Abstract
Episiotomy is a perineal incision enlarging the vaginal opening during labor, preventing severe perineal/vaginal/ano-rectal lacerations. We performed a systematic literature review (PRISMA guidelines; Pubmed, Scopus and Web of Science databases) of primary malignant tumors arising from the episiotomy site. Thirteen primary carcinomas were reported, mainly endometriosis-related histotypes (77%) (nine clear cell, CCC; one endometrioid, EC) with only two vulvar invasive squamous cell carcinomas and one adenoid cystic carcinoma of Bartholin’s gland. No sarcomas, melanomas or malignant trophoblastic tumors were described. Endometriosis was associated with tumors or reported in history (62%). Malignant transformation occurred 3 to 27 (mean 16) years after diagnosis of endometriosis. Patients were usually post-/peri-menopausal (eight cases, 61%) (age range: 31–70 years, mean 50). Imaging should exclude distant (0% in our series) or lymph node metastases (three cases, 23%), looking for potential invasion of vagina (five cases, 39%), anus (including sphincter) (four cases, 31%) and/or other deep pelvic soft tissues (five cases, 39%). All patients underwent surgery, except for a CCC-patient (only chemoradiation) subsequently progressing and dying of disease. Adjuvant chemotherapy and/or radiotherapy were administered to five (39%) cases, neoadjuvant therapy to four cases (31%). Globally, three (23%) cases recurred or progressed, and two-thirds (15%) died of disease (1 CCC, 1 EC). Radical surgery with lymph node status evaluation and eventual excision should be performed when possible. Chemotherapy and/or radiotherapy can be considered in an adjuvant and/or neoadjuvant setting (or as only treatment in inoperable patients). However, the role of different treatments should be studied in further larger multicenter series.
1. Introduction
Perineal trauma (PT) of any grade after vaginal delivery is a frequent event, involving about 90% of pregnant women, and it may be associated with short- and long-term morbidities (dyspareunia, persistent pain, pelvic floor disorders, depression, negative influence on mother’s ability to care for the newborns, etc.) [1,2,3,4]. The degree of PT-associated morbidity depends on laceration type, repair technique and materials, skill and knowledge of the birth attendant. Risk factors associated with second-degree PT include increased fetal birthweight, operative vaginal birth, prolonged second stage of labor, maternal birth position, and advanced maternal age [1,2,3,4].
Obstetrical anal sphincter injury significantly favor the development of anal incontinence (10% of cases with symptoms within a year from delivery), potentially having medicolegal implications with great impact on healthcare costs (£3.7–9.8 million from 2013 to 2014 in United Kingdom; approximately $83 million between 2007 and 2011 in the United States). Risk factors include induction or augmentation of labor, epidural, increased fetal birthweight, fetal malposition (occiput posterior), operative vaginal birth, midline episiotomy, primiparity and Asian ethnicity. Second-degree perineal tears are more common in primiparous women (incidence: 40%), similarly to obstetrical anal sphincter injury events (6% primiparous vs. 2% multiparous) [1,2,3,4].
Episiotomy is the incision of the perineum to enlarge the vaginal opening during the second stage of labor [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21]. It has a protective role in preventing severe perineal lacerations involving the anal sphincter (3rd-degree) and/or rectal mucosa (4th-degree) [1,2,3,4,5,19,20,21]. For these reasons, this procedure is widely used in Latin America, Europe and United States; however, some studies have identified adverse consequences of episiotomy, such as insufficient prevention of obstetric sphincter ani muscle injuries and hemorrhage [1,2,3,4,5,19,20,21]. Routine episiotomy practice may also increase the risk of major perineal injury according to other studies [1,2,3,4,5,19,20,21,22,23,24,25,26,27,28].
Therefore, the World Health Organization (WHO) and the American College of Obstetricians and Gynecologists (ACOG) have suggested that there are insufficient objective evidence-based criteria to recommend episiotomy as a routine practice, and that clinical judgment remains the best guide for using this procedure; in association with forceps or vacuum delivery, mediolateral episiotomy may have a lower risk of anal sphincter injury than midline episiotomy, but it is associated with an increased likelihood of long-term perineal pain and dyspareunia [29,30,31,32]. Despite these warnings, the prevalence of episiotomy varies widely between countries, from the lowest rate (9.7%) in Sweden to the highest one (100%) in Taiwan according to some studies [33,34].
Pregnancy may also favor the development of new tumors or the malignant transformation of benign conditions such as endometriosis [22,23,24,25,26].
Although rare, benign or malignant tumors have been described to arise from or recur in the episiotomy scar site [6,7,8,9,10,11,12,13,14,15,16,17,18]. In this paper, we have performed a systematic literature review to describe the features and associations of the primary malignant tumors arising from the episiotomy site.
2. Materials and Methods
2.1. Systematic Review of the Literature
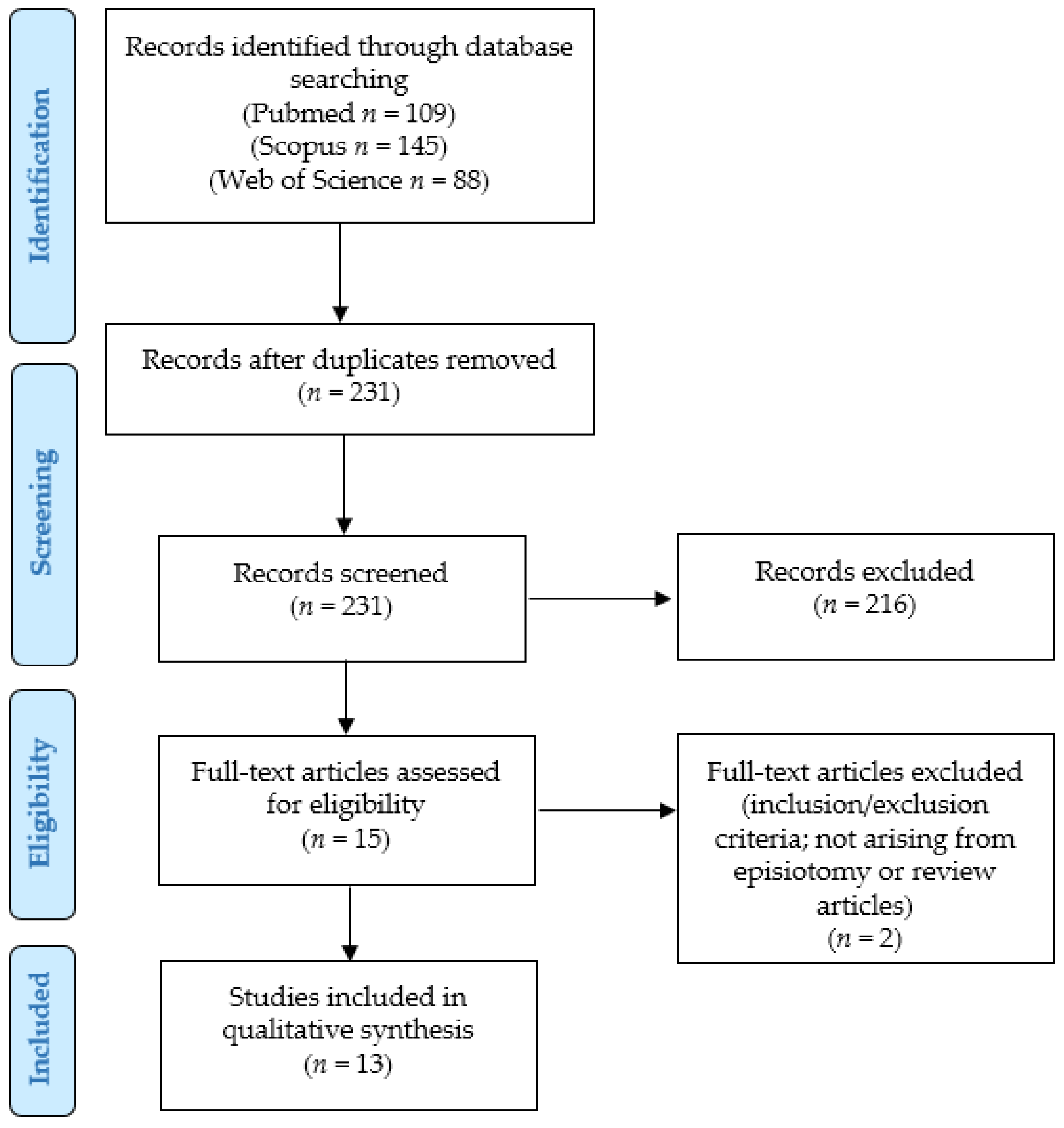
To identify primary malignant tumors arising from the episiotomy scar site, we conducted a systematic literature review according to the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) guidelines (http://www.prisma-statement.org/; accessed on 2 December 2024) and by using a retrospective observational approach (PICO process) (Figure 1):
Figure 1.
PRISMA flow-chart of our systematic literature review.
- Population: human patients with carcinomas primary arising from episiotomy site;
- Intervention: any;
- Comparison: none;
- Outcomes: clinical outcomes (status at last follow-up, and survival and recurrence rates).
We searched for (carcinoma OR carcinomas OR adenocarcinoma OR adenocarcinomas OR cancer OR sarcoma OR sarcomas OR melanoma OR melanomas OR “gestational trophoblastic” OR choriocarcinoma OR choriocarcinomas OR mole OR molar OR “epithelioid trophoblastic” OR “placental site tumor” OR “placental site tumors” OR “placental-site tumor” OR “placental-site tumors” OR “placental site trophoblastic tumor” OR “placental site trophoblastic tumors” OR “placental-site trophoblastic tumor” OR “placental-site trophoblastic tumors” OR “placental site nodule” OR “placental site nodules” OR “placental-site nodule” OR “placental-site nodules” OR “placental site trophoblastic nodule” OR “placental site trophoblastic nodules” OR “placental-site trophoblastic nodule” OR “placental-site trophoblastic nodules”) AND (episiotomies OR episiotomy) in Pubmed (all fields, 109 results; https://pubmed.ncbi.nlm.nih.gov, accessed on 2 December 2024), Scopus (Title/Abstract/Keywords, 145 results; https://www.scopus.com/home.uri, accessed on 2 December 2024) and Web of Science (Topic/Title, 88 results; www.webofknowledge.com, accessed on 2 December 2024) databases. No limitations were set. The bibliographic research ended on 30 June 2024. We applied the following criteria:
- Eligibility/inclusion criteria: studies describing cases of patients with primary malignant tumors arising in the episiotomy site.
- Exclusion criteria: unclear diagnosis; tumors not primarily arising on episiotomy; results not analyzable (too aggregated or scant data).
After the removal of duplicates, two independent authors read the titles and abstracts of all the retrieved results (n = 227). By applying the eligibility/inclusion and exclusion criteria, 15 articles were considered eligible; they were all obtained in full-text format and their reference lists were also screened to search for additional relevant articles. After reading the full-text, 2 papers were excluded as they reported primary vulvar cases not associated with episiotomy [27] or did not describe any additional case [28]; the remaining 13 articles were finally included in our study [6,7,8,9,10,11,12,13,14,15,16,17,18]. The extracted results were checked and confirmed by two other authors.
2.2. Statistical Analysis
Data collection was study- and case-related. Age of the patient, clinical symptoms, laboratory and diagnostic investigation such as imaging data, immunohistochemistry, histopathology, treatment, and follow-up information have been evaluated. Categorical variables were analyzed as frequencies and percentages, continuous variables by ranges and mean values.
Statistical analysis was performed using R Foundation for Statistical Computing (R-4.1.3, Vienna, Austria). Distribution of all the continuous variables was tested by the Shapiro test. Associations between clinical and pathological parameters were assessed by the Kruskal-Wallis test for continuous variables and Fisher’s exact test for categorical variables. The overall survival (OS) was computed as the time from the date of surgery to either the date of death or last follow-up, recurrence free survival (RFS) was computed as the time period from the date of surgery to either the date of recurrence or last follow-up. Survival analysis was performed applying by log-rank test. Associations were considered statistically significant for a p-value lower than 0.05.
3. Results
Globally, we identified 13 primary carcinomas arising from the episiotomy scar site (PriC) [6,7,8,9,10,11,12,13,14,15,16,17,18]. All of the studies reported just one case; the majority of PriCs were equally reported in Europe (n = 6; 3 United Kingdom [15,16,17], 1 France [12], 1 Hungary [13], 1 Croatia [14]) and Asia (n = 5; 2 Japan [6,9], 2 China [8,10], 1 Korea [11]), while 1 case was described in the United States [18] and Chile [7]. To our review, sarcomas, melanomas or gestational trophoblastic disease (including moles, choriocarcinomas, epithelioid trophoblastic tumors, placental site tumors/nodules) were not reported in association with episiotomy site.
3.1. Patient’s Age, Diagnosis and Association with Endometriosis
Globally, PriC patients’ age at presentation ranged from 31 to 70 (mean 50; median 53) years (Table 1) [6,18].

Table 1.
Primary carcinomas arising from the episiotomy scar site.
Non-gynecological history details included: 1 previous breast carcinoma (9 years before presentation) (treatment: radical mastectomy + chemotherapy) [8]; 1 hypertension, ischaemic heart disease and psychiatric disease [13]; 1 previous subtotal thyroidectomy for benign node and cholecystectomy [12].
Most of the 13 PriC were histotypes usually related to endometriosis (ERH) (n = 10, 77%), including 8 (62%) clear cell carcinomas (CCC) [6,7,8,9,10,11,15,18] and 1 (8%) endometrioid carcinoma (EC) [13]; the remaining case was diagnosed as a serous papillary cystadenocarcinoma but in our opinion, it was likely a CCC or an EC as it was associated with endometriotic foci (unlike serous carcinoma) and the reported immunophenotype did not exclude a CCC/EC (CD10, calretinin, Ki-67) (Table 1) [12].
Indeed, in eight (62%) cases [6,8,10,11,12,13,15,18], endometriosis was associated with the tumor (2 cases, 15%) [6,13], reported in patient’s history at the episiotomy site (1 case, 8%) [18] or both (5 cases, 39%) [10,11,12,15,18]. In two cases, there was evidence of a transitional dysplastic zone between CCC and endometriosis [8,10]. Time from delivery/episiotomy to the histological diagnosis (excision) of endometriosis ranged from 9 months to 12 years (mean 7 years, 83 months) [8,10,11,12,18]. Time from diagnosis of endometriosis to cancer presentation ranged from 3 to 27 years (mean 16 years, 190 months) [8,10,11,12,15,18]. Medical therapy for endometriosis was also administered in 4 cases (Danazol [8,12]; Mifesterone/Medroxy-progesterone acetate injectable suspension, DMPA, followed by mifesterone and Chinese traditional medicine [10]; leuprorelin acetate [11]).
No endometriosis in the three cases revealing endometriosis-independent carcinomas (EIC) (23%), including two vulvar invasive squamous cell carcinomas (VSCC, 15%) [16,17] and one adenoid cystic carcinoma of Bartholin’s gland (ACCBG) [14]. The latter patient had a history of marsupialization of left and right Bartholin’s gland abscesses (nine and seven years before presentation, respectively).
3.2. Obstetric History
Most of the patients (61%) were surely postmenopausal (2 cases, 15%; 70 years each) [9,13] or peri-/post-menopausal (6 cases, 46%; decade 50s years) [6,7,8,12,15,17], while five (39%) women were premenopausal (<45 years) (Table 1) [10,11,14,16,18].
Most of ERH patients delivered once (6 G1P1, 60%) [7,8,10,12,15,18] while four (40%) women were multiparous (3 G2P2 [6,9,11], 1 G3P3 [13]); conversely, two-thirds (67%) of EIC were multiparous (1 G2P2 [14], 1 G4P4 [17]) while one woman had at least one previous delivery [16].
Details about episiotomy were available for 8/13 (62%) cases (1 large [7]; 1 left anterior [8]; 2 left mediolateral [9,14]; 1 lateral [10]; 2 right mediolateral [11,18]; 1 right side of introitus [17]). Time from episiotomy to tumor presentation ranged from 3 months to 30 years (mean 20.7 years; median 22 years; available data in nine cases, all being CCCs except 1 ACCBG) [6,8,10,11,12,13,14,15,18]. Three patients had a previous forceps-assisted vaginal delivery [7,10,12].
A PAP smear was performed in one VSCC revealing severe dyskeratosis; recurrent smears with mild abnormalities were found in the previous 12 years [17].
3.3. Clinical Presentation
Clinical symptoms at tumor presentation included pain (five cases, 39%) [6,11,12,14,17] in the perineal/episiotomy/tumor area (one prolonged for 10 years [6]; one cyclic [11]; one severe and cyclic pain in seated position, for defecation/miction [12]; one for 18 months [17]; one painful nodule [14]), dyspareunia (two cases, 15%) (one permanent [12], one superficial for two years [16]), abnormal genital bleeding (three cases, 23%) [9,16,18] (one month [9]; one foul-smelling [18]), pruritus (two cases, 15%) [10,15] (one for six months [15]) and vulvar discomfort (one case) [10] (Table 2).

Table 2.
Primary carcinomas arising from the episiotomy scar site: clinical presentation, size and tumor site.
Information about tumor marker levels were available in 5/13 (39%) cases, all being ERHs [6,8,9,12,18]: CA125 serum levels were increased in one-fifth (20%) of cases (79.1 U/mL) [6,8,9,12,18], while CEA (n = 4) [6,8,9,18], CA19-9 (n = 4) [6,8,9,12], CA15-3 (n = 1) [12], SCC (n = 3) [6,8,9], AFP (n = 2) [8,18], HE4 (n = 1) [8], NSE (n = 1) [12] and ACE (n = 1) [12] levels were always normal.
In all the five cases reporting the clinical suspect, the tumor was misdiagnosed as a benign lesion (n = 3; one endometriosis [12], one granuloma [14], one granulation tissue [16]) or a malignant carcinoma of different origin (one anal fistula carcinoma probably as to the involvement of anal sphincter [6]; one Bartholin’s gland cancer, while it was an endometriosis-related CCC [7]).
All of the 13 patients discovered a tumor mass/lesion [6,7,8,9,10,11,12,13,14,15,16,17,18] one month to four years before presentation to clinicians (mean 15 months) (gradual appearing [6]; four years [8]; one month [9]; six months [15]; several months, ulcerated in recent six months [18]; three months [13]; two years [14]). The tumor was described as prominent/exophytic/polypoid [6,9,11,13], nodular [9,14,16,17], hemorrhagic/bleeding [9,11,13], ulcerated/depressed [11,18], with normal/smooth surface [7,9]. Consistency was solid [11,15], hard [12], firm [8,14], tender [17] or soft [8,10], while the tumor color was variably described as tan or red-tan [8], purple [10], bright pink, non-necrotic [13] or dark-reddish [9]. The lesions were well-demarcated/with clear boundaries [9,11], partially mobile [7] or showing infiltrative margins [8].
Globally, the tumor size ranged from 1 to 10 cm (mean 4.6 cm; median 3 cm) (available data in 12/13 cases) [6,7,8,9,10,11,12,13,14,15,17,18]; the mean size was larger for ERH cases (4.4 cm; range 1–10 cm; median 3.5 cm) than for EICs (2.9 cm) but just three cases of the second group gave analyzable data (1.3 cm, 3 cm and 4.5 cm, respectively) [6,7,8,9,10,11,12,13,14,15,17,18].
The tumor site was vulvar [9], perineal [8,10,15,18], vulvar-perineal [7] or vaginal [11,14], and in each case it was related to the episiotomy scar [6,7,8,9,10,11,12,13,14,15,16,17,18]. Six (46%) cases arose from the right side [6,7,11,12,17,18] (including two posterior primary sites) [7,11], while four (31%) tumors were mainly located on the left side [8,9,14,15] and one showed a 1-cm bilateral extension on each side from the midline fourchette [16] (unavailable data in two cases) [10,13].
To better define the tumor features, ultrasound examination (US) was performed in three (23%) cases [8,10,12], magnetic resonance imaging (MRI) in nine (69%) cases [6,7,9,11,12,13,15,18], computed tomography scans (CT) in five (38%) cases [7,8,9,15,18], positron emission tomography (PET) in one (8%) case (uptake 9.13) [9], and PET-CT in three (23%) cases [6,8,12].
Vaginal involvement was reported in five (39%) cases (one vaginal mass, posterior commissure/distal vagina [11]; two cases grew between vagina and anus [6,8]; one upper two-thirds of vagina [13]; one left vaginal introitus [14]), while anal invasion was reported in four (31%) cases (one invasion of anal sphincter/levator ani but involved mucosa [6]; one between the left region of the anus and vagina [8]; one involvement of external anal sphincter and anterolateral anal canal [15]; one right side of anus and distal digestive tract [12]) and five (39%) tumors extended to other deep pelvic soft tissues (one right ischio-anal fossa [7]; one ischio-rectal fossa [18]; two deep pelvis [8,13]; one rectovaginal pouch [15]).
3.4. Surgical Treatment and Lymph Node Status
Fine needle aspiration cytology of the tumor was performed in 1 case revealing an adenocarcinoma [6] (Table 3).

Table 3.
Primary carcinomas arising from the episiotomy scar site: lymph node status, surgical treatment, tumor recurrence and follow-up information.
Radical/wide surgery was performed in 12 (92%) cases [6,7,8,9,12,13,14,17] (one laparoscopic posterior pelvic exenteration including rectal resection, total mesorectal excision, perineal reconstruction with right gracilis musculocutaneous flap [6]; one with additional V-Y gluteal advancement flap [7]; one radical vulvar excision with skin graft [10]; one radical vaginectomy + wide vulvar excision with partial skin graft + total abdominal hysterectomy, TAH [11]; one also included Hartmann’s procedure, partial vaginectomy and bilateral salpingo-oophorectomy, BSO [15]; one radical vulvectomy [16]) (Table 3).
In three cases, previous gynecological surgery was performed, including TAH + BSO for leiomyomas (n = 1) (15 years before) [9], one TAH for adenomyosis and leiomyomas (7 years before) [15] and one prolapse surgery (laparoscopic suspension procedure + posterior vaginal colpoperineoplasty) (4 years before) [12].
In seven (54%) cases, the surgical margins were free of tumor [9,10,11,12,14,16,17] (unavailable data in the remaining cases).
Enlarged inguinal lymph nodes were found in four (31%) cases (two left [8,9], one bilateral [18], one unclear [6]); in two-quarters (50%) of cases, this enlargement was clinically evident [9,18] while it seemed identified only by MRI or CT in the two other patients which also revealed uptake of fluorodeoxyglucose (FDG) on PET/CT and metastases in the lymphadenectomy specimen [6,8]. Internal iliac lymph node enlargement was additionally identified by MRI in one case [6]. In 6/13 (46%) cases, lymph nodes were not enlarged [7,10,11,12,15,17] while data were unavailable in the remaining three cases [13,14,16].
FNAC was performed on inguinal lymph nodes in two (15%) cases [8,11]; one was suggestive for an epithelial neoplasm (subsequent lymphadenectomy was positive for metastasis) [8], while the second case was negative for neoplasia, but subsequent lymphadenectomy revealed a metastasis [11].
An inguinal lymph node was biopsied in four (31%) cases [6,9,12,18]: in all the cases, the biopsy result agreed with the following lymphadenectomy specimen. In particular, two cases revealed a metastatic carcinoma [6,18], and two biopsies were negative for neoplasia (one found endometriosis) [9,12].
Globally, inguinal lymphadenectomy (LND) was performed in seven (54%) cases [6,8,9,10,11,16,17] (three bilateral [6,8,16], one left LND + right inguinal lymph node biopsy [9], one right [11], one unclear side [10], one superficial and deep ipsilateral inguinofemoral [17]) while additional pelvic LND was carried out in two (15%) cases (one bilateral [6], one unclear site [11]).
3.5. Stage at Presentation
The pTNM/AJCC category was difficult to apply, as the pT category was not provided in any case, the endometriosis-related histotypes are unusual in the vulvar site, the descriptions were sometimes difficult to interpret, and it was sometimes unclear which could represent the primary site (vulva? vagina?).
Globally, three cases were pN+ (1 bilateral inguinal and right internal iliac [6], one bilateral superficial inguinal, one lymph node per site [8], one right inguinal lymph node biopsy [18]) and 4 (31%) cases were N0 [9,11,12,17], while data were unavailable in two cases (Table 3) [10,16]. In four (31%) cases, lymphovascular space invasion was not identified [9,11,14,16], while data were not available in the other cases. One tumor showed perineural invasion [14], but this information was not highlighted in the remaining cases.
Distant metastases at presentation were not reported in any case [6,7,8,9,10,11,12,13,14,15,16,17,18].
3.6. Neoadjuvant and Adjuvant Treatment
Four (31%) patients underwent neoadjuvant treatment with gonadotropin releasing hormones (Gn-RH) (one case) [12], chemotherapy (paclitaxel + cisplatin, one cycle) (one case) [10], chemotherapy (5-fluorouracil with leucovorin and oxaliplatin, mFOLFOX6) + panitumumab (seven courses) (one case, initially misdiagnosed as an anal fistula adenocarcinoma, achieving partial response) [6] or radiotherapy (RT) (19 fractions, then discontinued for severe skin reaction; partial response) [15].
While primary surgery was performed in 12 (92%) cases [6,7,8,9,12,13,14,17], one patient did not undergo surgery and only chemoradiation was administered achieving partial response; later, she progressed and died of disease [18].
Adjuvant chemotherapy was administered to three (23%) patients (one paclitaxel + carboplatin, four cycles [6]; paclitaxel + cisplatin, one cycle [10]; one carboplatin, weekly [12]) while adjuvant RT was performed in one of these cases (perineal area and inguinal LNs, 45 Gy in four weeks + interstitial application of iridium) [12] and in two other cases (unclear data; one month duration in one case) [8,13] (total: three cases, 23%).
3.7. Follow-Up
Follow-up data were available for all 13 cases, ranging from 5 to 30 (mean 11.7, median 11) months (Table 3) [6,7,8,9,10,11,12,13,14,15,16,17,18]. Globally, 3 (23%) cases recurred or progressed [13,14,18], while 10 (77%) cases did not recur [6,7,8,9,10,11,12,15,16,17].
Eight ERH cases and three EIC cases showed no evidence of disease from five to fifteen (mean 7.8) months [6,7,8,9,10,11,12,15] and eleven to thirteen (mean 12) months after diagnosis [14,16,17], respectively. One of these cases showed local recurrence after six months, but the patient was surgically treated with hemivulvectomy + left LND (pN0) followed by RT achieving complete response and being free of disease thirteen months after diagnosis [14].
Only two (15%) cases progressed (one CCC: locally and in the lungs, after twelve months [18]; one EC: unclear sites and timing [13]) and died of disease thirty months (CCC) [18] and twelve months (EC) [13] after diagnosis, respectively.
3.8. Immunohistochemical and Molecular Analysis
Immunohistochemistry was tested on six (43%) cases, including four CCC [6,7,8,9], the serous carcinoma (probable CCC) [12] and the ACCBG [14]. The following markers were positive in all the few tested ERH cases: PAX-8 (n = 3) [6,7,9], HNF1-β (n = 3) [6,8,9], CA125 (n = 1) [9], napsin (n = 1) [7], pan-cytokeratin and AMACR (n = 1) [8]. Hormone receptors are typically negative in CCCs, but can sometimes be positive: estrogen receptor (ER) resulted positive in both the tested cases [6,9], but the intensity and extension of staining was not completely clear. Conversely, progesterone receptor (PR) was negative in the only tested case [8], as well as GATA-3 [9], SALL-4 [9], PTEN [9], PAX-2 [9], AFP [9] and calretinin [12], while ARID1A was retained in one case [9] and another tumor has a CK7+/CK20− phenotype [6]. As expected, the two tested CCCs resulted in p53 wild-type [8,9], while an unclear positivity for p16 was reported in one of the two cases [8,9]. No clear data about Ki67 were available. CD10 was tested in three cases [6,9,12] but it was not always clear if positivity was evident in the tumor or in the endometriotic stroma.
Two CCC were examined by molecular analysis [6,9]. One case revealed no KRAS mutation [6], while no pathogenic/oncogenic mutations in 50 cancer-related genes (such as BRAF, EGFR, ERBB2, FBXW7, GNAS, HRAS, KIT, KRAS, NRAS, PIK3CA, PTEN, APC, CTNNB1, and TP53) were detected in the second case by targeted sequencing (Ion Ampliseq Cancer Hotspot panel version 2) [9].
The ACCBG case showed the following immunophenotype: EMA + (few luminal cells), pan-cytokeratin + (few luminal cells), smooth muscle actin + (basaloid peripheral cells), S100 (basaloid peripheral cells) ER −, PR − [14]. Moreover, flow cytometry was performed revealing a DNA diploid tumor with low S-phase fraction of 3.43% [14].
3.9. Statistical Analysis
All the following relevant variables were analyzed for association with histology (each histotype; ERH vs. EIC), OS and RFS: mean age, primiparous vs. multiparous, left/right side of episiotomy, endometriosis associated with tumor and/or present in history or absent, time from diagnosis of endometriosis to tumor presentation, time from episiotomy to tumor presentation, involvement of deep pelvis tissues, anus or vagina, enlarged lymph nodes, estimated pT stage, pN stage, radical surgical excision, lymphadenectomy, neoadjuvant treatment (Cht or RT), neoadjuvant Cht, neoadjuvant RT, adjuvant treatment (Cht or RT), adjuvant Cht, adjuvant RT, Cht (neoadjuvant or adjuvant), RT (neoadjuvant or adjuvant). Moreover, associations of histotype (ERH vs. EIC) with OS and RFS were investigated. However, no statistical significance was identified (p < 0.05) for all the statistical analyses, probably because of the low number of reported cases.
4. Discussion
In our review, we identified only 13 primary carcinomas arising from the episiotomy scar site [6,7,8,9,10,11,12,13,14,15,16,17,18] while no other malignant non-carcinomatous histotypes (such as sarcomas, melanomas or trophoblastic tumors, which rarely arise from extrauterine gynecologic organs) [35,36,37,38,39,40,41,42,43,44] resulted from our search to be associated with the episiotomy site.
The three endometriosis-independent histotypes arose one decade earlier if compared to ERHs (43 vs. 53 years) and may have been related to HPV infection (VSCC, 15%) [16,17] or chronic inflammation/stimulation of Bartholin’s glands (history of marsupialization for abscesses) (one ACCBG) [14]; representing exceptional events, they may be incidental findings not significantly associated with episiotomy.
Chronic inflammation and autoimmune diseases are well-known risk factors for tumor development as they facilitate tumor progression and treatment resistance, while acute inflammation stimulates dendritic cell maturation and antigen presentation, leading to anti-tumor immune responses [45,46].
Similarly, some reports suggested that HPV infection (not confirmed in our cases) may be associated with poor healing of the episiotomy repair, thus favoring chronic inflammation [47,48]. Moreover, episiotomy and Bartholin’s gland marsupialization may favor local inflammation and the arising of fistulae which may represent a chronic stimulus and/or cover the presence of an underlying neoplasm; however, it is difficult to speculate on the relevance of these features in our rarely reported cases [49,50].
Conversely, most (n = 10/13, 77%) of the described cases seemed to arise from a background of endometriosis [6,7,8,9,10,11,12,13,15,18], which was identified in association with the tumor or in history in the majority of cases (n = 8, 62%) [6,8,10,11,12,13,15,18]. These ERHs were typically CCCs, with just one EC [6,7,8,9,10,11,12,13,15,18]. Molecular and immunohistochemical data were too scant to classify these tumors according to the molecular classification proposed for the similar endometrial carcinoma histotypes [51,52,53,54,55,56].
Endometriosis is a chronic, estrogen-dependent, inflammatory disease defined by the implantation of ectopic endometrial glandular and stromal cells outside the uterine cavity [57,58,59,60,61,62,63,64,65,66,67,68]. Endometriosis affects about 5% to 15% of women, prevailing in the reproductive age (25–38%) and presenting with severe dysmenorrhea, dyspareunia, infertility and/or chronic pelvic pain; however, it can also continue to cause morbidities in post-menopausal women [49,50,51,52,53,54,55,56,57,58,59,60]. In our series, pain either in the vulvar-perineal/episiotomy/tumor (five cases, 39%) [6,11,12,14,17] or in the form of dyspareunia (two cases, 15%) [12,16] was the most common symptom, followed by abnormal genital bleeding (three cases, 23%) [9,16,18], pruritus (two cases, 15%) [10,15] and vulvar discomfort (one case) [10].
Endometriosis usually occurs in pelvic sites (ovaries, Fallopian tubes, peritoneum, uterine serosa, round ligament, uterosacral ligament, pouch of Douglas, rectovaginal septum, etc.) but it is not unusual to find endometriotic foci in upper abdomen (peritoneum, gastrointestinal or genitourinary tracts, etc.), while extra-abdominal sites may also be rarely involved (vulva, lymph nodes, thorax/lung/pleura, diaphragm, nervous system, mucocutaneous tissues, etc.) [57,58,59,60,61,62,63,64,65,66,67,68]. Globally, extrapelvic endometriosis seems to occur in about 20% of women with endometriosis [57,58].
In particular, vulvar-perineal endometriosis affects less than 1% of patients and it can be due to traumatic and/or iatrogenic seeding of endometrial tissue during vaginal deliveries, episiotomy (incidence: 0.03–0.15%) or other surgical or obstetrical procedures (cesarean section, myomectomy, hysterectomy) [23,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. In our series, time from delivery/episiotomy to the histological diagnosis of endometriosis ranged from 9 months to 12 years (mean 7 years, 83 months) [8,10,11,12,18]. The vulvo-perineal damaged mucosa can favor the implant of endometriotic foci. Viable endometrial tissue may also circulate into the peritoneal fluid. Rare cases maybe be spontaneous and unrelated to these risk factors potentially supporting the hypothesis of a lymphatic or hematogenous dissemination theory and/or the possibility of a direct extension of endometrial mucosa from the pelvis to the vulvo-perineal region through the round ligament/Nuck canal. Moreover, the cellular immunity theory suggests that a deficiency in immunity cells may favor the proliferation of ectopic endometrial tissue [57,58,59,60,61,62,63,64,65,66,67,68].
Luckily, malignant transformation of endometriosis is uncommon (1% of cases); this event is more frequent in the ovaries (80% of the endometriosis-associated malignancies) while it is extremely rare in extra-gonadal endometriosis [68,69,70,71,72,73,74,75,76,77,78,79,80,81].
Hyperestrogenism and long-lasting unopposed estrogen therapy (22 months to 17 years) may favor the malignant transformation of endometriosis, especially in case of estrogen-responsive ECs [69,73,74,75,76,77,78]. In contrast, the high physiological concentration of progesterone typical of pregnancy can antagonize the proliferation of estrogen-dependent tumor cells, a well-known mechanism that allows fertility to be preserved in endometrial cancer patients [82]. Thus, multiparous women have a lower risk of developing cancer; in our series, most of ERH patients delivered once (six cases, 60%) [7,8,10,12,15,18] while two-thirds (67%) of EIC were multiparous [14,17].
However, CCC commonly arises from endometriosis (4.5% of extragonadal ERHs) and typically show estrogen receptors (ERs) downregulation with lack the immunohistochemical ER expression; moreover, mesonephric-like adenocarcinomas, a rare new entity which also downregulate ER and PR, can also exceptionally arise from endometriosis [69,73,74,75,76,77,78,79,80,81,82,83,84]. In particular, in some series, CCCs represent the most frequent histotype [85]. Indeed, almost all of our ERHs were CCCs and most of the patients were surely postmenopausal (two cases, 15%) [9,13] or peri-/post-menopausal (six cases, 46%) [6,7,8,12,15,17], while five (39%) women were premenopausal (<45 years) [10,11,14,16,18].
The etiopathogenesis of these histotypes associated with endometriosis but not with ER expression is still under evaluation. Repeated bleeding of endometriosis during the menstrual cycle or retrograde menstruations cause changes in the microenvironment and carry highly pro-oxidant factors into the ovarian endometrioma or peritoneal cavity. In particular, this cyclic or persistent inflammation causes heme and redox active iron-mediated oxidative stress which modifies DNA, proteins and lipids, favoring DNA damage or loss of heterozygosity, as well as aberrant methylation of CpG islands or other epigenetic changes of a number of key regulatory genes. The loss of ER expression seems to be a result of the hypermethylation of the ER-α promoter. Other epigenetic events including histones deacetylation and methylation, and the effects of PPAR-γ and ubiquitin protein ligases, are involved in the complex mechanism regulating promoter transcription and driving stable gene expression modifications. The switch from a normal-stress-response phenotype to a stress-resistant phenotype may induce gene mutations (such as ARID1A, PIK3CA, PPP2R1A, KRAS, etc.) causing progression to CCC. Immune cell dysfunction and inflammation may play a role as well [86,87,88,89,90,91,92].
Malignant transformation of endometriosis seems to more frequently occur some years after the diagnosis of endometriosis. A systematic review of abdominal wall endometriosis found that time between first surgery to malignant transformation ranged from 4 to 41 (mean 19.9) years [85], while in our series time from diagnosis of endometriosis to cancer presentation ranged from 3 to 27 (mean 16) years [8,10,11,12,15,18].
Especially in patients with a history endometriosis, the appearance of a new nodule at the site of episiotomy or an increase in size of a pre-existing small lesion could represent a benign (inflammatory or endometriotic) lesion; indeed, three cases of our series presented with this clinical suspect [12,14,16]. However, an accurate gynecological investigation should be performed in these women with vulvo-vaginal-perineal cyclic pain or nodules, to prevent potential complications such as malignant transformation. Not all endometriotic lesions need to be resected but follow-up and biopsy of selected cases may be considered; a complete resection (achieving free resection margins) of endometriotic nodules increasing in size, long-standing, with persistent symptoms and/or resistant to medical therapy, can be recommended to reduce the risk of persistence and recurrence, as well as the rare possibility of malignant transformation [81,93].
Some studies reported that cancers associated with endometriosis have a better prognosis than those not associated [80,94]; only two (15%) of our cases progressed and died but larger series are needed as, unfortunately, our sample size was too small.
All primary vulvar carcinomas may potentially involve the episiotomy site, and the rarity of some episiotomy-associated tumors could not exclude incidental findings as abovementioned [14,16,17,47,48,49,50,95]. One CCC of our series was clinically suspected to represent a Bartholin’s gland cancer [7].
Moreover, cancers arising from other organs (gastro-intestinal, gynecological, genitourinary tracts, breast, etc.) may rarely metastasize (synchronously or metachronously) to unusual sites, including the vulva, sometimes mimicking a primary Paget’s disease or revealing the subtle primary origin after careful clinical and imaging investigations [95,96,97,98,99,100,101,102,103,104,105,106,107,108]; conversely, vulvar cancers may also metastasize to uncommon sites, potentially mimicking another primary tumor [109,110,111]. One of our cases was indeed misdiagnosed as an anal fistula carcinoma, probably due to the involvement of anal sphincter [6].
We feel that a point of strength of our literature review is the multidisciplinary detailed description of the state of the art about this infrequently analyzed topic through a systematic search in multiple databases according to the PRISMA guidelines, which include an evidence-based minimum set of items for reporting and are useful for the critical evaluation of the submitted manuscripts; indeed, systematic literature reviews and meta-analyses are increasingly relevant to keep clinicians up-to-date, also representing a starting point for developing clinical practice guidelines or further studies/trials [112,113,114,115,116,117,118,119,120,121,122,123].
The rarity of episiotomy-associated tumors has not allowed us to get significant results from statistical analysis, representing the main limit of drawing clear conclusions and clinical indications from our results. As just 13 cases were previously described (typically as case reports), the risk of malignant transformation for patients who underwent episiotomy seems low, but publication selection bias due to the choices of authors and policies of scientific journals may also have underestimated the incidence of this event.
The provided clinic-pathologic data were sometimes scant or questionable, representing another limit of our analysis. For example, the pT stage category was not provided in any case and the proper pTNM/AJCC stage was difficult to apply in most of the cases. In addition, some histotypes lack detailed immunohistochemical and molecular data, including a case with a maybe questionable histologic diagnosis [12]. Sometimes, it was also unclear if the tumor was centered on the vulva, vagina or perineum. For all these reasons, the statistical analysis was not applicable to evaluate our data with reliable significance.
Geographic variations in the frequency of performing episiotomy, as in the incidence of tumors and their risk factors, may represent another bias for our analysis and may affect the generalizability of the findings. Conditions other than episiotomy identified in our series may represent the real risk factors or co-factors for malignant transformation, as a synergistic effect cannot be excluded. However, they also may just represent incidental findings.
Future larger multicenter series with case centralization for histopathological review and/or analysis may be helpful to identify the real incidence of PriCs and to verify if this procedure increases the risk of cancer development [124,125,126].
Imaging (CT, PET and MRI) can exclude distant (0% in our series) or lymph node metastases (three cases, 23%) [6,8,18] and can define the potential tumor invasion of vagina (five cases, 39%) [6,8,11,13,14], anus (including sphincter) (four cases, 31%) [6,8,12,15] and/or other deep pelvic soft tissues (five cases, 39%) [7,8,13,15,18].
When achievable after complete staging, radical local surgical excision with lymph node status evaluation and eventual excision should be performed in order to avoid recurrence and progression; adjuvant and/or neoadjuvant treatment can be administered to improve the survival and disease-free recurrence rates, but no clear surgical or oncologic guidelines could be defined due to the few cases described. Globally, three (23%) cases recurred or progressed [13,14,18] and two of them (15%) died of disease [13,18]. One relapsing ACCBG-patient was surgically treated with hemivulvectomy + left LND (pN0) followed by RT achieving complete response and being free of disease 13 months after diagnosis [14]. Surgery was performed in all cases except for a CCC-patient who just underwent chemoradiation, achieving partial response and subsequently showing lung progression after one year and dying of disease [18]. The last recurring patient with EC died of disease after one year [13]. Globally, three cases were pN+ [6,8,18]; two cases treated with lymphadenectomy showed no evidence of disease after 15 months [6,8] while the remaining case was the non-surgically treated progressing and dying patient [18]. Adjuvant treatment (chemotherapy and/or RT) was administered to five (39%) cases [6,8,10,12,13], while neoadjuvant therapy was occasionally administered (four cases, 31%) [6,10,12,15].
5. Conclusions
Primary carcinomas arising from episiotomy were rarely reported in literature. Most of the cases were CCCs in post-/peri-menopausal patients that arose from endometriotic foci. Malignant transformation is a rare and not early event (mean 16 years after diagnosis of endometriosis). The diagnosis may be late when the disease is already in an advanced stage. At follow-up, a careful gynecological examination should be performed, and complete resection of long-standing endometriosis may be considered.
For tumors arising from episiotomy, complete imaging staging and exclusion of a vulvo-perineal metastasis from neoplasms arising from other primary sites are mandatory. Radical surgery with lymph node status evaluation and eventual excision should be performed when possible. Chemotherapy and/or radiotherapy can be considered in an adjuvant and/or neoadjuvant setting (or as only treatment in inoperable patients). However, the impact of surgery, radiotherapy and chemotherapy should be studied further in larger series with a multicenter and multidisciplinary study approach.
Author Contributions
Conceptualization, A.P., G.T., V.D.M. and V.D.M.-I.; methodology, A.P., F.T., A.B., E.Z., V.D.M.-I., B.M., A.M., G.S. and M.P.B.; software, A.P., F.T., I.B., M.Z. (Maurizio Zizzo), A.A., G.B., R.C., F.S. and N.I.K.; validation, A.P., L.A., G.T. and V.D.M.; formal analysis, A.P., M.Z. (Magda Zanelli), A.B., G.B., R.C., F.S., I.B., N.I.K., E.Z. and V.D.M.-I.; investigation, A.B., G.T., V.D.M. and L.A.; resources, M.Z. (Maurizio Zizzo) and M.Z. (Magda Zanelli); data curation, A.P., M.Z. (Maurizio Zizzo), F.S., V.D.M.-I. and V.D.M.; writing—original draft preparation, A.P., V.D.M., F.T. and V.D.M.-I.; writing—review and editing, A.P., F.T., G.T., A.B., M.Z. (Magda Zanelli), R.C., G.B., I.B., N.I.K., V.D.M.-I., L.A. and V.D.M.; visualization, G.S. and A.A.; supervision, L.A., A.A., R.C. and F.S.; project administration, B.M., A.B., E.Z. and M.P.B.; funding acquisition, A.P. and M.Z. (Magda Zanelli). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. The study was partially supported by the Italian Ministry of Health—Ricerca Corrente Annual Program 2025.
Acknowledgments
We are grateful to Francesca Sabrina Vinci, Giovanni Mattia, and Virginia Dolcini of the Grant Office and Research Administration (Azienda USL-IRCCS di Reggio Emilia) for their support. The present review was not registered and a protocol was not prepared.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Aragaw, F.M.; Belay, D.G.; Endalew, M.; Asratie, M.H.; Gashaw, M.; Tsega, N.T. Level of episiotomy practice and its disparity among primiparous and multiparous women in Ethiopia: A systematic review and meta-analysis. Front. Glob. Womens Health 2023, 4, 1153640. [Google Scholar] [CrossRef] [PubMed]
- Carroli, G.; Mignini, L. Episiotomy for vaginal birth. Cochrane Database Syst. Rev. 2009, 1, CD000081, Update in: Cochrane Database Syst. Rev. 2017, 2, CD000081. [Google Scholar] [CrossRef]
- Thacker, S.B.; Banta, H.D. Benefits and risks of episiotomy: An interpretative review of the English language literature, 1860–1980. Obstet Gynecol Surv. 1983, 38, 322–338. [Google Scholar] [CrossRef] [PubMed]
- Okeahialam, N.A.; Sultan, A.H.; Thakar, R. The prevention of perineal trauma during vaginal birth. Am. J. Obstet. Gynecol. 2024, 230, S991–S1004. [Google Scholar] [CrossRef] [PubMed]
- Shiono, P.; Klebanoff, M.; Carey, J.C. Midline episiotomies: More harm than good? Obstet. Gynecol. 1990, 75, 765–770. [Google Scholar] [PubMed]
- Kasahara, K.; Itatani, Y.; Kawada, K.; Takahashi, Y.; Yamamoto, T.; Hoshino, N.; Okada, T.; Oshima, N.; Hida, K.; Nishigori, T.; et al. Laparoscopic posterior pelvic exenteration for clear cell adenocarcinoma arising in an episiotomy scar. Asian J. Endosc. Surg. 2022, 15, 642–646. [Google Scholar] [CrossRef] [PubMed]
- Barrena-Medel, N.; Diaz, L.; Pabon, M. Episiotomy-site clear cell carcinoma. Am. J. Obstet. Gynecol. 2021, 224, 225–226. [Google Scholar] [CrossRef]
- Xu, S.; Wang, W.; Sun, L.P. Comparison of clear cell carcinoma and benign endometriosis in episiotomy scar—Two cases report and literature review. BMC Womens Health 2020, 20, 11. [Google Scholar] [CrossRef]
- Kojima, N.; Yoshida, H.; Uehara, T.; Ushigusa, T.; Asami, Y.; Shiraishi, K.; Kato, T. Primary Clear Cell Adenocarcinoma of the Vulva: A Case Study With Mutation Analysis and Literature Review. Int. J. Surg. Pathol. 2019, 27, 792–797. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Zheng, A.; Wang, H. Clear cell carcinoma arising in previous episiotomy scar: A case report and review of the literature. J. Ovarian Res. 2016, 9, 1. [Google Scholar] [CrossRef][Green Version]
- Kwon, Y.S.; Nam, J.H.; Choi, G. Clear cell adenocarcinoma arising in endometriosis of a previous episiotomy site. Obstet. Gynecol. 2008, 112 Pt 2, 475–477. [Google Scholar] [CrossRef] [PubMed]
- Chene, G.; Darcha, C.; Dechelotte, P.; Mage, G.; Canis, M. Malignant degeneration of perineal endometriosis in episiotomy scar, case report and review of the literature. Int. J. Gynecol. Cancer 2007, 17, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Nagy, P. Episiotomia hegében endometriosis talaján kialakult méhnyálkahártya carcinoma [Endometrial carcinoma arising from endometriosis in the episiotomy scar]. Orv. Hetil. 2003, 144, 373–374. [Google Scholar] [PubMed]
- Krasević, M.; Haller, H.; Iternicka, Z.; Valstelić, I.; Matejcić, N. Adenoid cystic carcinoma of Bartholin’s gland: A case report. Eur. J. Gynaecol. Oncol. 2001, 22, 213–214. [Google Scholar] [PubMed]
- Todd, R.W.; Kehoe, S.; Gearty, J. A case of clear cell carcinoma arising in extragonadal endometriosis. Int. J. Gynecol. Cancer 2000, 10, 170–172. [Google Scholar] [CrossRef]
- Olah, K.S.J.; Clarke, F.; Kingston, R.; Neilson, J.P. Vulval carcinoma in an episiotomy scar—A rare cause of superficial dyspareunia. J. Obstet. Gynaecol. 1995, 15, 208. [Google Scholar] [CrossRef]
- Van Dam, P.A.; Irvine, L.; Lowe, D.G.; Fisher, C.; Barton, D.P.; Shepherd, J.H. Carcinoma in episiotomy scars. Gynecol. Oncol. 1992, 44, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Hitti, I.F.; Glasberg, S.S.; Lubicz, S. Clear cell carcinoma arising in extraovarian endometriosis: Report of three cases and review of the literature. Gynecol. Oncol. 1990, 39, 314–320. [Google Scholar] [CrossRef]
- Ejegård, H.; Ryding, E.L.; Sjögren, B. Sexuality after delivery with episiotomy: A longterm follow-up. Gynecol. Obstet. Investig. 2008, 66, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, K.; Viswanathan, M.; Palmieri, R.; Gartlehner, G.; Thorp, J.; Lohr, K.N. Outcomes of routine episiotomy: A systematic review. JAMA 2005, 293, 2141–2148. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Qian, X.; Carroli, G.; Garner, P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst. Rev. 2017, 2, CD000081. [Google Scholar] [CrossRef] [PubMed]
- Palicelli, A.; Giaccherini, L.; Zanelli, M.; Bonasoni, M.P.; Gelli, M.C.; Bisagni, A.; Zanetti, E.; De Marco, L.; Torricelli, F.; Manzotti, G.; et al. How Can We Treat Vulvar Carcinoma in Pregnancy? A Systematic Review of the Literature. Cancers. 2021, 13, 836. [Google Scholar] [CrossRef]
- D’Agostino, C.; Surico, D.; Monga, G.; Palicelli, A. Pregnancy-related decidualization of subcutaneous endometriosis occurring in a post-caesarean section scar: Case study and review of the literature. Pathol. Res. Pract. 2019, 215, 828–831. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Wei, H.; Huang, J.; Shen, H.; Wang, X.; Hu, C. Clear Cell Adenocarcinoma Arising from Endometriosis in Abdominal Wall Cesarean Section Scar: A Case Report and Literature Review. Int. J. Womens Health 2023, 15, 25–32. [Google Scholar] [CrossRef]
- Scheyda-Yoo, K.; Hofer, U.; Várnai-Händel, A.; Maus, M.K.; Dumoulin, F.L. Massive Größenprogredienz und maligne Transformation einer muzinös-zystischen Neoplasie des Pankreas in der Schwangerschaft—Ein Fallbericht [Rapid growth and malignant transformation of a mucinous cystic neoplasm during pregnancy—A case report]. Z. Gastroenterol. 2024, 62, 1048–1052. [Google Scholar] [CrossRef]
- Gao, Y.; Han, N.; Jiang, Y.; Lu, Z. Transformation from acute promyelocytic leukemia in pregnancy to acute myeloid leukemia with MLL-AF9 fusion gene: A case report and literature review. Medicine 2023, 102, e36403. [Google Scholar] [CrossRef] [PubMed]
- Pomerantz, T.; Rubin, N.J.; Karnezis, A.N.; Zhao, X.; Brooks, R. Primary clear cell carcinoma of the vulva: A case report. Gynecol. Oncol. Rep. 2023, 50, 101283. [Google Scholar] [CrossRef]
- Carvalho, M.J.; Pais, A.S.; Rodrigues, Â.; Areia, A.L.; Figueiredo-Dias, M. Providing new insights into the endometriosis associated cancer arising in episiotomy scars. Ginekol. Pol. 2021, 92, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Liljestrand, J. Episiotomy for Vaginal Birth: RHL Commentary (2003) The WHO Reproductive Health Library; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Kozhimannil, K.B.; Karaca-Mandic, P.; Blauer-Peterson, C.J.; Shah, N.T.; Snowden, J.M. Uptake and Utilization of Practice Guidelines in Hospitals in the United States: The Case of Routine Episiotomy. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 41–48. [Google Scholar] [CrossRef]
- Gabbe, S.G.; Niebyl, J.R.; Simpson, J.L.; Landon, M.B.; Galan, H.L.; Jauniaux, E.R.M.; Driscoll, D.A. Obstetrics: Normal and Problem Pregnancies, 6th ed.; Elsevier: Philadelphia, PA, USA, 2012. [Google Scholar]
- Operative Vaginal Birth: ACOG Practice Bulletin, Number 219. Obstet. Gynecol. 2020, 135, e149–e159. [CrossRef] [PubMed]
- Izuka, E.; Dim, C.; Chigbu, C.; Obiora-Izuka, C. Prevalence and predictors of episiotomy among women at first birth in enugu, South-East Nigeria. Ann. Med. Health Sci. Res. 2014, 4, 928–932. [Google Scholar] [CrossRef] [PubMed]
- Graham, I.D.; Carroli, G.; Davies, C.; Medves, J.M. Episiotomy rates around the world: An update. Birth 2005, 32, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Li, K.P.; Ajebo, E.M.; Diamond, D.; Powell, M.; Belcher, M. Primary vulvar melanoma in an adolescent patient. Pediatr. Dermatol. 2023, 40, 749–750. [Google Scholar] [CrossRef] [PubMed]
- Dobrică, E.C.; Vâjâitu, C.; Condrat, C.E.; Crețoiu, D.; Popa, I.; Gaspar, B.S.; Suciu, N.; Crețoiu, S.M.; Varlas, V.N. Vulvar and Vaginal Melanomas-The Darker Shades of Gynecological Cancers. Biomedicines 2021, 9, 758. [Google Scholar] [CrossRef] [PubMed]
- Boufettal, H. Vulva choriocarcinoma. Pan Afr. Med. J. 2016, 24, 328. [Google Scholar] [CrossRef] [PubMed]
- Boufettal, H.; Samouh, N. Vulva choriocarcinoma. Pan Afr. Med. J. 2016, 25, 225. [Google Scholar] [CrossRef]
- Mitrovic, S.L.j.; Arsenijevic, P.S.; Kljakic, D.; Djuric, J.M.; Milosavljevic, M.Z.; Protrka, Z.M.; Vojinovic, R.H. Gestational choriocarcinoma of the cervix. Arch. Iran. Med. 2014, 17, 783–785. [Google Scholar]
- Mandato, V.D.; Torricelli, F.; Mastrofilippo, V.; Palicelli, A.; Costagliola, L.; Aguzzoli, L. Primary Ovarian Leiomyosarcoma Is a Very Rare Entity: A Narrative Review of the Literature. Cancers 2023, 15, 2953. [Google Scholar] [CrossRef]
- Ferron, G.; Bataillon, G.; Martinez, A.; Chibon, F.; Valentin, T. Gynecological sarcomas, surgical management: Primary, metastatic, and recurrent disease. Int. J. Gynecol. Cancer 2024, 34, 393–402. [Google Scholar] [CrossRef]
- Rekhi, B.; Bhatia, S.; Shetty, O.; Maheshwari, A. Poorly differentiated biphasic synovial sarcoma of the vulva, displaying SS18∷SSX1 fusion and weak to absent (mosaic) INI1/SMARCB1 immunostaining: A rare case with literature review. Indian. J. Pathol. Microbiol. 2024, 67, 396–400. [Google Scholar] [CrossRef]
- Sharma, A.E.; Wepy, C.B.; Chapel, D.B.; Maccio, L.; Irshaid, L.; Al-Ibraheemi, A.; Dickson, B.C.; Nucci, M.R.; Crum, C.P.; Fletcher, C.D.M.; et al. Ewing Sarcoma of the Female Genital Tract: Clinicopathologic Analysis of 21 Cases With an Emphasis on the Differential Diagnosis of Gynecologic Round Cell, Spindle, and Epithelioid Neoplasms. Am. J. Surg. Pathol. 2024. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Nongo, B.H.; Isah, D.A.; Ahmed, A.B.; Abdul, O.A. Vaginal Endometrial Stroma Sarcoma: A Case Report of A Rare Disease. J. West. Afr. Coll. Surg. 2024, 14, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Piura, B.; Rabinovich, A.; Shaco-Levy, R.; Sukenik, S. Vulvar invasive squamous cell carcinoma occurring in a young woman with systemic lupus erythematosus. Eur. J. Gynaecol. Oncol. 2005, 26, 103–105. [Google Scholar] [PubMed]
- Zhao, H.; Wu, L.; Yan, G.; Chen, Y.; Zhou, M.; Wu, Y.; Li, Y. Inflammation and tumor progression: Signaling pathways and targeted intervention. Signal Transduct. Target. Ther. 2021, 6, 263. [Google Scholar] [CrossRef] [PubMed]
- Snyder, R.R.; Hammond, T.L.; Hankins, G.D. Human papillomavirus associated with poor healing of episiotomy repairs. Obstet. Gynecol. 1990, 76, 664–667. [Google Scholar] [PubMed]
- Thompson, E.F.; Hoang, L.; Höhn, A.K.; Palicelli, A.; Talia, K.L.; Tchrakian, N.; Senz, J.; Rusike, R.; Jordan, S.; Jamieson, A.; et al. Molecular subclassification of vulvar squamous cell carcinoma: Reproducibility and prognostic significance of a novel surgical technique. Int. J. Gynecol. Cancer 2022, 32, 977–985. [Google Scholar] [CrossRef]
- Thiele, H.; Wesch, G.; Nüsser, C.J. Chirurgische Therapie entero-vaginaler Fisteln im Gefolge gynäkologischer Primäreingriffe [Surgical therapy of enterovaginal fistulae following gynecologic primary procedures (author’s transl)]. Langenbecks Arch. Chir. 1982, 357, 35–40. [Google Scholar] [CrossRef]
- Zizzo, M.; Tumiati, D.; Bassi, M.C.; Zanelli, M.; Sanguedolce, F.; Porpiglia, F.; Fiori, C.; Campobasso, D.; Castro Ruiz, C.; Bergamaschi, F.A.; et al. Management of colovesical fistula: A systematic review. Minerva Urol. Nephrol. 2022, 74, 400–408. [Google Scholar] [CrossRef]
- WHO Classification of Tumours Editorial Board. Female Genital Tumours: WHO Classification of Tumours, 5th ed.; IARC: Lyon, France, 2020; Volume 4.
- De Leo, A.; Santini, D.; Ceccarelli, C.; Santandrea, G.; Palicelli, A.; Acquaviva, G.; Chiarucci, F.; Rosini, F.; Ravegnini, G.; Pession, A.; et al. What Is New on Ovarian Carcinoma: Integrated Morphologic and Molecular Analysis Following the New 2020 World Health Organization Classification of Female Genital Tumors. Diagnostics 2021, 11, 697. [Google Scholar] [CrossRef] [PubMed]
- Santandrea, G.; Piana, S.; Valli, R.; Zanelli, M.; Gasparini, E.; De Leo, A.; Mandato, V.D.; Palicelli, A. Immunohistochemical Biomarkers as a Surrogate of Molecular Analysis in Ovarian Carcinomas: A Review of the Literature. Diagnostics 2021, 11, 199. [Google Scholar] [CrossRef] [PubMed]
- Tuninetti, V.; Pace, L.; Ghisoni, E.; Quarà, V.; Arezzo, F.; Palicelli, A.; Mandato, V.D.; Geuna, E.; Cormio, G.; Biglia, N.; et al. Retrospective Analysis of the Correlation of MSI-h/dMMR Status and Response to Therapy for Endometrial Cancer: RAME Study, a Multicenter Experience. Cancers 2023, 15, 3639. [Google Scholar] [CrossRef] [PubMed]
- Ardighieri, L.; Palicelli, A.; Ferrari, F.; Bugatti, M.; Drera, E.; Sartori, E.; Odicino, F. Endometrial Carcinomas with Intestinal-Type Metaplasia/Differentiation: Does Mismatch Repair System Defects Matter? Case Report and Systematic Review of the Literature. J. Clin. Med. 2020, 9, 2552. [Google Scholar] [CrossRef]
- Edmondson, R.J.; Crosbie, E.J.; Nickkho-Amiry, M.; Kaufmann, A.; Stelloo, E.; Nijman, H.W.; Leary, A.; Auguste, A.; Mileshkin, L.; Pollock, P.; et al. Markers of the p53 pathway further refine molecular profiling in high-risk endometrial cancer: A TransPORTEC initiative. Gynecol. Oncol. 2017, 146, 327–333. [Google Scholar] [CrossRef]
- Andres, M.P.; Arcoverde, F.V.L.; Souza, C.C.C.; Fernandes, L.F.C.; Abrão, M.S.; Kho, R.M. Extrapelvic endometriosis: A systematic review. J. Minim. Invasive Gynecol. 2020, 27, 373–389. [Google Scholar] [CrossRef] [PubMed]
- Nominato, N.S.; Prates, L.F.V.S.; Lauar, I.; Morais, J.; Maia, L.; Geber, S. Endometriose de cicatriz cirúrgica: Estudo retrospectivo de 72 casos. Rev. Bras. Ginecol. Obstet. 2007, 29, 423–427. [Google Scholar] [CrossRef]
- Nasu, K.; Okamoto, M.; Nishida, M.; Narahara, H. Endometriosis of the perineum. J. Obstet. Gynaecol. Res. 2013, 39, 1095–1097. [Google Scholar] [CrossRef]
- Su, H.; Chen, H.; Chen, C. Extra-pelvic endometriosis presenting as a vulvar mass in a teenage girl. Int. J. Gynecol. Obstet. 2004, 87, 252–253. [Google Scholar] [CrossRef] [PubMed]
- Borges, A.C.; Sousa, N.; Nogueira-Silva, C. Vulvar endometriosis: A rare primary location in adolescence. Arch. Gynecol. Obstet. 2024, 309, 1663–1664. [Google Scholar] [CrossRef]
- Dhillon-Smith, M.R.; Cutner, A.S.; Yap, M.; Creighton, S.M. The prevalence of endometriosis in adolescents with pelvic pain: A systematic review. J. Pediatr. Adolesc. Gynecol. 2020, 33, 623–630. [Google Scholar]
- Hagiwara, Y.; Hatori, M.; Moriya, T.; Terada, Y.; Yaegashi, N.; Ehara, S.; Kokubun, S. Inguinal endometriosis attaching to the round ligament. Australas. Radiol. 2007, 51, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Licheri, S.; Pisano, G.; Erdas, E.; Ledda, S.; Casu, B.; Cherchi, M.V.; Pomata, M.; Daniele, G.M. Endometriosis of the round ligament: Description of a clinical case and review of the literature. Hernia 2005, 9, 294–297. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, R.; Krishna, S.; Shenoy, R.; Thangavelu, S. Endometriosis of extra-pelvic round ligament, a diagnostic dilemma for physicians. BMJ Case Rep. 2013, 2013, bcr2013200465. [Google Scholar] [CrossRef] [PubMed]
- Abu Saadeh, F.; Wahab, N.A.; Gleeson, N. An unusual presentation of endometriosis. BMJ Case Rep. 2014, 2014, bcr2014204270. [Google Scholar] [CrossRef]
- Candiani, G.B.; Vercellini, P.; Fedele, L.; Vendola, N.; Carinelli, S.; Scaglione, V. Inguinal endometriosis: Pathogenetic and clinical implications. Obstet. Gynecol. 1991, 78, 191–194. [Google Scholar] [PubMed]
- Sarpietro, G.; Matarazzo, M.G.; Vecchio, G.M.; Palermo, G.; Cianci, A. Primary vulvar endometriosis in postmenopausal woman: A case report and review of the literature. Minerva Obstet. Gynecol. 2023, 75, 387–389. [Google Scholar] [CrossRef]
- Ferrandina, G.; Palluzzi, E.; Fanfani, F.; Gentileschi, S.; Valentini, A.L.; Mattoli, M.V.; Pennacchia, I.; Scambia, G.; Zannoni, G. Endometriosis-associated clear cell carcinoma arising in caesarean section scar: A case report and review of the literature. World J. Surg. Oncol. 2016, 14, 300. [Google Scholar] [CrossRef] [PubMed]
- Botezatu, R.; Turcu-Duminica, A.; Ciobanu, A.M.; Gica, N.; Peltecu, G.; Panaitescu, A.M. Episiotomy Scar Endometriosis. Case Presentation. Maedica 2021, 16, 713–716. [Google Scholar] [CrossRef] [PubMed]
- Saloum, N.M.; Qureshi, S.; Ibrahim, S.A.; Alrashid, A. A rare case report of endometriosis in an episiotomy scar without anal sphincter involvement. EC Gynaecol. 2018, 7, 466–470. [Google Scholar]
- Francica, G.; Giardiello, C.; Angelone, G.; Cristiano, S.; Finelli, R.; Tramontano, G. Abdominal wall endometriomas near cesarean delivery scars: Sonographic and color doppler findings in a series of 12 patients. J. Ultrasound Med. 2003, 22, 1041–1047. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.D.; Owen, E.; Berresford, A.; Sutton, C. Endometrial adenocarcinoma arising from endometriosis of the rectosigmoid colon. Gynecol. Oncol. 2002, 86, 220–222. [Google Scholar] [CrossRef] [PubMed]
- Kawate, S.; Takeyoshi, I.; Ikota, H.; Numaga, Y.; Sunose, Y.; Morishita, Y. Endometrioid adenocarcinoma arising from endometriosis of the mesenterium of the sigmoid colon. Jpn. J. Clin. Oncol. 2005, 35, 154–157. [Google Scholar] [CrossRef] [PubMed]
- Nomura, S.; Suganuma, T.; Suzuki, T.; Ito, T.; Kajiyama, H.; Okada, M.; Shibata, K.; Ino, K.; Kikkawa, F.; Mizutani, S. Endometrioid adenocarcinoma arising from endometriosis during 2 years of estrogen replacement therapy after total hysterectomy and bilateral salpingo-oophorectomy. Acta Obstet. Gynecol. Scand. 2006, 85, 1019–1021. [Google Scholar] [CrossRef] [PubMed]
- Al-Talib, A.; Gilbert, L.; Arseneau, J. Endometrioid adenocarcinoma 13 years after total abdominal hysterectomy and bilateral salpingo-oophorectomy. Saudi Med. J. 2008, 29, 1044–1047. [Google Scholar] [PubMed]
- Abu, M.A.; Sinha, P.; Totoe, L.; McCune, G. Endometrial cancer thirteen years after total abdominal hysterectomy and bilateral salpingo-oophorectomy and hormone replacement therapy: A case report. Eur. J. Gynaecol. Oncol. 1997, 18, 482–483. [Google Scholar]
- Debus, G.; Schuhmacher, I. Endometrial adenocarcinoma arising during estrogenic treatment 17 years after total abdominal hysterectomy and bilateral salpingo-oophorectomy: A case report. Acta Obstet. Gynecol. Scand. 2001, 80, 589–590. [Google Scholar] [PubMed]
- Euscher, E.D.; Marques-Piubelli, M.L.; Ramalingam, P.; Wistuba, I.; Lawson, B.C.; Frumovitz, M.; Malpica, A. Extrauterine Mesonephric-like Carcinoma: A Comprehensive Single Institution Study of 33 Cases. Am. J. Surg. Pathol. 2023, 47, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Poon, C.; Rome, R. Malignant extra-ovarian endometriosis: A case series of ten patients and review of the literature. Aust N Z J Obs. Gynaecol. 2020, 60, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Vilches Jimenez, J.C.; Villegas Muñoz, E.; González Poveda, I.; Santos Lorente, D.; Sanchez Pérez, B.; Jimenez Lopez, J.S. Diagnostic challenges: Low-grade adenosarcoma on deep endometriosis. BMC Womens Health 2019, 19, 124. [Google Scholar] [CrossRef]
- Shang, Y.; Wu, M.; He, R.; Ye, Y.; Sun, X. Administration of growth hormone improves endometrial function in women undergoing in vitro fertilization: A systematic review and meta-analysis. Hum. Reprod. Update 2022, 28, 838–857. [Google Scholar] [CrossRef] [PubMed]
- Nagase, S.; Saeki, H.; Ura, A.; Terao, Y.; Matsumoto, T.; Yao, T. Mixed Mesonephric-like Adenocarcinoma, Clear Cell Carcinoma, and Endometrioid Carcinoma Arising from an Endometriotic Cyst. Int. J. Surg. Pathol. 2024, 32, 1140–1148. [Google Scholar] [CrossRef]
- Alaert, J.; Lancelle, M.; Timmermans, M.; Tanos, P.; Nisolle, M.; Karampelas, S. Malignancy in Abdominal Wall Endometriosis: Is There a Way to Avoid It? A Systematic Review. J. Clin. Med. 2024, 13, 2282. [Google Scholar] [CrossRef]
- Sun, Y.; Liu, G. Endometriosis-associated Ovarian Clear Cell Carcinoma: A Special Entity? J. Cancer 2021, 12, 6773–6786. [Google Scholar] [CrossRef] [PubMed]
- Tanase, Y.; Yamada, Y.; Shigetomi, H.; Kajihara, H.; Oonogi, A.; Yoshizawa, Y.; Furukawa, N.; Haruta, S.; Yoshida, S.; Sado, T.; et al. Modulation of estrogenic action in clear cell carcinoma of the ovary (Review). Exp. Ther. Med. 2012, 3, 18–24. [Google Scholar] [CrossRef]
- Wiegand, K.C.; Shah, S.P.; Al-Agha, O.M.; Zhao, Y.; Tse, K.; Zeng, T.; Senz, J.; McConechy, M.K.; Anglesio, M.S.; Kalloger, S.E.; et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N. Engl. J. Med. 2010, 363, 1532–1543. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, F.; Akahira, J.; Miura, I.; Suzuki, T.; Ito, K.; Hayashi, S.; Sasano, H.; Yaegashi, N. Loss of estrogen receptor beta isoform expression and its correlation with aberrant DNA methylation of the 5′-untranslated region in human epithelial ovarian carcinoma. Cancer Sci. 2008, 99, 2365–2372. [Google Scholar] [CrossRef]
- Malutan, A.M.; Drugan, T.; Costin, N.; Ciortea, R.; Bucuri, C.; Rada, M.P.; Mihu, D. Pro-inflammatory cytokines for evaluation of inflammatory status in endometriosis. Cent. Eur. J. Immunol. 2015, 1, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Edwards, R.P.; Huang, X.; Vlad, A.M. Chronic inflammation in endometriosis and endometriosis-associated ovarian cancer: New roles for the “old” complement pathway. Oncoimmunology 2015, 4, e1002732. [Google Scholar] [CrossRef] [PubMed]
- Suryawanshi, S.; Huang, X.; Elishaev, E.; Budiu, R.A.; Zhang, L.; Kim, S.; Donnellan, N.; Mantia-Smaldone, G.; Ma, T.; Tseng, G.; et al. Complement Pathway Is Frequently Altered in Endometriosis and Endometriosis-Associated Ovarian Cancer. Clin. Cancer Res. 2014, 20, 6163–6174. [Google Scholar] [CrossRef] [PubMed]
- Scioscia, M.; Noventa, M.; Desgro, M.; Iaria, L.; Sacchi, D.; Virgilio, B.A. A rare case of primary vulvar endometriosis: Case report and review of the literature. J. Obstet. Gynaecol. 2022, 42, 354–356. [Google Scholar] [CrossRef] [PubMed]
- Mateoiu, C.; Palicelli, A.; Maloberti, T.; De Biase, D.; De Leo, A.; Lindh, M.; Bohlin, K.S.; Stolnicu, S. Primary vulvar adenocarcinoma of intestinal type: Report of two cases showing molecular similarity with colorectal adenocarcinoma. Pathol. Res. Pract. 2024, 255, 155181. [Google Scholar] [CrossRef]
- Chen, P.; Zhang, C.Y. Association Between Endometriosis and Prognosis of Ovarian Cancer: An Updated Meta-Analysis. Front. Oncol. 2022, 12, 732322. [Google Scholar] [CrossRef]
- Heron, D.E.; Axtel, A.; Gerszten, K.; Amortegui, A.; Kelley, J.; Comerci, J.; Edwards, R.P. Villoglandular adenocarcinoma of the cervix recurrent in an episiotomy scar: A case report in a 32-year-old female. Int. J. Gynecol. Cancer 2005, 15, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Goldman, N.A.; Goldberg, G.L. Late recurrence of squamous cell cervical cancer in an episiotomy site after vaginal delivery. Obstet. Gynecol. 2003, 101 Pt 2, 1127–1129. [Google Scholar] [CrossRef]
- Mandato, V.D.; Mastrofilippo, V.; Palicelli, A.; Silvotti, M.; Serra, S.; Giaccherini, L.; Aguzzoli, L. Solitary vulvar metastasis from early-stage endometrial cancer: Case report and literature review. Medicine 2021, 100, e25863. [Google Scholar] [CrossRef] [PubMed]
- Tang, T.Y.; Wang, T.Y. A vulvar mass as the first presentation in colorectal carcinoma: An unusual site of metastasis masquerading a primary Cancer. Taiwan. J. Obstet. Gynecol. 2018, 57, 157–160. [Google Scholar] [CrossRef]
- Aoun, F.; El Rassy, E.; Kourie, H.R.; Hawaux, E.; van Velthoven, R. Vulvar metastasis from bladder Cancer. Case Rep. Obstet. Gynecol. 2015, 2015, 324634. [Google Scholar] [CrossRef]
- Gandhi, A.K.; Roy, S.; Mridha, A.R.; Sharma, D.N. Vulvar metastasis from carcinoma breast unveiling distant metastasis: Exploring an unusual metastatic pattern. J. Egypt. Natl. Cancer Inst. 2015, 27, 243–246. [Google Scholar] [CrossRef]
- Kim, N.R.; Cho, H.Y.; Baek, J.H.; Jeong, J.; Ha, S.Y.; Seok, J.Y.; Park, S.W.; Sym, S.J.; Lee, K.C.; Chung, D.H. Rare Case of Anal Canal Signet Ring Cell Carcinoma Associated with Perianal and Vulvar Pagetoid Spread. J. Pathol. Transl. Med. 2016, 50, 231–237. [Google Scholar] [CrossRef][Green Version]
- Kajtezovic, S.; Walker, A.R.; Hjalmarsson, B.; Bell, S.G.; Everett, E.; Wong, C. Management of secondary Paget’s disease of the vulva associated with transitional cell carcinoma. J. Cancer Res. Clin. Oncol. 2022, 148, 1697–1702. [Google Scholar] [CrossRef]
- Olmes, G.L.; Breitbach, G.P.; Tepikin, A.; Nistor, A.; Solomayer, E.F.; Hamoud, B.H. A Metastasis of Ovarian Cancer in the Bartholin Gland: A Case Report with Systematic Literature Review. Reprod. Sci. 2024, 31, 550–554. [Google Scholar] [CrossRef] [PubMed]
- Heller, A.; Breitner, D.; Cracchiolo, B.; Heller, D.S. Metastatic Neoplasms to the Vulva-A Review. J. Low. Genit. Tract. Dis. 2022, 26, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, W.; Beasley, W.H. Carcinoma of stomach with a metastasis in the clitoris. J. Pak. Med. Assoc. 1979, 29, 62–63. [Google Scholar] [PubMed]
- Matak, M.; Lisica-Šikić, N.; Matak, L. Cutaneous vulvar metastasis in a patient with rectal adenocarcinoma. Int. J. Dermatol. 2022, 61, e168–e169. [Google Scholar] [CrossRef]
- Koufopoulos, N.; Pouliakis, A.; Boutas, I.; Samaras, M.G.; Kontogeorgi, A.; Dimas, D.; Sitara, K.; Zacharatou, A.; Zanelli, M.; Palicelli, A. Axillary Lymph Node Metastasis from Ovarian Carcinoma: A Systematic Review of the Literature. J. Pers. Med. 2023, 13, 1532. [Google Scholar] [CrossRef]
- Cabitza, E.; Pirola, M.; Baldessari, C.; Bernardelli, G.; Zunarelli, E.; Pipitone, S.; Vitale, M.G.; Nasso, C.; Molinaro, E.; Oltrecolli, M.; et al. Cerebellar metastasis of ovarian cancer: A case report. J. Med. Case Rep. 2023, 17, 553. [Google Scholar] [CrossRef] [PubMed]
- Minareci, Y.; Ak, N.; Tosun, O.A.; Sozen, H.; Saip, P.M.; Topuz, S.; Salihoglu, M.Y. Central nervous system metastasis in gynecologic cancers: Seeking the prognostic factors. J. Cancer Res. Ther. 2023, 19 (Suppl. S2), S523–S529. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Xiao, Y.; Wang, L.; Wang, Z.; Pan, J.; Bai, Z. Case report: A kidney metastasis from vulvar squamous cell carcinoma. Front. Oncol. 2024, 13, 1280531. [Google Scholar] [CrossRef]
- Linder, R.; Lauterbach, R.; Reiss, A. A Case of Recurrent Vulvar Carcinoma With Cardiac Metastasis: Case Report and Review of the Literature. Int. J. Gynecol. Pathol. 2020, 39, 400–403. [Google Scholar] [CrossRef]
- Young, C.; Horton, R. Putting clinical trials into context. Lancet 2005, 366, 107–108. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Turetta, C.; Mazzeo, R.; Capalbo, G.; Miano, S.; Fruscio, R.; Di Donato, V.; Falcone, F.; Mangili, G.; Pignata, S.; Palaia, I. Management of primary and recurrent Bartholin’s gland carcinoma: A systematic review on behalf of MITO Rare Cancer Group. Tumori. 2024, 110, 96–108. [Google Scholar] [CrossRef]
- Leis, M.; Singh, A.; Li, C.; Ahluwalia, R.; Fleming, P.; Lynde, C.W. Risk of Vulvar Squamous Cell Carcinoma in Lichen Sclerosus and Lichen Planus: A Systematic Review. J. Obstet. Gynaecol. Can. 2022, 44, 182–192. [Google Scholar] [CrossRef]
- Te Grootenhuis, N.C.; Pouwer, A.W.; de Bock, G.H.; Hollema, H.; Bulten, J.; van der Zee, A.G.J.; de Hullu, J.A.; Oonk, M.H.M. Prognostic factors for local recurrence of squamous cell carcinoma of the vulva: A systematic review. Gynecol. Oncol. 2018, 148, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Dogan, A.; Hilal, Z.; Krentel, H.; Cetin, C.; Hefler, L.A.; Grimm, C.; Tempfer, C.B. Paget’s Disease of the Vulva Treated with Imiquimod: Case Report and Systematic Review of the Literature. Gynecol. Obstet. Investig. 2017, 82, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Olivadese, R.; Ramponi, A.; Boldorini, R.; Dalla Dea, G.; Palicelli, A. Mitotically Active Cellular Fibroma of the Ovary Recurring After the Longest Interval of Time (16 yr): A Challenging Case With Systematic Literature Review. Int. J. Gynecol. Pathol. 2021, 40, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Edey, K.A.; Allan, E.; Murdoch, J.B.; Cooper, S.; Bryant, A. Interventions for the treatment of Paget’s disease of the vulva. Cochrane Database Syst. Rev. 2019, 6, CD009245. [Google Scholar] [CrossRef]
- Karseladze, A.I.; Asaturova, A.V.; Kiseleva, I.A.; Badlaeva, A.S.; Tregubova, A.V.; Zaretsky, A.R.; Uvarova, E.V.; Zanelli, M.; Palicelli, A. Androgen Insensitivity Syndrome with Bilateral Gonadal Sertoli Cell Lesions, Sertoli-Leydig Cell Tumor, and Paratesticular Leiomyoma: A Case Report and First Systematic Literature Review. J. Clin. Med. 2024, 13, 929. [Google Scholar] [CrossRef] [PubMed]
- Koufopoulos, N.I.; Pouliakis, A.; Samaras, M.G.; Kotanidis, C.; Boutas, I.; Kontogeorgi, A.; Dimas, D.; Sitara, K.; Zacharatou, A.; Ieronimaki, A.I.; et al. Malignant Brenner Tumor of the Ovary: A Systematic Review of the Literature. Cancers 2024, 16, 1106. [Google Scholar] [CrossRef]
- van Der Velden, J.; Ansink, A. Primary groin irradiation versus primary groin surgery for early vulvar Cancer. Cochrane Database Syst. Rev. 2000, 3, CD002224, Update in: Cochrane Database Syst. Rev. 2001, 4, CD002224. [Google Scholar] [CrossRef]
- Palicelli, A.; Ardighieri, L.; Broggi, G.; Caltabiano, R.; Melli, B.; Gelli, M.C.; Zanelli, M.; Bonasoni, M.P.; Asaturova, A.; Zizzo, M.; et al. Lipoleiomyomas of the Uterine Cervix: A New Series including the First Recurrent Case and the First Systematic Literature Review. J. Pers. Med. 2022, 12, 1852. [Google Scholar] [CrossRef] [PubMed]
- Mandato, V.D.; Palicelli, A.; Torricelli, F.; Mastrofilippo, V.; Leone, C.; Dicarlo, V.; Tafuni, A.; Santandrea, G.; Annunziata, G.; Generali, M.; et al. Should Endometrial Cancer Treatment Be Centralized? Biology 2022, 11, 768. [Google Scholar] [CrossRef] [PubMed]
- Narva, S.; Polo-Kantola, P.; Oksa, S.; Kallio, J.; Huvila, J.; Rissanen, T.; Hynninen, J.; Hietanen, S.; Joutsiniemi, T. Is it safe to operate selected low-risk endometrial cancer patients in secondary hospitals? Eur. J. Surg. Oncol. 2024, 50, 108317. [Google Scholar] [CrossRef] [PubMed]
- Leoni, J.; Rougemont, A.L.; Calinescu, A.M.; Ansari, M.; Compagnon, P.; Wilde, J.C.H.; Wildhaber, B.E. Effect of Centralization on Surgical Outcome of Children Operated for Liver Tumors in Switzerland: A Retrospective Comparative Study. Children 2022, 9, 217. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).