Understanding Elderly Chinese Cancer Patients in a Multicultural Clinical Setting: Embracing Mortality and Addressing Misperceptions of Vulnerability
Abstract
1. Introduction
2. Materials and Methods
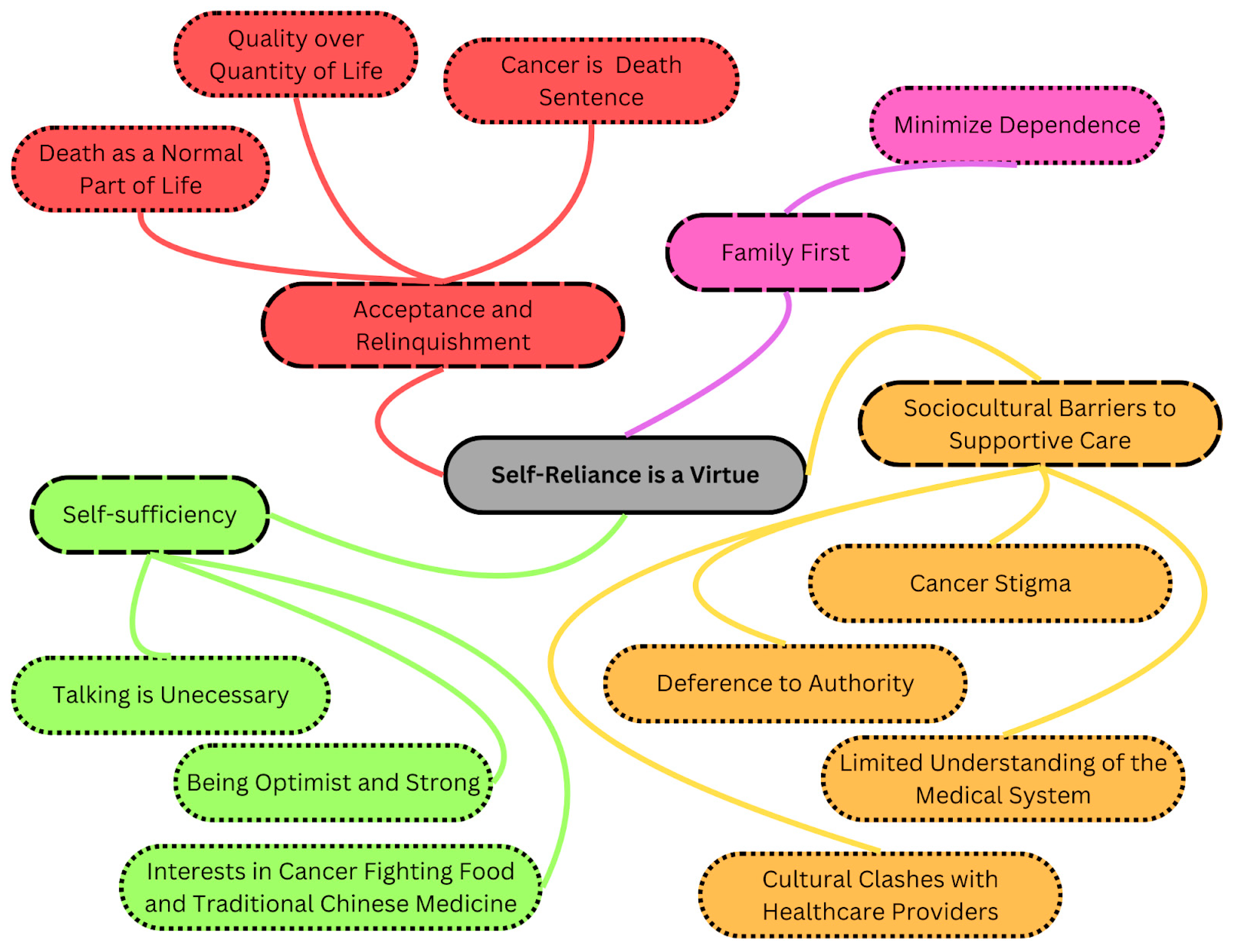
3. Results
3.1. Acceptance and Relinquishment
3.1.1. Cancer Is a Death Sentence
“My disease is fatal. Even though everyone puts so much effort to help me with my treatments, including the government, hospital, doctors and you (EK) as well, but my disease is still fatal nevertheless… But I’m afraid that this disease cannot be cured, I could leave this world any time… I’m going to die no matter what. The treatment extends my life for a couple months. But I’m not sure if it is worth going through these painful experiences (treatments) just to extend my life for a couple extra months”—022F.
3.1.2. Death as a Normal Part of Life
“If I were to be sick, I’ll let it be. If I were to die, so be it. No big deal… What can you do? Some things cannot be changed even if you want to. So you can only do it this way… It was useless saying anything… In this world, living and dying is a normal course of life… There is nothing to be optimistic or pessimistic about.”—016M.
“My feeling towards cancer was not so big of a reaction. I am already quite old now right? So it’s normal to be sick. The kids are all grown up, all of them are working now. There is no financial problem. And I have lived a hard life for decades, and I have paid off my debts.”—014M.
3.1.3. Quality over Quantity of Life
“My wife was allergic to chemotherapy, so she had to do this special chemotherapy instead, then she stopped eating entirely because she had lost her appetite… If treatment compromises my quality of life I’d rather give up treatment than live longer. I’d rather be walking than crawling (wasting away) … Alcohol harms the liver right? That means if I want to die earlier, I only need to drink more?”
“Yes I’m going to stop the treatment because I’m going to die no matter what. The radiotherapy extends my life for a couple months, but I don’t think it is worth to go through these painful experiences.”—019M.
“If I were to have cancer recurrence right now or anything alike, I would refuse treatment. The treatment would cause my quality of life to decrease significantly. There is no point living like that… I’d then choose to live in (palliative care) and pay a funeral home some money to bury myself somewhere.”—007M.
3.2. Family First
“My biggest worry is my family worrying about me… I think it would help my family if I face it (my illness) optimistically… Of course family is the most important. Their caring helped the most. In fact many things in my daily life depend on my family.”—002F.
Minimize Dependence
“After all, there is mental stress and burden in my life. Two of my grandchildren, one from my son, another from my daughter, are autistic… So we would think of ways to lessen their (son and daughter) burdens. I could take care of myself just fine, so I could help them out a bit.”—011M.
“Normally I don’t want to distract my son-in-law from work. It is because he is working as an engineer who has lots of responsibilities. Our 8-people family relies on him as he is the only person who works. Due to my illness, I can’t even do housework. We have four elderlies and two young children and him (patient’s son-in-law) at home… I am trying my best to not get him involved. I don’t want him to be involved with someone who is dying. If he lost his job, what should the family do? … My daughter told me that she wanted to stop going to school and stay with me during the treatment. But I cannot ruin her future because of a dying person like me.”—012F.
3.3. Self-Sufficiency
3.3.1. Talking Is Unnecessary
“I don’t think that I need to discuss it with others. There is no use talking about it. At the most it is a release; but after all they are just words.”—008M.
“I did not use it (the medical/ hospital support) because I did not think I needed it and I am not depressed… I am not greedy, not stressed, not worried. If I am worried then I will be checking here and there for information, how to prevent (prolong his life) … Not really interested (in the supportive care).”—005M.
“Right now I have no need for such things (supportive care/community services) … It is very inconvenient for elderly to travel around if they can’t drive anymore … I don’t need others to help me, I am not used to that.”—003M.
3.3.2. Being Optimistic and Strong
“I was upset but I tried to have a positive attitude. This is a stage in life and if I can overcome it then I will overcome it. But I need to maintain a quality of life.”—019M.
“People told me to be more optimistic and I thought ‘oh yeah that’s right’. Since it’s the reality and being depressed will still lead to the same outcome so why not be more optimistic.”—015M.
“I did not see a social worker, no time for these services because I need to make money to support my grandkids … I think I will be able to self-manage my mood. I listen to music and exercise a lot. I forced myself to be positive but sometimes I find it very difficult.”—011M.
3.3.3. Interests in Cancer-Fighting Food and Traditional Chinese Medicine
“Traditional Chinese medicine is simple, easy to do with no side effects. I have tried the ‘sunbathe’ before recommended by a Chinese doctor. It was quite effective.”—018F.
“I went to Vancouver to see this famous Chinese doctor who is known for his treatments… I was given Chinese medicine… I have continued taking it even when I was undergoing chemotherapy… I have felt better psychologically… No side effect and it has strengthened my body. The medicine was high in protein so it kind of saved my life because I was not eating enough.”—002F.
3.4. Sociocultural Barriers to Supportive Care
3.4.1. Limited Understanding of the Medical System
“In fact two years before I had done couple of ultrasounds but nothing was detected. I find this the most frustrating thing.”—015M.
“They (doctors) didn’t need to do many check-ups in China, things like cardiogram, in order to operate on you. But here you would need to check many things, like cardiogram and EEG, to make sure your heart and lungs are good. It (the process for surgery) was a lot simpler in China.”—011M.
3.4.2. Deference to Authority
“Because I don’t think (psychosocial support) is necessary, so I didn’t look for them… doctor’s explanation is enough. I did ask my doctor about taking Chinese medicine but he told me not to take it because I was going to get chemotherapy and radiotherapy… I have heard about combining Chinese and Western medical treatments for cancer but I decided to listen to my doctor.”—008M.
“The (Canadian) doctor said that it’s best not to remove it for my age. Radiotherapy was fine, this way the body wouldn’t be too depleted. But back in China, they said it’s best to remove it. Because I trust the doctors in China very much. They are all professors. Plus, they’ve seen thousands of cases a year.”—010M.
3.4.3. Cultural Clashes with Healthcare Providers
“The triage nurse wouldn’t let me in so I walked over there and confronted her. Then she told me that everyone else was more urgent than I was, I was so furious as if my eyes were going to pop… I replied ‘How do you know that I am not urgent?’ Actually, my head, my hands and my legs were all covered with acupuncture needles. I couldn’t wear shoes so I was in my slippers.”—018F.
3.4.4. Cancer Stigma
“So I asked them to take it (ostomy bag) off within 2 months… Back then I didn’t always want to go outside. I didn’t want to go to things like weddings and gatherings… I didn’t want to tell others but now I’m open about it. If I tell others about this, they’d think that I deserve this.”—001F.
“Now when I go out, I won’t eat anything. If anything were to happen, I wouldn’t be eating outside. Rather, I’d eat at home because I can go to the washroom whenever I want, right? …I’m always worried that I would need to buy bigger-sized t-shirts to make sure it covers my ostomy bag.”—001F.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Statistics Canada. The Canadian Census: A Rich Portrait of the Country’s Religious and Ethnocultural Diversity. 2021. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/221026/dq221026b-eng.htm (accessed on 11 July 2023).
- Trinh, Q.-D.; Li, H.; Meyer, C.P.; Hanske, J.; Choueiri, T.K.; Reznor, G.; Lipsitz, S.R.; Kibel, A.S.; Han, P.K.; Nguyen, P.L.; et al. Determinants of cancer screening in Asian-Americans. Cancer Causes Control. 2016, 27, 989–998. [Google Scholar] [CrossRef] [PubMed]
- Coplan, B. An Ecological Approach to Understanding Preventive Service Utilization Among the Underserved. Fam. Community Health 2018, 41, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Mason, S.E.; Scott, A.J.; Markar, S.R.; Clarke, J.M.; Martin, G.; Beatty, J.W.; Sounderajah, V.; Yalamanchili, S.; Denning, M.; Arulampalam, T.; et al. Insights from a global snapshot of the change in elective colorectal practice due to the COVID-19 pandemic. PLoS ONE 2020, 15, e0240397. [Google Scholar] [CrossRef] [PubMed]
- Patt, D.; Gordan, L.; Diaz, M.; Okon, T.; Grady, L.; Harmison, M.; Markward, N.; Sullivan, M.; Peng, J.; Zhou, A. Impact of COVID-19 on Cancer Care: How the Pandemic Is Delaying Cancer Diagnosis and Treatment for American Seniors. JCO Clin. Cancer Inform. 2020, 4, 1059–1071. [Google Scholar] [CrossRef] [PubMed]
- Nwankwo, E.C.; Hendrix, C.; Pollard, K.; Kallal, C.; Cruschiel, T.; Buckhold, F.; Hachem, C. Epidemiologic disparities in colon cancer screening and adherence during the COVID-19 pandemic: A retrospective cohort analysis. Int. J. Color. Dis. 2022, 37, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Butow, P.; Bell, M.; Goldstein, D.; Sze, M.; Aldridge, L.; Abdo, S.; Mikhail, M.; Dong, S.; Iedema, R.; Ashgari, R.; et al. Grappling with cultural differences; Communication between oncologists and immigrant cancer patients with and without interpreters. Patient Educ. Couns. 2011, 84, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Kwok, C.; White, K. Cultural and linguistic isolation: The breast cancer experience of Chinese-Australian women—A qualitative study. Contemp. Nurse 2011, 39, 85–94. [Google Scholar] [CrossRef]
- Leung, A.Y.M.; Bo, A.; Hsiao, H.-Y.; Wang, S.S.; Chi, I. Health literacy issues in the care of Chinese American immigrants with diabetes: A qualitative study. BMJ Open 2014, 4, e005294. [Google Scholar] [CrossRef]
- Rahman, R. Characteristics of gastric cancer in Asia. World J. Gastroenterol. 2014, 20, 4483–4490. [Google Scholar] [CrossRef]
- Wang, Z.J.; Ramcharan, S.; Love, E.J. Cancer Mortality of Chinese in Canada. Leuk. Res. 1989, 18, 17–21. [Google Scholar] [CrossRef]
- Li, C.-C.; Matthews, A.K.; Dong, X. The Influence of Health Literacy and Acculturation on Cancer Screening Behaviors Among Older Chinese Americans. Gerontol. Geriatr. Med. 2018, 4, 2333721418778193. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.L.; Tsoh, J.; Davis, T.; Davis, J.; Braun, K.L. Low health literacy and cancer screening among Chinese Americans in California: A cross-sectional analysis. BMJ Open 2015, 5, e006104. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.Y.; Li, J.; Li, K. Cervical Cancer Screening Experiences Among Chinese American Immigrant Women in the United States. J. Obstet. Gynecol. Neonatal Nurs. 2018, 47, 52–63. [Google Scholar] [CrossRef] [PubMed]
- Sarpel, U.; Huang, X.; Austin, C.; Gany, F. Barriers to Care in Chinese Immigrants with Hepatocellular Carcinoma: A Focus Group Study in New York City. J. Community Health 2018, 43, 1161–1171. [Google Scholar] [CrossRef] [PubMed]
- Shaw, S.J.; Huebner, C.; Armin, J.; Orzech, K.; Vivian, J. The Role of Culture in Health Literacy and Chronic Disease Screening and Management. J. Immigr. Minor. Health 2008, 11, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Oyserman, D.; Coon, H.M.; Kemmelmeier, M. Rethinking individualism and collectivism: Evaluation of theoretical assumptions and meta-analyses. Psychol. Bull. 2002, 128, 3–72. [Google Scholar] [CrossRef] [PubMed]
- Lai, D.W.L.; Chau, S.B. Effects of service barriers on health status of older Chinese immigrants in Canada. Soc. Work. 2007, 52, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Wong-Kim, E.; Sun, A.; Merighi, J.R.; Chow, E.A. Understanding quality-of-life issues in Chinese women with breast cancer: A qualitative investigation. Cancer Control. 2005, 12 (Suppl. S2), 6–12. [Google Scholar] [CrossRef] [PubMed]
- Aroian, K.J.; Wu, B.; Tran, T.V. Health care and social service use among Chinese immigrant elders. Res. Nurs. Health 2005, 28, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Butow, P.N.; Sze, M.; Eisenbruch, M.; Bell, M.L.; Aldridge, L.J.; Abdo, S.; Tanious, M.; Dong, S.; Iedema, R.; Vardy, J.; et al. Should culture affect practice? A comparison of prognostic discussions in consultations with immigrant versus native-born cancer patients. Patient Educ. Couns. 2013, 92, 246–252. [Google Scholar] [CrossRef]
- Leng, J.; Lei, L.; Lei, S.F.; Zhu, Z.; Ocampo, A.; Gany, F. Use of Traditional Chinese Herbal Medicine Concurrently with Conventional Cancer Treatment Among Chinese Cancer Patients. J. Immigr. Minor. Health 2020, 22, 1240–1247. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.W.; Kazanjian, A.; Wong, H. Why do Chinese Canadians not consult mental health services: Health status, language or culture? Transcult. Psychiatry 2009, 46, 623–641. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W. Is Death Taboo for Older Chinese Immigrants? Omega 2022, 84, 1061–1080. [Google Scholar] [CrossRef] [PubMed]
- Hines, S.C.; Glover, J.J.; Babrow, A.S.; Holley, J.L.; Badzek, L.A.; Moss, A.H. Improving advance care planning by accommodating family preferences. J. Palliat. Med. 2001, 4, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Lynn, J.; Goldstein, N.E. Advance care planning for fatal chronic illness: Avoiding commonplace errors and unwarranted suffering. Ann. Intern. Med. 2003, 138, 812–818. [Google Scholar] [CrossRef] [PubMed]
- Bowman, K.W.; Singer, P.A. Chinese seniors’ perspectives on end-of-life decisions. Soc. Sci. Med. 2001, 53, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Lai, D.W.L.; Chau, S.B.Y. Predictors of health service barriers for older Chinese immigrants in Canada. Health Soc. Work. 2007, 32, 57–65. [Google Scholar] [CrossRef]
- Chen, L.-M.; Miaskowski, C.; Dodd, M.; Pantilat, S. Concepts within the Chinese culture that influence the cancer pain experience. Cancer Nurs. 2008, 31, 103–108. [Google Scholar] [CrossRef]
- Leung, A.Y.M.; Cheung, M.K.T.; Chi, I. Relationship among patients’ perceived capacity for communication, health literacy, and diabetes self-care. J. Health Commun. 2014, 19 (Suppl. S2), 161–172. [Google Scholar] [CrossRef]
- Chou, F.-Y.; Dodd, M.; Abrams, D.; Padilla, G. Symptoms, self-care, and quality of life of Chinese American patients with cancer. Oncol. Nurs. Forum 2007, 34, 1162–1167. [Google Scholar] [CrossRef]
- Htut, Y.; Shahrul, K.; Poi, P. The views of older Malaysians on advanced directive and advanced care planning: A qualitative study. Asia Pac. J. Public Health 2007, 19, 58–66. [Google Scholar] [CrossRef]
- Lu, Y.; Racine, L. Reviewing Chinese immigrant women’s health experiences in English-speaking Western Countries: A postcolonial feminist analysis. Health Sociol. Rev. 2015, 24, 15–28. [Google Scholar] [CrossRef]
- Simon, M.A.; Tom, L.S.; Taylor, S.; Leung, I.; Vicencio, D. ‘There’s nothing you can do…it’s like that in Chinatown’: Chinese immigrant women’s perceptions of experiences in Chicago Chinatown healthcare settings. Ethn. Health 2021, 26, 893–910. [Google Scholar] [CrossRef]
- Armstrong, T.L.; Swartzman, L.C. Cross-Cultural Differences in Illness Models and Expectations for the Health Care Provider-Client/Patient Interaction. In Handbook of Cultural Health Psychology; Elsevier: Amsterdam, The Netherlands, 2001; pp. 63–84. [Google Scholar] [CrossRef]
- Chen, Y. Chinese values, health and nursing. J. Adv. Nurs. 2001, 36, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Sandelowski, M. Whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Sandelowski, M. Qualitative analysis: What it is and how to begin. Res. Nurs. Health 1995, 18, 371–375. [Google Scholar] [CrossRef]
- Huang, R. RQDA: R-Based Qualitative Data Analysis. R Package version 0.2-8. 2016. Available online: http://rqda.r-forge.r-project.org/ (accessed on 7 January 2016).
- Kwok, W.; Bhuvanakrishna, T. The relationship between ethnicity and the pain experience of cancer patients: A systematic review. Indian J. Palliat. Care 2014, 20, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.-Y.; Pilkington, F.B.; Ho, G. Living with Cancer: The Experiences of Chinese Canadian Cancer Survivors. Int. J. Psychol. Stud. 2014, 6, p106. [Google Scholar] [CrossRef]
- Costante, A.; Lawand, C.; Cheng, C. Access to Palliative Care in Canada. World Health Popul. 2019, 21, 10–12. [Google Scholar] [CrossRef]
- Laporte, A.; Nauenberg, E.; Shen, L. Aging, social capital, and health care utilization in Canada. Health Econ. Policy Law 2008, 3, 393–411. [Google Scholar] [CrossRef]
- Ng, E.; Sanmartin, C.; Tu, J.; Manuel, D. Use of acute care hospital services by immigrant seniors in Ontario: A linkage study. Health Rep. 2014, 25, 15–22. [Google Scholar] [PubMed]
- Todd, L.; Hoffman-Goetz, L. A Qualitative Study of Cancer Information Seeking Among English-as-a-Second-Language Older Chinese Immigrant Women to Canada: Sources, Barriers, and Strategies. J. Cancer Educ. 2011, 26, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, L.C.; Smith, S.G. Cancer Fatalism, Literacy, and Cancer Information Seeking in the American Public. Health Educ. Behav. 2016, 43, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Liu, J.; Yuan, Y.C. Cultural Differences in Cancer Information Acquisition: Cancer Risk Perceptions, Fatalistic Beliefs, and Worry as Predictors of Cancer Information Seeking and Avoidance in the U.S. and China. Health Commun. 2022, 37, 1442–1451. [Google Scholar] [CrossRef] [PubMed]
- Powe, B.D.R.; Finnie, R.M. Cancer fatalism: The state of the science. Cancer Nurs. 2003, 26, 454–465. [Google Scholar] [CrossRef] [PubMed]
- Fong, T.C.T.; Ho, R.T.H. Re-examining the factor structure and psychometric properties of the Mini-Mental Adjustment to Cancer Scale in a sample of 364 Chinese cancer patients. Support. Care Cancer 2015, 23, 353–358. [Google Scholar] [CrossRef][Green Version]
- Mechanic, D.; Homer, J.; Milstein, B.; Hirsch, G.B.; Fisher, E.S.; Tanner, J.; Williams, D.R.; Jackson, P.B.; Marmot, M.; Berwick, D.M.; et al. Disadvantage, Inequality, And Social Policy. Health Aff. 2002, 21, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Powe, B.D.; Johnson, A. Fatalism as a barrier to cancer screening among African-Americans: Philosophical perspectives. J. Relig. Health 1995, 34, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, L.N.; Gottlieb, B.; Shamian, J. Principles of strengths-based nursing leadership for strengths-based nursing care: A new paradigm for nursing and healthcare for the 21st century. Nurs. Leadersh. 2012, 25, 38–50. [Google Scholar] [CrossRef]
- Morrison, V.D.; Hauch, R.R.D.; Perez, E.M.; Bates, M.D.; Sepe, P.M.; Dans, M.M. Diversity, Equity, and Inclusion in Nursing. Nurs. Adm. Q. 2021, 45, 311–323. [Google Scholar] [CrossRef]
- Kwong, K.; Mak, A. Health Care and Cancer Screening Experience of Chinese Immigrants in New York City: A Qualitative Study. Soc. Work. Health Care 2009, 48, 321–347. [Google Scholar] [CrossRef] [PubMed]
| Sex | |
| Male | 15 (75) |
| Age | |
| >70 | 6 (30) |
| 66–70 | 5 (25) |
| 60–65 | 9 (45) |
| Employment status | |
| Full time | 2 (10) |
| Part time | 3 (15) |
| Unemployed | 13 (65) |
| Retired | 1 (5) |
| Permanent disability | 1 (5) |
| Education | |
| Less than elementary | 1 (5) |
| Elementary | 5 (25) |
| High school | 5 (25) |
| University, college or higher | 9 (45) |
| Location of disease | |
| Liver | 6 (30) |
| Colorectal | 9 (45) |
| Pancreatic | 3 (15) |
| Other locations | 2 (10) |
| Stages of disease | 3 |
| II | 3 (15) |
| III | 2(10) |
| IV | 9 (45) |
| Unstated | 6 (30) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leung, Y.W.; Kwong, E.W.Y.; Wong, K.L.Y.; So, J.; Poon, F.; Cheng, T.; Chen, E.; Molasiotis, A.; Howell, D. Understanding Elderly Chinese Cancer Patients in a Multicultural Clinical Setting: Embracing Mortality and Addressing Misperceptions of Vulnerability. Curr. Oncol. 2024, 31, 2620-2635. https://doi.org/10.3390/curroncol31050197
Leung YW, Kwong EWY, Wong KLY, So J, Poon F, Cheng T, Chen E, Molasiotis A, Howell D. Understanding Elderly Chinese Cancer Patients in a Multicultural Clinical Setting: Embracing Mortality and Addressing Misperceptions of Vulnerability. Current Oncology. 2024; 31(5):2620-2635. https://doi.org/10.3390/curroncol31050197
Chicago/Turabian StyleLeung, Yvonne W., Enid W. Y. Kwong, Karen Lok Yi Wong, Jeremiah So, Frankie Poon, Terry Cheng, Eric Chen, Alex Molasiotis, and Doris Howell. 2024. "Understanding Elderly Chinese Cancer Patients in a Multicultural Clinical Setting: Embracing Mortality and Addressing Misperceptions of Vulnerability" Current Oncology 31, no. 5: 2620-2635. https://doi.org/10.3390/curroncol31050197
APA StyleLeung, Y. W., Kwong, E. W. Y., Wong, K. L. Y., So, J., Poon, F., Cheng, T., Chen, E., Molasiotis, A., & Howell, D. (2024). Understanding Elderly Chinese Cancer Patients in a Multicultural Clinical Setting: Embracing Mortality and Addressing Misperceptions of Vulnerability. Current Oncology, 31(5), 2620-2635. https://doi.org/10.3390/curroncol31050197






