Abstract
The purpose of this study was to present the management of a series of patients referred with infraorbital nerve paraesthesia that developed after insignificant orbital floor fracture without diplopia or exophthalmos, and that did not require initial surgical repair. This is a retrospective interventional case series. The main outcome and measures were assessment of preoperative symptoms including neuralgia and sensory symptoms; review of periorbital computed tomography (CT) scans; and assessment of postoperative effects of surgery for infraorbital nerve decompression. Nine patients were identified who developed neuralgia affecting the infraorbital nerve distribution from a cohort of 79 patients who presented with orbital floor fracture. Six were female and three were male. Age range was 22 to 73 years with a mean of 48 years. Six patients were clinically depressed due to the chronic pain. In addition, two patients had dizziness on upgaze; one patient had blurring of central vision on eye movements; and one patient had mood swings. Reviews of CT scans revealed subtle disruption of the infraorbital canal in all cases. All nine patients underwent infraorbital nerve decompression. Abnormal adhesions between the nerve and its bony canal were found in five of nine cases. Follow-up ranged from 3 to 37 months (mean: 18 months). Following surgery, after a variable period of time ranging from 1 day to 3 months, all patients had resolution of their symptoms. Mean follow-up was 18 months. Reconstructive surgeons should be aware that infraorbital nerve neuralgia, secondary to disruption of the nerve in the distorted bony canal, may be another indication for surgical intervention following orbital floor trauma in selected cases, in addition to more traditionally accepted indications. Neuralgia and causalgia are probably more common than previously thought and symptoms should be actively sought in the patient’s history or else risk being overlooked and inappropriately managed. Long-term follow-up of such patients is unlikely to be practical. Patient and/or family practitioner education of possible sequelae may be one possible solution to detect this type of problem early. Nerve decompression, where indicated, may improve the patient’s neuralgia and associated behavioral changes and quality of life. An optimal diagnostic and management algorithm is yet to be established.
Orbital blowout fractures commonly occur along the floor of the orbit, medial to the infraorbital nerve canal. Therefore, the infraorbital nerve may be contused, and the canal deformed, causing symptomatic dysesthesia in the region of its distribution. In many cases, this will settle and surgical intervention is not required [1]. The accepted indications for intervention in orbital floor fractures include muscle entrapment in a trapdoor-type fracture (white-eyed fracture); enophthalmos/hypoglobus causing facial asymmetry; and symptomatic diplopia with positive forced ductions.
Less typically, orbital floor fractures might result in persistent neuralgia (pain) or causalgia (burning sensation) in the region of the infraorbital nerve distribution [2,3,4]. We report on a series of patients who developed infraorbital nerve neuralgia and other sensory symptoms causing a deterioration in their quality of life, and the outcome of nerve decompression on their symptoms.
Patients and Methods
Institutional approval for this study has been received and each patient provided informed consent. In a 9-year period, 79 pure orbital fractures were referred to the orbital clinic [5]. Fourteen patients did not meet the criteria for their orbital floor surgery because they had full ocular movements with no diplopia and no significant enophthalmos. Infraorbital nerve neuralgia and other sensory symptoms (Table 1) had developed in 8 out of 14 patients who did not need surgery, and 1 of the patients who had had orbital floor surgery.
Assessment and Operative Procedure
A computed tomography (CT) scan of the patients with the infraorbital nerve sensory symptoms was requested with a soft tissue protocol for further evaluation of the fracture site and infraorbital nerve canal.
A McCord eyelid swing approach was used in all patients. After lateral canthotomy and division of inferior limb of lateral canthus, conjunctiva was divided with lower lid retractors half way between the fornix and lower border of tarsus parallel to orbital rim and anterior to septum all the way to inferior aspect of the caruncle. Following blunt dissection in the same plane, the arcus marginalis of orbital rim is exposed. This approach gives an adequate access to the floor medial and lateral wall. The periorbitum 3 mm anterior to orbital rim is divided horizontally. The periorbitum is lifted medial and lateral to the infraorbital nerve canal all the way to inferior orbital fissure laterally and trigon medially. The dissection is then extended from lateral and medial floor centrally to expose orbital floor in its entirety. Infraorbital canal is identified centromedially, emerging from infraorbital fissure posteriorly. With the use of a Mitchell strimmer, part of the soft infraorbital roof canal is lifted and this is extended posteriorly and anteriorly to expose infraorbital nerve. If there was a need to augment the volume of the orbit, a Medpor (Stryker, Chicago, IL) barrier implant (1 mm) was shaped appropriately and placed on the orbital floor. In the cases that the infraorbital nerve canal was significantly distorted following deroofing, the canal part of orbital bone was removed medially and laterally (see Figure 1). In these cases, a titanium mesh was cut to the shape and screwed to the orbital rim. The periorbitum was then repaired by 5/0 Vicryl suture (Ethicon, Somerville, NJ) at the orbital rim. The conjunctiva was repaired by 6/0 Vicryl and lateral canthus was repaired by 5/0 Vicryl suture.
Results
Nine patients were identified who developed neuralgia affecting the infraorbital nerve distribution. Six were female and three were male. The age range was 22 to 73 years with a mean of 48 years. Six patients became depressed (diagnosed by their general practitioner or hospital psychiatrist) due to their pain. Four patients had other associated sensory symptoms including dizziness on upgaze (two patients), blurring of central vision on eye movements (one patient), and mood swings (one patient). Review of the CT scans of these patients at a radiology multidisciplinary team meeting revealed subtle disruption of the infraorbital canal and the infraorbital nerve in all cases (Figure 2a–d). All nine patients underwent infraorbital nerve decompression. In five of nine cases, adhesions between the nerve and its canal were noted. Follow-up ranged from 3 to 37 months (mean, 18 months). Subjective symptoms of neuralgia and depression improved significantly following surgery in all cases. Table 1 summarizes cases and findings.
Representative Cases
Case 1
A 24-year-old woman sustained blunt trauma to the left orbit (kicked in the face). A CT scan, done 2 days after the injury, was reported as normal. Over the next 12 months, she suffered from a severe burning sensation (causalgia) of her cheek, exacerbated by looking up. The pain affected her mood necessitating the introduction of antidepressants. She required referral to the pain clinic for control. She was eventually referred 12 months after the injury for an orbital opinion. She had no enophthalmos, no diplopia, and her ocular movements were full. The CT scan (see Figure 2) was reviewed which showed a small depressed inferomedial orbital wall fracture adjacent to the infraorbital nerve canal. Thirteen months after the initial injury, the patient underwent surgery. Adhesions to the inferior orbital floor and infraorbital nerve were found and divided. The infraorbital canal was deroofed and the infraorbital nerve was freed. The infraorbital nerve bruising was due to old trauma. There was immediate resolution of her symptoms on the postoperative day. The initial infraorbital nerve anesthesia settled. The patient was extremely happy, having stopped her antidepressants, and she remained symptom free for 17 months.
Case 5
A 73-year-old woman sustained blunt trauma to the right orbit following a fall. A CT scan revealed a right orbital floor fracture with no incarceration muscle. She had no enophthalmos and her ocular movements were full. She initially had pain around her right orbit, but over the next 2 years, she suffered with paraesthesia over the right cheek.
She was also having dizziness on looking up and down. A repeat CT scan showed distortion of the right orbital floor in the region of the infraorbital canal. The infraorbital canal was widened and its contents showed abnormally dense nerve with the presence of adhesions and scarring. Orbital floor surgery with a titanium mesh was performed. She had improved paraesthesia and dizziness. She remains symptom free after 15 months follow-up.

Table 1.
Cases and findings of infraorbital nerve neuralgia and other sensory symptoms.
Table 1.
Cases and findings of infraorbital nerve neuralgia and other sensory symptoms.
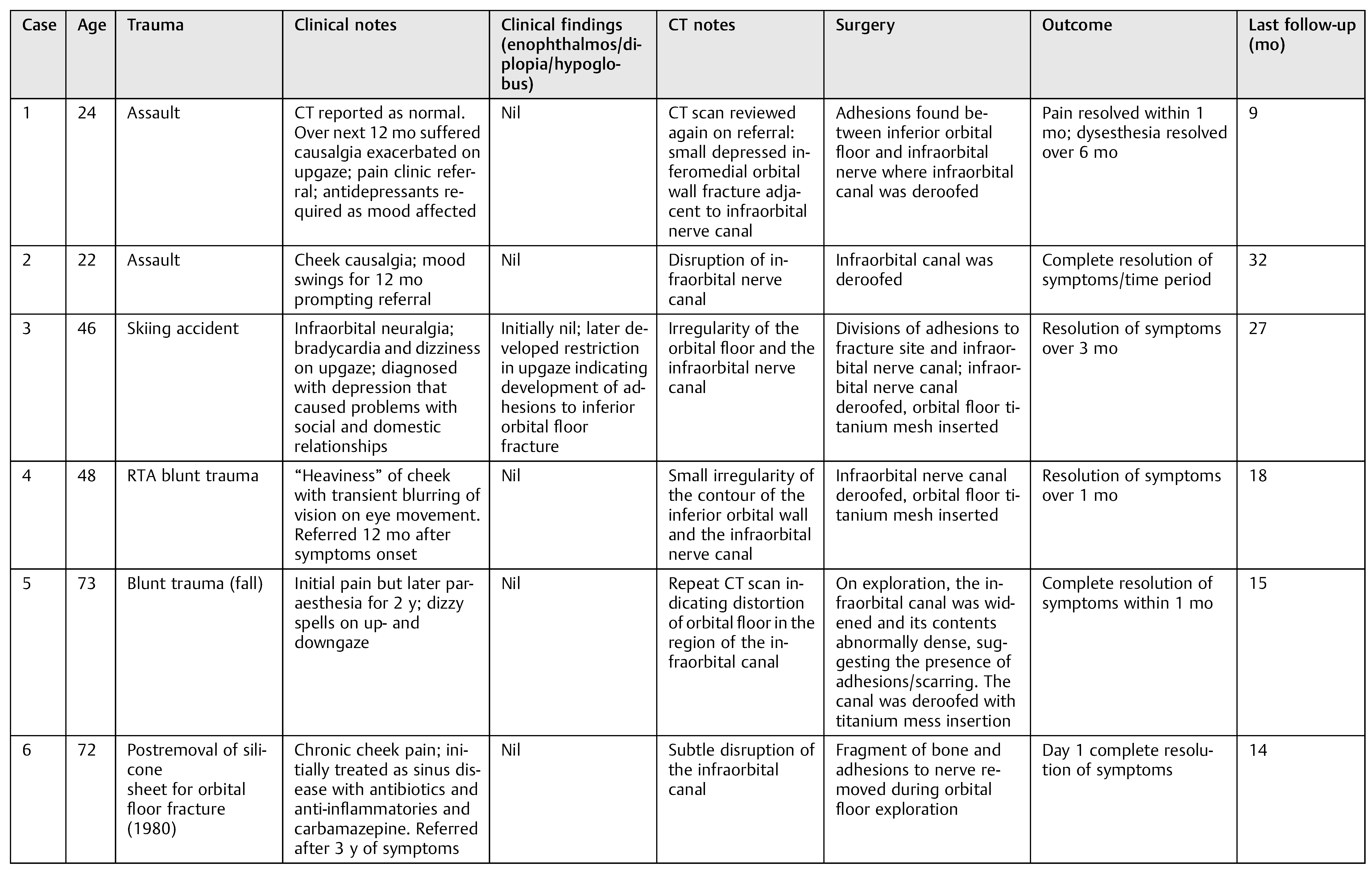 |
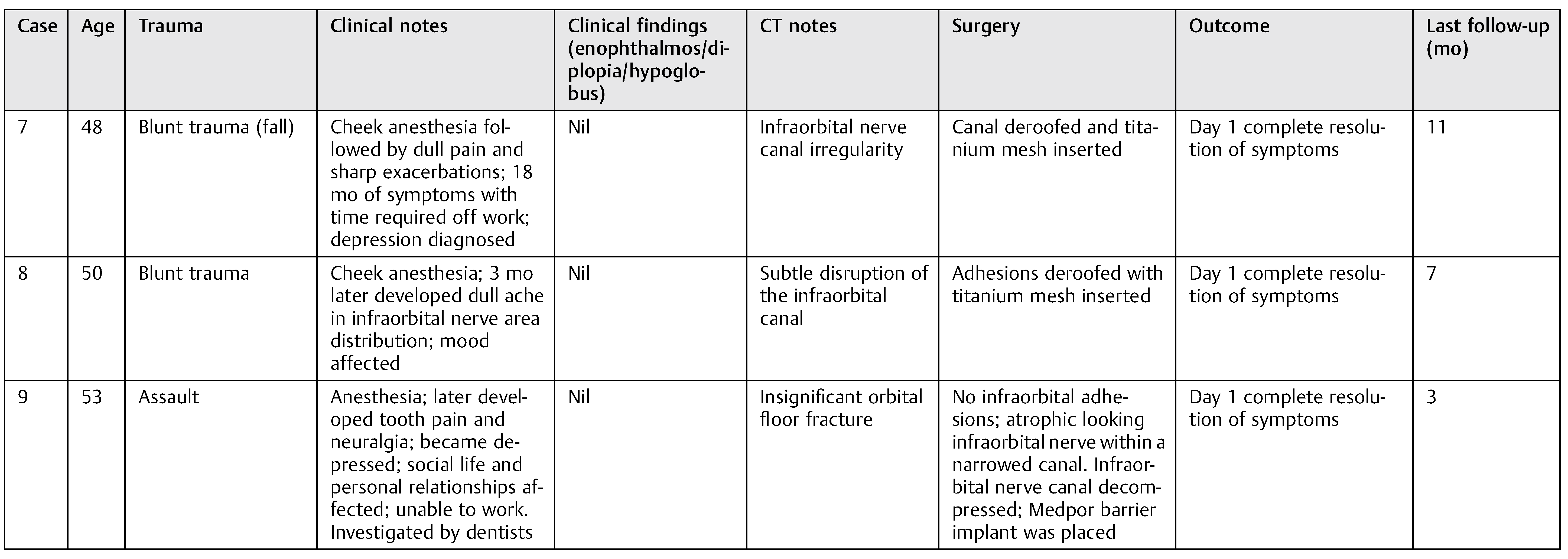 |
Abbreviation: CT, computed tomography; RTA, road traffic accident.
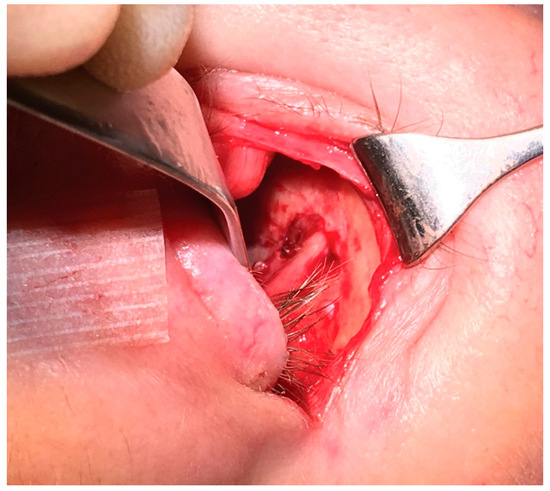
Figure 1.
Infraorbital nerve canal deroofed to expose infraorbital nerve in its canal.
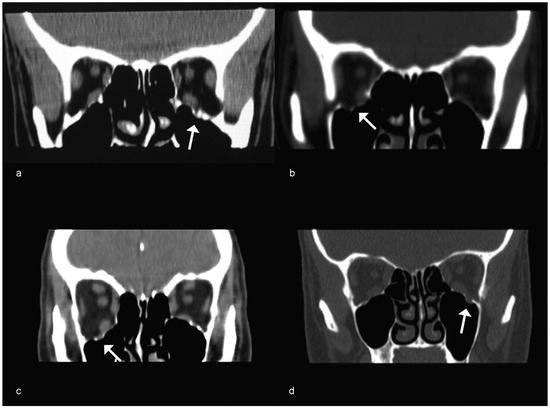
Figure 2.
(a) Case 1: Subtle left orbital floor fracture involving the infraorbital nerve canal (arrow). There is no muscle entrapment. (b) Case 2: Right orbital floor fracture involving the infraorbital nerve canal (arrow). (c) Case 3: Right orbital floor fracture involving the infraorbital nerve canal (arrow). (d) Case 4: Left orbital floor fracture involving the infraorbital nerve canal (arrow).
Case 9
A 53-year-old woman sustained a left orbital floor fracture following an assault 14 years before referral. The orbital floor had not been repaired. She developed infraorbital anesthesia and then experienced severe infraorbital neuralgia and tooth pain over the following years that had been investigated for dental causes. She became depressed and the pain affected her social life and relationships. She could not cope working full time. A CT scan of her orbits showed an insignificant left orbital floor fracture. She underwent surgery. Following deroofing of the canal, an atrophic looking infraorbital nerve was found tight within its narrowed canal. The nerve was decompressed. A Medpor barrier implant was placed. Her infraorbital neuralgia and tooth pain had resolved by the following day. The area of infraorbital anesthesia that she had suffered with for 14 years reduced significantly. She remained symptom free during the next 3 months’ follow-up.
Discussion
Transient infraorbital nerve anesthesia is common following an orbital floor fracture [6,7,8]. The clinical and surgical focus is often on skeletal anatomy, orbital volume, and soft tissue, but the long-term effects on the infraorbital nerve are not often considered. There is a paucity of literature addressing the topic. Occasionally, patients can develop pain in the distribution of the infraorbital nerve months after the initial injury or after open reduction of the fracture [9,10,11]. The infraorbital nerve within this canal is vulnerable to damage in many orbital floor fractures due to its proximity to the typical fracture site. Persistent paraesthesia is likely to be due to compression of the infraorbital nerve in the collapsed canal, or irritation of the nerve by sharp fragments of bone, or adhesional bands.
We have reported a series of nine patients with infraorbital neuralgia. All these patients had insignificant orbital floor fractures without extraocular muscle entrapment or need for initial orbital repair, initially regarded as nonoperative. Subsequent to their trauma, six patients (cases 1, 3, 5, and 7–9) became clinically depressed (diagnosed either by their general practitioner or hospital psychiatrist) with the chronic pain that resulted in problems with their work, social, and domestic life. Many of these patients required antidepressants before referral. Decompression of the infraorbital canal was performed and, in five of nine cases, adhesions between the nerve and its canal were noted during surgery. Resolution of patients’ sensory symptoms and depression was noted in all cases. The improvement in pain has been noted in only one study involving three patients with neuralgia [9].
The patients in our series did not meet the widely accepted criteria for surgical intervention for blowout fractures as they had insignificant inferior orbital wall fractures without extraocular muscle entrapment, no significant enophthalmos, no diplopia, and full ocular movements. However, they all benefited from infraorbital nerve decompression, whether done as a single procedure or as part of repair of the inferior orbital wall fracture. In addition to the resolution of the neuralgia, there was a great improvement in the patient’s mood and their mental well-being.
In our experience, the presence of neuralgia/causalgia is probably more common than previously accepted. The symptoms are of a subjective nature, difficult to quantify objectively, and risk being overlooked. Patients can present at a time remote from the initial trauma. It is also difficult to predict those patients likely to develop such problems. To confuse the picture further, they can present to other subspecialties. Long-term follow-up of nonoperative patients is impractical. Patient and/or family practitioner education of possible sequelae would be one possible solution to detect this type of problem early.
Our study does have limitations. It is retrospective in nature with only nine cases over a 9-year period. We did not have a set protocol in dealing with these patients as the problem is not well recognized. For the same reason, the indications and timing of intervention for surgeons are difficult to comment on. Each patient was evaluated on a case-bycase basis and offered surgery when there was suspicion on CT imaging of disruption of the infraorbital nerve canal. Patients were warned that there was a risk that surgery may not resolve their dysesthesia symptoms. Also, the time to improvement may be variable based on our experience but nevertheless did occur.
Future studies in this area would benefit from more objective neuropsychological testing of depression, apathy, and anxiety, as well as objective electrical testing of nerves. Surgery can have a placebo effect and there are potentially many compounding variables, such as the use of analgesics and their effect on behavior. We did attempt an assessment of mental well-being to identify the psychological effects of surgery on our patients by using the Frontal Systems Behavior Scale (FrSBe) (PAR, Inc., Lutz, FL). The FrSBe provides a brief, reliable, and valid measure of three frontal systems behavioral syndromes: apathy, disinhibition, and executive dysfunction. It quantifies behavioral changes over time by including both baseline (retrospective) and current assessments of behavior. This was not included in the main body of this study as an insufficient number of patients completed the survey. In three of six patients who completed the survey (cases 1, 3, and 7), a noticeable improvement in their mental well-being on the FrSBe was recorded after surgery.
Objective electrical neurosensory testing has been shown to be useful in the context of zygoma fractures where there are persistent sensibility abnormalities, indicating injury to the infraorbital nerve. Bilateral neurosensory measurements obtained with a Pressure-Specified Sensory Device (Sensory Management Services, Baltimore, MD) demonstrated abnormal sensibility on the side of the zygoma fracture, compared with the contralateral side in one series [12]. Where available, neurosensory testing can be used as a clinical adjunct for the evaluation of patients with facial pain or dysesthesia after facial fracture reconstruction. The authors concluded that algorithms for the diagnosis and treatment of trigeminal nerve injuries after craniofacial trauma needed to be developed.
In conclusion, infraorbital nerve neuralgia, secondary to disruption of the nerve in the distorted bony canal, may be another indication for surgical intervention in selected cases, in addition to traditional criteria. Neuralgia and causalgia are probably more common than previously thought and symptoms should be actively sought in the patient’s history or else risk being overlooked and inappropriately managed. Long-term follow-up of nonoperative patients is impractical and patient and/or family practitioner education of possible sequelae would be one possible solution to detect this type of problem early. Nerve decompression, where indicated, may improve the patient’s neuralgia and associated behavioral changes and quality of life. An optimal diagnostic and management algorithm is yet to be established.
References
- Putterman, A.M.; Stevens, T.; Urist, M.J. Nonsurgical management of blow-out fractures of the orbital floor. Am J Ophthalmol 1974, 77, 232–239. [Google Scholar] [PubMed]
- Burnstine, M.A. Clinical recommendations for repair of orbital facial fractures. Curr Opin Ophthalmol 2003, 14, 236–240. [Google Scholar] [PubMed]
- Freeman, B.S. Post-traumatic infraorbital neuralgia. Tex State J Med 1961, 57, 352–354. [Google Scholar] [PubMed]
- Boush, G.A.; Lemke, B.N. Progressive infraorbital nerve hypesthesia as a primary indication for blow-out fracture repair. Ophthal Plast Reconstr Surg 1994, 10, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Beigi, B.; Khandwala, M.; Gupta, D. Management of pure orbital floor fractures: A proposed protocol to prevent unnecessary or early surgery. Orbit 2014, 33, 336–342. [Google Scholar] [PubMed]
- Ellis, E.I.I.I.; el-Attar, A.; Moos, K.F. An analysis of 2067 cases of zygomatico-orbital fracture. J Oral Maxillofac Surg 1985, 43, 417–428. [Google Scholar] [PubMed]
- Peltomaa, J.; Rihkanen, H. Infraorbital nerve recovery after minimally dislocated facial fractures. Eur Arch Otorhinolaryngol 2000, 257, 449–452. [Google Scholar] [PubMed]
- Taicher, S.; Ardekian, L.; Samet, N.; Shoshani, Y.; Kaffe, I. Recovery of the infraorbital nerve after zygomatic complex fractures: A preliminary study of different treatment methods. Int J Oral Maxillofac Surg 1993, 22, 339–341. [Google Scholar] [CrossRef]
- Tengtrisorn, S.; McNab, A.A.; Elder, J.E. Persistent infra-orbital nerve hyperaesthesia after blunt orbital trauma. Aust N Z J Ophthalmol 1998, 26, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Norman, J.E.; Dan, N.G.; Rogers, P.A. Post-traumatic infraorbital neuropathy. Orbit 1982, 1, 259–266. [Google Scholar]
- Bailey, K.; Ng, J.D.; Hwang, P.H.; Saulny, S.M.; Holck, D.E.; Rubin, P.A. Infraorbital nerve surgical decompression for chronic infraorbital nerve hyperesthesia. Ophthal Plast Reconstr Surg 2007, 23, 49–51. [Google Scholar] [PubMed]
- Fogaçc, W.; Ferreira, M.C.; Dellon, A.L. Neurosensory testing in evaluation of infraorbital nerve injuries associated with zygoma fracture. Plast Reconstr Surg 2004, 113, 834–838. [Google Scholar]
© 2016 by the author. The Author(s) 2016.