Testing Machine Learning Models to Predict Postoperative Ileus after Colorectal Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Acquisition and Variable Selection
2.3. Statistical Analysis
2.4. Model Training and Validation
Model Descriptions
- –
- –
- –
- –
- AdaBoost Classifier (Adaptive Boosting): This technique builds upon the core idea of boosting by strategically adjusting the weights assigned to training instances during each iteration. Instances that were previously misclassified by the model receive higher weights, forcing the subsequent learners to focus on these challenging cases [5,8,9,10].
- –
- –
2.5. Model Performance
3. Results
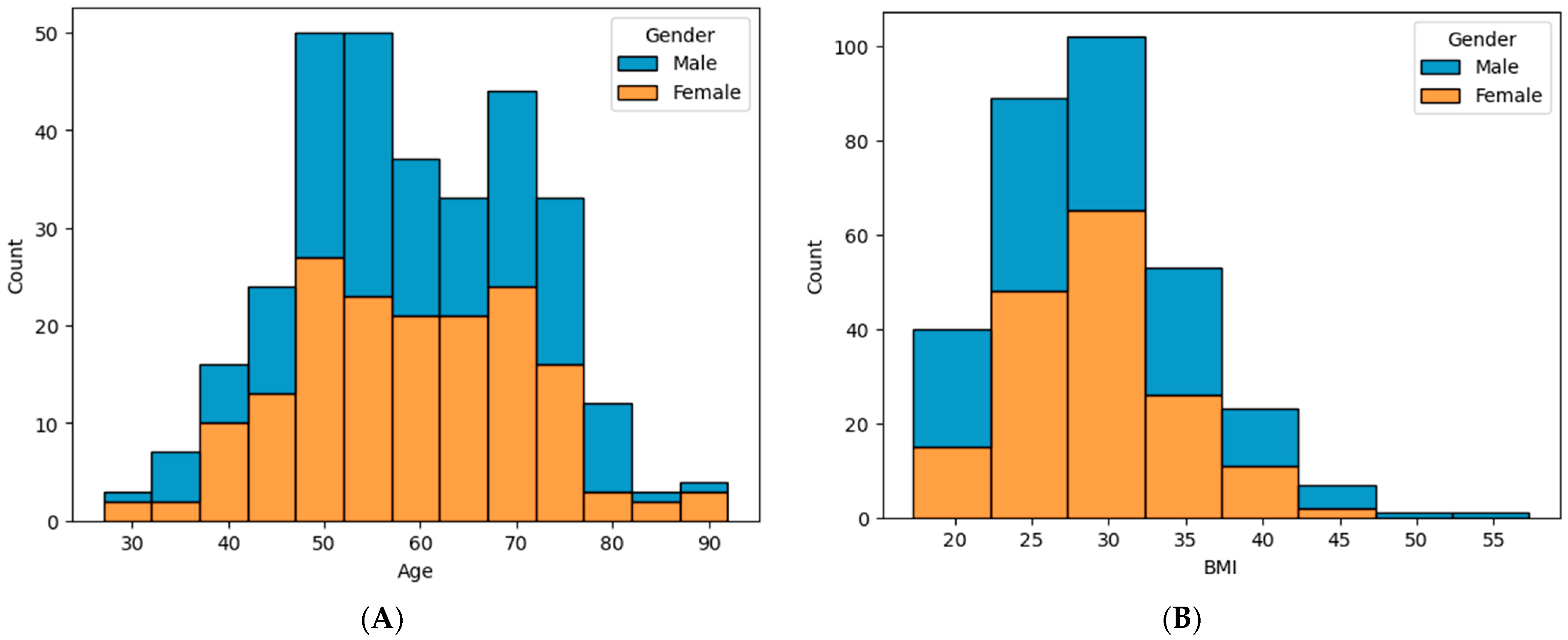
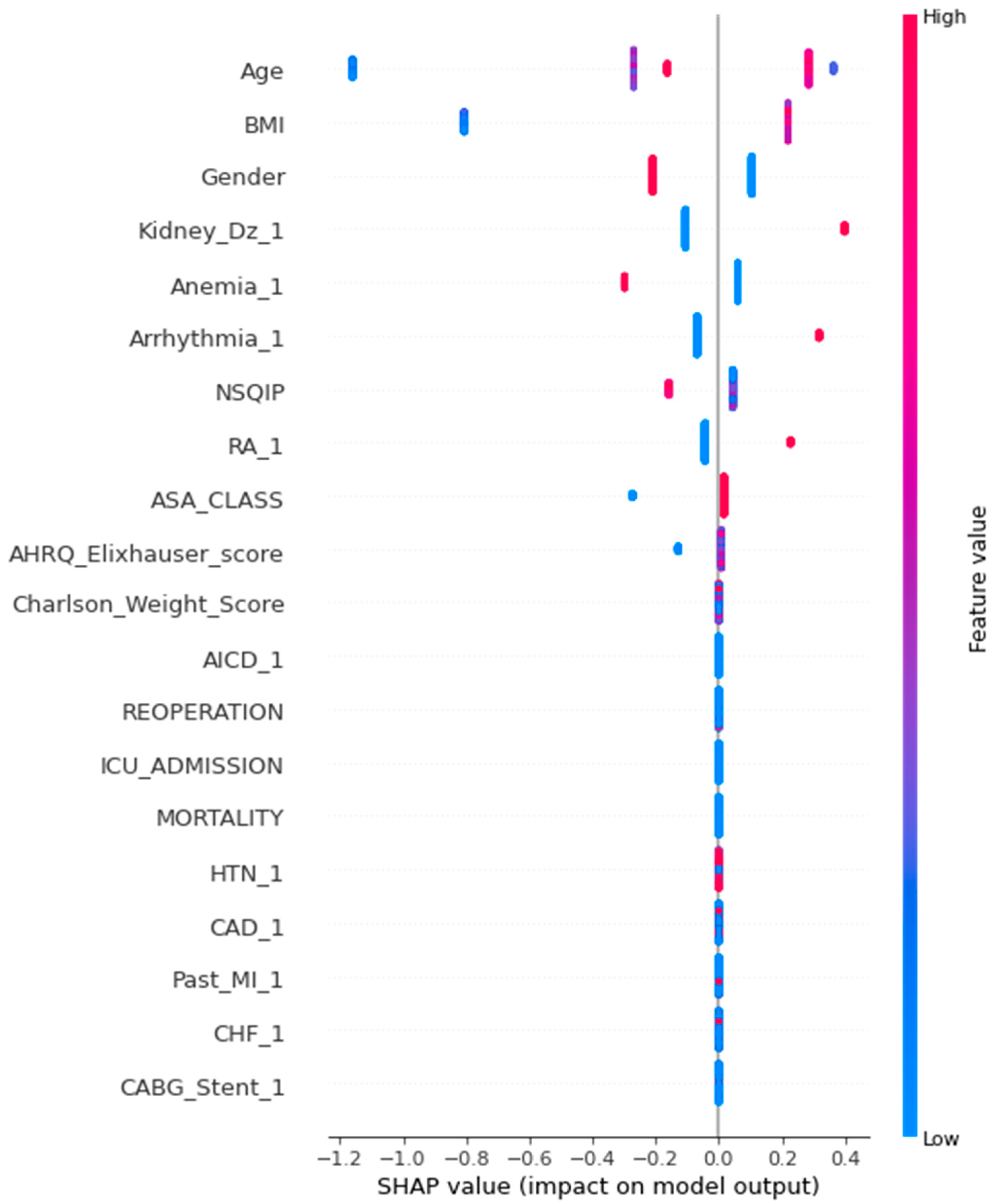
3.1. Baseline Characteristics
3.2. Comorbidities of Importance
3.3. ML Model Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Ada boosting classifier | adaptive boosting classifier |
| ASA physical status | American Society of Anesthesiologists Physical Status |
| AUC ROC curve | area under the curve receiver operating characteristic curve |
| BMI | body mass index |
| CCI | Charlson Comorbidity Index |
| CVA | cerebral vascular accident |
| ECI | Elixhauser Comorbidity Index |
| EHR | electronic health record |
| EDA | exploratory data analysis |
| XG boosting classifier | extreme gradient boosting classifier |
| IQR | inter-quantile range |
| kNN | k-nearest neighbors imputation |
| LOS | length of stay |
| ML | machine learning |
| NSQIP | National Surgical Quality Improvement Program index |
| POEM | perioperative evaluation and management |
| POI | postoperative ileus |
| PPV | positive predictive values |
| SMOTE | synthetic minority oversampling technique |
| UHC | University Health System Consortium |
References
- Merath, K.; Hyer, J.M.; Mehta, R.; Farooq, A.; Bagante, F.; Sahara, K.; Tsilimigras, D.I.; Beal, E.; Paredes, A.Z.; Wu, L.; et al. Use of Machine Learning for Prediction of Patient Risk of Postoperative Complications After Liver, Pancreatic, and Colorectal Surgery. J. Gastrointest. Surg. 2020, 24, 1843–1851. [Google Scholar] [CrossRef]
- Steinberg, S.M.; Popa, M.R.; Michalek, J.A.; Bethel, M.J.; Ellison, E.C. Comparison of Risk Adjustment Methodologies in Surgical Quality Improvement. Surgery 2008, 144, 662–669. [Google Scholar] [CrossRef]
- Bellman, R. Control Theory. Sci. Am. 1964, 211, 186–201. [Google Scholar] [CrossRef]
- Baloch, Z.Q.; Raza, S.A.; Pathak, R.; Marone, L.; Ali, A. Machine Learning Confirms Nonlinear Relationship between Severity of Peripheral Arterial Disease, Functional Limitation and Symptom Severity. Diagnostics 2020, 10, 515. [Google Scholar] [CrossRef]
- Lones, M.A. How to Avoid Machine Learning Pitfalls: A Guide for Academic Researchers. arXiv 2023, arXiv:2108.02497. [Google Scholar]
- Matsui, R.; Nagakari, K.; Igarashi, M.; Hatta, R.; Otsuka, T.; Nomoto, J.; Kohama, S.; Azuma, D.; Takehara, K.; Mizuno, T.; et al. Impact of Post-Operative Paralytic Ileus on Post-Operative Outcomes after Surgery for Colorectal Cancer: A Single-Institution, Retrospective Study. Surg. Today 2022, 52, 1731–1740. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). International Classification of Diseases, Tenth Revision (ICD-10). Available online: https://www.cdc.gov/nchs/icd/icd10.htm (accessed on 23 January 2024).
- Fouad, K.M.; Ismail, M.M.; Azar, A.T.; Arafa, M.M. Advanced methods for missing values imputation based on similarity learning. PeerJ Comput. Sci. 2021, 7, e619. [Google Scholar] [CrossRef]
- Choudhary, M.; Jain, S.; Arya, G. Classical Models Vs Deep Leaning: Time Series Analysis. In Advancements in Interdisciplinary Research; Springer: Berlin/Heidelberg, Germany, 2023; Volume 1738. [Google Scholar] [CrossRef]
- Walters, S.J.; Campbell, M.J. The use of bootstrap methods for analysing Health-Related Quality of Life outcomes (particularly the SF-36). Heal. Qual. Life Outcomes 2004, 2, 70. [Google Scholar] [CrossRef]
- Harre, F.E., Jr.; Lee, K.L.; Pollock, B.G. Regression models in clinical studies: Determining relationships between predictors and response. J. Natl. Cancer Inst. 1988, 80, 1198–1202. [Google Scholar] [CrossRef]
- Heagerty, P.J.; Zheng, Y. Survival model predictive accuracy and ROC curves. Biometrics 2005, 61, 92–105. [Google Scholar] [CrossRef]
- Corey, K.M.; Kashyap, S.; Lorenzi, E.; Lagoo-Deenadayalan, S.A.; Heller, K.; Whalen, K.; Balu, S.; Heflin, M.T.; McDonald, S.R.; Swaminathan, M.; et al. Development and validation of machine learning models to identify high-risk surgical patients using automatically curated electronic health record data (Pythia): A retrospective, single-site study. PLoS Med. 2018, 15, e1002701. [Google Scholar] [CrossRef]
- Lin, V.; Tsouchnika, A.; Allakhverdiiev, E.; Rosen, A.W.; Gögenur, M.; Clausen, J.S.R.; Bräuner, K.B.; Walbech, J.S.; Rijnbeek, P.; Drakos, I.; et al. Training prediction models for individual risk assessment of postoperative complications after surgery for colorectal cancer. Tech. Coloproctol. 2022, 26, 665–675. [Google Scholar] [CrossRef]
- Hosaka, H.; Takeuchi, M.; Imoto, T.; Yagishita, H.; Yu, A.; Maeda, Y.; Kobayashi, Y.; Kadota, Y.; Odaira, M.; Toriumi, F.; et al. Machine Learning-based Model for Predicting Postoperative Complications among Patients with Colonic Perforation: A Retrospective study. J. Anus Rectum Colon 2021, 5, 274–280. [Google Scholar] [CrossRef]
- Wells, C.I.; Milne, T.G.E.; Seo, S.H.B.; Chapman, S.J.; Vather, R.; Bissett, I.P.; O’Grady, G. Post-operative ileus: Definitions, mechanisms and controversies. ANZ J. Surg. 2021, 92, 62–68. [Google Scholar] [CrossRef]
- Millan, M.; Biondo, S.; Fraccalvieri, D.; Frago, R.; Golda, T.; Kreisler, E. Risk factors for prolonged postoperative ileus after colorectal cancer surgery. World J. Surg. 2011, 36, 179–185. [Google Scholar] [CrossRef]
- Kronberg, U.; Kiran, R.P.; Soliman, M.S.M.M.; Hammel, J.P.; Galway, U.; Coffey, J.C.; Fazio, V.W. A characterization of factors determining postoperative ileus after laparoscopic colectomy enables the generation of a novel predictive score. Ann. Surg. 2011, 253, 78–81. [Google Scholar] [CrossRef]
- Rybakov, E.G.; Shelygin, Y.A.; Khomyakov, E.A.; Zarodniuk, I.V. Risk factors for postoperative ileus after colorectal cancer surgery. Color. Dis. 2018, 20, 189–194. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows; Version 26.0; IBM Corp: Armonk, NY, USA, 2019. [Google Scholar]
- Haeuser, L.; Herzog, P.; Ayub, A.; Nguyen, D.-D.; Noldus, J.; Cone, E.B.; Mossanen, M.; Trinh, Q.-D. Comparison of Comorbidity Indices for Prediction of Morbidity and Mortality after Major Surgical Procedures. Am. J. Surg. 2021, 222, 998–1004. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Russell, M.M. The National Surgical Quality Improvement Program: Background and Methodology. Semin. Colon Rectal Surg. 2012, 23, 141–145. [Google Scholar] [CrossRef]
- Menendez, M.E.; Neuhaus, V.; van Dijk, N.C.; Ring, D. The Elixhauser comorbidity method outperforms the CCI in predicting inpatient death after orthopaedic surgery. Clin. Orthop. Relat. Res. 2014, 472, 2878–2886. [Google Scholar] [CrossRef]
- Elixhauser, A.; Steiner, C.; Harris, D.R.; Coffey, R.M. Comorbidity measures for use with administrative data. Med. Care 1998, 36, 8–27. [Google Scholar] [CrossRef]
- Moltó, A.; Dougados, M. Comorbidity indices. Clin. Exp. Rheumatol. 2014, 32 (Suppl. 85), 131–134. [Google Scholar]
- Ondeck, N.T.; Bovonratwet, P.; Ibe, I.K.; Bohl, D.D.; McLynn, R.P.; Cui, J.J.; Baumgaertner, M.R.; Grauer, J.N. Discriminative Ability for Adverse Outcomes After Surgical Management of Hip Fractures: A Comparison of the Charlson Comorbidity Index, Elixhauser Comorbidity Measure, and Modified Frailty Index. J. Orthop. Trauma 2018, 32, 231–237. [Google Scholar] [CrossRef]
- Mehta, H.B.; Dimou, F.; Adhikari, D.; Tamirisa, N.P.; Sieloff, E.B.; Williams, T.P.B.; Kuo, Y.-F.; Riall, T.S.M. Comparison of Comorbidity Scores in Predicting Surgical Outcomes. Med. Care 2016, 54, 180–187. [Google Scholar] [CrossRef]
- Wei, R.; Guan, X.; Liu, E.; Zhang, W.; Lv, J.; Huang, H.; Zhao, Z.; Chen, H.; Liu, Z.; Jiang, Z.; et al. Development of a machine learning algorithm to predict complications of total laparoscopic anterior resection and natural orifice specimen extraction surgery in rectal cancer. Eur. J. Surg. Oncol. EJSO 2023, 49, 1258–1268. [Google Scholar] [CrossRef]
- Weller, G.B.; Lovely, J.; Larson, D.W.; Earnshaw, B.A.; Huebner, M. Leveraging electronic health records for predictive modeling of post-surgical complications. Stat. Methods Med. Res. 2017, 27, 3271–3285. [Google Scholar] [CrossRef]
- Rencuzogullari, A.; Benlice, C.; Costedio, M.; Remzi, F.H.; Gorgun, E. Nomogram-Derived Prediction of Postoperative Ileus after Colectomy: An Assessment from Nationwide Procedure-Targeted Cohort. Am. Surg. 2017, 83, 564–572. [Google Scholar] [CrossRef]




| Data Science Stage | Sub-Stage | Description | Tools/Metrics |
|---|---|---|---|
| Data Acquisition | Source Import | Load data from CSV files, databases, etc. | File paths, data size |
| Cleaning and Preprocessing | Check for missing values, inconsistencies, duplicates. Format data types. | Imputation methods, error checking tools | |
| Exploratory Data Analysis (EDA) | Feature Distribution | Analyze data distribution for each feature using histograms, boxplots. | Visualizations, skewness measures |
| Feature Relationships | Identify relationships between features and target variable using scatter plots, correlation matrices. | Correlation coefficients, feature importance scores | |
| Outlier and Bias Detection | Check for outliers and potential biases using boxplots, statistical tests. | Outlier detection algorithms, bias analysis tools | |
| Imbalanced Data Handling | Class Imbalance Assessment | Calculate class imbalance ratio, visualize class distribution using pie charts. | Class imbalance ratio, visualization tools |
| Mitigation Strategy Decision | Choose appropriate strategy: SMOTE, undersampling, oversampling, none. | Imbalance severity, data type, problem type | |
| Data Oversampling (Optional) | SMOTE Application | Apply SMOTE or other oversampling techniques to increase minority class. | SMOTE algorithms, minority class size increase |
| Oversampling Control | Ensure oversampling does not introduce overfitting or class overlap. | Cross-validation, visualization | |
| Data Undersampling (Optional) | Undersampling Techniques | Apply undersampling techniques to reduce majority class. | Random undersampling, stratified undersampling |
| Undersampling Control | Ensure undersampling does not introduce bias or loss of information. | Class balance metrics, cross-validation | |
| Model Selection and Training | Feature Engineering (Optional) | Create new features based on existing ones (ratios, transformations). | Feature engineering algorithms, interpretability measures |
| Model Selection | Choose suitable ML algorithms based on data type, problem type, and interpretability needs. | Logistic Regression, Random Forest, Decision Trees, Gradient Boosting, Extreme Gradient Boosting | |
| Model Training and Regularization | Split data into training, validation, and test sets. Train models with cross-validation and regularization (L1, L2). | Train/validation/test ratios, regularization parameters | |
| Model Evaluation and Testing | Model Validation | Evaluate model performance on validation set using accuracy, precision, recall, F1-score, AUC-ROC (for imbalanced data). | Validation set metrics, model comparison tools |
| Best Model Selection | Compare performance across models and select the best one. | Validation metrics comparison, statistical tests | |
| Model Testing | Evaluate final model on unseen test set to assess real-world performance. | Test set metrics, model generalization analysis | |
| Error Analysis | Analyze model errors and identify potential limitations. | Error analysis tools, visualization | |
| Production | Interpretation and Deployment | Interpret model results and explain predictions. Deploy model and monitor performance. | Explainable AI tools, model monitoring systems |
| Variable of Importance | No Ileus (n = 296) | SD/Range | Ileus (n = 20) | SD/Range | Chi-Square | p-Value |
|---|---|---|---|---|---|---|
| Gender | 2.603 | 0.107 | ||||
| Male | 153 | 14 (70%) | ||||
| Female | 143 | 6 (30%) | ||||
| Age (mean/SD) | 58 | +/−12.33 | 62 | +/−10.05 | 0.055 | |
| BMI (median/range) | 21.8 | 17.31–56.10 | 30.5 | 20.94–41.53 | 0.00 | |
| NISQP (median/range) | 33.6 | 13.01–46.12 | 56.2 | 45.1–78.4 | 0.00 | |
| Length of Stay (Days) (median/range) | 3.74 | 1–20 | 11.64 | 6–25 | 0.00 | |
| Cost of Care (Ratio) | 1.0 | +/−0.36 | 1.77 | +/−0.34 | ||
| Co-Morbidity | ||||||
| Kidney Disease | 50 | 5 (25%) | 0.629 | 0.428 | ||
| Anemia | 77 | 5 (25%) | 0.033 | 0.855 | ||
| Arrhythmia | 41 | 4 (20%) | 0.458 | 0.498 | ||
| Rheumatoid Arthritis | 32 | 4 (20%) | 1.613 | 0.204 | ||
| Surgical Approach | ||||||
| Coloanal Anastomosis | 9 | 4 (20%) | 0.703 | 0.402 | ||
| Extended Right Hemicolectomy | 14 | 2 (10%) | 0.259 | 0.611 | ||
| Left Hemicolectomy | 21 | 1 (5%) | 0.091 | 0.763 | ||
| Low Anterior Resection | 161 | 3 (15%) | 0.085 | 0.771 | ||
| Right Hemicolectomy | 64 | 3 (15%) | 0.091 | 0.763 | ||
| Sigmoid Colectomy | 13 | 1 (5%) | 0.154 | 0.695 | ||
| Subtotal Colectomy (Ileosigmoid) | 1 | 0 | 0.000 | 0.996 | ||
| Total Colectomy, Ileorectal | 1 | 1 (5%) | 1.047 | 0.306 | ||
| Transverse Colectomy | 1 | 0 | 0.000 | 0.996 | ||
| Ultra Low Anterior Resection | 11 | 1 (5%) | 0.167 | 0.683 | ||
| Surgery Type | 3.848 | 0.050 | ||||
| Minimally Invasive Surgery (MIS) | 248 (95%) | 13 (5%) | ||||
| Open Approach | 48 (87.3%) | 7 (12.7%) |
| Co-Morbidity | Sample Size | Frequency | % of Sample |
|---|---|---|---|
| HTN | 316 | 178 | 56.3% |
| CAD | 316 | 62 | 19.6% |
| Past MI | 316 | 17 | 5.4% |
| CHF | 316 | 25 | 7.9% |
| CABG Stent | 316 | 20 | 6.3% |
| Arrhythmia | 316 | 41 | 13.0% |
| AICD | 316 | 1 | 0.3% |
| Pacemaker | 316 | 51 | 16.1% |
| Valvular | 316 | 18 | 5.7% |
| PVD | 316 | 7 | 2.2% |
| Anemia | 316 | 77 | 24.4% |
| Diabetes | 316 | 63 | 19.9% |
| Hypothyroidism | 316 | 56 | 17.7% |
| Electrolyte Disturbance | 316 | 308 | 97.5% |
| Asthma | 316 | 60 | 19.0% |
| COPD | 316 | 30 | 9.5% |
| OSA | 316 | 48 | 15.2% |
| CVA | 316 | 65 | 20.6% |
| TIA | 316 | 6 | 1.9% |
| Seizures | 316 | 7 | 2.2% |
| Neuromuscular Disease | 316 | 0 | 0.0% |
| Hepatitis | 316 | 26 | 8.2% |
| Cirrhosis | 316 | 13 | 4.1% |
| AIDS_HIV | 316 | 3 | 0.9% |
| Dyslipidemia | 316 | 118 | 37.3% |
| Kidney Disease | 316 | 50 | 15.8% |
| RA | 316 | 32 | 10.1% |
| Depression | 316 | 39 | 12.3% |
| Dementia | 316 | 39 | 12.3% |
| AdaBoost Tuned with Grid Search | AdaBoost Tuned with Random Search | XGboost Tuned with Grid Search | XGboost Tuned with Random Search | |
|---|---|---|---|---|
| Accuracy | 0.942 | 0.942 | 0.852 | 0.852 |
| Recall | 0.083 | 0.083 | 0.833 | 0.833 |
| Precision | 1.000 | 1.000 | 0.278 | 0.278 |
| F1 | 0.154 | 0.154 | 0.417 | 0.417 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brydges, G.; Chang, G.J.; Gan, T.J.; Konishi, T.; Gottumukkala, V.; Uppal, A. Testing Machine Learning Models to Predict Postoperative Ileus after Colorectal Surgery. Curr. Oncol. 2024, 31, 3563-3578. https://doi.org/10.3390/curroncol31060262
Brydges G, Chang GJ, Gan TJ, Konishi T, Gottumukkala V, Uppal A. Testing Machine Learning Models to Predict Postoperative Ileus after Colorectal Surgery. Current Oncology. 2024; 31(6):3563-3578. https://doi.org/10.3390/curroncol31060262
Chicago/Turabian StyleBrydges, Garry, George J. Chang, Tong J. Gan, Tsuyoshi Konishi, Vijaya Gottumukkala, and Abhineet Uppal. 2024. "Testing Machine Learning Models to Predict Postoperative Ileus after Colorectal Surgery" Current Oncology 31, no. 6: 3563-3578. https://doi.org/10.3390/curroncol31060262
APA StyleBrydges, G., Chang, G. J., Gan, T. J., Konishi, T., Gottumukkala, V., & Uppal, A. (2024). Testing Machine Learning Models to Predict Postoperative Ileus after Colorectal Surgery. Current Oncology, 31(6), 3563-3578. https://doi.org/10.3390/curroncol31060262






