of assault. Motor vehicle accidents convey a large force, which, when directed at the craniofacial skeleton, can cause a variety of fracture patterns. The decreasing number of fractures as a result of motor vehicle accidents may represent improved safety devices such as airbags.
Maxillofacial injury represents a significant number of emergency room visits worldwide [1,2,3,4]. Several studies have examined the trends and demographics associated with patients sustaining facial fractures [2,3,5,6]. The mechanism of injury, age, and sex distribution, and the types of bones cited as most commonly fractured have been shown to vary by region [4,6,7,8].
Etiologies typically reported as most common are often motor vehicle accidents (MVA) or interpersonal violence [3,9]. Males have been observed to sustain facial fractures more often than women, and the mechanism of injury often varies between the sexes [5,6]. In most studies, the nasal bones, mandible, orbit, and zygoma are cited as the most commonly fractured bones of the facial skeleton. The purpose of this paper is to examine the demographic characteristics, mechanism of injury, and trends of facial fracture distribution in all patients with maxillofacial injury at a level 1 trauma center over a 12-year period.

Table 1.
Average/median age for each mechanism of injury observed in our study.
Table 1.
Average/median age for each mechanism of injury observed in our study.
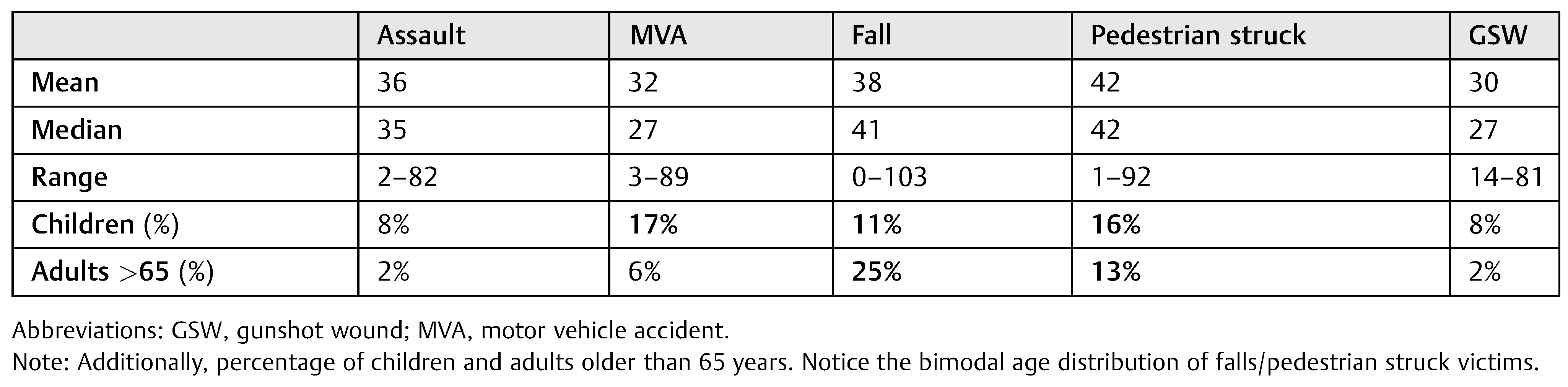 |
Methods
Following institutional review board approval, a retrospective review of all radiologically confirmed facial fractures in a level 1 trauma center (University Hospital, Newark, NJ) was performed for the years 2000 to 2012. Patient demographics, etiology of injury, and location of fractures were collected by using the International Classification of Disease Revision 9 codes to identify radiologically diagnosed facial fractures. Categorical data were analyzed by Pearson chi-squared test for independence, and continuous data were analyzed by a t-test for comparison of means. A value of 0.05 was used to determine significance.
Results
A total of 2,998 patients with facial fractures were identified over the time period. Within this group, the average age at the time of injury was 36.9 years. Victims of gunshot wounds had the lowest average age in our study, whereas patients who sustained facial fractures by falling tended to be older than other groups (Table 1). There was a bimodal age distribution observed in both fall victims and pedestrian struck victims. More than 80% of patients were males, and the most common type of injury was interpersonal violence (45%), followed by MVAs (14%). Other mechanisms of injury observed in our patient population included falls, all-terrain/off-road vehicle accidents, occupational injury, pedestrian struck by motor vehicles, sports-related injuries, seizure, and unknown mechanism (Figure 1).
In total, 17% of MVA victims were children and 15% of pedestrians struck by MVA in our study were children. Additionally, children were involved in 11% of falls leading to facial injury and 8% of both gunshot wound and assault cases. Twenty fall victims were less than 3 years of age. From 2000 to 2012, the number of assault cases remained constant, while the number of MVAs showed a slight decrease over time. Assault cases were significantly more common during the summer months, while all other mechanisms of injury did not vary with seasonal change.
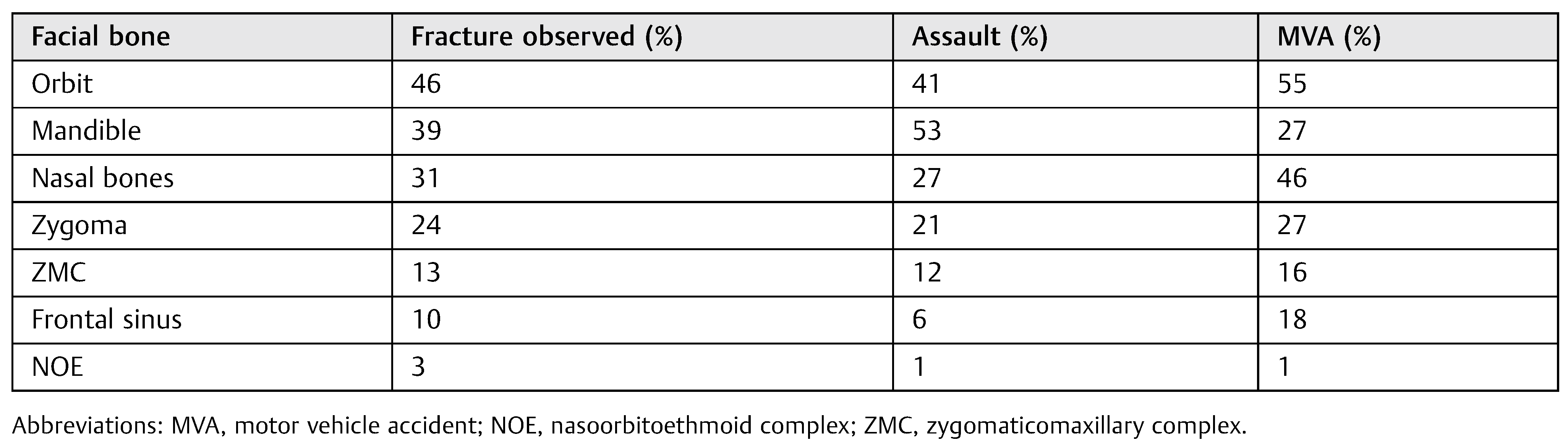
In our patient population, the most common fracture was of the orbit (46%), followed by the mandible (39%), nasal bones (31%), zygoma (23.6%), and frontal sinus (9.9%). Of the nearly 1,400 orbital fractures, 93 were nasoorbitoethmoid fractures and 399 were zygomaticomaxillary complex fractures. Victims of interpersonal violence were more likely to sustain a fracture of the mandible (p < 0.01), while patients who sustained MVAs were more likely to have a fracture of the maxilla (p < 0.01), orbit (p < 0.05), and frontal sinus (p < 0.01; Table 2 and Figure 2). Mandible fractures due to interpersonal violence were most commonly located at the angle, followed by the mandibular body (Figure 3). Coronoid fractures were the least commonly observed fracture site for all etiology types.
Discussion
It is well documented that the epidemiology of facial trauma varies by geographic region and socioeconomic differences [10]. Our study was based on a patient population observed at an urban trauma center in northern New Jersey. The majority of our patients were young, with a strong male predominance. In our patient population, the most common etiology observed was interpersonal violence, followed by MVAs. Other studies have shown trends similar to what we observed [3,11,12,13]. A retrospective study from Lithuania observed interpersonal violence among patients with ages between 15 and 34 years to be the predominant cause of facial fractures in their population [3]. Zaleckas et al. remarked on the increased incidence of facial trauma between April and October, on weekends and at night. In addition, 14% of patients were found to be under the influence of alcohol during the event [3].
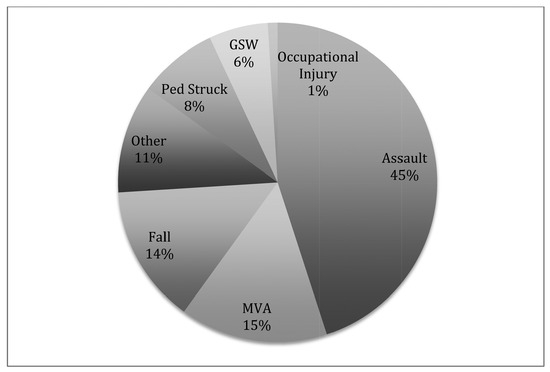
Figure 1.
Common mechanisms of facial bone injury in our patient population. “Other” mechanisms of injury observed in our study include all-terrain vehicle, seizure-related, sports, and unknown. GSW, Gunshot wound; Ped Struck, Pedestrian struck.

Table 2.
Common facial fractures and their associated etiologies.
Table 2.
Common facial fractures and their associated etiologies.
 |
Interpersonal violence has been recognized as a principal cause of facial fractures in developed countries, especially in pediatric and young adult patients, and has been increasing in incidence within the United States [14]. A study performed at our institution observed 43.5% of pediatric facial fractures to be a direct result of interpersonal violence. In this patient population, the number of fractures due to assault remained relatively constant [11]. In contrast, a study from Australia observed a steady increase in the number of facial fractures as a result of interpersonal violence over an 11-year period. This study also noted the association of alcohol with interpersonal violence-related injuries [12]. The EURMAT (European Maxillofacial Trauma) study published in 2014 also found assault to be the most common mechanism of injury in most centers in Europe [13]. This is a new development, as MVAs had traditionally been shown to be the most common cause of facial fractures in many European countries [13].
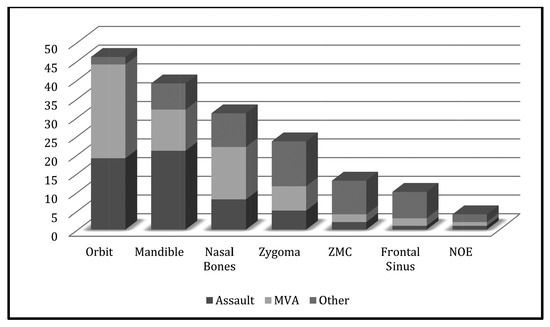
Figure 2.
Common facial fractures and their associated etiologies based on data in Table 2. ZMC, zygomaticomaxillary complex; NOE, nasoorbitoethmoid complex; MVA, motor vehicle accident.
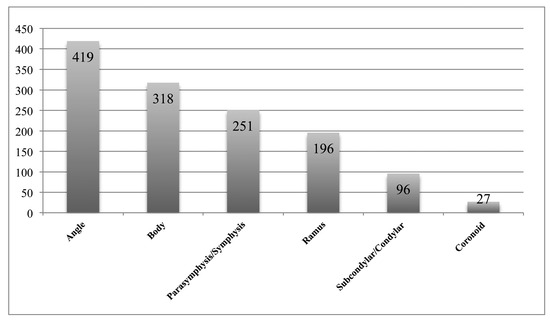
Figure 3.
Location of mandibular fractures caused by interpersonal violence. The most commonly observed fractures were of the angle and body; coronoid fractures were the least commonly observed fracture.
In most developing countries, MVAs remain the predominate cause of facial fractures. A retrospective review of facial injuries in Turkey by Erol et al. observed fractures as a result of road traffic accidents (38%) and falls (36.7%) to occur much more commonly than those associated with interpersonal violence [8]. Interestingly, their study showed facial fractures to occur more often during the summer months and were most common in patients aged between 0 and 10 years [8]. An article from Nigeria demonstrated MVAs and motorbike accidents to be the cause of 80% of facial fractures, whereas interpersonal violence was the inciting event in only 4% of patients. 15 Many studies included pedestrian struck events with road traffic accidents.
With the increased use of safety restraint devices, the number of MVAs has decreased in the United States [10,14,16]. We observed a similar trend, with a slight decrease in fractures as a result of MVAs across the study period. Stacey et al. found the decreasing incidence of facial fractures to be associated with seatbelts, frontal airbags, and newer car models [17]. In developing countries, legislation defining requirements for seatbelts and automobile safety is inconsistent [16,17,18] MVAs cause high-velocity trauma to the facial skeleton and can result in concomitant injury of the brain/ skull, spine, long bones, and pleural/abdominal viscera [7,15,19,20]. At our institution, 60% of facial fractures within the pediatric population accompanied by cervical spine injury were caused by MVAs.21 In our adult population, nearly 50% of our cervical spine injuries were observed to be caused by gunshot wounds. With regard to concomitant intracranial hemorrhage, 37% of pediatric facial fractures associated with intracranial bleeding were caused by motor vehicle collisions.22 This is in contrast to our adult population, where assault and gunshot wound injuries, along with pedestrian struck injuries and falls, caused a large proportion of intracranial hemorrhages, all roughly equivalent to the number of intracranial hemorrhages caused by motor vehicles.
Depending on the study, the nasal bone, zygoma, orbit, and mandible are cited as the most common bones fractured within the facial skeleton [2,4,7,23,24]. In our study, the bones of the orbit were the most commonly fractured, followed by the mandible, nasal bones, zygoma, and frontal sinus. In patients suffering an injury as a result of interpersonal violence, the mandible was found to be the most common bone fractured. In similar studies with interpersonal violence as the most common mechanism of injury, mandible and zygoma fractures are cited as the predominant fracture type [13,24]. The predilection for victims of interpersonal violence to suffer fractures of the mandible and zygoma is obvious mechanistically, as most victims undergo blunt traumatic force to their jaw or cheek by another’s fist.
In our study, patients involved in MVAs were more likely to suffer fractures of the maxilla, orbit, and frontal sinus. The greater thickness of bone in these facial buttresses prevents their injury in most cases of lower velocity trauma [10]. However, MVAs can provide enough force to disrupt this rigid protective framework of the orbital contents, intracranial space, and midfacial structures [10,25].
Conclusion
The epidemiology of facial fractures varies between regions and populations around the world, although the young male population almost universally appears to be the most likely group to suffer such an injury. Interpersonal violence is the most common cause of facial fractures in many developed countries, including the United States, though MVAs remain an important etiology worldwide. Mandible fractures are commonly observed in cases of interpersonal violence, while road traffic accidents tend to cause fractures of the more resilient buttresses, with resulting concomitant injuries. The decreasing number of fractures as a result of MVAs may represent improved safety devices. Reporting etiologies and fracture patterns is important to document changing epidemiologic patterns and the effect that new safety measures may have.
References
- Kaul, R.P.; Sagar, S.; Singhal, M.; Kumar, A.; Jaipuria, J.; Misra, M. Burden of maxillofacial trauma at level 1 trauma center. Craniomaxillofac Trauma Reconstr 2014, 7, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Schneider, D.; Kämmerer, P.W.; Schön, G.; Dinu, C.; Radloff, S.; Bschorer, R. Etiology and injury patterns of maxillofacial fractures from the years 2010 to 2013 in Mecklenburg-Western Pomerania, Germany: A retrospective study of 409 patients. J Craniomaxillofac Surg 2015, 43, 1948–1951. [Google Scholar] [CrossRef]
- Zaleckas, L.; Pečiulienė, V.; Gendvilienė, I.; Pūrienė, A.; Rimkuvienė, J. Prevalence and etiology of midfacial fractures: A study of 799 cases. Medicina (Kaunas) 2015, 51, 222–227. [Google Scholar] [CrossRef]
- Gassner, R.; Tuli, T.; Hächl, O.; Rudisch, A.; Ulmer, H. Cranio-maxillofacial trauma: A 10. year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg 2003, 31, 51–61. [Google Scholar] [CrossRef]
- Hoppe, I.C.; Kordahi, A.M.; Paik, A.M.; Lee, E.S.; Granick, M.S. Age and sexrelated differences in 431 pediatric facial fractures at a level 1 trauma center. J Craniomaxillofac Surg 2014, 42, 1408–1411. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.H.; Liu, Q.; Yang, R.T.; Li, Z.; Li, Z.B. Maxillofacial fractures in women and men: A 10. year retrospective study. J Oral Maxillofac Surg 2015, 73, 2181–2188. [Google Scholar] [CrossRef] [PubMed]
- Kumar, G.B.; Dhupar, V.; Akkara, F.; Kumar, S.P. Patterns of maxillofacial fractures in goa. J Maxillofac Oral Surg 2015, 14, 138–141. [Google Scholar] [CrossRef]
- Erol, B.; Tanrikulu, R.; Görgün, B. Maxillofacial fractures. Analysis of demographic distribution and treatment in 2901 patients (25-year experience). J Craniomaxillofac Surg 2004, 32, 308–313. [Google Scholar] [CrossRef]
- Iida, S.; Kogo, M.; Sugiura, T.; Mima, T.; Matsuya, T. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg 2001, 30, 286–290. [Google Scholar] [CrossRef]
- Rodriguez, E.D.; Dorafshar, A.H.; Manson, P.N. Facial fractures. In Plastic Surgery Section I: Craniofacial Trauma; Neligan, P.C., Ed.; Elsevier: New York, NY, 2013; pp. 48–88. [Google Scholar]
- Hoppe, I.C.; Kordahi, A.M.; Lee, E.S.; Granick, M.S. Pediatric facial fractures: Interpersonal violence as a mechanism of injury. J Craniofac Surg 2015, 26, 1446–1449. [Google Scholar] [CrossRef]
- Lee, K. Global trends in maxillofacial fractures. Craniomaxillofac Trauma Reconstr 2012, 5, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Roccia, F.; Zavattero, E.; et al. European Maxillofacial Trauma (EURMAT) project: A multicentre and prospective study. J Craniomaxillofac Surg 2015, 43, 62–70. [Google Scholar] [CrossRef]
- Sharabi, S.E.; Koshy, J.C.; Thornton, J.F.; Hollier, L.H., Jr. Facial fractures. Plast Reconstr Surg 2011, 127, 25e–34e. [Google Scholar] [CrossRef] [PubMed]
- Udeabor, S.; Akinmoladun, V.I.; Olusanya, A.; Obiechina, A. Pattern of midface trauma with associated concomitant injuries in a Nigerian referral centre. Niger J Surg 2014, 20, 26–29. [Google Scholar] [PubMed]
- World Health Organization. Global Status Report on Road Safety 2013: Supporting a Decade of Action; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Stacey, D.H.; Doyle, J.F.; Gutowski, K.A. Safety device use affects the incidence patterns of facial trauma in motor vehicle collisions: An analysis of the National Trauma Database from 2000 to 2004. Plast Reconstr Surg 2008, 121, 2057–2064. [Google Scholar] [CrossRef]
- Boffano, P.; Kommers, S.C.; Karagozoglu, K.H.; Forouzanfar, T. Aetiology of maxillofacial fractures: A review of published studies during the last 30 years. Br J Oral Maxillofac Surg 2014, 52, 901–906. [Google Scholar] [CrossRef]
- Alvi, A.; Doherty, T.; Lewen, G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope 2003, 113, 102–106. [Google Scholar] [CrossRef]
- Hoppe, I.C.; Kordahi, A.M.; Paik, A.M.; Lee, E.S.; Granick, M.S. Examination of life-threatening injuries in 431 pediatric facial fractures at a level 1 trauma center. J Craniofac Surg 2014, 25, 1825–1828. [Google Scholar] [CrossRef]
- Halsey, J.N.; Hoppe, I.C.; Marano, A.A.; Kordahi, A.M.; Lee, E.S.; Granick, M.S. Characteristics of cervical spine injury in pediatric patients with facial fractures. J Craniofac Surg 2016, 27, 109–111. [Google Scholar] [CrossRef]
- Marano, A.A.; Hoppe, I.C.; Halsey, J.N.; Kordahi, A.M.; Granick, M.S.; Lee, E.S. Patterns of intracranial hemorrhage in pediatric patients with facial fractures. Craniomaxillofac Trauma Reconstr 2016, 9, 35–39. [Google Scholar] [CrossRef]
- Park, K.P.; Lim, S.U.; Kim, J.H.; et al. Fracture patterns in the maxillofacial region: A four-year retrospective study. J Korean Assoc Oral Maxillofac Surg 2015, 41, 306–316. [Google Scholar] [CrossRef] [PubMed]
- Salentijn, E.G.; Boffano, P.; Boverhoff, J.; van den Bergh, B.; Forouzanfar, T. The epidemiological characteristics of zygomatic complex fractures: A comparison between the surgically and non-surgically treated patients. Natl J Maxillofac Surg 2013, 4, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Whitesell, R.T.; Steenburg, S.D.; Shen, C.; Lin, H. Facial fracture in the setting of whole-body CT for trauma: Incidence and clinical predictors. AJR Am J Roentgenol 2015, 205, W4–W10. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the author. The Author(s) 2016.