Potential Application of Luteolin as an Active Antibacterial Composition in the Development of Hand Sanitizer Products
Abstract
1. Introduction
2. Results and Discussion
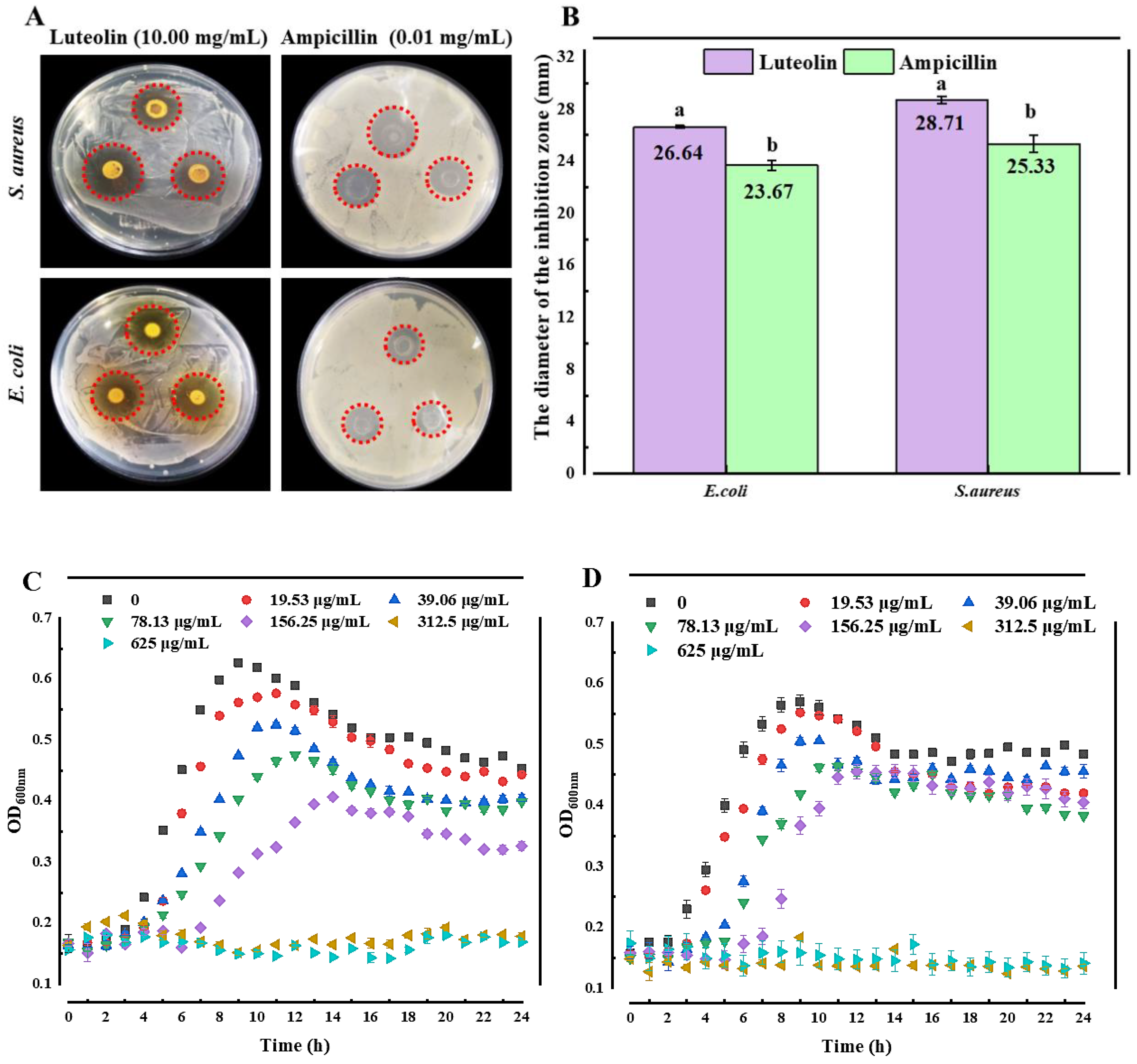
2.1. Antibacterial Activity
2.2. Antibacterial Mechanism
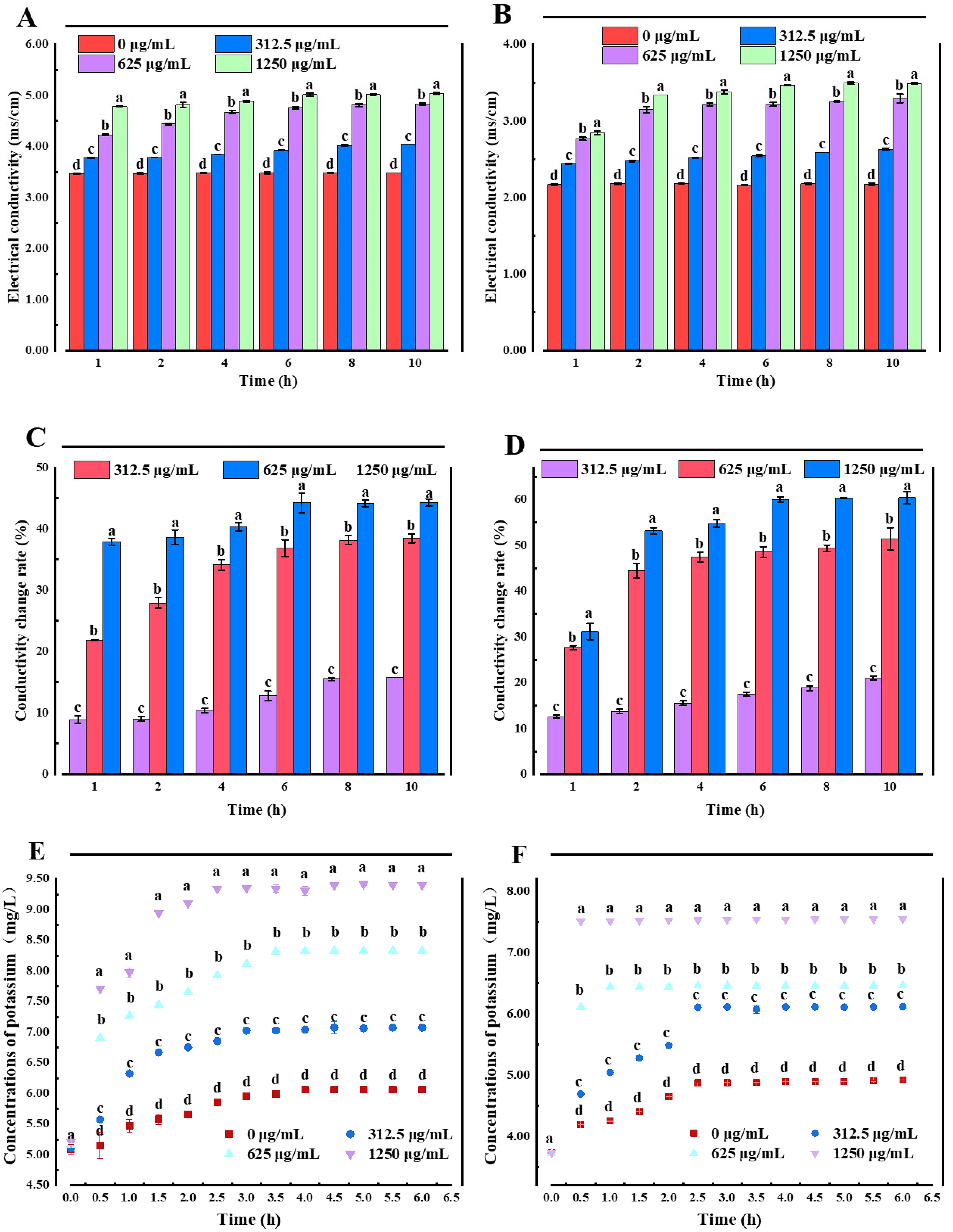
2.2.1. Membrane Permeability Analysis
2.2.2. Cell Membrane Integrity
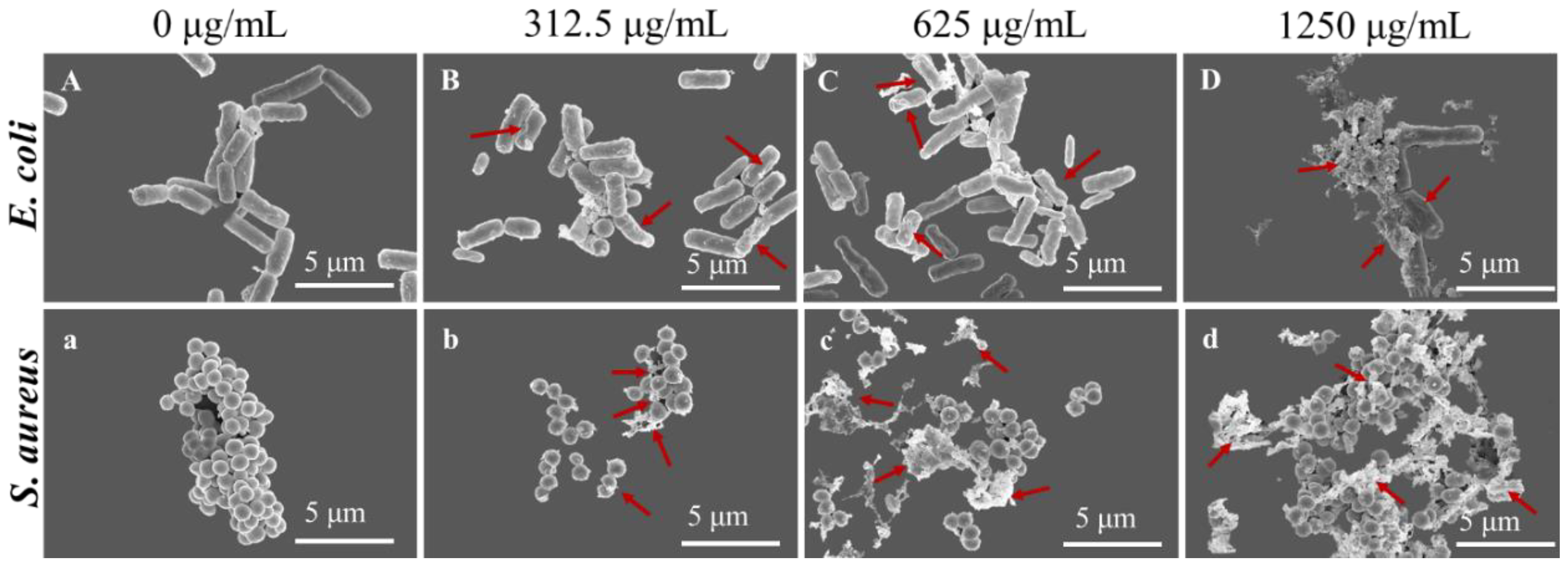
2.2.3. SEM Analysis
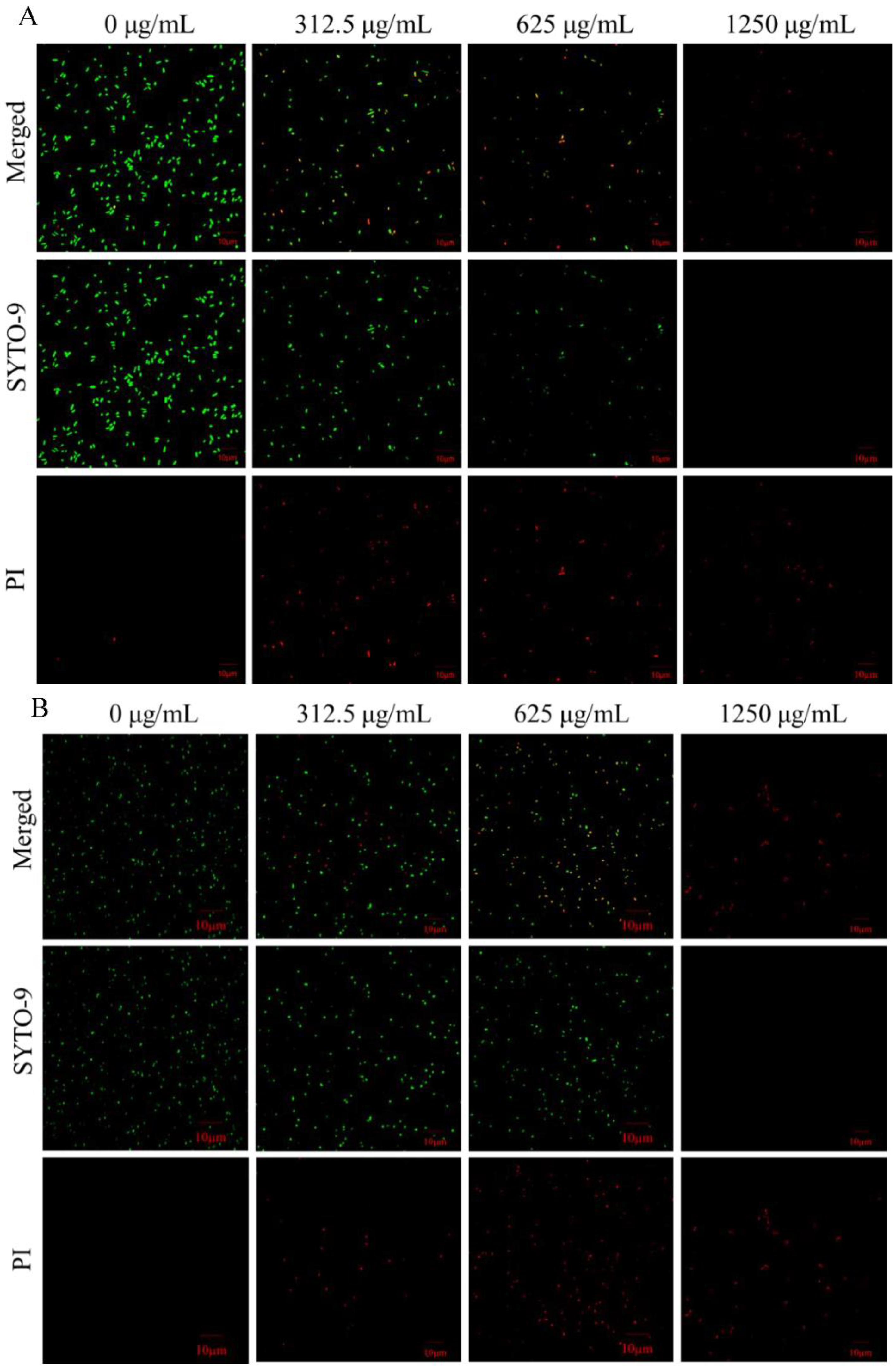
2.2.4. CLSM Analysis
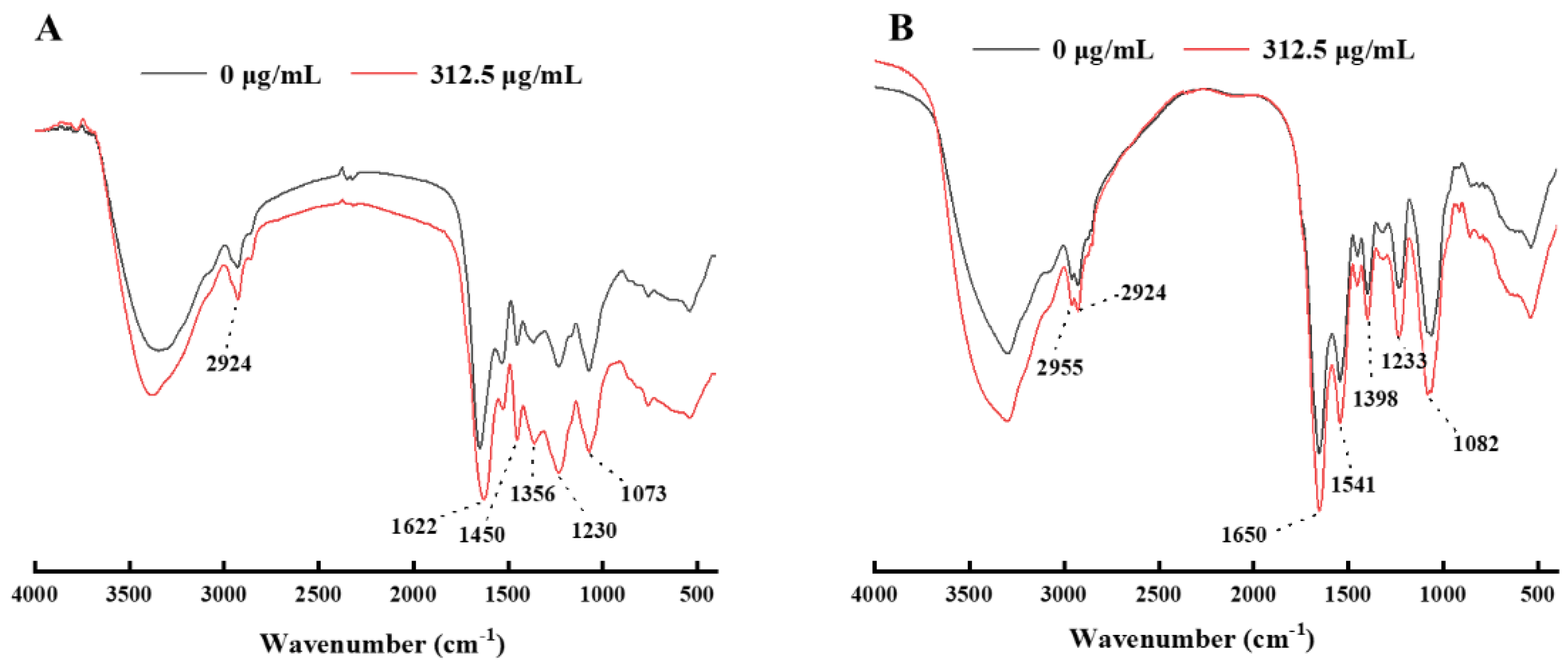
2.2.5. FTIR
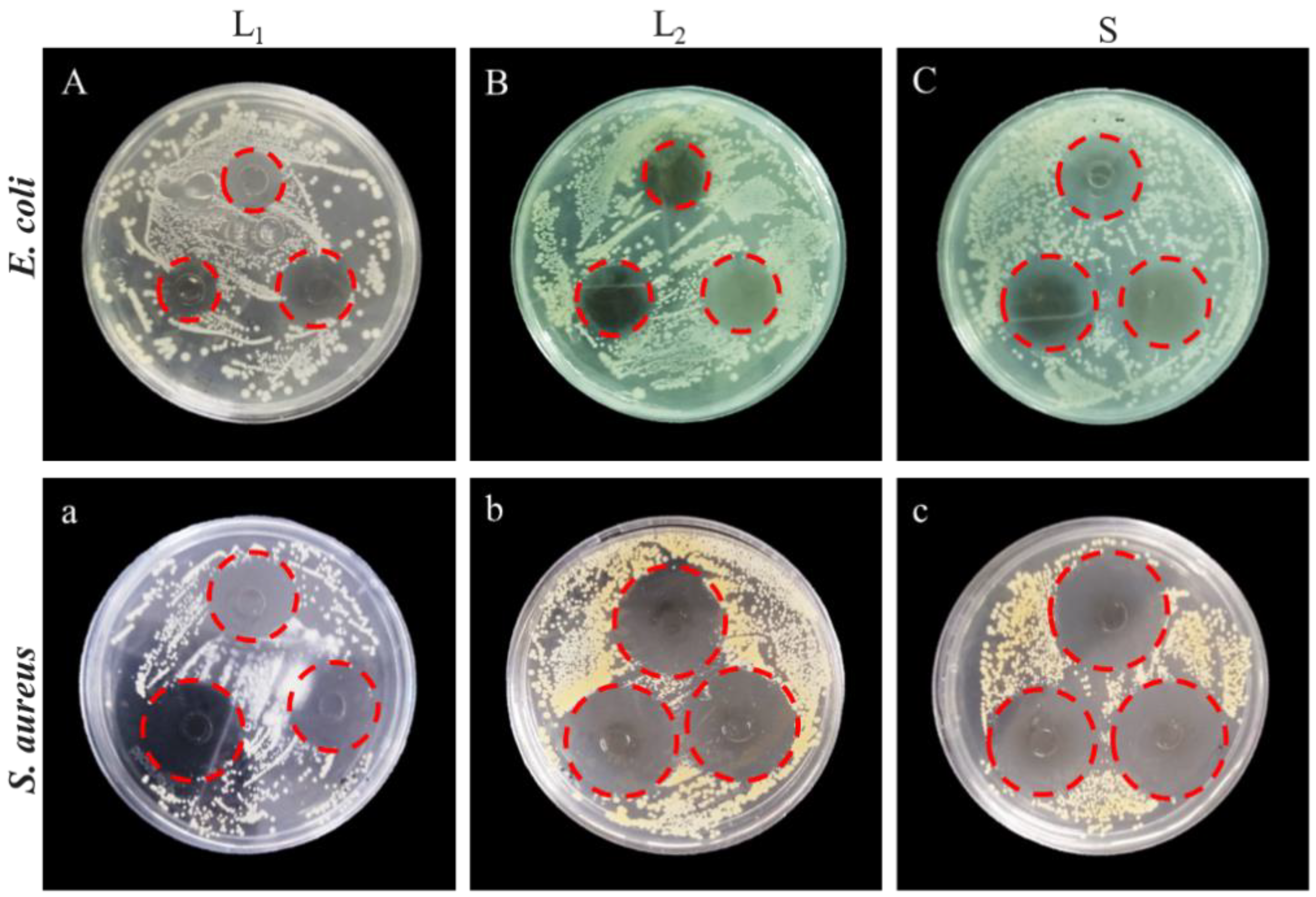
2.3. Application of LUT in Antibacterial Hand Sanitizer
3. Materials and Methods
3.1. Materials
3.2. Strains and Culture Conditions
3.3. Determination of the Diameter of the Inhibition Zone (DIZ)
3.4. Determination of Minimum Inhibitory Concentration (MIC) and Minimal Bactericidal Concentration (MBC)
3.5. Determination of Growth Curves
3.6. Extracellular Conductivity
3.7. Extracellular Potassium Ion Concentration
3.8. Cell Membrane Integrity
3.9. Scanning Electron Microscopy (SEM)
3.10. Confocal Laser Scanning Microscopy (CLSM)
3.11. Fourier Transform Infrared Spectroscopy (FTIR)
3.12. Product
3.12.1. Formulations of Hand Sanitizers
3.12.2. Antibacterial Effect Comparison
3.12.3. Stability Evaluation
3.13. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shang, K.; Ai, S.; Ma, Q.; Tang, T.; Yin, H.; Han, H. Effective photocatalytic disinfection of Escherichia coli and Staphylococcus aureus using polythiophene/MnO2 nanocomposite photocatalyst under solar light irradiation. Desalination 2011, 278, 173–178. [Google Scholar] [CrossRef]
- Aruwa, C.E.; Amoo, S.O.; Koorbanally, N.; Kudanga, T. Enzymatic dimerization of luteolin enhances antioxidant and antimicrobial activities. Biocatal. Agric. Biotechnol. 2021, 35, 102105. [Google Scholar] [CrossRef]
- Ergüden, B. Phenol group of terpenoids is crucial for antibacterial activity upon ion leakage. Lett. Appl. Microbiol. 2021, 73, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Koubaa, M.; Ktata, A.; Bouaziz, F.; Driss, D.; Ghorbel, R.E.; Chaabouni, S.E. Solvent extract from Opuntia stricta fruit peels: Chemical composition and Biological activities. Free. Radic. Antioxid. 2015, 5, 52–59. [Google Scholar] [CrossRef]
- Xie, Y.; Chen, J.; Xiao, A.; Liu, L. Antibacterial activity of polyphenols: Structure-activity relationship and influence of hyperglycemic condition. Molecules 2017, 22, 1913. [Google Scholar] [CrossRef] [PubMed]
- Daglia, M. Polyphenols as antimicrobial agents. Curr. Opin. Biotechnol. 2012, 23, 174–181. [Google Scholar] [CrossRef]
- Li, F.; Fu, Y.; Yang, H.; Tang, Y. The inhibition mechanism of luteolin on peroxidase based on multispectroscopic techniques. Int. J. Biol. Macromol. 2021, 166, 1072–1081. [Google Scholar] [CrossRef]
- Funaro, A.; Wu, X.; Song, M.; Zheng, J.; Guo, S.; Rakariyatham, K.; Xiao, H. Enhanced anti-inflammatory activities by the combination of Luteolin and Tangeretin. J. Food Sci. 2016, 81, H1320–H1327. [Google Scholar] [CrossRef]
- Wang, S.; Fu, L.; Wu, Y.; Xiao, H.; Wang, J.; Sun, G. Influence of luteolin on the apoptosis of esophageal cancer Eca109 cells and its mechanism of action. Food Sci. Hum. Wellness 2019, 8, 189–194. [Google Scholar] [CrossRef]
- Imran, M.; Rauf, A.; Abu-Izneid, T.; Nadeem, M.; Shariati, M.A.; Khan, I.A.; Mubarak, M.S. Luteolin, a flavonoid, as an anticancer agent: A review. Biomed. Pharmacother. 2019, 112, 108612. [Google Scholar] [CrossRef]
- Gendrisch, F.; Esser, P.R.; Schempp, C.M.; Wölfle, U. Luteolin as a modulator of skin aging and inflammation. Biofactors 2021, 47, 170–180. [Google Scholar] [CrossRef] [PubMed]
- Tsakalidou, E. Detection of changes in the cellular composition of Salmonella enterica serovar Typhimurium in the presence of antimicrobial compound (s) of Lactobacillus strains using Fourier transform infrared spectroscopy. Int. J. Food Microbiol. 2010, 144, 202–207. [Google Scholar] [CrossRef]
- Qian, W.; Liu, M.; Fu, Y.; Zhang, J.; Liu, W.; Li, J.; Wang, T. Antimicrobial mechanism of luteolin against Staphylococcus aureus and Listeria monocytogenes and its antibiofilm properties. Microb. Pathog. 2020, 142, 104056. [Google Scholar] [CrossRef] [PubMed]
- Xiao, C.; Xia, M.L.; Wang, J.; Zhou, X.R.; Lou, Y.Y.; Tang, L.H.; Qian, L.B. Luteolin attenuates cardiac ischemia/reperfusion injury in diabetic rats by modulating Nrf2 antioxidative function. Oxidative Med. Cell Longev. 2019, 2019, 2719252. [Google Scholar] [CrossRef]
- He, Q.; Zhang, L.; Yang, Z.; Ding, T.; Ye, X.; Liu, D.; Guo, M. Antibacterial mechanisms of thyme essential oil nanoemulsions against Escherichia coli O157: H7 and Staphylococcus aureus: Alterations in membrane compositions and characteristics. Innov. Food Sci. Emerg. Technol. 2022, 75, 102902. [Google Scholar] [CrossRef]
- Wang, L.; Lin, L.; Guo, Y.; Long, J.; Mu, R.J.; Pang, J. Enhanced functional properties of nanocomposite film incorporated with EGCG-loaded dialdehyde glucomannan/gelatin matrix for food packaging. Food Hydrocoll. 2020, 108, 105863. [Google Scholar] [CrossRef]
- Richter, M.F.; Drown, B.S.; Riley, A.P.; Garcia, A.; Shirai, T.; Svec, R.L.; Hergenrother, P.J. Predictive compound accumulation rules yield a broad-spectrum antibiotic. Nature 2017, 545, 299–304. [Google Scholar] [CrossRef]
- Qiao, Y.; Xu, Y.; Liu, X.; Zheng, Y.; Li, B.; Han, Y.; Wu, S. Microwave assisted antibacterial action of Garcinia nanoparticles on Gram-negative bacteria. Nat. Commun. 2022, 13, 2461. [Google Scholar] [CrossRef]
- Li, K.; Guan, G.; Zhu, J.; Wu, H.; Sun, Q. Antibacterial activity and mechanism of a laccase-catalyzed chitosan–gallic acid derivative against Escherichia coli and Staphylococcus aureus. Food Control 2019, 96, 234–243. [Google Scholar] [CrossRef]
- Diao, W.R.; Hu, Q.P.; Zhang, H.; Xu, J.G. Chemical composition, antibacterial activity and mechanism of action of essential oil from seeds of fennel (Foeniculum vulgare Mill.). Food Control 2014, 35, 109–116. [Google Scholar] [CrossRef]
- Bajpai, V.K.; Sharma, A.; Baek, K.H. Antibacterial mode of action of Cudrania tricuspidata fruit essential oil, affecting membrane permeability and surface characteristics of food-borne pathogens. Food Control 2013, 32, 582–590. [Google Scholar] [CrossRef]
- Ning, Y.; Ma, M.; Zhang, Y.; Zhang, D.; Hou, L.; Yang, K.; Jia, Y. Antibacterial mechanism of sucrose laurate against Bacillus cereus by attacking multiple targets and its application in milk beverage. Food Res. Int. 2022, 154, 111018. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.G.; Bian, L.Q.; Zhu, Y.J.; Zhang, R.R.; Shao, S.Y.; Wu, Y.; Sun, H. Multifunctional alkyl ferulate esters as potential food additives: Antibacterial activity and mode of action against Listeria monocytogenes and its application on American sturgeon caviar preservation. Food Control 2019, 96, 390–402. [Google Scholar] [CrossRef]
- Li, Q.; Yu, S.; Han, J.; Wu, J.; You, L.; Shi, X.; Wang, S. Synergistic antibacterial activity and mechanism of action of nisin/carvacrol combination against Staphylococcus aureus and their application in the infecting pasteurized milk. Food Chem. 2022, 380, 132009. [Google Scholar] [CrossRef]
- Rao, S.Q.; Zhang, R.Y.; Chen, R.; Gao, Y.J.; Gao, L.; Yang, Z.Q. Nanoarchitectonics for enhanced antibacterial activity with Lactobacillus buchneri S-layer proteins-coated silver nanoparticles. J. Hazard. Mater. 2022, 426, 128029. [Google Scholar] [CrossRef]
- Wu, M.; Tian, L.; Fu, J.; Liao, S.; Li, H.; Gai, Z.; Gong, G. Antibacterial mechanism of Protocatechuic acid against Yersinia enterocolitica and its application in pork. Food Control 2022, 133, 108573. [Google Scholar] [CrossRef]
- Deepika, B.; Tiwari, M.; Tiwari, V. Molecular mechanism of antimicrobial activity of chlorhexidine against carbapenem-resistant Acinetobacter baumannii. PLoS ONE 2019, 14, e0224107. [Google Scholar] [CrossRef]
- Liu, M.; Liu, Y.; Cao, M.J.; Liu, G.M.; Chen, Q.; Sun, L.; Chen, H. Antibacterial activity and mechanisms of depolymerized fucoidans isolated from Laminaria japonica. Carbohydr. Polym. 2017, 172, 294–305. [Google Scholar] [CrossRef]
- Ji, S.H.; Ki, S.H.; Ahn, J.H.; Shin, J.H.; Hong, E.J.; Kim, Y.J.; Choi, E.H. Inactivation of Escherichia coli and Staphylococcus aureus on contaminated perilla leaves by Dielectric Barrier Discharge (DBD) plasma treatment. Arch. Biochem. Biophys. 2018, 643, 32–41. [Google Scholar] [CrossRef]
- Titaley, S. Formulasi dan Uji Efektifitas Sediaan Gel Ekstra Etanol Daun Mangrove Api-Api (Avicennia marina) sebagai Antiseptik Tangan. Pharmacon 2014, 3, 99–106. [Google Scholar] [CrossRef]
- Zong, X.; Zhang, X.; Bi, K.; Zhou, Y.; Zhang, M.; Qi, J.; Fu, M. Novel emulsion film based on gelatin/polydextrose/camellia oil incorporated with Lactobacillus pentosus: Physical, structural, and antibacterial properties. Food Hydrocoll. 2021, 121, 107063. [Google Scholar] [CrossRef]
- Han, Q.; Feng, L.; Zhang, Y.; Zhang, R.; Wang, G.; Zhang, Y. Effect of Juglone against Pseudomonas syringae pv Actinidiae Planktonic Growth and Biofilm Formation. Molecules 2021, 26, 7580. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Sun, Y.I.; Zheng, Z.; Zhang, X.; Song, K.; Jia, Z.; Xia, X. Antimicrobial activity of syringic acid against Cronobacter sakazakii and its effect on cell membrane. Food Chem. 2016, 197, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Choi, G.J.; Cho, K.Y. Correlation of Lipid Peroxidation in Botrytis c inerea Caused by Dicarboximide Fungicides with Their Fungicidal Activity. J. Agric. Food Chem. 1998, 46, 737–741. [Google Scholar] [CrossRef]
- He, Q.; Zhang, L.; Song, L.; Zhang, X.; Liu, D.; Hu, Y.; Guo, M. Inactivation of Staphylococcus aureus using ultrasound in combination with thyme essential oil nanoemulsions and its synergistic mechanism. LWT 2021, 147, 111574. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, Q.; Li, H.; Qiu, Z.; Yu, Y. Comparative Assessment of the Antibacterial Efficacies and Mechanisms of Different Tea Extracts. Foods 2022, 11, 620. [Google Scholar] [CrossRef]
- Yang, Z.; He, Q.; Ismail, B.B.; Hu, Y.; Guo, M. Ultrasonication induced nano-emulsification of thyme essential oil: Optimization and antibacterial mechanism against Escherichia coli. Food Control 2022, 133, 108609. [Google Scholar] [CrossRef]
- Su, M.; Liu, F.; Luo, Z.; Wu, H.; Zhang, X.; Wang, D.; Miao, Y. The antibacterial activity and mechanism of chlorogenic acid against foodborne pathogen Pseudomonas aeruginosa. Foodborne Pathog. Dis. 2019, 16, 823–830. [Google Scholar] [CrossRef]

| Organism | LUT Concentration (μg/mL) | ||
|---|---|---|---|
| MIC Value | MBC Value | MIC/MBC Ratio | |
| S. aureus | 312.5 | 625 | 0.5 |
| E. coli | 312.5 | 625 | 0.5 |
| Concentration (μg/mL) | Nucleic Acids (OD260 nm) | Protein (μg/mL) | ||
|---|---|---|---|---|
| E. coli | S. aureus | E. coli | S. aureus | |
| 0 | 0.26 ± 0.004 d | 0.22 ± 0.003 d | 1.12 ± 0.09 d | 1.46 ± 0.05 d |
| 312.5 | 0.28 ± 0.002 c | 0.27 ± 0.004 c | 7.27 ± 0.25 c | 9.05 ± 0.10 c |
| 625 | 0.31 ± 0.002 b | 0.29 ± 0.007 b | 10.66 ± 0.69 b | 11.15 ± 0.29 b |
| 1250 | 0.34 ± 0.001 a | 0.33 ± 0.006 a | 20.49 ± 0.59 a | 21.68 ± 0.20 a |
| Group | S. aureus (mm) | E. coli (mm) |
|---|---|---|
| L1 | 31.64 ± 0.13 a | 25.54 ± 0.12 b |
| L2 | 25.84 ± 0.39 b | 22.72 ± 0.23 c |
| S | 32.88 ± 0.45 a | 29.71 ± 0.61 a |
| Analysis | LUT Antibacterial Hand Sanitizer | ||
|---|---|---|---|
| pH value | 5.6 ± 0.18 | ||
| Cold resistance stability | Not solidified | ||
| Heat resistance stability | Not discolored | ||
| Color | L*: 98.34 ± 0.46 | a*: −2.57 ± 0. 59 | b*: 8.24 ± 0.28 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xi, M.; Hou, Y.; Wang, R.; Ji, M.; Cai, Y.; Ao, J.; Shen, H.; Li, M.; Wang, J.; Luo, A. Potential Application of Luteolin as an Active Antibacterial Composition in the Development of Hand Sanitizer Products. Molecules 2022, 27, 7342. https://doi.org/10.3390/molecules27217342
Xi M, Hou Y, Wang R, Ji M, Cai Y, Ao J, Shen H, Li M, Wang J, Luo A. Potential Application of Luteolin as an Active Antibacterial Composition in the Development of Hand Sanitizer Products. Molecules. 2022; 27(21):7342. https://doi.org/10.3390/molecules27217342
Chicago/Turabian StyleXi, Meihua, Yujie Hou, Ruolin Wang, Minhui Ji, Yingying Cai, Jingfang Ao, Heyu Shen, Mei Li, Jun Wang, and Anwei Luo. 2022. "Potential Application of Luteolin as an Active Antibacterial Composition in the Development of Hand Sanitizer Products" Molecules 27, no. 21: 7342. https://doi.org/10.3390/molecules27217342
APA StyleXi, M., Hou, Y., Wang, R., Ji, M., Cai, Y., Ao, J., Shen, H., Li, M., Wang, J., & Luo, A. (2022). Potential Application of Luteolin as an Active Antibacterial Composition in the Development of Hand Sanitizer Products. Molecules, 27(21), 7342. https://doi.org/10.3390/molecules27217342







