Trend and Cancer-Specific Prevalence of Kidney Stones Among US Cancer Survivors, 2007–2020
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Diagnosis of Cancer
2.3. Assessment of Kidney Stones
2.4. Sociodemographic Characteristics, Lifestyle Factors, and Chronic Conditions
2.5. Statistical Analyses
3. Results
3.1. Trend and Prevalence of Kidney Stones in Cancer Survivors and Non-Cancer Adults
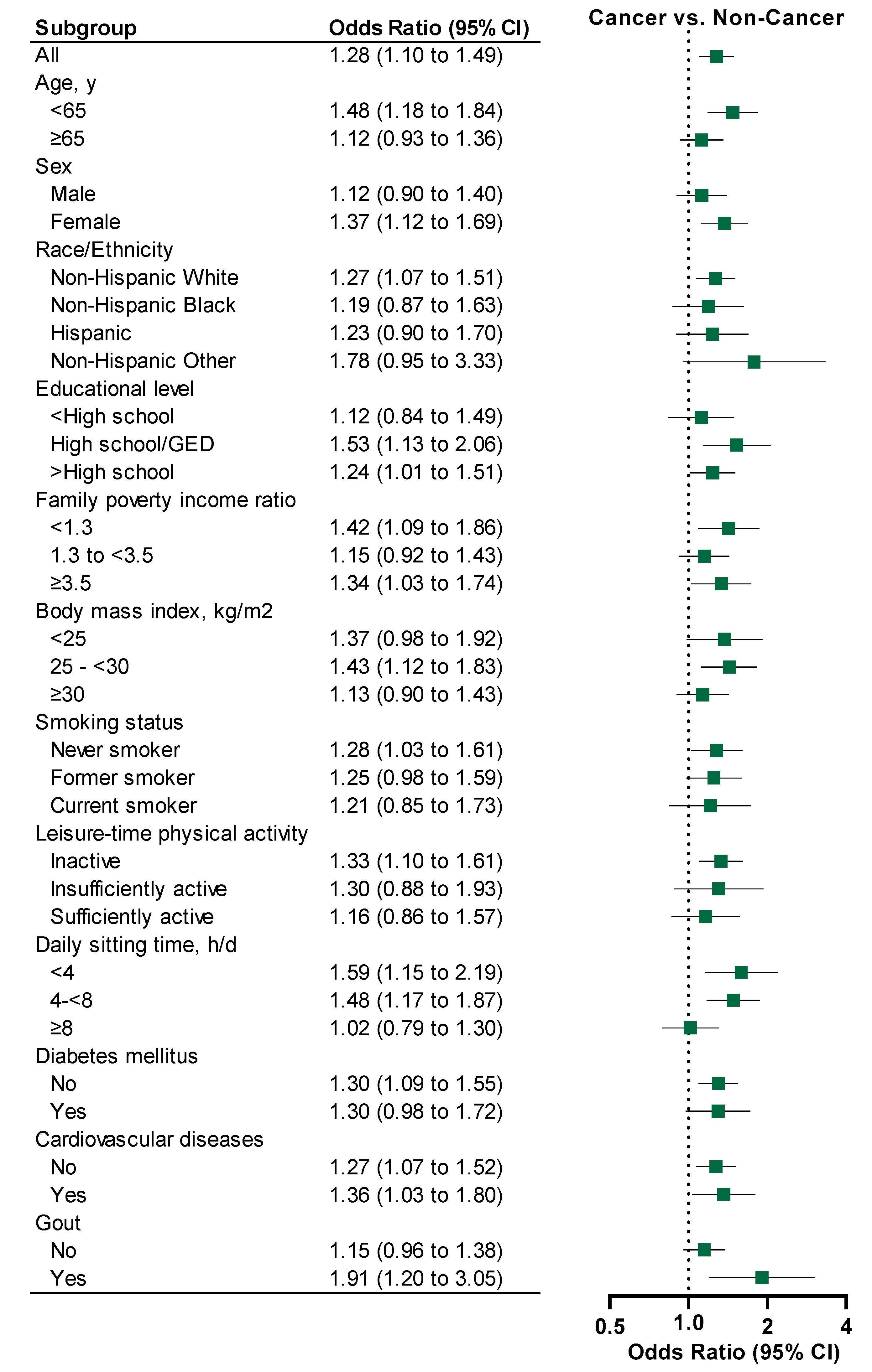
3.2. Kidney Stones and Sociodemographic, Lifestyle Factors and Chronic Conditions
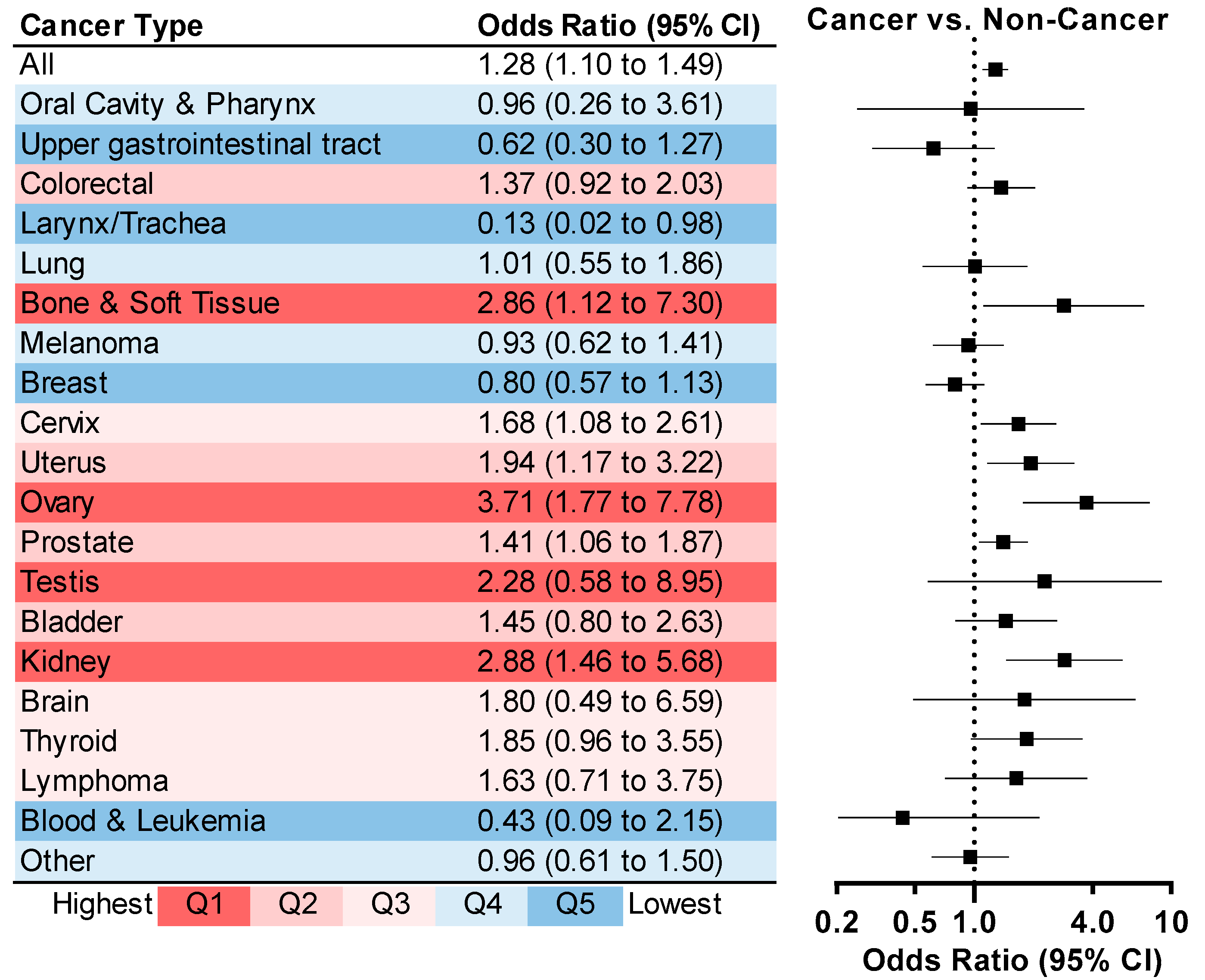
3.3. Cancer-Specific Patterns of Kidney Stones
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tonorezos, E.; Devasia, T.; Mariotto, A.B.; Mollica, M.A.; Gallicchio, L.; Green, P.; Doose, M.; Brick, R.; Streck, B.; Reed, C.; et al. Prevalence of cancer survivors in the United States. JNCI J. Natl. Cancer Inst. 2024, 116, 1784–1790. [Google Scholar] [CrossRef]
- Shapiro, C.L. Cancer survivorship. N. Engl. J. Med. 2018, 379, 2438–2450. [Google Scholar] [CrossRef]
- Lustberg, M.B.; Reinbolt, R.E.; Shapiro, C.L. Bone Health in Adult Cancer Survivorship. J. Clin. Oncol. 2012, 30, 3665–3674. [Google Scholar] [CrossRef]
- de Haas, E.C.; Oosting, S.F.; Lefrandt, J.D.; Wolffenbuttel, B.H.R.; Sleijfer, D.T.; Gietema, J.A. The metabolic syndrome in cancer survivors. Lancet Oncol. 2010, 11, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Wang, Q.; Wanchoo, R.; Eswarappa, M.; Deshpande, P.; Sise, M.E. Chronic Kidney Disease in Cancer Survivors. Adv. Chronic Kidney Dis. 2021, 28, 469–476.e1. [Google Scholar] [CrossRef] [PubMed]
- Ligibel, J. Lifestyle Factors in Cancer Survivorship. J. Clin. Oncol. 2012, 30, 3697–3704. [Google Scholar] [CrossRef] [PubMed]
- Holmes, H.M.; Nguyen, H.T.; Nayak, P.; Oh, J.H.; Escalante, C.P.; Elting, L.S. Chronic conditions and health status in older cancer survivors. Eur. J. Intern. Med. 2014, 25, 374–378. [Google Scholar] [CrossRef]
- van de Pol, J.A.A.; van den Brandt, P.A.; Schouten, L.J. Kidney stones and the risk of renal cell carcinoma and upper tract urothelial carcinoma: The Netherlands Cohort Study. Br. J. Cancer 2019, 120, 368–374. [Google Scholar] [CrossRef]
- Chow, W.-H.; Gridley, G.; Linet, M.S.; Pennello, G.A.; Fraumeni, J.F., Jr.; Lindblad, P.; Nyrén, O.; McLaughlin, J.K.; Adami, H.-O. Risk of Urinary Tract Cancers Following Kidney or Ureter Stones. JNCI J. Natl. Cancer Inst. 1997, 89, 1453–1457. [Google Scholar] [CrossRef]
- Malyszko, J.; Tesarova, P.; Capasso, G.; Capasso, A. The link between kidney disease and cancer: Complications and treatment. Lancet 2020, 396, 277–287. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention; National Center for Health Statistics. NHANES Survey Methods and Analytic Guidelines. Available online: https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx (accessed on 27 July 2025).
- Cao, C.; Patel, A.V.; Liu, R.; Cao, Y.; Friedenreich, C.M.; Yang, L. Trends and cancer-specific patterns of physical activity, sleep duration, and daily sitting time among US cancer survivors, 1997–2018. JNCI J. Natl. Cancer Inst. 2023, 115, 1563–1575. [Google Scholar] [CrossRef]
- Abufaraj, M.; Xu, T.; Cao, C.; Waldhoer, T.; Seitz, C.; D’andrea, D.; Siyam, A.; Tarawneh, R.; Fajkovic, H.; Schernhammer, E.; et al. Prevalence and Trends in Kidney Stone Among Adults in the USA: Analyses of National Health and Nutrition Examination Survey 2007–2018 Data. Eur. Urol. Focus 2021, 7, 1468–1475. [Google Scholar] [CrossRef]
- Jun, S.; Cowan, A.E.; Tooze, J.A.; Gahche, J.J.; Dwyer, J.T.; Eicher-Miller, H.A.; Bhadra, A.; Guenther, P.M.; Potischman, N.; Dodd, K.W. Dietary supplement use among US children by family income, food security level, and nutrition assistance program participation status in 2011–2014. Nutrients 2018, 10, 1212. [Google Scholar] [CrossRef]
- Torres da Costa e Silva, V.; Costalonga, E.C.; Coelho, F.O.; Caires, R.A.; Burdmann, E.A. Assessment of Kidney Function in Patients With Cancer. Adv. Chronic Kidney Dis. 2018, 25, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Dieffenbach, B.V.; Liu, Q.; Murphy, A.J.; Stein, D.R.; Wu, N.; Madenci, A.L.; Leisenring, W.M.; Kadan-Lottick, N.S.; Christison-Lagay, E.R.; Goldsby, R.E.; et al. Late-onset kidney failure in survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Eur. J. Cancer 2021, 155, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Lane, B.R.; Demirjian, S.; Derweesh, I.H.; Takagi, T.; Zhang, Z.; Velet, L.; Ercole, C.E.; Fergany, A.F.; Campbell, S.C. Survival and Functional Stability in Chronic Kidney Disease Due to Surgical Removal of Nephrons: Importance of the New Baseline Glomerular Filtration Rate. Eur. Urol. 2015, 68, 996–1003. [Google Scholar] [CrossRef]
- Eisenberg, M.S.; Thompson, R.H.; Frank, I.; Kim, S.P.; Cotter, K.J.; Tollefson, M.K.; Kaushik, D.; Thapa, P.; Tarrell, R.; Boorjian, S.A. Long-Term Renal Function Outcomes after Radical Cystectomy. J. Urol. 2014, 191, 619–625. [Google Scholar] [CrossRef]
- Miller, K.D.; Nogueira, L.; Devasia, T.; Mariotto, A.B.; Yabroff, K.R.; Jemal, A.; Kramer, J.; Siegel, R.L. Cancer treatment and survivorship statistics, 2022. CA Cancer J. Clin. 2022, 72, 409–436. [Google Scholar] [CrossRef]
- Tsimberidou, A.-M.; Keating, M.J. Hyperuricemic syndromes in cancer patients. Hyperuricemic Syndr.Pathophysiol. Ther. 2005, 147, 47–60. [Google Scholar]
- Hahn, K.; Kanbay, M.; Lanaspa, M.A.; Johnson, R.J.; Ejaz, A.A. Serum uric acid and acute kidney injury: A mini review. J. Adv. Res. 2017, 8, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Sahni, V.; Choudhury, D.; Ahmed, Z. Chemotherapy-associated renal dysfunction. Nat. Rev. Nephrol. 2009, 5, 450–462. [Google Scholar] [CrossRef]
- Chorbińska, J.; Krajewski, W.; Zdrojowy, R. Urological complications after radiation therapy—Nothing ventured, nothing gained: A Narrative Review. Transl. Cancer Res. 2021, 10, 1096. [Google Scholar] [CrossRef]
- Goldberg, I.D.; Garnick, M.B.; Bloomer, W.D. Urinary tract toxic effects of cancer therapy. J. Urol. 1984, 132, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Coleman, R.E.; Rathbone, E.; Brown, J.E. Management of cancer treatment-induced bone loss. Nat. Rev. Rheumatol. 2013, 9, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Twycross, R. The risks and benefits of corticosteroids in advanced cancer. Drug Saf. 1994, 11, 163–178. [Google Scholar] [CrossRef] [PubMed]
- Paquette, I.M.; Solan, P.; Rafferty, J.F.; Ferguson, M.A.; Davis, B.R. Readmission for dehydration or renal failure after ileostomy creation. Dis. Colon Rectum 2013, 56, 974–979. [Google Scholar] [CrossRef]
- McGarvey, N.; Gitlin, M.; Fadli, E.; Chung, K.C. Increased healthcare costs by later stage cancer diagnosis. BMC Health Serv. Res. 2022, 22, 1155. [Google Scholar] [CrossRef]
- Fass, L. Imaging and cancer: A review. Mol. Oncol. 2008, 2, 115–152. [Google Scholar] [CrossRef]
- Pearle, M.S.; Goldfarb, D.S.; Assimos, D.G.; Curhan, G.; Denu-Ciocca, C.J.; Matlaga, B.R.; Monga, M.; Penniston, K.L.; Preminger, G.M.; Turk, T.M. Medical management of kidney stones: AUA guideline. J. Urol. 2014, 192, 316–324. [Google Scholar] [CrossRef]
- Türk, C.; Petřík, A.; Sarica, K.; Seitz, C.; Skolarikos, A.; Straub, M.; Knoll, T. EAU guidelines on diagnosis and conservative management of urolithiasis. Eur. Urol. 2016, 69, 468–474. [Google Scholar] [CrossRef]

| Non-Cancer Adults | Cancer Survivors | |||||
|---|---|---|---|---|---|---|
| Sample Size | Weighted | Prevalence of Kidney Stones, % (95% CI) | Sample Size | Weighted | Prevalence of Kidney Stones, % (95% CI) | |
| (Weighted%) | Population | (Weighted%) | Population | |||
| All | 40,395 (100) | 210,662,296 | 9.2 (8.8 to 9.6) | 3492 (100) | 17,607,772 | 15.8 (14.0 to 17.5) |
| Age, y | ||||||
| <65 | 31,571 (83.7) | 176,318,137 | 8.5 (8.1 to 9.0) | 1430 (48.9) | 8,607,366 | 16.4 (13.5 to 19.2) |
| ≥65 | 8824 (16.3) | 34,344,159 | 12.9 (11.9 to 13.9) | 2062 (51.1) | 9,000,406 | 15.2 (13.1 to 17.2) |
| Sex | ||||||
| Female | 20,696 (51.2) | 102,793,435 | 8.2 (7.7 to 8.8) | 1913 (60.3) | 6,992,471 | 13.5 (11.3 to 15.6) |
| Male | 19,699 (48.8) | 107,868,861 | 10.3 (9.7 to 10.9) | 1579 (39.7) | 10,615,301 | 19.2 (16.3 to 22.1) |
| Race/Ethnicity | ||||||
| Non-Hispanic White | 15,228 (64.1) | 24,750,299 | 10.6 (10.0 to 11.2) | 1999 (80.5) | 1,323,639 | 16.3 (14.3 to 18.4) |
| Non-Hispanic Black | 9243 (11.7) | 135,096,183 | 5.2 (4.7 to 5.7) | 677 (7.5) | 14,181,746 | 9.1 (6.8 to 11.5) |
| Hispanic | 10,287 (15.4) | 32,377,212 | 7.8 (7.2 to 8.3) | 538 (6.8) | 1,195,831 | 13.8 (10.5 to 17.1) |
| Non-Hispanic Other | 5637 (8.8) | 18,438,602 | 7.1 (6.1 to 8.0) | 278 (5.1) | 906,556 | 19.0 (9.3 to 28.7) |
| Educational level | ||||||
| <High school | 9637 (15.5) | 32,650,750 | 9.6 (8.8 to 10.4) | 773 (13.0) | 2,286,309 | 14.0 (11.0 to 17.1) |
| High school/GED | 9406 (23.8) | 50,188,198 | 9.3 (8.5 to 10.1) | 771 (22.1) | 3,893,987 | 16.9 (13.1 to 20.7) |
| >High school | 21,352 (60.7) | 127,823,348 | 9.1 (8.6 to 9.7) | 1948 (64.9) | 11,427,476 | 15.7 (13.4 to 18.0) |
| Family poverty income ratio | ||||||
| <1.3 | 11,521 (20.1) | 42,372,259 | 8.6 (7.9 to 9.2) | 848 (15.5) | 2,733,864 | 16.0 (12.8 to 19.2) |
| 1.3 to <3.5 | 18,097 (41.0) | 86,396,421 | 9.6 (9.0 to 10.2) | 1636 (42.6) | 7,504,040 | 15.3 (12.7 to 17.8) |
| ≥3.5 | 10,777 (38.9) | 81,893,616 | 9.2 (8.5 to 9.9) | 1008 (41.9) | 7,369,868 | 16.1 (13.1 to 19.2) |
| Body mass index, kg/m2 | ||||||
| <25 | 10,994 (28.3) | 59,567,866 | 6.4 (5.7 to 7.0) | 851 (24.3) | 4,270,207 | 12.0 (8.9 to 15.1) |
| 25–<30 | 14,377 (35.3) | 74,354,693 | 8.8 (8.2 to 9.5) | 1345 (38.1) | 6,705,309 | 15.8 (13.0 to 18.6) |
| ≥30 | 15,024 (36.4) | 76,739,737 | 11.9 (11.1 to 12.6) | 1296 (37.7) | 6,632,256 | 18.1 (15.1 to 21.1) |
| Smoking status | ||||||
| Never smoker | 23,178 (56.9) | 119,891,617 | 8.4 (7.9 to 9.0) | 1632 (47.6) | 8,377,508 | 15.3 (12.8 to 17.8) |
| Former smoker | 9104 (23.5) | 49,490,164 | 11.1 (10.2 to 12.0) | 1298 (36.3) | 6,399,613 | 16.9 (14.0 to 19.8) |
| Current smoker | 8113 (19.6) | 41,280,515 | 9.3 (8.5 to 10.2) | 562 (16.1) | 2,830,651 | 14.5 (10.3 to 18.7) |
| Leisure-time physical activity | ||||||
| Inactive | 21,352 (46.2) | 97,304,212 | 10.4 (9.8 to 11.0) | 2145 (54.9) | 9,660,756 | 17.0 (14.6 to 19.3) |
| Insufficiently active | 5801 (16.0) | 33,615,289 | 8.7 (7.7 to 9.8) | 445 (13.8) | 2,427,753 | 15.8 (11.2 to 20.4) |
| Sufficiently active | 13,242 (37.9) | 79,742,795 | 8.1 (7.4 to 8.7) | 902 (31.3) | 5,519,263 | 13.6 (10.5 to 16.7) |
| Daily sitting time, h/d | ||||||
| <4 | 11,862 (25.1) | 52,795,175 | 8.8 (8.1 to 9.6) | 741 (18.7) | 3,298,830 | 17.1 (13.0 to 21.1) |
| 4–<8 | 15,882 (39.8) | 83,854,203 | 9.0 (8.4 to 9.7) | 1515 (41.9) | 7,384,669 | 17.0 (14.1 to 19.9) |
| ≥8 | 12,651 (35.1) | 74,012,918 | 9.8 (9.0 to 10.5) | 1236 (39.3) | 6,924,273 | 13.8 (11.3 to 16.3) |
| Diabetes mellitus | ||||||
| No | 35,164 (90.6) | 190,925,231 | 8.4 (8.0 to 8.8) | 2701 (81.7) | 14,389,302 | 14.4 (12.5 to 16.3) |
| Yes | 5231 (9.4) | 19,737,065 | 17.1 (15.5 to 18.7) | 791 (18.3) | 3,218,470 | 21.9 (17.7 to 26.1) |
| Cardiovascular diseases | ||||||
| No | 36,227 (92.1) | 194,017,838 | 8.6 (8.2 to 9.0) | 2619 (79.1) | 13,924,477 | 14.5 (12.6 to 16.4) |
| Yes | 4168 (7.9) | 16,644,458 | 16.5 (14.9 to 18.1) | 873 (20.9) | 3,683,295 | 20.4 (16.4 to 24.3) |
| Gout | ||||||
| No | 30,598 (82.0) | 172,784,482 | 9.0 (8.5 to 9.4) | 2393 (75.0) | 13,212,348 | 13.9 (12.0 to 15.8) |
| Yes | 1385 (3.1) | 6,590,860 | 16.9 (14.1 to 19.7) | 268 (7.3) | 1,276,682 | 30.6 (22.0 to 39.3) |
| Odds Ratio (95% CI) | p for Interaction c | ||
|---|---|---|---|
| Non-Cancer Adults (N = 40,395) | Cancer Survivors b (N = 3492) | ||
| Age, y | 1.02 (1.01 to 1.02) | 0.99 (0.98 to 1.01) | <0.001 |
| Sex | |||
| Female | 1 [Reference] | 1 [Reference] | 0.450 |
| Male | 1.51 (1.28 to 1.78) | 3.48 (2.08 to 5.81) | |
| Race/Ethnicity | |||
| Non-Hispanic White | 1 [Reference] | 1 [Reference] | 0.067 |
| Non-Hispanic Black | 0.45 (0.39 to 0.50) | 0.43 (0.30 to 0.62) | |
| Hispanic | 0.76 (0.67 to 0.85) | 0.75 (0.52 to 1.08) | |
| Non-Hispanic Other | 0.73 (0.62 to 0.86) | 1.10 (0.63 to 1.93) | |
| Educational level | |||
| <High school | 1 [Reference] | 1 [Reference] | 0.766 |
| High school/GED | 0.96 (0.83 to 1.11) | 1.19 (0.82 to 1.74) | |
| >High school | 1.05 (0.92 to 1.20) | 1.18 (0.84 to 1.67) | |
| Family poverty income ratio | |||
| <1.3 | 1 [Reference] | 1 [Reference] | 0.770 |
| 1.3 to <3.5 | 1.01 (0.90 to 1.13) | 0.83 (0.59 to 1.16) | |
| ≥3.5 | 0.93 (0.82 to 1.07) | 0.95 (0.64 to 1.42) | |
| Body mass index, kg/m2 | |||
| <25 | 1 [Reference] | 1 [Reference] | 0.279 |
| 25–<30 | 1.30 (1.13 to 1.49) | 1.30 (0.90 to 1.89) | |
| ≥30 | 1.76 (1.54 to 2.01) | 1.31 (0.90 to 1.92) | |
| Smoking status | |||
| Never smoker | 1 [Reference] | 1 [Reference] | 0.741 |
| Former smoker | 1.00 (0.88 to 1.12) | 0.97 (0.72 to 1.30) | |
| Current smoker | 1.14 (1.00 to 1.30) | 0.79 (0.51 to 1.24) | |
| Leisure-time physical activity | |||
| Inactive | 1 [Reference] | 1 [Reference] | 0.899 |
| Insufficiently active | 0.91 (0.78 to 1.05) | 0.85 (0.56 to 1.30) | |
| Sufficiently active | 0.92 (0.82 to 1.04) | 0.66 (0.48 to 0.93) | |
| Daily sitting time, h/d | |||
| <4 | 1 [Reference] | 1 [Reference] | 0.018 |
| 4–<8 | 0.91 (0.80 to 1.03) | 0.97 (0.67 to 1.41) | |
| ≥8 | 0.97 (0.85 to 1.10) | 0.69 (0.47 to 1.02) | |
| Diabetes mellitus | |||
| No | 1 [Reference] | 1 [Reference] | 0.298 |
| Yes | 1.55 (1.35 to 1.78) | 1.44 (1.06 to 1.96) | |
| Cardiovascular diseases | |||
| No | 1 [Reference] | 1 [Reference] | 0.550 |
| Yes | 1.26 (1.09 to 1.46) | 1.29 (0.95 to 1.76) | |
| Gout | |||
| No | 1 [Reference] | 1 [Reference] | 0.237 |
| Yes | 1.29 (1.05 to 1.60) | 2.28 (1.49 to 3.49) | |
| Pregnancy (female only) | |||
| Never | 1 [Reference] | 1 [Reference] | 0.929 |
| Ever | 1.23 (1.03 to 1.46) | 2.12 (1.29 to 3.50) | |
| Hormone therapy (female only) | |||
| Never | 1 [Reference] | 1 [Reference] | 0.547 |
| Ever | 1.08 (0.90 to 1.30) | 1.57 (1.06 to 2.31) | |
| Non-Cancer Adults (N = 40,395) | Cancer Survivors (N = 3492) | |
|---|---|---|
| Prevalence of Kidney Stone | Prevalence of Kidney Stone | |
| Weighted% (95% CI) | Weighted% (95% CI) | |
| All | 9.4 (9.0 to 9.9) | 16.7 (14.8 to 18.5) |
| Age, y | ||
| <65 | 9.4 (8.9 to 9.9) | 16.5 (14.4 to 18.6) |
| ≥65 | 9.7 (8.5 to 10.9) | 16.8 (14.9 to 18.7) |
| Sex | ||
| Male | 12 (11.1 to 12.8) | 19.6 (17.5 to 21.7) |
| Female | 7.1 (6.4 to 7.7) | 14.7 (12.8 to 16.6) |
| Race/Ethnicity | ||
| Non-Hispanic White | 10.9 (10.3 to 11.5) | 17.5 (15.6 to 19.4) |
| Non-Hispanic Black | 4.4 (3.8 to 5.0) | 11.0 (9.1 to 13.0) |
| Hispanic | 7.8 (7.0 to 8.5) | 14.4 (12.3 to 16.4) |
| Non-Hispanic Other | 8 (6.8 to 9.3) | 14.6 (12.3 to 17.0) |
| Educational level | ||
| <High school | 9.2 (8.1 to 10.2) | 16.3 (14.3 to 18.4) |
| High school/GED | 8.6 (7.7 to 9.5) | 15.8 (13.7 to 17.8) |
| >High school | 9.8 (9.3 to 10.4) | 17.0 (15.1 to 18.9) |
| Family poverty income ratio | ||
| <1.3 | 8.9 (8.2 to 9.7) | 16.1 (14.1 to 18.1) |
| 1.3 to <3.5 | 9.6 (9.0 to 10.3) | 16.8 (14.9 to 18.8) |
| ≥3.5 | 9.5 (8.7 to 10.3) | 16.7 (14.7 to 18.7) |
| Body mass index, kg/m2 | ||
| <25 | 7.1 (6.4 to 7.8) | 14.2 (12.2 to 16.2) |
| 25–< 30 | 9.3 (8.5 to 10) | 16.4 (14.4 to 18.3) |
| ≥30 | 11.4 (10.6 to 12.2) | 18.5 (16.5 to 20.4) |
| Smoking status | ||
| Never smoker | 9.1 (8.5 to 9.6) | 16.2 (14.3 to 18.2) |
| Former smoker | 9.9 (9.0 to 10.8) | 17.0 (15.0 to 19.0) |
| Current smoker | 10.0 (9.0 to 11.0) | 17.1 (15.0 to 19.2) |
| Leisure-time physical activity | ||
| Inactive | 10.2 (9.5 to 10.9) | 17.3 (15.4 to 19.2) |
| Insufficiently active | 8.5 (7.5 to 9.6) | 15.6 (13.5 to 17.7) |
| Sufficiently active | 8.9 (8.2 to 9.6) | 16.0 (14.1 to 18.0) |
| Daily sitting time, h/d | ||
| <4 | 9.9 (9.1 to 10.7) | 17.2 (15.1 to 19.2) |
| 4–< 8 | 9.2 (8.5 to 9.9) | 16.5 (14.5 to 18.4) |
| ≥8 | 9.4 (8.7 to 10.1) | 16.6 (14.7 to 18.6) |
| Diabetes mellitus | ||
| No | 8.9 (8.4 to 9.3) | 15.6 (13.7 to 17.5) |
| Yes | 15.0 (13.3 to 16.6) | 21.7 (19.3 to 24.0) |
| Cardiovascular diseases | ||
| No | 9.1 (8.7 to 9.6) | 15.8 (13.9 to 17.7) |
| Yes | 13.1 (11.4 to 14.8) | 19.8 (17.4 to 22.2) |
| Gout | ||
| No | 9.2 (8.7 to 9.7) | 16.2 (14.3 to 18.0) |
| Yes | 15.3 (12.4 to 18.2) | 22.2 (18.8 to 25.7) |
| Cancer Type | N | Prevalence of Kidney Stone |
|---|---|---|
| Weighted population | Weighted% (95% CI) | |
| All | 3492 | 15.8 |
| 17,607,772 | (14.0 to 17.5) | |
| Oral Cavity and Pharynx | 26 | 14.5 |
| 149,406 | (0 to 30.5) | |
| Upper gastrointestinal tract | 117 | 8.0 |
| 456,521 | (2.7 to 13.2) | |
| Colorectal | 351 | 19.2 |
| 1,429,235 | (13.5 to 24.8) | |
| Larynx/Trachea | 22 | 1.7 |
| 103,778 | (0 to 5.3) | |
| Lung | 127 | 13.8 |
| 523,098 | (6.9 to 20.8) | |
| Bone and Soft Tissue | 37 | 29.9 |
| 171,209 | (8.0 to 51.8) | |
| Melanoma | 304 | 13.7 |
| 2,172,236 | (8.8 to 18.5) | |
| Breast | 693 | 10.2 |
| 3,909,645 | (7.3 to 13.2) | |
| Cervix | 258 | 16.3 |
| 1,639,971 | (10.2 to 22.3) | |
| Uterus | 195 | 21.8 |
| 983,724 | (13.1 to 30.4) | |
| Ovary | 115 | 29.8 |
| 632,493 | (15.6 to 44.0) | |
| Prostate | 710 | 20.8 |
| 2,512,044 | (16.4 to 25.2) | |
| Testis | 23 | 26.3 |
| 282,685 | (0 to 53.6) | |
| Bladder | 121 | 23.0 |
| 483,796 | (12.8 to 33.2) | |
| Kidney | 98 | 34.7 |
| 376,685 | (21.0 to 48.3) | |
| Brain | 24 | 16.1 |
| 106,609 | (0 to 35.1) | |
| Thyroid | 115 | 18.2 |
| 660,376 | (8.0 to 28.4) | |
| Lymphoma | 107 | 16.3 |
| 497,990 | (5.1 to 27.5) | |
| Blood and Leukemia | 73 | 5.6 |
| 383,075 | (0 to 14.2) | |
| Other | 272 | 12.9 |
| 1,659,134 | (7.7 to 18.1) |
| Cancer Type | Prevalence, Weighted% (95% CI) | |
|---|---|---|
| Male | Female | |
| All | 19.2 | 13.5 |
| (16.3 to 22.1) | (11.3 to 15.6) | |
| Oral Cavity and Pharynx | 29.3 | |
| (0.1 to 58.4) | ||
| Upper gastrointestinal tract | 4.5 | 11.5 |
| (1.0 to 8.1) | (1.4 to 21.5) | |
| Colorectal | 25.6 | 14.4 |
| (15.9 to 35.3) | (7.8 to 21) | |
| Larynx/Trachea | 1.8 | |
| (0 to 5.9) | ||
| Lung | 7.9 | 18.9 |
| (1.1 to 14.6) | (7.3 to 30.4) | |
| Bone and Soft Tissue | 34.3 | 20.3 |
| (5.1 to 63.4) | (0 to 50.3) | |
| Melanoma | 20.0 | 5.6 |
| (12.1 to 28.0) | (2 to 9.2) | |
| Breast | 10.3 | |
| (7.3 to 13.2) | ||
| Cervix | 16.3 | |
| (10.2 to 22.3) | ||
| Uterus | 21.8 | |
| (13.1 to 30.4) | ||
| Ovary | 29.8 | |
| (15.6 to 44.0) | ||
| Prostate | 20.8 | |
| (16.4 to 25.2) | ||
| Testis | 26.3 | |
| (0 to 53.6) | ||
| Bladder | 24.3 | 19.9 |
| (11.6 to 36.9) | (3.1 to 36.8) | |
| Kidney | 36.5 | 30.2 |
| (19.4 to 53.6) | (7.9 to 52.4) | |
| Brain | 17.8 | 14.7 |
| (0 to 56.1) | (0 to 37.1) | |
| Thyroid | 1.9 | 22.2 |
| (0 to 6) | (9.8 to 34.5) | |
| Lymphoma | 13.3 | 18.9 |
| (0 to 26.7) | (1.4 to 36.5) | |
| Blood and Leukemia | 0.7 | 16.1 |
| (0 to 2) | (0 to 41.1) | |
| Other | 15.8 | 9.8 |
| (7.1 to 24.5) | (4.3 to 15.3) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, C.; Wang, R.; Wang, X.; Abufaraj, M.; Waldhoer, T.; Gotto, G.T.; Shariat, S.F.; Yang, L. Trend and Cancer-Specific Prevalence of Kidney Stones Among US Cancer Survivors, 2007–2020. Curr. Oncol. 2025, 32, 498. https://doi.org/10.3390/curroncol32090498
Cao C, Wang R, Wang X, Abufaraj M, Waldhoer T, Gotto GT, Shariat SF, Yang L. Trend and Cancer-Specific Prevalence of Kidney Stones Among US Cancer Survivors, 2007–2020. Current Oncology. 2025; 32(9):498. https://doi.org/10.3390/curroncol32090498
Chicago/Turabian StyleCao, Chao, Ruixuan Wang, Xiangren Wang, Mohammad Abufaraj, Thomas Waldhoer, Geoffrey T. Gotto, Shahrokh F. Shariat, and Lin Yang. 2025. "Trend and Cancer-Specific Prevalence of Kidney Stones Among US Cancer Survivors, 2007–2020" Current Oncology 32, no. 9: 498. https://doi.org/10.3390/curroncol32090498
APA StyleCao, C., Wang, R., Wang, X., Abufaraj, M., Waldhoer, T., Gotto, G. T., Shariat, S. F., & Yang, L. (2025). Trend and Cancer-Specific Prevalence of Kidney Stones Among US Cancer Survivors, 2007–2020. Current Oncology, 32(9), 498. https://doi.org/10.3390/curroncol32090498






