Acupuncture Improves Functional Limitations for Cancer Patients with Chronic Pain: A Secondary Analysis of PEACE Randomized Clinical Trial
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Intervention
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. Patient Information
3.2. Q-DASH
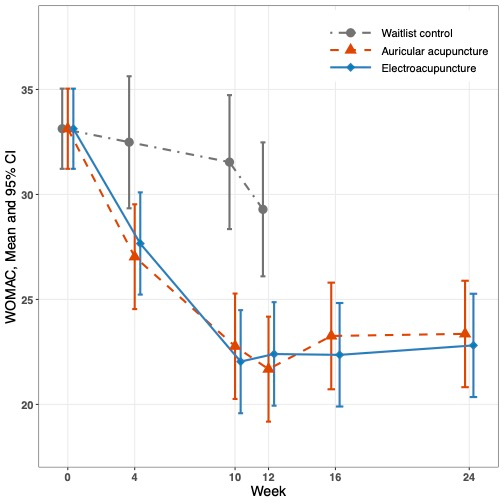
3.3. WOMAC
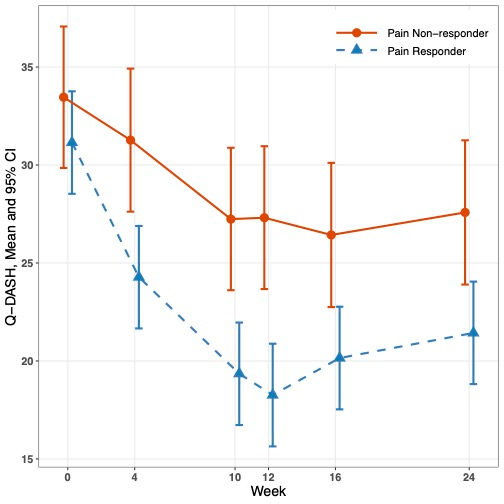
3.4. Pain Response and Extremity Function Improvement
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hjermstad, M.J.; Kaasa, S.; Caraceni, A.; Loge, J.H.; Pedersen, T.; Haugen, D.F.; Aass, N.; European Palliative Care Research Collaborative. Characteristics of breakthrough cancer pain and its influence on quality of life in an international cohort of patients with cancer. BMJ Support. Palliat. Care 2016, 6, 344–352. [Google Scholar] [CrossRef]
- Kang, J.H.; Koh, S.J.; Oh, S.Y.; Kim, R.B.; Shin, S.H.; Lee, Y.G.; Kim, B.S.; Ryoo, H.M.; Yoon, S.Y.; Jang, J.S.; et al. Interference with daily functioning by breakthrough pain in patients with cancer. Support. Care Cancer 2020, 28, 5177–5183. [Google Scholar] [CrossRef]
- Joshy, G.; Khalatbari-Soltani, S.; Soga, K.; Butow, P.; Laidsaar-Powell, R.; Koczwara, B.; Rankin, N.M.; Brown, S.; Weber, M.; Mazariego, C.; et al. Pain and its interference with daily living in relation to cancer: A comparative population-based study of 16,053 cancer survivors and 106,345 people without cancer. BMC Cancer 2023, 23, 774. [Google Scholar] [CrossRef]
- Isozaki, A.B.; Brant, J.M. The Impact of Pain on Mobility in Patients with Cancer. Semin. Oncol. Nurs. 2024, 40, 151672. [Google Scholar] [CrossRef]
- Tegegn, H.G.; Gebreyohannes, E.A. Cancer Pain Management and Pain Interference with Daily Functioning among Cancer Patients in Gondar University Hospital. Pain Res. Manag. 2017, 2017, 5698640. [Google Scholar] [CrossRef]
- Walsh, E.A.; Pedreira, P.B.; Moreno, P.I.; Popok, P.J.; Fox, R.S.; Yanez, B.; Antoni, M.H.; Penedo, F.J. Pain, cancer-related distress, and physical and functional well-being among men with advanced prostate cancer. Support. Care Cancer 2022, 31, 28. [Google Scholar] [CrossRef]
- Halabi, S.; Vogelzang, N.J.; Kornblith, A.B.; Ou, S.S.; Kantoff, P.W.; Dawson, N.A.; Small, E.J. Pain predicts overall survival in men with metastatic castration-refractory prostate cancer. J. Clin. Oncol. 2008, 26, 2544–2549. [Google Scholar] [CrossRef] [PubMed]
- Recchia, T.L.; Prim, A.C.; Luz, C.M. Upper Limb Functionality and Quality of Life in Women with Five-Year Survival after Breast Cancer Surgery. Rev. Bras. Ginecol. Obstet. 2017, 39, 115–122. [Google Scholar] [CrossRef]
- Roy, S.; Morgan, S.C.; Wallis, C.J.D.; Sun, Y.; Spratt, D.E.; Malone, J.; Grimes, S.; Mukherjee, D.; Kishan, A.U.; Saad, F.; et al. Association of dynamic change in patient—Reported pain with survival in metastatic castrate sensitive prostate cancer-exploratory analysis of LATITUDE study. Prostate Cancer Prostatic Dis. 2023, 26, 96–104. [Google Scholar] [CrossRef]
- Smyth, E.N.; Shen, W.; Bowman, L.; Peterson, P.; John, W.; Melemed, A.; Liepa, A.M. Patient-reported pain and other quality of life domains as prognostic factors for survival in a phase III clinical trial of patients with advanced breast cancer. Health Qual. Life Outcomes 2016, 14, 52. [Google Scholar] [CrossRef] [PubMed]
- Cheville, A.L.; Basford, J.R. Role of rehabilitation medicine and physical agents in the treatment of cancer-associated pain. J. Clin. Oncol. 2014, 32, 1691–1702. [Google Scholar] [CrossRef]
- Johnson, M.C.; McGregor, A.H.; A’Hern, R.; Leff, D.R.; Wells, M. ‘I presumed the pain would eventually get better by itself’; challenges with access to rehabilitation for upper limb dysfunction after breast cancer treatment—Descriptive and qualitative findings from a cross-sectional survey. Eur. J. Surg. Oncol. 2024, 50, 108591. [Google Scholar] [CrossRef]
- Bhavsar, N.A.; Doerfler, S.M.; Giczewska, A.; Alhanti, B.; Lutz, A.; Thigpen, C.A.; George, S.Z. Prevalence and predictors of no-shows to physical therapy for musculoskeletal conditions. PLoS ONE 2021, 16, e0251336. [Google Scholar] [CrossRef]
- Shahidi, B.; Padwal, J.; Lee, E.; Xu, R.; Northway, S.; Taitano, L.; Wu, T.; Raiszadeh, K. Factors impacting adherence to an exercise-based physical therapy program for individuals with low back pain. PLoS ONE 2022, 17, e0276326. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.J.; Ismaila, N.; Bao, T.; Barton, D.; Ben-Arye, E.; Garland, E.L.; Greenlee, H.; Leblanc, T.; Lee, R.T.; Lopez, A.M.; et al. Integrative Medicine for Pain Management in Oncology: Society for Integrative Oncology-ASCO Guideline. J. Clin. Oncol. 2022, 40, 3998–4024. [Google Scholar] [CrossRef]
- Chan, S.C.; Patrick Engkasan, J. Does acupuncture improve pain and function in people with hip osteoarthritis? A Cochrane Review summary with commentary. Int. J. Rheum. Dis. 2020, 23, 1741–1743. [Google Scholar] [CrossRef]
- Li, Y.X.; Yuan, S.E.; Jiang, J.Q.; Li, H.; Wang, Y.J. Systematic review and meta-analysis of effects of acupuncture on pain and function in non-specific low back pain. Acupunct. Med. 2020, 38, 235–243. [Google Scholar] [CrossRef]
- Voulgarakis, P.; Iakovidis, P.; Lytras, D.; Chatziprodromidou, I.P.; Kottaras, A.; Apostolou, T. Effects of Joint Mobilization Versus Acupuncture on Pain and Functional Ability in People with Chronic Neck Pain: A Randomized Controlled Trial of Comparative Effectiveness. J. Acupunct. Meridian Stud. 2021, 14, 231–237. [Google Scholar] [CrossRef]
- Shah, K.; Geller, D.A.; Tohme, S.; Antoni, M.; Kallem, C.J.; Vodovotz, Y.; Ramanathan, R.; Naveen, R.; Geroni, M.; Devine, L.; et al. Predictors and Consequences of Cancer and Non-Cancer-Related Pain in Those Diagnosed with Primary and Metastatic Cancers. Curr. Oncol. 2023, 30, 8826–8840. [Google Scholar] [CrossRef] [PubMed]
- Zhou, K.N.; Wang, Y.; Xie, Y.; Yang, S.H.; Liu, S.Y.; Fang, Y.H.; Zhang, Y. Symptom burden survey and symptom clusters in patients with cervical cancer: A cross-sectional survey. Support. Care Cancer 2023, 31, 338. [Google Scholar] [CrossRef]
- Mao, J.J.; Liou, K.T.; Baser, R.E.; Bao, T.; Panageas, K.S.; Romero, S.A.D.; Li, Q.S.; Gallagher, R.M.; Kantoff, P.W. Effectiveness of Electroacupuncture or Auricular Acupuncture vs Usual Care for Chronic Musculoskeletal Pain Among Cancer Survivors: The PEACE Randomized Clinical Trial. JAMA Oncol. 2021, 7, 720–727. [Google Scholar] [CrossRef]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Farrar, J.T.; Portenoy, R.K.; Berlin, J.A.; Kinman, J.L.; Strom, B.L. Defining the clinically important difference in pain outcome measures. Pain 2000, 88, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2025. [Google Scholar]
- Clement, N.D.; Bardgett, M.; Weir, D.; Holland, J.; Gerrand, C.; Deehan, D.J. What is the Minimum Clinically Important Difference for the WOMAC Index After TKA? Clin. Orthop. Relat. Res. 2018, 476, 2005–2014. [Google Scholar] [CrossRef]
- Galardini, L.; Coppari, A.; Pellicciari, L.; Ugolini, A.; Piscitelli, D.; La Porta, F.; Bravini, E.; Vercelli, S. Minimal Clinically Important Difference of the Disabilities of the Arm, Shoulder and Hand (DASH) and the Shortened Version of the DASH (QuickDASH) in People With Musculoskeletal Disorders: A Systematic Review and Meta-Analysis. Phys. Ther. 2024, 104, pzae033. [Google Scholar] [CrossRef] [PubMed]
- Giron, P.S.; Haddad, C.A.; Lopes de Almeida Rizzi, S.K.; Nazario, A.C.; Facina, G. Effectiveness of acupuncture in rehabilitation of physical and functional disorders of women undergoing breast cancer surgery. Support. Care Cancer 2016, 24, 2491–2496. [Google Scholar] [CrossRef]
- Pfister, D.G.; Cassileth, B.R.; Deng, G.E.; Yeung, K.S.; Lee, J.S.; Garrity, D.; Cronin, A.; Lee, N.; Kraus, D.; Shaha, A.R.; et al. Acupuncture for pain and dysfunction after neck dissection: Results of a randomized controlled trial. J. Clin. Oncol. 2010, 28, 2565–2570. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Lin, C.C.; Huang, T.W.; Kuan, Y.C.; Huang, Y.H.; Chen, H.C.; Kao, C.Y.; Su, C.M.; Tam, K.W. Effect of acupuncture on aromatase inhibitor-induced arthralgia in patients with breast cancer: A meta-analysis of randomized controlled trials. Breast 2017, 33, 132–138. [Google Scholar] [CrossRef]
- Zhi, W.I.; Ingram, E.; Li, S.Q.; Chen, P.; Piulson, L.; Bao, T. Acupuncture for Bortezomib-Induced Peripheral Neuropathy: Not Just for Pain. Integr. Cancer Ther. 2018, 17, 1079–1086. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wen, J.; Hong, J. The Effects of Auricular Therapy for Cancer Pain: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2020, 2020, 1618767. [Google Scholar] [CrossRef]
- Yeh, C.H.; Chien, L.C.; Lin, W.C.; Bovbjerg, D.H.; van Londen, G.J. Pilot Randomized Controlled Trial of Auricular Point Acupressure to Manage Symptom Clusters of Pain, Fatigue, and Disturbed Sleep in Breast Cancer Patients. Cancer Nurs. 2016, 39, 402–410. [Google Scholar] [CrossRef]
- Maltser, S.; Cristian, A.; Silver, J.K.; Morris, G.S.; Stout, N.L. A Focused Review of Safety Considerations in Cancer Rehabilitation. PM&R 2017, 9, S415–S428. [Google Scholar] [CrossRef] [PubMed]
- Stout, N.L.; Santa Mina, D.; Lyons, K.D.; Robb, K.; Silver, J.K. A systematic review of rehabilitation and exercise recommendations in oncology guidelines. CA Cancer J. Clin. 2021, 71, 149–175. [Google Scholar] [CrossRef]
- Mamipour, H.; Negahban, H.; Aval, S.B.; Zaferanieh, M.; Moradi, A.; Kachooei, A.R. Effectiveness of physiotherapy plus acupuncture compared with physiotherapy alone on pain, disability and grip strength in people with carpal tunnel syndrome: A randomized clinical trial. J. Bodyw. Mov. Ther. 2023, 35, 378–384. [Google Scholar] [CrossRef]
- Markenson, J.A. Mechanisms of chronic pain. Am. J. Med. 1996, 101, 6S–18S. [Google Scholar] [CrossRef]
- Courtney, C.A.; Fernandez-de-Las-Penas, C.; Bond, S. Mechanisms of chronic pain—Key considerations for appropriate physical therapy management. J. Man. Manip. Ther. 2017, 25, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Linton, S.J.; Shaw, W.S. Impact of psychological factors in the experience of pain. Phys. Ther. 2011, 91, 700–711. [Google Scholar] [CrossRef] [PubMed]
- Robinson, C.L.; Berger, A.; Sottosanti, E.; Li, M.; Kaneb, A.; Keefe, J.; Kim, E.; Kaye, A.D.; Viswanath, O.; Urits, I. Acupuncture as Part of Multimodal Analgesia for Chronic Pain. Orthop. Rev. 2022, 14, 38321. [Google Scholar] [CrossRef]
- Li, H.L.; Zhang, Y.; Zhou, J.W. Acupuncture for radicular pain: A review of analgesic mechanism. Front. Mol. Neurosci. 2024, 17, 1332876. [Google Scholar] [CrossRef] [PubMed]


| No. (%) | No. (%) | No. (%) | No. (%) | ||
|---|---|---|---|---|---|
| Characteristics/Group | Overall N = 360 | Electro-Acupuncture N = 145 | Auricular Acupuncture N = 143 | Waitlist Control N = 72 | |
| Age | Mean (SD), y | 62.1 (12.7) | 61.9 (13.2) | 62.6 (11.3) | 61.5 (14.4) |
| gender | |||||
| Male | 109 (30.3) | 43 (29.7) | 49 (34.3) | 17 (23.6) | |
| Female | 251 (69.7) | 102 (70/3) | 94 (65.7) | 55 (76.4) | |
| Race | |||||
| Non-white | 88 (24.4) | 42 (29.0) | 34 (23.8) | 12 (16.7) | |
| White | 272 (75.6) | 103 (71.0) | 109 (76.2) | 60 (83.3) | |
| Ethnicity | |||||
| Hispanic | 36 (10.1) | 19 (13.2) | 12 (8.5) | 5 (7.0) | |
| Not Hispanic | 321 (89.9) | 125 (86.8) | 130 (91.5) | 66 (93.0) | |
| Cancer type | |||||
| Breast | 165 (45.8) | 66 (45.5) | 67 (46.9) | 32 (44.4) | |
| Prostate | 41 (11.4) | 16 (11.0) | 18 (12.6) | 7 (9.7) | |
| Colorectal/GI | 15 (4.2) | 5 (3.4) | 4 (2.8) | 6 (8.3) | |
| Lymphoma | 51 (14.2) | 22 (15.2) | 19 (13.3) | 10 (13.9) | |
| Melanoma | 18 (5.0) | 5 (3.4) | 8 (5.6) | 5 (6.9) | |
| Lung | 12 (3.3) | 5 (3.4) | 7 (4.9) | 0 (0) | |
| Other | 58 (16.1) | 26 (17.9) | 20 (14.0) | 12 (16.7) | |
| Time since cancer diagnosis, mean (SD), y | 6.2 (6.7) | 6.1 (6.5) | 6.1 (6.8) | 6.5 (7.0) | |
| Pain duration, mean (SD), y | 5.3 (6.5) | 5.7 (6.7) | 4.8 (6.3) | 5.5 (6.4) | |
| Baseline measures | |||||
| Q-DASH, mean (SD) (0–100) | 33.2 (19.8) | 32.6 (19.9) | 33.4 (19.3) | 34.0 (20.9) | |
| WOMAC-function, mean (SD) (0–100) | 33.3 (20.3) | 33.8 (20.7) | 30.6 (19.4) | 37.7 (20.3) | |
| Mean (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Waitlist Control | Electro-Acupuncture | Auricular Acupuncture | Difference in Change from Baseline, Electro-Acupuncture to Auricular Acupuncture | |||
| Functional Performance | Baseline and Change from Baseline * | Baseline and Change from Baseline * | Difference from Waitlist Control in Change from Baseline | Baseline and Change from Baseline * | Difference from Waitlist Control in Change from Baseline | |
| Q-DASH | ||||||
| Baseline | 33.00 (31.08, 34.91) | 33.00 (31.08, 34.91) | NA | 33.00 (31.08, 34.91) | NA | NA |
| Week 4 | −1.21 (−3.83, 1.40) | −4.95 (−6.80, −3.10) | −3.74 (−6.90, −0.58) p = 0.02 | −6.02 (−7.95, −4.08) | −4.80 (−8.01, −1.60) p = 0.003 | 1.06 (−1.56, 3.68) p = 0.43 |
| Week 10 | 1.66 (−1.00, 4.32) | −9.42 (−11.29, −7.55) | −11.07 (−14.29, −7.86) p < 0.001 | −10.85 (−12.79, −8.92) | −12.51 (−15.76, −9.26) p < 0.001 | 1.43 (−1.21, 4.08) p = 0.29 |
| Week 12 | −2.65 (−5.31, 0.01) | −9.82 (−11.71, −7.94) | −7.18 (−10.39, −3.96) p < 0.001 | −12.29 (−14.22, −10.36) | −9.64 (−12.89, −6.40) p < 0.001 | 2.47 (−0.18, 5.11) p = 0.07 |
| Week 16 | NA | −9.45 (−11.34, −7.56) | NA | −10.04 (−12.01, −8.06) | NA | 0.59 (−2.09, 3.26) p = 0.67 |
| Week 24 | NA | −7.46 (−9.34, −5.57) | NA | −9.89 (−11.87, −7.92) | NA | 2.44 (−0.24, 5.12) p = 0.07 |
| WOMAC | ||||||
| Baseline | 33.13 (31.22, 35.04) | 33.13 (31.22, 35.04) | NA | 33.13(31.22,35.04) | NA | NA |
| Week 4 | −0.65 (−3.46, 2.16) | −5.47 (−7.45, −3.49) | −4.82 (−8.21, −1.44) p = 0.005 | −6.10 (−8.16, −4.04) | −5.45 (−8.88, −2.03) p=0.002 | 0.63 (−2.16, 3.42) p = 0.66 |
| Week 10 | −1.59 (−4.45, 1.27) | −11.10 (−13.11, −9.08) | −9.50 (−12.95, −6.06) p < 0.001 | −10.36 (−12.44, −8.29) | −8.77 (−12.25, −5.29) p < 0.001 | −0.73 (−3.56, 2.09) p = 0.61 |
| Week 12 | −3.84 (−6.70, −0.98) | −10.73 (−12.75, −8.71) | −6.89 (−10.33, −3.44) p < 0.001 | −11.45 (−13.52, −9.39) | −7.61 (−11.08, −4.14) p < 0.001 | 0.72 (−2.10, 3.55) p = 0.61 |
| Week 16 | NA | −10.77 (-12.79, −8.75) | NA | −9.87 (−11.99, −7.76) | NA | −0.90 (−3.76, 1.97) p = 0.54 |
| Week 24 | NA | −10.32 (−12.34, −8.31) | NA | −9.78 (−11.88, −7.76) | NA | −0.55 (−3.40, 2.30) p = 0.71 |
| Functional Performance | Mean (95% CI) | ||
|---|---|---|---|
| Pain Responder N = 173 | Pain Non-Responders N = 92 | Difference in Change from Baseline, Pain Responders to Non-Responders | |
| Baseline and Change from Baseline * | Baseline and Change from Baseline * | ||
| Q-DASH | |||
| Baseline | 31.16 (28.55, 33.77) | 33.40 (29.80, 37.00) | NA |
| Week 4 | −6.87 (−8.53, −5.21) | −2.18 (−4.53, 0.16) | −4.68 (−7.56, −1.81) p = 0.0014 |
| Week 10 | −11.80 (−13.46, −10.14) | −6.21 (−8.54, −3.88) | −5.59 (−8.44, −2.73) p = 0.0001 |
| Week 12 | −12.88 (−14.55, −11.22) | −6.14 (−8.49, −3.80) | −6.74 (−9.62, −3.86) p < 0.001 |
| Week 16 | −10.99 (−12.66, −9.33) | −7.03 (−9.42, −4.63) | −3.97 (-6.89, −1.05) p = 0.0077 |
| Week 24 | −9.71 (−11.38, −8.05) | −5.87 (−8.27, −3.47) | −3.84 (−7.76, −0.92) p = 0.01 |
| WOMAC | |||
| Baseline | 30.06 (27.46, 32.66) | 33.39 (29.81, 36.97) | NA |
| Week 4 | −5.94 (−7.74, −4.14) | −4.11 (−6.65, −1.57) | −1.83 (−4.94, 1.29) p = 0.25 |
| Week 10 | −11.70 (−13.51, −9.89) | −7.77 (−10.29, −5.25) | −3.93 (−7.03, −0.83) p = 0.013 |
| Week 12 | −12.50 (−14.31, −10.69) | −6.34 (−8.89, 3.79) | −6.16 (−9.29, −3.03) p = 0.0001 |
| Week 16 | −10.95 (−12.77, −9.13) | −8.20 (−10.80, −5.60) | −2.75 (−5.92, 0.43) p = 0.09 |
| Week 24 | −11.09 (−12.91, −9.28) | −6.75 (−9.35, −4.15) | −4.34 (−7.51, −1.17) p = 0.0073 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, L.; Ramalingam, M.B.; Baser, R.; Santos Teles, M.; Seluzicki, C.; Li, Q.S.; Mao, J.J. Acupuncture Improves Functional Limitations for Cancer Patients with Chronic Pain: A Secondary Analysis of PEACE Randomized Clinical Trial. Curr. Oncol. 2025, 32, 640. https://doi.org/10.3390/curroncol32110640
Sun L, Ramalingam MB, Baser R, Santos Teles M, Seluzicki C, Li QS, Mao JJ. Acupuncture Improves Functional Limitations for Cancer Patients with Chronic Pain: A Secondary Analysis of PEACE Randomized Clinical Trial. Current Oncology. 2025; 32(11):640. https://doi.org/10.3390/curroncol32110640
Chicago/Turabian StyleSun, Lingyun, Mothi Babu Ramalingam, Raymond Baser, Marco Santos Teles, Christina Seluzicki, Qing Susan Li, and Jun J. Mao. 2025. "Acupuncture Improves Functional Limitations for Cancer Patients with Chronic Pain: A Secondary Analysis of PEACE Randomized Clinical Trial" Current Oncology 32, no. 11: 640. https://doi.org/10.3390/curroncol32110640
APA StyleSun, L., Ramalingam, M. B., Baser, R., Santos Teles, M., Seluzicki, C., Li, Q. S., & Mao, J. J. (2025). Acupuncture Improves Functional Limitations for Cancer Patients with Chronic Pain: A Secondary Analysis of PEACE Randomized Clinical Trial. Current Oncology, 32(11), 640. https://doi.org/10.3390/curroncol32110640





