Potential Impact of Omega 6/3 Ratio and CD68+ Macrophage Infiltration on Survival in NSCLC Patients Undergoing Pulmonary Resection
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Exclusion Criteria
2.3. Preoperative Assessment
2.4. Blood Quantification Method for Ω6/Ω3 Ratio
2.5. Immunohistochemical Analysis
2.6. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Preoperative Nutritional and Inflammatory Study
3.3. Tumor Infiltration by Immune Cells
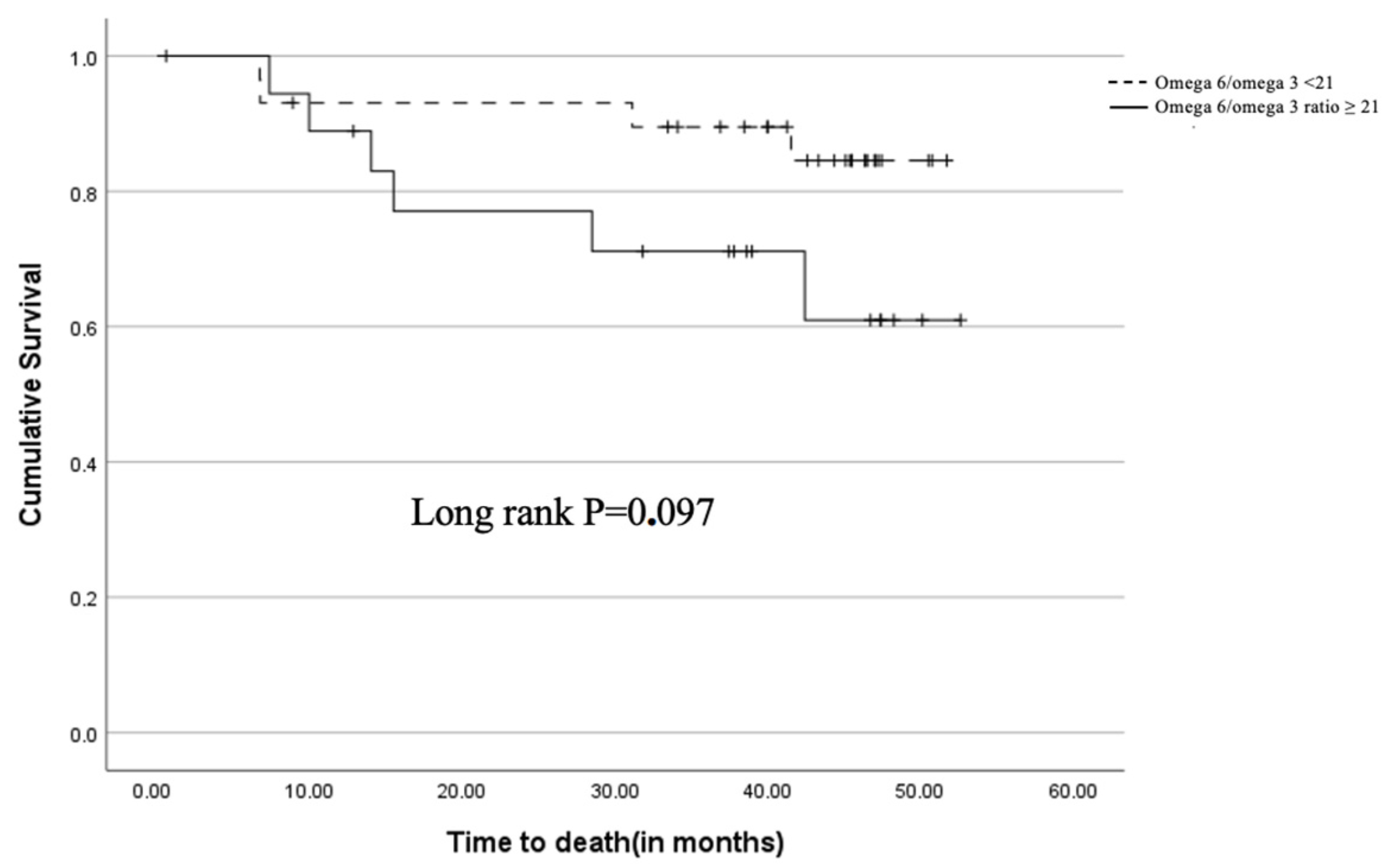
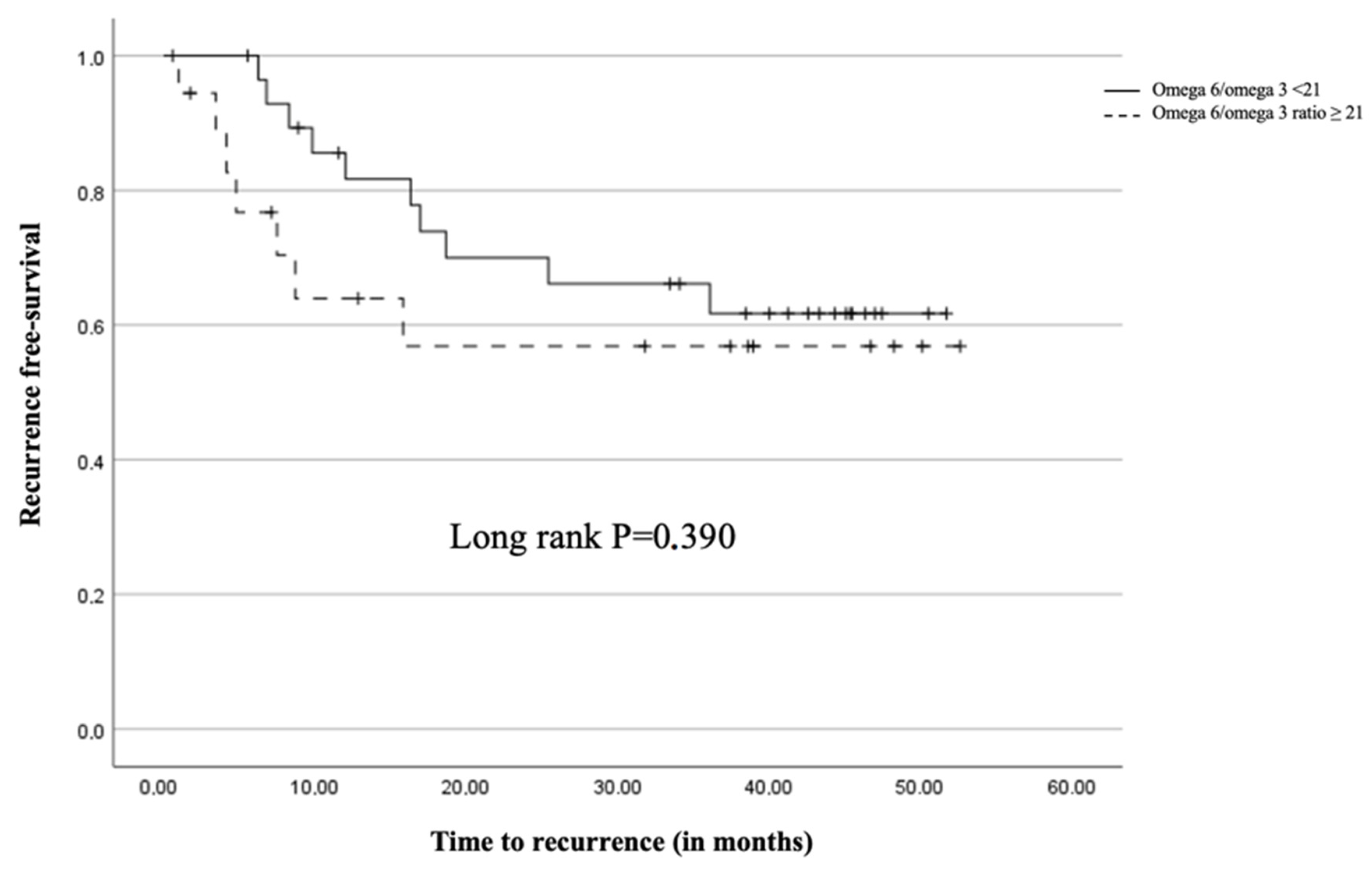
3.4. Survival Analysis
3.5. Recurrence and Mortality
3.6. Multivariate Analysis
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adams, S.J.; Stone, E.; Baldwin, D.R.; Vliegenthart, R.; Lee, P.; Finkelman, F.J. Lung cancer screening. Lancet 2023, 401, 390–408. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Steliarova-Foucher, E.; Lortet-Tieulent, J.; Rosso, S.; Coebergh, J.W.W.; Comber, H.; Forman, D.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. Eur. J. Cancer 2013, 49, 1374–1403. [Google Scholar] [CrossRef] [PubMed]
- Chirlaque, M.D.; Salmerón, D.; Galceran, J.; Ameijide, A.; Mateos, A.; Torrella, A.; Jiménez, R.; Larrañaga, N.; Marcos-Gragera, R.; REDECAN Working Group; et al. Cancer survival in adult patients in Spain. Results from nine population-based cancer registries. Clin. Transl. Oncol. 2017, 20, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, A.P. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed. Pharmacother. 2002, 56, 365–379. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C. Omega-3 polyunsaturated fatty acids and inflammatory processes: From molecules to man. Biochem. Soc. Trans. 2017, 45, 1105–1115. [Google Scholar] [CrossRef]
- Fridman, W.H.; Pagès, F.; Sautès-Fridman, C.; Galon, J. The immune contexture in human tumours: Impact on clinical outcome. Nat. Rev. Cancer 2012, 12, 298–306. [Google Scholar] [CrossRef]
- Chen, Y.; Li, F.; Hua, M.; Liang, M.; Song, C. Role of GM-CSF in lung balance and disease. Front. Immunol. 2023, 14, 1158859. [Google Scholar] [CrossRef]
- Mantovani, A.; Marchesi, F.; Malesci, A.; Laghi, L.; Allavena, P. Tumour-associated macrophages as treatment targets in oncology. Nat. Rev. Clin. Oncol. 2017, 14, 399–416. [Google Scholar] [CrossRef]
- Gajewski, T.F.; Schreiber, H.; Fu, Y.X. Innate and adaptive immune cells in the tumor microenvironment. Nat. Immunol. 2013, 14, 1014–1022. [Google Scholar] [CrossRef]
- Gordon, S.; Martinez, F.O. Alternative activation of macrophages: Mechanism and functions. Immunity 2010, 32, 593–604. [Google Scholar] [CrossRef]
- Vaughan, V.C.; Hassing, M.R.; Lewandowski, P.A. Marine polyunsaturated fatty acids and cancer therapy. Br. J. Cancer 2013, 108, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Shalapour, S.; Karin, M. Pas de deux: Control of anti-tumor immunity by cancer-associated inflammation. Immunity 2019, 51, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Janssen-Heijnen, M.L.G.; Coebergh, J.-W.W. The changing epidemiology of lung cancer in Europe. Lung Cancer 2003, 41, 245–258. [Google Scholar] [CrossRef]
- Déniz, C.; Raba-Parodi, C.; García, E.; Macía, I.; Rivas, F.; Ureña, A.; Muñoz, A.; Moreno, C.; Serratosa, I.; Masuet-Aumatell, C.; et al. Preoperative Omega-6/Omega-3 Fatty Acid Ratio predicts postoperative outcomes in patients with surgically resected Non-Small Cell Lung Cancer. Res. Sq. 2022, 29, 7086–7098. [Google Scholar] [CrossRef] [PubMed]
- Ramos, R.; Nadal, E.; Peiró, I.; Masuet-Aumatell, C.; Macia, I.; Rivas, F.; Rosado, G.; Rodriguez, P.; Ureña, A.; Padrones, S.; et al. Preoperative nutritional status assessment predicts postoperative outcomes in patients with surgically resected non-small cell lung cancer. Eur. J. Surg. Oncol. 2018, 44, 1419–1424. [Google Scholar] [CrossRef]
- Ramos, R.; Macía, I.; Navarro-Martin, A.; Déniz, C.; Rivas, F.; Ureña, A.; Masuet-Aumatell, C.; Moreno, C.; Nadal, E.; Escobar, I. Prognostic value of the preoperative lymphocyte-to-monocyte ratio for survival after lung cancer surgery. BMC Pulm. Med. 2021, 21, 75. [Google Scholar] [CrossRef]
- Hou, Z.; Zhao, L.; Zou, L.; Li, B. The prognostic value of tumour-infiltrating lymphocytes in non-small cell lung cancer patients who received neoadjuvant chemotherapy followed by surgery. Adv. Clin. Exp. Med. 2023, 32, 847–853. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Wan, B.; He, X.; Li, X. Identification of novel subtypes in lung adenocarcinoma: Evidence from gene set variation analysis in tumour and adjacent nontumor samples. Dis. Markers 2022, 2022, 2602812. [Google Scholar] [CrossRef]
- Vega, O.M.; Abkenari, S.; Tong, Z.; Tedman, A.; Huerta-Yepez, S. Omega-3 polyunsaturated fatty acids and lung cancer: Nutrition or pharmacology? Nutr. Cancer 2021, 73, 541–561. [Google Scholar] [CrossRef]
- Kaya, S.O.; Akcam, T.I.; Ceylan, K.C.; Samancılar, O.; Ozturk, O.; Usluer, O. Is preoperative protein-rich nutrition effective on postoperative outcome in non-small cell lung cancer surgery? A prospective randomized study. J. Cardiothorac. Surg. 2016, 11, 14. [Google Scholar] [CrossRef]
- Fabian, C.J.; Kimler, B.F.; Hursting, S.D. Omega-3 fatty acids for breast cancer prevention and survivorship. Breast Cancer Res. 2015, 17, 62. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, S.; Liu, F.; Yang, K. Role of CD68 in tumor immunity and prognosis prediction in pan-cancer. Sci. Rep. 2022, 12, 2275. [Google Scholar] [CrossRef] [PubMed]
| Variable | N (%) |
|---|---|
| Age | 63.9 (±10.3) * |
| Male sex | 39 (73.6%) |
| Active smoker | 15 (28.3%) |
| Diabetes | 16 (30.2%) |
| COPD | 38 (71.7%) |
| Ischemic Heart Disease | 6 (11.3%) |
| With previous pulmonary neoplasia | 1 (1.9%) |
| Without previous pulmonary neoplasia | 19 (35.8%) |
| Cerebral vascular accident (CVA) | 1 (1.9%) |
| Peripheral vasculopathy | 2 (3.8%) |
| Previous cardiac surgery | 1 (1.9%) |
| Nephropathy | 3 (5.7%) |
| Dyslipidemia | 20 (37.7%) |
| Hypertension | 27 (50.9%) |
| ASA | 3.95 (±0.99) |
| 1 | 6 (11.3%) |
| 2 | 35 (66%) |
| >3 | 12 (22.6%) |
| Maxime Expiratory Volume in the first second (FEV) | 100.44 (±94.95) * |
| Thoracoscore Index | |
| Histology | |
| Adenocarcinoma | 36 (67.9%) |
| Squamous cell carcinoma | 8 (15.1%) |
| Carcinoid Tumour | 2 (3.8%) |
| Large Cell | 4 (7.5%) |
| Metastasis CCR | 3 (5.7%) |
| Pathological staging | |
| Ia1 | 1 (1.9%) |
| Ia2 | 9 (17.3%) |
| Ia3 | 4 (7.7%) |
| Ib | 13 (25%) |
| IIa | 1 (1.9%) |
| IIb | 11 (21.2%) |
| IIIa | 6 (11.5%) |
| IIIb | 2 (3.8%) |
| Surgery | |
| Lobectomy | 46 (86.8%) |
| Wedge | 7 (13.2%) |
| Approach | |
| Thoracotomy | 27 (50.9%) |
| Thoracoscopy/VATS | 26 (49.1%) |
| Variable | Mean or Median (SD or IQR) |
|---|---|
| Height | 1.66 (±0.09) |
| weight | 75.61 (±14.22) |
| BCMI (Body Cell Mass Index) | 11 (±2.33) |
| BCM (Body Composition Monitor) (kg) | 30.29 (±8.01) |
| FFM (Fat Free Mass) (kg) | 54.6 (±9.92) |
| FM (Fat Mass) (kg) | 19.52 (±8.92) |
| Adherence to the Mediterranean diet Test | 40 (±58.82) |
| BMI (Body Mass Index) | 27.06 (±4.96) |
| IPN (Prognostic Nutritional Index) | 47.1 (±5.85) |
| Preoperative Plasmatic Test | |
| Albumin | 39.63 (±3.75) * |
| Prealbumin | 225.05 (±67.69) * |
| Cholesterol | 34.64 (117.91) |
| Vitamin D | 35.78 (±21.05) * |
| Fatty acids | |
| Ratio Omega 6/3 | 17.39 (±9.45) |
| EPA | 0.36 (±0.29) |
| DHA | 1.23 (±0.71) |
| Linolenic Acid | 0.41 (±0.27) |
| ARA | 6.33 (±1.90) |
| Linoleic Acid | 24.07 (±7.40) |
| Inflammatory Parameters | |
| Neutrophils | 4720.44 (±2398.10) |
| Lymphocytes | 1561.03 (±779.70) |
| Platelets | 205,177.94 (±79,743.10) |
| Monocytes | 525.59 (±206.60) |
| Ratio Neutrophils/Lymphocytes | 3.91 (±3.64) |
| Ratio Platelets/Lymphocytes | 152.32 (±70.36) |
| Ratio Lymphocytes/Monocytes | 3.3 (±1.64) |
| Transferrin | 41.66 (±58.30) |
| PCR | 9.04 (±16.22) |
| Fibrinogen | 4.05 (±51.63) * |
| SII (Systemic Inmune-inflamation Index) | 12,162.21 (±581,087.45) |
| Immunohistochemical analysis | |
| CD8 | 106.9 (±65.47) |
| CD68 | 115.19 (±62.9) |
| Hazard Ratio | 95.0% CI | Sig. | ||
|---|---|---|---|---|
| Upper | Lower | |||
| CD68 | 1.376 | 1.056 | 1.793 | 0.018 |
| Age | 0.173 | 0.042 | 0.716 | 0.016 |
| Male | 0.001 | 0.001 | 0.697 | 0.043 |
| Thoracoscore Index | 0.001 | 0.001 | 0.004 | 0.018 |
| Omega 6/Omega 3 ratio ≥ 21 | 0.001 | 0.001 | 0.018 | 0.02 |
| adenocarcinoma histology | 0.001 | 0.001 | 0.193 | 0.027 |
| pathological staging | 0.001 | 0.001 | 0.218 | 0.027 |
| Lpreoperative MST | 0.001 | 0.001 | 0.001 | 0.015 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Déniz, C.; Moreno, C.; Macía, I.; Rivas, F.; Ureña, A.; Muñoz, A.; Serratosa, I.; Aso, S.; García, M.; Masuet-Aumatell, C.; et al. Potential Impact of Omega 6/3 Ratio and CD68+ Macrophage Infiltration on Survival in NSCLC Patients Undergoing Pulmonary Resection. Curr. Oncol. 2024, 31, 5098-5106. https://doi.org/10.3390/curroncol31090377
Déniz C, Moreno C, Macía I, Rivas F, Ureña A, Muñoz A, Serratosa I, Aso S, García M, Masuet-Aumatell C, et al. Potential Impact of Omega 6/3 Ratio and CD68+ Macrophage Infiltration on Survival in NSCLC Patients Undergoing Pulmonary Resection. Current Oncology. 2024; 31(9):5098-5106. https://doi.org/10.3390/curroncol31090377
Chicago/Turabian StyleDéniz, Carlos, Camilo Moreno, Iván Macía, Francisco Rivas, Anna Ureña, Anna Muñoz, Ines Serratosa, Samantha Aso, Marta García, Cristina Masuet-Aumatell, and et al. 2024. "Potential Impact of Omega 6/3 Ratio and CD68+ Macrophage Infiltration on Survival in NSCLC Patients Undergoing Pulmonary Resection" Current Oncology 31, no. 9: 5098-5106. https://doi.org/10.3390/curroncol31090377
APA StyleDéniz, C., Moreno, C., Macía, I., Rivas, F., Ureña, A., Muñoz, A., Serratosa, I., Aso, S., García, M., Masuet-Aumatell, C., Escobar, I., & Ramos, R. (2024). Potential Impact of Omega 6/3 Ratio and CD68+ Macrophage Infiltration on Survival in NSCLC Patients Undergoing Pulmonary Resection. Current Oncology, 31(9), 5098-5106. https://doi.org/10.3390/curroncol31090377






